Abstract
Chronic lower back pain is a potentially incapacitating condition associated with disc degeneration. Although therapy is primarily pharmaceutical, surgery comprising arthrodesis constitutes an alternative. Anterior intersomatic lumbar arthrodesis (ALIF, anterior interbody lumbar fusion) is the reference approach, although total disc arthroplasty may also be undertaken. Analysis of pelvic and spinal parameters provides the best indication of sagittal balance.
Materials and methods
This was a prospective study in a continuous series of 99 patients presenting chronic lower back pain due to disc disease. Pelvic incidence, sacral slope, pelvic tilt, spino-sacral angle (SSA) and the four back types in the Roussouly classification were studied in radiographs of the whole spine under load using an EOS imaging system.
Results
The pre-operative SSA value for the study population was 126.09° ± 8.45° and the mean spine tilt angle was 90° compared with 95° in healthy subjects. Following surgery, the SSA was considerably increased in the discal arthroplasty, resulting in a significantly more balanced spinal position. In the group of patients undergoing arthrodesis using the ALIF technique, no such significant improvement was found despite the use of a lordosis cage. We showed that in cases of low pelvic incidence, it was necessary to maintain a Roussouly type 1 or 2 back without increasing lordosis. The results demonstrated the value of L4–L5 disc prostheses in these subjects. L5–S1 arthrodesis seemed a more suitable approach for treating patients with elevated sacral slope (back type 3 or 4). This new type of analysis of sagittal parameters should be performed prior to all surgical procedures involving lumbar prostheses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
One of the essential roles of the spine is to support mechanical loads in the upright position. While in this position, humans are never completely immobile but are in fact continually adjusting their balance by means of micro-movements, thereby ensuring that the body’s centre of gravity remains harmoniously within a base of support in a fashion requiring minimal muscular effort. This is the definition of economic sagittal balance [1].
According to Barrey [1], patients with chronic lower back pain presented a minor balance defect. In order to verify this hypothesis, we conducted a comparative study of pelvic–spinal sagittal parameters in a group of patients with lower back pain of disc origin before and after surgical disc treatment alone.
We investigated the effects of two surgical techniques (anterior lumber intersomatic arthrodesis, or ALIF, and total disc prosthesis) on spinal status with analysis of all pelvic and spinal parameters, in particular spino-sacral angle [1] (SSA), preoperatively and post-operatively. The aim of the study was to identify any difference in results in order to create a decision-making algorithm based on initial spinal–pelvic configuration.
Materials and methods
All patients in the study were recruited following multidisciplinary meetings for spinal disease and underwent surgery at the Spinal Unit 2 of the Bordeaux University Hospital. This was a continuous, non-randomised, single-centre prospective cohort study of all patients undergoing surgery between June 2002 and October 2007 for disc-related anterior lumbar surgery. Every second patient was assigned to one of the following groups: ALIF or total disc prosthesis. No criteria clearly identified in the literature indicate the superiority of either of these two techniques, and the study was approved by the Ethics Committee of the University of Bordeaux 2 in 2002. One series of patients received Maverick® disc prostheses (Medtronic, Memphis, USA) while the other underwent anterior arthrodesis using the ALIF technique involving a Perimeter® 12° lordosis cage, a Union® 10° lordosis cage or a Pyramid® plate (Medtronic™, Memphis, USA) together with an autograft in the cage or bone morphogenic protein type Rh-BMP 2 (Inductos® Medtronic, Memphis, TN, USA). 300 patients were included in the study and we analysed patients with more than 2 years of follow-up (minimum follow-up 3 years, maximum 6 years). Thus, 99 patients were selected for this study.
Patients were operated by the same surgeon using an identical surgical procedure: a minimally invasive, video-assisted left retroperitoneal approach, in dorsal decubitus, placed in the so-called “French” position.
Inclusion criteria All patients had been presenting lower back pain for more than 6 months and pharmaceutical therapy had failed. No other pain was associated with degenerative lumbar disc disease at a single level, as confirmed by MRI imaging. Discography was not performed routinely. The disc disease was either primary or secondary to a percutaneous disc procedure or discectomy. The lower back pain was either isolated or associated with minimal radicular pain. In all cases, radicular pain was inferior to lower back pain in terms of score on a pain visual analogue scale. Discectomy by the anterior route using the ALIF technique was considered effective in eliminating any minimal radicular compression.
General exclusion criteria Osteoporosis and bone diseases, local and systemic infection, morbid obesity (BMI > 35); spondylolisthesis, prior lumbar spinal surgery other than lumbar discectomy, absence of ongoing disease, confirmed serious psychiatric disorder, inability to complete a minimum period of 2-year follow-up.
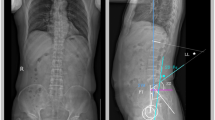
Radiological evaluation criteria All patients underwent frontal and lateral standing lumbar spine radiography, and long-cassette whole-spine radiography, as well as lateral radiography in flexion and extension. MRI was performed in all cases with analysis of the free vertebral vessels (angioMRI). Analysis of pre- and post-operative radiological data was performed using Optispine® software (Optimage, Lyon, France), version 2007/10 (Fig. 1). Inter- and extra-observer validation for this software was performed for 4 observers by analysis of 60 cases. The inter-observer reproducibility test result was between 0.92 and 0.99, while the intra-observer reproducibility test result was between 0.93 and 0.99 [2]. The straightforward reading of directions and of a number of radiologically identifiable points ensured swift and reproducible automatic geometric construction of the sagittal curves of the spine. The reproducibility of these parameters was validated by this clinical study. Regardless of the parameter analysed, using this computerised approach, inter- and intra-observer variability was better than measurements made manually. This optimisation was associated with the use of digital images allowing image processing (e.g. better analysis of vertebral contours) by varying luminosity, contrast or magnification.
Pelvic parameters
The following pelvic parameters were measured pre-operatively and post-operatively: sacral slope (SS), pelvic tilt (PT) and pelvic incidence (PI) according to Legaye [3] and Duval-Beaupere [4].
Using the software, routine analysis was carried out of other variables, such as those described by Jackson [5]:
-
angle of pelvic rotation or PA (pelvic angle), linear pelvic parameters: HA-S1 (hip axis and S1 vertebra) and HA-SP, comprising the horizontal distance between the vertical bicoxofemoral axis (hip axis) and a vertical line passing through the posterior superior corner of the superior sacral endplate (S1), i.e. HA-S1, and the vertical line passing through the sacral promontory, i.e. HA-SP, in millimetres. Finally, the PRS1 angle, calculated using the Jackson’s pelvic radius technique [5], a constant morphological pelvic parameter in the same way as pelvic incidence.
Spinal parameters
The angle of distal lordosis, C1 according to Roussouly [6], defined by the lumbar apex and the inflection point, allowing construction of the kyphotic angle, C2 (i.e. thoracic curve), and the number of vertebrae involved in each curve.
The tilt angle, RT, which defines the overall orientation of distal lordosis, between the vertical and the inflection point. This value was positive if the spine tilted forward of this vertical, indicating inadequate lordosis.
Back type [6], indicating the morphology of the distal (lumbar) lordosis, was classified as one of four types, according to sacral slope value, defining a characteristic spinal morphology and allowing prediction of local and general biomechanical phenomena of the spine potentially responsible for certain degenerative diseases such as spondylolisthesis, facet syndrome, disc disease, etc.
Sagittal balance parameters
The SSA formed by a straight line through the centre of the S1 endplate and the centre of C7 and the orientation of the sacral endplate (Fig. 2); this is an intrinsic parameter [7]. In a balanced spine, SSA is extremely strongly correlated with the sacral slope angle (R = 0.91, P < 0.001) according to Roussouly [7] and this could be an important parameter in analysis of the study population.
The horizontal distance between the C7 plumb line and the vertical passing through the posterior superior corner of S1, i.e. S1–C7. This index for the position of C7 described by Barrey [1] as the ratio of S1–C7 to HA-S1 ranged between 0 and 1 or more where global balance was positioned in front of the posterior corner of S1 (unbalanced spine), and was negative position where it was behind (balanced spine).
Statistics
Statistical calculations were performed with the help of the Public Health Department (ISPED) of the Medical Faculty of Bordeaux 2.
Data were entered anonymously using Excel software (Microsoft, CA, USA) and then processed using EPI-INFO 3.5.1 software for the descriptive part of the analysis and with SPSS 14.0 software for the comparative study. Graphs were generated using Excel.
For the description of the study population, qualitative variables were described in terms of patient numbers and percentages while quantitative variables were described in terms of patient numbers, mean values, and standard deviations (and range or median and interquartile range) according to data distribution.
Pre- and post-operative quantitative data were compared using tests for paired data: Student’s t test (comparison of means) with a significance level of 0.05 (type I error).
Correlations between two quantitative variables were determined by Pearson correlation analysis.
Results
The effect of each surgical technique on pelvic-spinal balance parameters is given in Tables 1 and 2
The SSA was increased significantly; disc arthroplasty resulted in a more balanced spinal position, approaching the mean seen in an asymptomatic population (135°) [1]. The C7 plumb line was shifted behind the posterior superior corner of S1 and became negative. The RC7 position index, the S1-C7/HA-S1 ratio, described by Barrey, was shifted towards the global ideal anatomic plane of balance, moving just behind the posterior superior corner of S1 (Fig. 3).
The effect of the fused level on pelvic-spinal balance parameters was studied separately
The results for L5-S1 in the prosthesis group are shown in Table 3. A significant increase was seen in SSA, as well as backward displacement of the C7 plumb line. The C7 position index showed a tendency to decrease, becoming negative, although this decrease was not significant. The results for L4–L5 in the prosthesis group are shown in Table 4. The SSA increased, but not significantly, while the post-operative plumb line had moved behind the posterior superior angle at S1. In addition, a significant increase was seen in HA-S1 distance (Fig. 4).
Type 3 spine according to Roussouly’s classification, a preoperatively there is lost of lumbar lordosis, and b postoperatively after total disc arthroplasty at level L4/L5 there is an increase of the segmental lordosis without modification of the global lumbar lordosis. Preop SS is 46.7° and postoperatively due to the restoration of L4/L5 disc height the spine recovered its original shape corresponding to a type 3. SSA preop: 124°, SSA postop: 134°
The effect of preoperative back type was analysed for both groups using the various parameters. The SSA angle was distributed in increasing fashion between type 1 and type 4: from 117° to 137° with a mean angle of 126°. The mean spine tilt angle for each back type, obtained by subtraction of SSA and PS, was 90° compared with a mean 95° for healthy subjects according to Barrey [1]. No change was seen in S1-C7 post-operatively for types 1 and 2. Comparative analysis of variance (ANOVA) for each variable across several groups showed a clear difference in the 4 back types in terms of pelvic parameters (PI, PT, PS and SSA) but not of balance parameters (S1-C7, HA-S1 and C7 ratio). The difference in terms SSA found preoperatively between the different back types was not seen post-operatively.
Pearson’s correlation analysis of the parameters is shown in Table 5. The SSA was highly correlated with incidence (R = 0.73, p < 0.001), sacral slope (R = 0.92, p < 0.001) and distal lumbar lordosis. It was negatively correlated with the C7 plumb line (R = −0.24, p = 0.02).
Discussion
Analysis of the two series of patients presenting chronic lower back pain predominantly of disc origin showed no difference between the two treated groups, demonstrating homogeneity of selection. Roussouly [7] defined a mathematical formula associating SSA angle and sacral slope: SSA = 0.96SS + 97°. This was a constant geometric relationship between the position of the top of the spine and the sacral slope. In an asymptomatic spinal balance population (n = 160), he found the mean angle to be 135° ± 7.8°. He noted that SSA was extremely closely correlated with sacral slope. We observed this correlation (R = 0.921) in our population of patients with lower back pain of disc origin. Roussouly also indicated spine tilt (ST) or spinal balance using the formula: ST = SSA − SS; in other words, regardless of the orientation of the sacral endplate, the angle formed by the sacrum/C7 line and the horizontal was approximately 95°, i.e. spinal balance of 5° backwards (in relation to the vertical). This formula was not used for patients in our series, for whom the value calculated from the sacral slope produced a higher theoretical angle than that determined by the software, indirectly confirming that our patients were imbalanced, while also accounting for the fact that they were symptomatic. We found a mean ST value of 90° corresponding to forward balance of 5° for the vertebral column in this series of patients with lower back disc disease at only one level.
In a series of 32 patients with disc disease similar to that of our patients, Barrey [1] found an SSA of 127 ± 11.3. The characteristics of these patients were similar to those of our own in terms of sex ratio M/F, age and BMI. We found a similar value for SSA of 126.09 ± 8.45. However, our series was three times larger, thus emphasising this characteristic feature of lumbar back pain of disc origin. Thus, like Jackson [5], we confirmed anterior spinal imbalance in lower back pain associated with disc degeneration.
In an asymptomatic population, no “standard position” was found. Sagittal spinal balance is defined at any given moment by the position of the spinal column in relation to a particular posture, and this reflects only one part of a continually changing dynamic status. It represents a state of energy economy for the body and of minimal mechanical effort. The anterior imbalance we found in lumbar disc degeneration was also related to loss of lumbar lordosis, and cannot be accounted for by disc disease alone and loss of disc height, and in addition to this isolated structural component there is likely to be a postural component probably caused by patients efforts to avoid pain [8].
In the arthroplasty group, the presence of a disc prosthesis affected all spinal-pelvic balance parameters: SSA, C7 plumb line, HA-S1 and C7 ratio. Its role as a “regulator” was warranted and it allowed patients to position themselves in such a way as to achieve postural and muscular economy. Arthroplasty appears to work most effectively at L4–L5 for all back types, in accordance with Tournier [9]. It provided better control of sagittal balance, yielded a better defined mean centre of rotation and gave better clinical results without affecting the lordosis of the underlying L5–S1 segment. A disc prosthesis in L5–S1 appeared more suitable for backs with a lower sacral slope. Backs with a higher sacral slope produce increased shear constraints and reduce this regulator role due to reduced mobility of the prostheses [10]. It will be possible to vary the different sizes/heights and angles of prostheses in order to optimise their effect on L5–S1, although in practice this effect appeared very limited and random [9]. The ALIF group presented no significant improvement in SSA angle, allowing us to confirm that insertion of an intersomatic cage, even a lordosis cage (12° in this series), did not in fact restore lordosis but more generally resulted in restoration of disc height alone. Two levels DDD with fusion L5S1 and prosthesis L4L5 showed similar results [11].
We established the correlation between the lumbar–sacral angle and sacral slope and SSA, thus underlining the idea of the need for adaptation of lordosis to initial pelvic incidence and thus to a given preoperative back type in order to ensure the best possible spino-pelvic balance, and consequently postural economy.
Conclusion
Our study demonstrated marked anomalies in numerous sagittal balance parameters (HA-S1, S1-C7, C7 ratio, PLL, SSA, etc) in a setting of lower back pain of disc origin, and in particular in the SSA, for which measurement at the T9 site alone does not allow adequate assessment of these fine degrees of postural imbalance.
The tendency towards normalisation of the SSA angle confirmed the regulatory role of total disc prosthesis, which allows patients to position themselves appropriately, in contrast with arthrodesis, since fusion of L5 and S1 results in an unchanging position.
Use of the EOS™ system allowed more precise measurement of sagittal parameters, and in particular variables involving distance, since X-ray diffraction is corrected in the vertical plane. For example, we were able to measure the distance PLL in a 3D image of the spinal-pelvic complex. Computerised quantitative analysis should be used routinely in sagittal spinal studies and in preoperative planning in the same way as SSA.
References
Barrey C, Jund J, Noseda O, Roussouly P (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases: a comparative study about 85 cases. Eur Spine J 16:1459–1467
Berthonnaud E, Labelle H, Roussouly P, Grimard G, Vaz G, Dimnet J (2005) A variability study of sagittal spino-pelvic radiological measurements of trunk balance with the Sagittal OptiSoft® software. J Spinal Disord Tech 18:1
Legaye J, Hecquet J, Marty C et al (1993) Equilibre sagittal du rachis, relation entre bassin et courbures sagittales en position debout (in French). Rachis 5:215–226
Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20:451–462
Jackson RP, Kanemura T, Kawakami N et al (2000) Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine 25:575–586
Roussouly P, Gollogly S, Berthonnaud E et al (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30:346–353
Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J (2006) The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumbline: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine 31:E320–E325
Rajnics P, Pomero V, Templier A et al (2001) Computer-assisted assessment of spinal sagittal plane radiographs. J Spinal Disord 14:135–142
Tournier C, Aunoble S, Le Huec JC, Lemaire JP, Tropiano P, Lafage V, Skalli W (2007) Total disc arthroplasty: consequences for sagittal balance and lumbar spine movement. Eur Spine J 16:411–421
Le Huec JC, Basso Y, Mathews H, Mehbod A, Aunoble S, Friesem T, Zdeblick T (2005) The effect of single-level, total disc arthroplasty on sagittal balance parameters: a prospective study. Eur Spine J 14:480–486
Aunoble S, Meyrat R, Al Sawad Y, Tournier C, Leijssen P, Le Huec JC (2010) Hybrid construct for two levels disc disease in Lumbar Spine: a valid alternative to two levels disc arthroplasty. Eur Spine J 19:290–296
Acknowledgments
We would like to thank Prof. Chêne Geneviève, Dept. of Public Health (ISPED) of the Faculty of Medicine of Bordeaux 2, 146 rue Leo Saignat, 33076, Bordeaux, France.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pellet, N., Aunoble, S., Meyrat, R. et al. Sagittal balance parameters influence indications for lumbar disc arthroplasty or ALIF. Eur Spine J 20 (Suppl 5), 647 (2011). https://doi.org/10.1007/s00586-011-1933-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-011-1933-0