Abstract
Purpose
This study investigated the impact of dental prophylaxis on 5-fluorouracil (5-FU)–related oral mucositis (OM) according to the head and neck cancer (HNC) locations and treatment times.
Methods
A total of 13,969 HNC participants, including 482 5-FU–related OM subjects and 13,487 comparisons were enrolled from the Longitudinal Health Insurance Database for Catastrophic Illness Patients of Taiwan between 2000 and 2008. All subjects were stratified into subgroups based on the times to perform chlorhexidine use, scaling, and fluoride application before 5-FU administration. The dental prophylaxis related to 5-FU–related OM was estimated by multiple logistic regression and represented with odds ratio (OR) and 95% confidence interval (CI).
Results
Fluoride gel application and scaling significantly impacted on OM development (p < 0.001), and the joint effect of fluoride gel and scaling induced 5-FU–related OM (OR = 3.46, 95% CI = 2.39–5.01). The risk of OM was raised 2.25-fold as scaling within 3 weeks before 5-FU–related chemotherapy (95% CI = 1.81–2.81), and a 3.22-fold increased risk of OM while fluoride gel was applied during 5-FU–related treatment (95% CI = 1.46–7.13).
Conclusion
Dental prophylaxis significantly affected 5-FU–related OM in the HNC population. A short interval between dental scaling or fluoride application and 5-FU administration may be associated with higher prevalence of OM. Scaling simultaneously combined with chlorohexidine promoted 5-FU–related OM in specific HNC patients excluding the oral cancer and nasopharyngeal cancer population. Proper timing of the prophylactic dental treatments prior to 5-FU therapy could reduce the risk to develop 5-FU–related OM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
5-Fluorouracil (5-FU) is a common chemotherapy agent used in head and neck cancer (HNC) therapy, but it has several adverse effects such as oral mucositis (OM), diarrhea, dermatitis, myelosuppression, and cardiac toxicity. OM is one of the most common and troublesome among these complications [1]; patients with these painful lesions often have difficulty eating and swallowing, which leads to malnutrition and systemic infections [2]. Almost 40% of HNC patients suffer from OM while undergoing 5-FU therapy, and there is no effective treatment method; therefore, learning how to prevent 5-FU–related OM is a valuable issue for HNC patients that are undergoing chemotherapy.
Undergoing preventive dental prophylaxis before cancer therapy to eliminate oral infection pathogens can effectively maintain good oral health and reduce oral complications during cancer therapy. Many oncology centers routinely perform dental prophylaxis such as scaling, fluoride application, and chlorhexidine mouth rinsing for plaque control, caries prevention, and oral hygiene maintenance [3]. However, several authors have also mentioned the potential cytotoxicity of fluoride and chlorhexidine to oral tissues [4, 5]. Our previous study indicated that improper timing when performing dental scaling and chlorhexidine mouth rinse for dental prophylaxis raises the risk of osteoradionecrosis [6]. The impact of dental prophylaxis and risk of 5-FU–related OM is still a controversial issue; it is worthwhile to investigate whether dental prophylaxis can effectively prevent 5-FU–related OM. This study aims to determine the impact of different modalities and times to perform dental prophylaxis including scaling, chlorohexidine, or fluoride gel application on 5-FU–related OM in different HNC locations. The hypothesis of this study was that dental prophylactic modalities and times are both related to OM in the HNC population undergoing 5-FU chemotherapy.
Methods
Data source
Instituted in 1995, the National Health Insurance (NHI) system is a mandatory universal program that offers comprehensive medical care coverage to all Taiwanese residents. The NHI covered 96.2% of Taiwan’s population in 2000, and coverage was increased to over 99.5% by 2005 [7]. Therefore, the NHI Research Database (NHIRD) contains inclusive health care information of nearly 23.72 million residents in Taiwan. We used the longitudinal health insurance database of catastrophic illness patients (LHID-CIP) registry in this study, which is a part of the NHIRD. Thirty diseases were defined as catastrophic illness, such as ulcerative colitis, malignancies, end-stage renal disease, and autoimmune diseases (http://www.nhi.gov.tw/english/index.aspx). The related Diplomats must confirm the illness of the patient carefully based on the guidelines from the National Health Insurance Administration, Ministry of Health and Welfare (NHIAMHW) prior to registration in the Registry of Catastrophic Illness. Since patients with catastrophic illnesses can be exempt from copayment of medical care under the guidelines from NHIAMHW, we believe that every patient suffering from catastrophic illness was registered in the Registry of Catastrophic Illness. The LHID-CIP is composed of demographic data, all records of medical visits, prescriptions and treatments, and diagnoses of diseases for each patient in the period from 01 Jan 1997 to 31 Dec 2011. Diseases were identified according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Based on the Personal Information Protection Act, each patient’s identification was encoded before being transmitting to researchers. This human observational study was permitted by the Institutional Review Board of China Medical University and Hospital. We also conformed to the STROBE guidelines in this observational study.
Study subjects
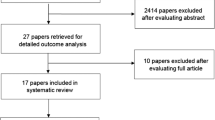
We organized this cross-sectional study to determine the association between dental prophylactic modalities (namely fluoride gel application, chlorhexidine mouth rinse, and scaling) and the risk of OM in HNC patients undergoing 5-FU–related treatment. During the period from 01 Jan 2000 to 31 Dec 2008, a total of 20,715 HNC (ICD-9-CM 140-149) patients with newly 5-FU–related chemotherapy were selected from the LHID-CIP registry, and the date of 5-FU therapy initiation was defined as the index date (Fig. 1). We further excluded patients from the study participants that were less than 20 years old (n = 58), who had been diagnosed with other cancers (ICD-9-CM 150–208) (n = 782), presented xerostomia (ICD-9-CM 527.2, 527.3, 527.5–527.7, 527.9, and 710.2) (n = 1002), had partial or total salivary excision before the index date (n = 0), and who had been diagnosed with a OM history within 1 year before the index date (n = 4904). In addition, these HNC patients were stratified into three subgroups according to their cancer locations: oral cancers (ICD-9-CM 140–145), nasopharyngeal cancer (NPC) (ICD-9-CM 147), and other cancers (ICD-9-CM 146, 148, and 149).
The end date was defined as the date of OM diagnosis, withdrawal from the NHI program, or the twenty-first day after the 5-FU therapy initiation date, whichever came first. Patients with OM diagnosis (ICD-9 CM 528.00, 528.01, 528.2, and 528.9) and undergoing OM therapy within the twenty-first day after the date of 5-FU therapy initiation were defined as the OM group.
The covariates included gender, age (in the age group of 20–34, 35–49, 50–64, and ≥ 65 years), comorbidity, dental treatment, and cancer treatment. The records of comorbidity were determined for each patient before the index date, which included diabetes mellitus (ICD-9-CM 250), hyperlipidemia (ICD-9-CM 272), hypertension (ICD-9-CM 401–405), and periodontitis (ICD-9-CM 523.3 and 523.4). The records of dental treatment were determined for each patient within 180 days prior to the index date, which included fluoride gel application, chlorhexidine mouth rinse, scaling, and major oral surgery. The major oral surgery comprised excision of lower jaw malignancy, mandible resection (viz. marginal, partial, and hemi-resection), mandibular osteotomy, open reduction of mandible or maxilla, maxilla suspension wiring or inter-maxillary wiring, and open reduction of palate fractures. Cancer treatment encompassed chemotherapy and radiotherapy.
Statistical analysis
The Chi-square test was used to examine the difference of gender, age group, comorbidity, dental treatment, and NHC locations between patients with and without OM, and the difference of mean age between these two groups was identified using Student’s t test. Fisher’s exact test was applied to inspect the difference between cancer treatments. The odds ratio (OR) and 95% confidence interval (CI) were determined by a multiple logistic regression model and were used to estimate the association between dental prophylactic modalities and the risk of OM. Gender, age, all comorbidities, and cancer treatments were adjusted in the multiple logistic regression model. Furthermore, we estimated the association between different timings of different oral prophylactic modalities and the risk of OM. All statistical analyses were executed using SAS software version 9.4 (SAS Institute, Cary, NC), and the level of statistical significance was set at a two-tailed test p < 0.05.
Results
A total of 13,969 HNC patients that received 5-FU–related chemotherapy were recruited, including 482 patients with OM development and 13,487 patients without OM development. There were no significant differences between the OM and non-OM groups in the distribution of gender and age. Patients with OM were more likely to have periodontitis (36.9% vs. 28.4%), and more likely to have undergone dental prophylactic modalities including fluoride gel application (10.2% vs. 4.6%) and scaling (53.3% vs. 36.0%). Patients with OM were more likely to have experienced NPC than patients without OM (57.7% vs. 45.4%) (Table 1).
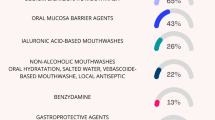
Compared to patients without dental prophylaxis, patients with fluoride gel application plus scaling were associated with the greatest risk of OM (OR = 3.46, 95% CI = 2.39–5.01), followed by only scaling (OR = 1.72, 95% CI = 1.36–2.16), and chlorhexidine mouth rinse plus scaling (OR = 1.53, 95% CI = 1.12–2.10) after adjustment for gender, age, comorbidities, and cancer treatments. More details are shown in Table 2.
After dividing these HNC subjects into three groups based on their cancer locations, NPC patients with fluoride gel application plus scaling (OR = 4.05, 95% CI = 2.61–6.31) and only scaling (OR = 1.62, 95% CI = 1.21–2.16) were associated with the greatest risk of OM when compared to those without dental prophylaxis. Additionally, other cancer patients with chlorhexidine mouth rinse plus scaling (OR = 2.33, 95% CI = 1.13–4.80) and only scaling (OR = 2.09, 95% CI = 1.18–3.69) were associated with a higher risk of OM (Table 3).
Table 4 presents the correlation between different scaling times and the risk of OM occurrence in HNC patients. After adjustment for gender, age, comorbidities, and cancer treatments, patients receiving scaling both within 3 weeks, and from 3 weeks to 6 months, before the index date had a higher risk of OM than those without scaling (OR = 2.25, 95% CI = 1.81–2.81; OR = 1.51, 95% CI = 1.19–1.92, respectively).
The relationship between different strategies of daily fluoride gel application and the risk of OM development in HNC patients is displayed in Table 5. Compared with the non-fluoride gel application group, patients with a fluoride gel application during and prior to 5-FU therapy were associated with a significant risk of OM (OR = 3.22, 95% CI = 1.46–7.13; OR = 1.90, 95% CI = 1.37–2.65, respectively) after being adjusted for gender, age, comorbidities, and cancer treatments.
Discussion
Preventing 5-FU–related OM through early risk factor detection is mandatory for better life quality in the HNC population. This study preliminarily elucidated the significant association between scaling, fluoride gel application, 5-FU–related OM (Table 1), and the closely related joint effect of prophylactic dental treatment to develop 5-FU–related OM among HNC patients (Table 2). Our results are coincident with previous research that proposed critical professional dental prevention measures to prevent chemoradiotherapy-induced complications in HNC patients [8,9,10].
This result demonstrated that periodontitis, cancer location, dental prophylactic treatment prior cancer therapy, radiotherapy, and chemotherapy all significantly raised the risk of 5-FU–related OM (p < 0.05) (Table 1). That was coincident to OM being an acute response derived from high-dose 5-FU administration and radiotherapy [11]. Previous investigations also indicated the host derived inflammatory responses in oral cavity, periodontitis, and radiation significantly impacted chemotherapy-induced OM [12]. Based on this study, 5-FU–related OM was a multifactorial complication as proven by the significant association between dental prophylaxis and 5-FU–related OM in the HNC population. To determine the impact of dental prophylaxis on the risk of developing 5-FU–related OM, all the confounders such as periodontitis, chemotherapy, and radiotherapy were adjusted in the statistics (Tables 2, 3, 4, 5).
Dental scaling is an effective approach in removal of plaque and calculus to decrease the risk of dental caries and periodontitis, which plays a major part of dental prophylaxis prior to cancer therapy. Previous investigations revealed that weekly scaling during chemotherapy period reduces the risk of OM in female breast cancer patients [13]. Nevertheless, this result indicated that prophylactic scaling significantly increased the risk of 5-FU–related OM among HNC patients after adjusting for several confounders including periodontitis (Table 2). The association between prophylactic dental scaling and OM seems a controversial issue. Many pieces of research indicate that the time to perform scaling is a crucial factor in the development of oral complications derived from cancer treatment [6, 7]. Several investigations advocated that a 3-week interval between invasive dental therapy and cancer treatment initiation are essential for socket healing [14, 15], we therefore used a 3-week interval as a cut-off point to determine the association between scaling time and the risk of 5-FU–related OM. This study divided the different dental scaling times as either 3 weeks or 6 months before 5-FU administration to investigate the various risks of 5-FU–related OM (Table 4). The results disclosed that the time of scaling was closely related to 5-FU–related OM after being adjusted for all other confounders (p < 0.001). The risk of OM was raised 2.25-fold among those who received dental scaling within 3 weeks compared to 6 months before 5-FU administration. The incidence of developing OM gradually decreases as the interval between dental scaling and 5-FU administration is prolonged. This result was coincident to a previous study that revealed that the intensive oral hygiene care is not clinically impressive because it is not necessary to prevent OM in patients receiving chemotherapy [16]. Based on this finding, we might infer the risk of 5-FU–related OM gradually decreases as the time interval between dental scaling and 5-FU administration increases. The study reaffirmed that the scaling time significantly affects the risk of developing oral complications derived from cancer therapy. Dental scaling should be conducted as early as possible before the 5-FU therapy is started.
Fluoride gel can effectively prevent dental caries in patients with HNC [17], so daily fluoride gel application is widely used as a part of standard prophylactic modalities. This is the first study to demonstrate that fluoride gel application could be associated with 5-FU–related OM (Table 1). Fluoride gel application during 5-FU administration raised the risk in developing OM by 3.22-fold (Table 5). This might be attributed to the issue that both fluoride and 5-FU induce the generation of reactive oxygen species as well as the activation of the nuclear factor-κB pathway [18]. The coupling pathologic mechanism related to OM development is worthy of being investigated further. A remarkable joint effect of scaling and fluoride gel application greatly raised the risk of experiencing 5-FU–related OM by 3.46-fold (Table 2). The result was coincident to a previous study that indicated fluoride can inhibit fibroblast spreading on human dentine, so the fluoride-containing solutions have to be prohibited during and after periodontal surgery and scaling [19]. Clinicians should be vigilant about dental scaling and fluoride gel application, as concurrent use might greatly raise the incidence of 5-FU–related OM in the HNC population. This result was not only a major discovery but also led to another issue to explore the safe interval between fluoride application and dental scaling prior to 5-FU therapy to prevent OM.
These results (Table 1) and the previous investigation [20] both pointed out the malignancy itself was closely related to chemotherapy-induced OM and might attribute the severity of OM on the 5-FU–administered dose as the treatment dosages of 5-FU depend on the different cancer locations [21]. To further investigate the impact of cancer location, this study subdivided the HNC population into three subgroups including oral cancer, NPC, and other HNC (Table 3). Excluding the patients with oral cancer, dental scaling prior 5-FU administration within 6 months greatly raised the risk of OM from 1.62-fold to 2.09-fold. Hence, this result reiterated the previous statement mentioned in this research that the interval of dental scaling and 5-FU administration should be as long as possible. If NPC patients are treated with scaling and fluoride application simultaneously prior to 5-FU administrated, the risk in developing OM is raised 4.05-fold compared to those who never received any dental prophylaxis. The higher risk when compared with the other HNC patients might be attributed to the fact that the NPC population must be treated with higher 5-FU doses [22]. This finding also strengthened the synergic effect of fluoride and 5-FU as previously proposed.
A previous study indicated the oral hygiene and periodontitis were closely related to the incidence of OM [23]. Chlorhexidine is a topical antiseptic, and so is commonly used to prevent dental plaque accumulation in dental prophylactic treatments [24]. However, in 2020, the clinical practice guidelines of the Mucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) announced a warning against utilizing chlorohexidine mouthwash to prevent OM in patients receiving head and neck radiotherapy [25]. The heterogeneity of these previous investigations might be attributed to different cancer treatments including chemotherapy, radiotherapy, and chemoradiotherapy [26]. To increase the realism of the results, this study creatively explored the association between chlorohexidine and 5-FU–related OM after adjusting for all confounders including the chemotherapy, radiation, and chemoradiation therapy in the statistics. This result revealed chlorohexidine did not significantly reduce the incidence of 5-FU–related OM (P = 0.21) (Table 1), which was coincident to a previous investigation [26]. The pilot finding of this research indicated that the simultaneous use of dental scaling and chlorohexidine before chemotherapy significantly raises the risk in developing 5-FU–related OM, and this effect is especially evident in some specific HNC patients excluding the NPC and oral cancer population (Tables 2 and 3). We might infer the cytotoxicity of chlorohexidine related to 5-FU–related OM is correlated to the cancer location, so the pathologic mechanism is worth further investigation.
To ensure the OM was related to 5-FU administration, the definition of the 5-FU–related OM in this study was very rigorous. A total of 20,715 HNC patients that had undergone 5-FU–related chemotherapy were selected from the LHID-CIP registry, and the date of 5-FU therapy initiation was defined as the index date. Patients that had been diagnosed with an OM history within 1 year before the index date were excluded from this study. Hence, there were 4904 subjects that were excluded from this study so only 482 OM cases among the total of 13,969 5-FU-treated HNC patients were identified as 5-FU–related OM subjects (Fig. 1). The careful identification of 5-FU–related OM cases in this study lead to the lower incidence of HNC patients suffering from OM while undergoing 5-FU therapy when compared to the general consensus. Based on some ethical concerns, it is difficult to investigate whether some dental prophylaxis induces 5-FU–related OM in this prospective randomized controlled study. This research not only successfully overcame this difficulty but also provided a multiple pioneer consensus even if there are still some limitations regarding lifestyle information such as cigarette smoking, alcohol consumption, and betel nut chewing, which have been demonstrated to influence the process of OM [27], but these lifestyle choices could not be obtained from Taiwan’s LHID-CIP registry. Although the grading of OM, plaque index, probing depth, mode, and dosage of 5-FU were not revealed in the database, the study was adjusted for all confounders including periodontitis, chemotherapy, and radiotherapy to clearly aim at the impact of scaling, fluoride, and chlorohexidine on the risk of 5-FU–related OM in the HNC population. The cancer location can clearly represent the dosage of 5-FU administration to overcome this limitation. Moreover, the association between the mode of 5-FU administration, including bolus or slow infusion, and the different grading of OM is another interesting issue that requires further study. Further investigation is also needed to determine whether the variant dental prophylactic treatments affect the different grading 5-FU–related OM. The dental assessment prior to cancer therapy proposed in The Mucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) guidelines included: toothbrushing with a soft toothbrush, regular toothbrush replacement, flossing, and the use of bland rinses and moisturizers. The clinical evaluation of this oral care regimen is subjective because it usually depends on self-reporting by the patient [28, 29]. The personal prophylactic habits, including brushing, flossing, and rinsing with a bland rinse, were not revealed in the database, but the definition of dental prophylactic treatments in this study were identified as the ICD-9 code in the database to be objective and increase the realism of the results. In this study, the joint effect of those different dental prophylactic therapies was defined to perform scaling, fluoride, or chlorohexidine concurrently. Based on this preliminary finding, determining which time intervals between these treatments are safe to prevent 5-FU–related OM development is worthy of further discussion.
Conclusions
5-FU–related OM seems to be a multifactorial side effect in HNC treatments. To reduce risk of developing OM, dental scaling and fluoride application should be performed separately and accomplished as early as possible before 5-FU administration. Although chlorohexidine mouth rinse might not induce 5-FU–related OM, scaling combined chlorohexidine might significantly increase the risk in developing 5-FU–related OM in some specific HNC patients that excludes the oral cancer and NPC population. Optimal dental prophylactic treatments, including the proper time to perform dental scaling and fluoride application, could not only effectively eliminate oral infections but also reduce complications derived from cancer treatment.
Data availability
All data are shown in the article.
References
Longley DB, Harkin DP, Johnston PG (2003) 5-fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer 3(5):330–338
Nonzee NJ, Dandade NA, Patel U, Markossian T, Agulnik M, Argiris A, Patel JD, Kern RC, Munshi HG, Calhoun EA, Bennett CL (2008) Evaluating the supportive care costs of severe radiochemotherapy-induced mucositis and pharyngitis: results from a Northwestern University Costs of Cancer Program pilot study with head and neck and nonsmall cell lung cancer patients who received care at a county hospital, a Veterans Administration hospital, or a comprehensive cancer care center. Cancer 113(6):1446–1452
Joshi VK (2010) Dental treatment planning and management for the mouth cancer patient. Oral Oncol 46(6):475–479
Mariotti AJ, Rumpf DA (1999) Chlorhexidine-induced changes to human gingival fibroblast collagen and non-collagen protein production. J Periodontol 70(12):1443–1448
Wurtz T, Houari S, Mauro N, MacDougall M, Peters H, Berdal A (2008) Fluoride at non-toxic dose affects odontoblast gene expression in vitro. Toxicology 249(1):26–34
Chang CT, Liu SP, Muo CH, Tsai CH, Huang YF (2017) Dental prophylaxis and osteoradionecrosis: a population-based study. J Dent Res 96(5):531–538
Huang YF, Liu SP, Muo CH, Tsai CH, Chang CT (2020) The association between dental therapy timelines and osteoradionecrosis: a nationwide population-based cohort study. Clin Oral Investig 24(1):455–463
Qutob AF, Allen G, Gue S, Revesz T, Logan RM, Keefe D (2013) Implementation of a hospital oral care protocol and recording of oral mucositis in children receiving cancer treatment : a retrospective and a prospective study. Support Care Cancer 21(4):1113–1120
Epstein JB, Güneri P, Barasch A (2014) Appropriate and necessary oral care for people with cancer: guidance to obtain the right oral and dental care at the right time. Support Care Cancer 22(7):1981–1988
Morais MO, Martins AFL, de Jesus APG, de Sousa Neto SS, da Costa AWF, Pereira CH, Oton-Leite AF, de Freitas NMA, Leles CR, Mendonça EF (2020) A prospective study on oral adverse effects in head and neck cancer patients submitted to a preventive oral care protocol. Support Care Cancer 28(9):4263–4273
Sroussi HY, Epstein JB, Bensadoun RJ, Saunders DP, Lalla RV, Migliorati CA, Heaivilin N, Zumsteg ZS (2017) Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer medicine 6(12):2918–2931
Khaw A, Logan R, Keefe D, Bartold M (2014) Radiation-induced oral mucositis and periodontitis - proposal for an inter-relationship. Oral Dis 20(3):e7–e18
Saito H, Watanabe Y, Sato K, Ikawa H, Yoshida Y, Katakura A, Takayama S, Sato M (2014) Effects of professional oral health care on reducing the risk of chemotherapy-induced oral mucositis. Support Care Cancer 22(11):2935–2940
Epstein JB, Wong FL, Stevenson-Moore P (1987) Osteoradionecrosis: clinical experience and a proposal for classification. J Oral Maxillofac Surg 45(2):104–110
Marx RE, Johnson RP (1987) Studies in the radiobiology of osteoradionecrosis and their clinical significance. Oral surgery, oral medicine, and oral pathology 64(4):379–390
Borowski B, Benhamou E, Pico JL, Laplanche A, Margainaud JP, Hayat M (1994) Prevention of Oral mucositis in patients treated with high-dose chemotherapy and bone marrow transplantation: a randomised controlled trial comparing two protocols of dental care. Eur J Cancer B Oral Oncol 30b(2):93–97
Deng J, Jackson L, Epstein JB, Migliorati CA, Murphy BA (2015) Dental demineralization and caries in patients with head and neck cancer. Oral Oncol 51(9):824–831
Sonis S, Haddad R, Posner M, Watkins B, Fey E, Morgan TV, Mookanamparambil L, Ramoni M (2007) Gene expression changes in peripheral blood cells provide insight into the biological mechanisms associated with regimen-related toxicities in patients being treated for head and neck cancers. Oral Oncol 43(3):289–300
De Jong HP, Schakenraad JM, Busscher HJ (1988) Spreading of human fibroblasts on pretreated human root dentine. Journal de biologie buccale 16(1):31–34
Russi EG, Raber-Durlacher JE, Sonis ST (2014) Local and systemic pathogenesis and consequences of regimen-induced inflammatory responses in patients with head and neck cancer receiving chemoradiation. Mediat Inflamm 2014:518261
Gibson MK, Li Y, Murphy B, Hussain MH, DeConti RC, Ensley J, Forastiere AA (2005) Randomized phase III evaluation of cisplatin plus fluorouracil versus cisplatin plus paclitaxel in advanced head and neck cancer (E1395): an intergroup trial of the Eastern Cooperative Oncology Group. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology 23(15):3562–3567
Kua VF, Ismail F, Chee Ee Phua V, Aslan NM (2013) Carboplatin/5-fluorouracil as an alternative to cisplatin/5-fluorouracil for metastatic and recurrent head and neck squamous cell carcinoma and nasopharyngeal carcinoma. Asian Pacific Journal of Cancer Prevention: APJCP 14(2):1121–1126
Sonis ST (2004) Pathobiology of mucositis. Semin Oncol Nurs 20(1):11–15
McGaw WT, Belch A (1985) Oral complications of acute leukemia: prophylactic impact of a chlorhexidine mouth rinse regimen. Oral Surgery, Oral Medicine, and Oral Pathology 60(3):275–280
Elad S, Cheng KKF, Lalla RV, Yarom N, Hong C, Logan RM, Bowen J, Gibson R, Saunders DP, Zadik Y, Ariyawardana A, Correa ME, Ranna V, Bossi P (2020) MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 126(19):4423–4431
Cardona A, Balouch A, Abdul MM, Sedghizadeh PP, Enciso R (2017) Efficacy of chlorhexidine for the prevention and treatment of oral mucositis in cancer patients: a systematic review with meta-analyses. Journal of Oral Pathology & Medicine: Official Publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology 46(9):680–688
Raber-Durlacher JE, Elad S, Barasch A (2010) Oral mucositis. Oral Oncol 46(6):452–456
Elad S, Raber-Durlacher JE, Brennan MT, Saunders DP, Mank AP, Zadik Y, Quinn B, Epstein JB, Blijlevens NM, Waltimo T, Passweg JR, Correa ME, Dahllof G, Garming-Legert KU, Logan RM, Potting CM, Shapira MY, Soga Y, Stringer J, Stokman MA, Vokurka S, Wallhult E, Yarom N, Jensen SB (2015) Basic oral care for hematology-oncology patients and hematopoietic stem cell transplantation recipients: a position paper from the joint task force of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) and the European Society for Blood and Marrow Transplantation (EBMT). Support Care Cancer 23(1):223–236
Hong CHL, Gueiros LA, Fulton JS, Cheng KKF, Kandwal A, Galiti D, Fall-Dickson JM, Johansen J, Ameringer S, Kataoka T, Weikel D, Eilers J, Ranna V, Vaddi A, Lalla RV, Bossi P, Elad S (2019) Systematic review of basic oral care for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 27(10):3949–3967
Funding
This study is supported in part by the Ministry of Health and Welfare, Taiwan (MOHW109-TDU-B-212-114004), MOST Clinical Trial Consortium for Stroke (MOST 109-2321-B-039-002), China Medical University Hospital (DMR-108-103), Chang Gung Memorial Hospital CMRPG3J1801,CMRPG3H1671, CMRPG3G0301, CMRPG3I0151, and CMRPG3E1341), Taiwan, Far Eastern Memorial Hospital (FEMH-2019-C-039), and Tseng-Lien Lin Foundation, Taichung, Taiwan.
Author information
Authors and Affiliations
Contributions
Y.F. Huang contributed to conception, design, and data interpretation and drafted the manuscript; S.P. Liu contributed to data acquisition and analysis and drafted the manuscript; C.H. Muo contributed to data acquisition and analysis and drafted the manuscript; H.J. Chen contributed to data acquisition and drafted the manuscript; Y.F Liao and C.C. Chen contributed to data acquisition and drafted the manuscript; K.M. Chiu and C.H. Tsai contributed to data interpretation and critically revised the manuscript; H.H. Hong contributed to conception, design, and data interpretation and critically revised the manuscript; C.T. Chang, contributed to conception, design, data interpretation, and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, YF., Liu, SP., Muo, CH. et al. The impact of timing and modalities of dental prophylaxis on the risk of 5-fluorouracil–related oral mucositis in patients with head and neck cancer: a nationwide population-based cohort study. Support Care Cancer 29, 3163–3171 (2021). https://doi.org/10.1007/s00520-020-05825-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05825-y