Abstract
A prospective radiographic study of the influence of total disc replacement on spinal sagittal balance. The goal of this study was to prospectively determine the effect of a single-level, total disc replacement on the sagittal balance of the spine, especially on sacral tilt (ST), pelvic tilt (PT), and lumbar lordosis. It has been shown that lumbar fusion may deleteriously alter the sagittal balance of the spine, including a decrease in the ST and lumbar lordosis. Clinically, postfusion pain has been shown to be significantly related to a decreased ST, increased PT, and decreased lumbar lordosis, independent of other factors such as pseudoarthrosis. To our knowledge, the influence of total disc replacement on spinal sagittal balance has not yet been reported in the literature. This is a prospective study of 35 patients who received a single level disc replacement using the Maverick Total Disc Arthroplasty system (Medtronic Sofamor Danek, Memphis, Tennessee) by a single surgeon at one institution from March 2002 to September 2003. The preoperative and postoperative radiographic evaluation included standing anteroposterior and lateral full spine films that included the femoral heads. The parameters studied were ST, PT, global and segmental lordosis, and global kyphosis. The average age of the 35 patients studied was 44.3 years (range 35–57). There were 18 females and 17 males. The disc arthroplasty was performed at the L4–L5 level in 19 patients and at the L5–S1 level in 16 patients. The average follow-up was 14 months (range 6–22 months). The preoperative values of global lordosis, ST, and PT were 51.5°, 37.8°, 16.9° and, at last follow-up, they were 51.4°, 37.4°, and 17.5°, respectively. These changes were not significantly different. When the groups were separated according to the level operated, there was still no statistical difference with regard to the overall lordosis, ST, PT or kyphosis from pre- to postoperative period or when the two groups were compared with each other. The level above the prosthesis has always significantly less lordosis. In the present study with use of a motion-preserving Maverick prosthesis, it appears that the patient is able to maintain the preoperative sagittal balance. The prosthesis has enough freedom of motion to allow the patient to maintain the natural sagittal and spinopelvic balance needed to prevent potential undue stress on the muscles and the sacroiliac joint. Although the number of patients is small, this is the first study to our knowledge that evaluates the sagittal balance after motion-preserving total disc arthroplasty.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Critical evaluation of surgical results has allowed for a better understanding of the importance of spinal sagittal balance and its influence on clinical outcomes of patients undergoing surgical interventions. Duval-Beaupere [2, 13] has shed considerable insight into understanding spinal sagittal balance and spinopelvic angulation, including variables such as sacral tilt (ST), pelvic tilt (PT) and their influence on lumbar lordosis. Multiple studies have reported on the spinal sagittal balance, including the aforementioned variables, in asymptomatic population of different age groups [4, 8, 11, 21, 22]. The correlation between the ST and lumbar lordosis has been well established [10, 11, 21]
As our understanding of sagittal balance has improved, we have become more aware of the harmful affects that surgical interventions may have on it. While spinal fusion has increased in popularity, though with variable clinical results, its effect on sagittal balance has recently been studied more critically. It has been shown that lumbar fusion may deleteriously alter the sagittal balance of the spine including a decrease in the ST and in lumbar lordosis [5, 6, 11, 18, 19]. The fused levels are locked in a position that is dependent on operative position [18, 19], geometry of the bone graft [5], and the surgical approach [6]. Additionally, postfusion pain has been shown to be significantly related to a decreased ST, increased PT, and decreased lumbar lordosis [11], independent of other factors such as pseudoarthrosis.
Our search for better treatment options for our patients has led us to motion-preserving total disc arthroplasty [12] to avoid fusion. Yet, the influence of motion preservation on sagittal balance of the spine has not been studied. The goal of this study was to prospectively determine the effect of a single-level total disc replacement on the sagittal balance of the spine, especially on ST, PT, and lumbar lordosis.
Materials and methods
This is a prospective study of 35 patients each of whom received a single-level disc replacement using the Maverick Total Disc Arthroplasty system by a single surgeon at one institution during the period March 2002 to September 2003. This study includes a subgroup of patients from one center participating in a multicenter trial evaluating the clinical results of the prosthesis and is only reporting on the effect of the arthroplasty on the sagittal balance of the patients. The clinical results with in-depth analysis will be presented when the 2-year clinical results from the patients are available.
The inclusion criteria to receive a prosthesis in this study were age of 18–60 years; primary complaint of back pain; symptomatic single-level degenerative disc at L4–L5 or L5–S1 level confirmed by X-rays, magnetic resonance imaging and provocative discography; Oswestry score of at least 40; visual analog score of at least 40; and failure to achieve pain relief for at least 6 months of nonoperative care. Exclusion criteria included symptomatic multilevel disc degeneration, spondylolysis, spondylolisthesis, scoliosis, spinal tumors, infections, fracture, or evidence of facet joint arthropathy on computed-tomography scans.
Surgical device and procedure
The Maverick Total Disc Arthroplasty system used in this study is a device made up of two cobalt chrome parts that articulate together according to the principles of a ball and socket. The center of rotation is in the posterior half of the vertebra, below the vertebral end plate allowing controlled translation during flexion and extension. The prosthesis is anchored to the vertebral bodies via hydroxyapatite-coated fins. The prosthesis is available in three different diameters including small, medium, and large. Additionally, the prosthesis is available in three different heights including 10, 12, and 14 mm. Finally, the upper and lower parts of the prosthesis are available in either 3° or 6° of lordosis, which in combination allow a total lordosis of 6°, 9°, or 12 °. This lordosis is only for ease of insertion of the prosthesis into the disc space allowing the two parts of the prosthesis to be inserted parallel to the vertebral endplates. This lordosis does not affect the lordosis of the lumbar spine as the prosthesis is a ball and socket joint, which after insertion can obtain its own lordosis depending on the forces exerted on it by the patient. This ball and socket joint allows for 32° of motion.
The surgical technique has been well described, but it will be summarized briefly here. The patient is positioned supine on the operating table in the French position—a supine position with legs spread apart laterally to allow the surgeon to stand between the legs facing the lumbar spine in a cephalad–caudad direction which is ergonomic for verifying the midline of the vertebral bodies for precise insertion of the disc prosthesis. The exposure of the spine is via a video-assisted retroperitoneal approach. The disc space is prepared in standard fashion, with removal of the anterior annulus, the nucleus, and posterior annulus. The lateral annulus and the posterior longitudinal ligament are conserved. A thorough posterior release is performed under fluoroscopy including removal of the posterior osteophytes and release of the PLL from the edge of the vertebral end plates on either side of the disc space. The vertebral endplates are prepared with maintenance of the subchondral bone to prevent subsidence. The preparation and insertion of the Maverick prosthesis are performed according to the manufacturer’s recommendations.
Postoperatively, the patients are encouraged to ambulate and start a rehabilitation program of conditioning, strengthening, and motion exercises. The patients are evaluated clinically and radiographically at 6 weeks, 3 months, 6 months, and 12 months after the operation.
Radiographic evaluation
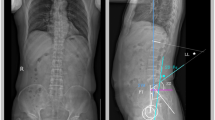
The preoperative and postoperative radiographic evaluation involved standing antero-posterior and lateral full spine films which included the femoral heads. The patient was asked to stand straight with arms folded across the chest, and knees fully extended. The radiographic parameters studied were based on the study of Duval Beaupere [2, 13], Vaz [21], and Lazennec [11]. When the femoral heads were not exactly superimposed on each other, the middle of the segment connecting the center of the femoral heads was used. The parameters studied were (Figs. 1, 2a–d):
-
1.
ST—angle formed between the sacral endplate and the horizontal
-
2.
PT—angle formed between the vertical plane and the line connecting the center of the hip to the center of the sacral endplate
-
3.
Global lordosis—angle formed between the upper endplate of L1 and the sacral endplate
-
4.
Segmental lordosis L4–L5—angle formed between the upper endplate of L4 and lower endplate of L5
-
5.
Segmental lordosis L5–S1—angle formed between the upper endplate of L5 and the sacral endplate
-
6.
Global kyphosis—angle between the upper endplate of T4 and lower endplate of T12
The pelvic incidence is a constant for each individual and is the geometric sum of ST and PT. Since it is a constant in each individual, it was not studied. All radiographs were digitized and the landmarks and angles were created by one single senior radiologist. The inter- and intra-observer variability of Cobb-angle measurements has been studied previously [3, 15, 16, 20]. A comparison of manual versus computer-assisted radiographic measurement has also been performed, and the intra-observer variability for manual and computer Cobb angle measurements yielded a 95% confidence interval of approximately 3°, with the computer having a slightly lower variability [17]. The computer technique removes sources of intrinsic error such as the variability of using different manual protractors, the inaccuracy of manual protractors, and the use of wide-diameter radiographic markers.
a Preoperative radiograph in which the angles created by line 1 are sacral tilt (ST) and those created by line 2 are pelvic tilt (PT). b Postoperative radiograph where angles created by line 1 are PT, and those created by line 2 are ST; line 3 is pelvic incidence. c Measurement of overall kyphosis and lordosis preoperatively. d Measurement of postoperative overall kyphosis and lordosis
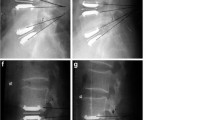
Additionally, flexion and extension lateral lumbar radiographs were evaluated for motion at the level of the prosthesis using Cobb angle measurements between the upper endplate of the upper vertebra and the lower endplate of the lower vertebra.
Statistical analysis
For analysis of our results, we utilized McNemar’s test for comparing two related series, the Mann Whitney test to compare medians of continuous values in unrelated samples, and Pearsons correlation coefficient for evaluating the relationships between variables.
Results
The average age of the 35 patients studied was 44.3 years (range 35–57). There were 18 females and 17 males. The disc arthroplasty was performed at the L4–L5 level in 19 patients and at the L5–S1 level in 16 patients. The average follow-up was 14 months (range 6–22 months).
The parameters studied preoperatively and postoperatively at last follow-up are presented in Table 1. The preoperative global lordosis, ST, and PT were 51.5°, 37.8°, 16.9° and at last follow-up, they were 51.4°, 37.4°, and 17.5°, respectively. These changes were not significantly different. Additionally, there was no significant difference in the preoperative and postoperative values of the other variables studied: the kyphosis, segmental lordosis of L4–L5 or the segmental lordosis of L5–S1.
We then separated the groups according to the level operated. The data are presented in Table 2, 3. There was no statistical difference with regard to the overall lordosis, ST, PT, or kyphosis when the two groups were compared with each other. In the L4–L5 group, the segmental lordosis was significantly increased after the total disc arthroplasty. Similarly, in the L5–S1 group, the segmental lordosis was significantly increased after the total disc arthroplasty. While the prosthesis increased lordosis at the level implanted, the overall lordosis did not change, thus indicating the adaptability of the spine as a whole to maintain lordosis. Again, in this subgroup analysis, there was no statistical difference from preoperative to postoperative results of overall lordosis, ST, PT, or kyphosis.
Motion, defined as angular change of more than 3°, was observed in all 35 cases with average motion of 6.5°. At the L4–L5 level, the average motion was 7.3°, while at the L5–S1 level, it was 5.2°. When the prosthesis is implanted at level L5–S1, the level L4–L5 has significantly less lordosis postoperatively. It is the same when the prosthesis is at level L4–L5 (Table 2 and 3).
Clinical data was available for 6 months follow-up. The Oswestry improved from pre-op average of 42 to postoperative average of 22. The Oswestry improved by 15 points (i.e. 30%) in 82% of patients at this short follow-up. The visual analog scale improved from preoperative level of 7.5 to 3.0 at follow-up. The SF-36 score improved from preoperative level of 40 to 72 at follow-up. The clinical results will be presented more in depth when 2-years follow-up data are available.
Discussion
Sagittal balance of the spine has gained new interest, mainly due to a greater understanding of the topic. Duval-Beaupere [2, 13] described in detail the relationships between the pelvic anatomy and lumbar lordosis, concentrating on a fundamental anatomical pelvic parameter, the pelvic incidence. The pelvic incidence is an anatomical characteristic specific for each individual and remains constant for that individual. However, the parameters studied, including ST and PT, are changing variables that add up to be the pelvic incidence in a simple geometric relationship. Since then, many authors have studied the sagittal balance including these parameters in healthy asymptomatic individuals [4, 8, 11, 21, 22] to establish a data bank for “normal” asymptomatic individuals.
Vaz and Roussouly [21] prospectively analyzed the sagittal profile of 100 healthy adults between the ages of 20 years and 45 years with no history of spinal disorder. They used 30×90-cm sagittal radiographs and measured multiple variables including the lumbar lordosis, thoracic kyphosis, pelvic incidence, ST and PT. They reported on the averages and range of values for these parameters. They found a significant statistical correlation between the ST and lumbar lordosis. They concluded after much analysis that the spinal shape is adapted to the pelvic shape, the quantity of lordosis increasing with the ST, resulting in a good relationship between the spine and the pelvis. Our measurements of the variables in this patient population with degenerative disc disease were similar to these published results of asymptomatic individuals. We also found a significant correlation between the ST and the lumbar lordosis. Thus, in our opinion, the patients with degenerative disc disease do not have a major sagittal balance problem and hence this balance should not be altered. However, much of the surgical treatment that can be offered to patients with spine problems includes a spinal fusion which has been shown to deleteriously alter the sagittal balance of the spine including a decrease in the ST and lumbar lordosis [5, 6, 11, 18, 19]. The clinical significance of this was studied by Lazennec [11].
The only study that has evaluated the influence of spinal alignment on the occurrence and pattern of post-spinal-fusion pain is by Lazennec et al. [11]. They studied a group of 103 patients with an average age of 61 years and a mean follow-up of 2.8 years. They all underwent lumbosacral fusions for different diagnosis including degenerative disc in 44 patients, recurrent herniation in 12, spondylolisthesis in 9 and failed stabilization in 16. All patients were evaluated at follow-up by means of magnetic resonance imaging or computed-tomography scan and neuropsychiatrist evaluation in order to determine possible causes of pain, such as pseudoarthrosis, neurogenic pain, or psychopathology. The patients who were found to have classic etiologies for postoperative pain were excluded from the study. The remaining 81 patients were then studied to see whether sagittal balance could be correlated with the presence of postoperative pain. The patients were separated into two groups: patients with and without residual pain after surgery. Subsequently, measurements were done on full-length lateral radiographs of the spine with measurements of different parameters.
Overall, the fusion caused changes in the sagittal parameters, including a decrease in ST and an increase in PT. No statistical analysis was done on this finding. However, when comparing the patients without pain to those with pain, they found that the PT was significantly higher and the ST was significantly lower in patients with postfusion pain. Using logistic regression, the authors found the only prognostic factor for residual pain at last follow-up was the variable ST. They concluded that achieving a strong fusion should not be the only goal and that the position of the fused vertebra is an important parameter to minimize pain, the main risk being a decrease in the ST. Thus, it would be beneficial if one is able to maintain the patient’s sagittal balance, especially ST and PT.
With the advent of the total disc arthroplasty and the maintenance of the disc motion segment, it may be possible for the patients to maintain their sagittal balance as well. The maintenance of disc mobility has been studied and recently published by Lemaire [14], Griffith [7], Bertagnoli [1], and Huang [9]. Disc mobility was also evident in the present study. However, the influence of the total disc arthroplasty on the sagittal balance and its multiple variables has not been studied until now.
We have shown that the patient undergoing a single level disc replacement with the Maverick prosthesis is able to maintain the global preoperative sagittal balance parameters including lordosis, ST, and PT. We think that since motion is preserved in the disc arthroplasty, the patient is able to achieve his or her own equilibrium, one that puts the least amount of strain on the adjacent levels of the lumbar spine or on the sacroiliac joint. Spinal fusion, if done correctly with good technique, may be able to do the same. However, if for whatever reason the spinal fusion is not done correctly, and the sagittal balance of the patient is not in equilibrium, then there is potential of continued problems postoperatively as shown by Lazennec [11].
In this study, we have analyzed the sagittal balance parameters of patients with single-level degenerative disc disease. The preoperative values for these parameters were not different from the parameters studied for the asymptomatic volunteers of the same age in Vaz’s series. Thus, we do not believe that the sagittal balance is a problem in these individuals preoperatively. This is why the preoperative sagittal balance parameters stayed the same postoperatively. An interesting study would be to look at the effect of disc arthroplasty on patients with degenerative disc disease and sagittal imbalance.
In the present study, with use of a motion-preserving Maverick prosthesis, it appears that the patient is able to maintain the preoperative sagittal balance with no significant change in any of the variables studied, including ST, PT, or overall lordosis. The prosthesis has enough freedom of motion to allow the patient to achieve or maintain the natural sagittal and spinopelvic balance needed to prevent undue stress on the muscles and the sacroiliac joint. When a prosthesis is implanted at level L5–S1 or L4–L5, the local lordosis increases and the lordosis at the above level significantly decreases. Although the number of patients is small, this is the first study to our knowledge that evaluates the sagittal balance after motion preserving total disc arthroplasty. Future prospective randomized studies comparing fusion to disc replacement should include an evaluation of the pre- and postoperative sagittal balance to better understand the potential benefits presented in this study.
Conclusion (key phrases)
-
The influence of the total disc arthroplasty on the sagittal balance of the spine and its multiple variables has not been studied until now.
-
A significant correlation was found between ST and global lordosis, between ST and segmental lordosis at L4–L5 and between global lordosis and segmental lordosis at L4–L5, both preoperatively and after placement of a Maverick prosthesis.
-
Compared with the preoperative status, there was no significant change in any of the variables studied including ST, PT, or overall lordosis after placement of Maverick total disc arthroplasty.
-
In the present study with use of a motion-preserving prosthesis, it appears that the patient is able to maintain their preoperative sagittal balance.
References
Bertagnoli R, Kumar S (2002) Indications for full prosthetic disc arthroplasty: a correlation of clinical outcome against a variety of indications. Eur Spine J 11(Suppl 2):S131–S136
Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20(4):451–462
Espeland A et al (1998) Observer variation in plain radiography of the lumbosacral spine. Br J Radiol 71(844):366–375
Gelb DE et al (1995) An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine 20(12):1351–1358
Godde S et al (2003) Influence of cage geometry on sagittal alignment in instrumented posterior lumbar interbody fusion. Spine 28(15):1693–1699
Goldstein JA et al (2001) Lumbar sagittal alignment after fusion with a threaded interbody cage. Spine 26(10):1137–1142
Griffith SL et al (1994) A multicenter retrospective study of the clinical results of the LINK SB Charite intervertebral prosthesis. The initial European experience. Spine 19(16):1842–1849
Hammerberg EM, KB Wood (2003) Sagittal profile of the elderly. J Spinal Disord Tech 16(1):44–50
Huang RC et al (2003) Long-term flexion-extension range of motion of the prodisc total disc replacement. J Spinal Disord Tech 16(5):435–440
Korovessis P, Stamatakis M, Baikousis A (1999) Segmental roentgenographic analysis of vertebral inclination on sagittal plane in asymptomatic versus chronic low back pain patients. J Spinal Disord 12(2):131–137
Lazennec JY et al (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9(1):47–55
Le Huec JC et al (2003) Maverick Total Lumbar Disc Replacement: A prospective study and preliminary report of 30 cases at 1 year follow-up. In: Annual meeting of the spine society of Europe. Prague
Legaye J et al (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7(2):99–103
Lemaire JP et al (1997) Intervertebral disc prosthesis. Results and prospects for the year 2000. Clin Orthop 337:64–76
Ng JK et al (2001) Range of motion and lordosis of the lumbar spine: reliability of measurement and normative values. Spine 26(1):53–60
Polly DW Jr et al (1996) Measurement of lumbar lordosis. Evaluation of intraobserver, interobserver, and technique variability. Spine (discussion 1535–1536) 21(13):1530–1535
Shea KG et al (1998) A comparison of manual versus computer-assisted radiographic measurement. Intraobserver measurement variability for Cobb angles. Spine 23(5):551–555
Stephens GC, Yoo JU, Wilbur G (1996) Comparison of lumbar sagittal alignment produced by different operative positions. Spine (discussion 1807) 21(15):802–806
Tribus CB, Belanger TA, Zdeblick TA (1999) The effect of operative position and short-segment fusion on maintenance of sagittal alignment of the lumbar spine. Spine 24(1):58–61
Troyanovich SJ et al (1995) Intra- and interexaminer reliability of the chiropractic biophysics lateral lumbar radiographic mensuration procedure. J Manipulative Physiol Ther 18(8):519–524
Vaz G et al (2002) Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J (discussion 88) 11(1):80–87
Vedantam R et al (1998) Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine 23(2):211–215
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Le Huec, J., Basso, Y., Mathews, H. et al. The effect of single-level, total disc arthroplasty on sagittal balance parameters: a prospective study. Eur Spine J 14, 480–486 (2005). https://doi.org/10.1007/s00586-004-0843-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-004-0843-9