Abstract
Purpose
This retrospective/prospective study was carried out to implement a standardized hospital oral care protocol and record the incidence of oral mucositis for inpatients with childhood cancer.
Methods
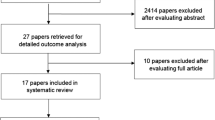
The implementation process included stages of collaboration, consultation, education, and evaluation. The retrospective part of the study documented the existing hospital oral care protocol and audited medical records of all pediatric patients diagnosed with cancer over a 12-month period. The frequency of recorded oral mucositis and the rate of referral to the pediatric dentistry department were assessed. Following evaluation of the retrospective study, the literature was searched to create a new hospital oral care protocol. Referral to the dental department was standardized and frequent in-service presentations were given to staff. The oral mucositis scale was recorded daily for all inpatients, and compliance rates were assessed.
Results
Fifty-nine patients’ medical records were audited during the retrospective study. Oral mucositis prevalence was clearly documented at 34%, while an additional 20% lacked a definitive diagnosis. During the prospective study, 38 patients were followed and had a verified incidence of oral mucositis of 33%. The rate of compliance of implementing the oral mucositis scale improved from 41% during the first 4 months to 87% during last 3 months. Referral rates to the dental department increased from 53% during the retrospective study to 100% during the prospective study.
Conclusions
Mutual understanding and collaboration between the oncology and dental departments in hospitals is crucial for standardizing patient care and for improving oral care standards.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The incidence of childhood cancers is reported to be increasing in Western Countries with one in 500–600 children developing childhood cancer prior to the age of 15 years [1]. Despite being rare, childhood cancer between the ages of 0 to 14 years is considered the second most common cause of death among Australian children, accounting for 17% of all child deaths [2]. Fortunately survival rates are increasing due to dose intensification and combination chemotherapy with improved supportive care [3, 4]. However, the increased survival rate comes at the cost of an increase in patient morbidity with 58% of pediatric patients’ pain being attributed to treatment complications such as oral mucositis [5, 6].
Oral mucositis is a common debilitating complication of cancer treatment, chemotherapy and radiotherapy [7]. It has an incidence of approximately 20–40% in adult patients undergoing standard dose chemotherapy regimens [8]. Oral mucositis does not occur in all patients receiving cancer treatment however, certain cancer treatments such as high dose chemotherapy regimens and head and neck radiotherapy are known to produce oral complications including oral mucositis [9]. This can lead to dosage reductions and delays of further cancer treatments. The incidence of oral mucositis among children has increased in comparison to the adult population; however, there are many variations in the literature with estimates ranging from 52% to 80% [10].
Oral mucositis is painful and can lead to an inability to swallow, eat or drink, and subsequently to hospitalization, therefore decreasing patients’ quality of life [11]. Hospitalization also poses economic constrains on the health care system in addition to its clinical implications [9]. At present, there is a scarcity in the literature investigating oral mucositis in children, despite their increased risk of developing this complication when compared to the adult population [7].
Prevention of oral mucositis in children by performing a standardized oral care protocol has been documented in the literature [5, 10, 12, 13]. However, establishing and implementing a new oral care protocol and a scale for the daily recording of the incidence of oral mucositis in a hospital environment can be challenging. This is due to the involvement of different health care workers including nurses, medical staff, dental staff, as well as patients and parents who all need to be compliant and motivated for the change. Implementing a new hospital policy can be very rewarding when embraced by patients, parents and staff. Few studies have documented the details of the process of successfully implementing a new hospital oral care protocol [14–16]. Other studies have documented the process of implementing other hospital policies in areas other than oral care [17–20]. A similar pattern was recognized in these processes which included interventions to raise knowledge, establish collaboration, improve communication, and continuously assess the ongoing progress of the new policy. Collectively these interventions were responsible for the success of implementing new hospital policy projects. Projects that were lacking some of these interventions, such as long term follow up and continuous assessment did not succeed in sustaining their policies for a long time [21].
This two-part study is aimed at documenting the existing hospital oral care protocol for children receiving cancer treatment, audit the recoding of oral mucositis, establish and implement a new standardized hospital oral care protocol, and to record oral mucositis for all inpatients at the oncology ward of the Women’s and Children’s Hospital in Adelaide, Australia.
Methods
The process of implementing the new hospital oral care protocol and the use of the oral mucositis scale for pediatric inpatients was performed in several stages at the Oncology Ward of the Women’s and Children’s Hospital in Adelaide, Australia. These stages included collaboration, consultation, education, and evaluation. These stages started during the retrospective study that provided data about the current status, followed by the prospective study that led to the final implementation of the new hospital policy.
Ethics approval was obtained from the Human Research Ethics Committee (HREC) of the Children, Youth and Women’s Health Services (approval No. REC2112/10/11), to carry out a retrospective medical case note audit for all pediatric patients diagnosed with cancer over the 12-month period from July 1, 2007 to June 30, 2008. The available medical and dental records were audited for the frequency of oral mucositis and the rate of referral to the department of pediatric dentistry. Dependent upon the date of diagnosis, each child had at least between three and five volumes of medical records containing between 12 and 24 months of oncology treatment details. During the retrospective audit, the frequency of oral mucositis was assessed and recorded based on what is written in the medical records. A diagnosis of oral mucositis was recorded in the retrospective study if the term “oral mucositis” or mucositis with reference to oral ulcerations was documented in the medical records by either the treating medical staff or nursing staff. All medical records were audited by the same individual to eliminate disagreement issues.
After discussion of the results of the retrospective study, ethics approval was also obtained for the prospective study from the Human Research Ethics Committee (approval No. REC2256/2/13). Consultants at the pediatric oncology and the pediatric dentistry departments have agreed to refer all pre-diagnosed and newly diagnosed oncology patients to the department of pediatric dentistry, to be screened by a trained and calibrated dentist from the research team. Comprehensive dental treatments were provided to all patients who needed them either before the commencement of cancer treatment or during the early stages of their treatment. These comprehensive dental treatments included restoration of carious restorable teeth and extraction of carious non-restorable or pulpally involved teeth either in the dental chair or under general anesthesia.
Several meetings were held between the authors and the head of the nursing staff of the oncology ward. These meetings were carried out to check the feasibility and the order of events of implementing the new hospital oral care protocol (Table 1) and the new scale to record oral mucositis (Fig. 1). In-service presentations were given at different intervals to the nursing and the medical staff at the oncology department. These presentations were aimed at familiarizing the staff with the new hospital oral care protocol and the oral mucositis scale, encouraging them to advocate for its implementation, and to answer any related questions or concerns.
The new hospital oral care protocol has incorporated the use of mechanical and microbial aspects of oral care as well as the use of re-mineralizing agents against dental decay. As explained in Table 1, the hospital oral care protocol consisted of tooth brushing with a fluoridated toothpaste and a soft toothbrush twice daily, rinsing or swabbing with an alcohol-free chlorhexidine mouthwash twice daily, and three monthly dental visits to the dental department for thorough oral examination and preventive management. The recommendation of using different concentrations of fluoridated toothpaste was based on children’s age according to the Australian guidelines on the use of fluoride agents [22]. The chlorhexidine mouthwash was aimed at reducing oral infections, preventing dental caries, and improving oral hygiene [23, 24]. The frequency of using the mouthwash was limited to twice daily, along with tooth brushing, to simplify its use and to encourage patients to comply with the oral care protocol. The three monthly periodic dental visits were based on the fact that pediatric oncology patients are considered high risk patients for developing dental diseases and hence the short intervals between the visits [25]. Oral mucositis-related pain was addressed partly by the new oral care protocol in the form of 2% lignocaine mouth rinse however; more potent pain relief medications were managed by the pain control team.
The new protocol was posted in patients’ rooms, the nursing station, and the nursing/doctors coffee room. A dentist from the research team also explained the oral care protocol during the initial dental visit and also by the nursing staff during the individual patient/parents educational sessions. Patients/parents were also reminded during their hospital stay in the morning and at night to brush and use the mouthwash. The oral care protocol was also emphasized by the dentist during the three monthly reviews.
Oral mucositis was recorded daily for all inpatients at the oncology ward by simultaneous use of the Children’s International Mucositis Evaluation Scale (ChIMES) [26] and the World Health Organization (WHO) oral mucositis scale [27] as shown in Fig. 1. The smiley faces of the ChIMES scale helped in recording the levels of pain and discomfort related to eating, swallowing and drinking. The WHO scale on the other hand, helped in recoding the presence and severity of oral mucositis. The compliance of daily recording of oral mucositis by the nursing staff at the oncology ward was assessed and modified at different stages to ensure a consistent and correct recording of the condition. A trained dentist from the research team was responsible for following up the compliance and the accuracy of daily recording of oral mucositis by auditing the medical records and by examining the patients. In the first phase of implementing the new oral mucositis scale (January–April 2010), the nursing staffs were asked to daily record the oral mucositis scale. No reminders or feedback were given to the nurses during this first phase. During the second phase of the implementation process (May–July 2010), a designated clinical administrator was responsible for posting the oral mucositis scale stickers in the medical records of all inpatients on a daily bases. Furthermore, recording of the oral mucositis scale was included in the nursing handover checklist avoid it being overlooked between shifts.
Results
The retrospective study
Medical records of 72 patients who started cancer treatment were audited during the retrospective study. These patients were diagnosed between July 2007and June 2008. The medical records of two patients were deemed missing as these patients were not admitted and did not have any outpatient appointments at the time of request. Additionally, not all children were receiving cancer treatment of known risk to produce oral complications. Eleven children were treated with surgery and/or radiotherapy to a localized area not involving the head and neck region. Therefore, the results of only 59 of the 72 children were considered during the retrospective study. These 59 patients were at known risk of developing oral mucositis as a result of their cancer treatment that included multi-agent, intensive chemotherapy with or without radiotherapy and/or bone marrow transplantation. The types and frequencies of the different cancer diagnoses, age, and gender distribution are shown in Table 2.
Prior to and during the retrospective study there were no standardized means of recording oral mucositis in the medical records of affected children. Thirty-four percent of the patients were documented to have at least one episode of oral mucositis while 20% were suspected of having oral mucositis as they had signs and symptoms documented in their medical records but no definitive diagnosis was made.
The existing hospital oral care protocol included the following:
-
(1)
Tooth brushing for as long as it can be tolerated but not during periods of neutropenia or thrombocytopenia
-
(2)
Chlorhexidine mouthwash four times daily
-
(3)
Antifungal medication:
-
Nystatin oral drops four times a day for children less than 6 months of age
-
Miconazole oral gel four times daily for children from 6 months to more than 5 years of age
-
Amphotericin lozenges four times daily for children over 5 years of age
-
There was no standardized referral system between the oncology and the dental departments during the retrospective study period. The rate of referral of children diagnosed with childhood cancer to the department of pediatric dentistry was reported at 53%. Only 15% of these patients were referred before the start of their cancer treatment. The rest were referred either during their cancer treatment or after the completion of treatment. About 52% of the referred patients required dental treatments beyond preventative measures.
The prospective study
Thirty-eight patients were followed up during the prospective study from January 2010 to July 2010. These 38 patients were known to be at risk of developing oral mucositis as a result of their cancer treatment that included multi-agent, intensive chemotherapy with or without radiotherapy and/or bone marrow transplantation. The types and frequencies of the different cancer diagnoses, age, and gender distribution are shown in Table 2. The incidence of oral mucositis was 33% of which 75% were scored as WHO grades 1–2 while 25% were scored as WHO grades 3–4. The intra-examiner reliability was regularly checked throughout the study period with kappa results of 0.87, i.e., almost perfect agreement. The accuracy of inter-examiner reliability among hospital staff recording the scale was not planned to be targeted during the implementation period and will be addressed at a later stage. Besides the accurate recording of oral mucositis, the daily recording of the oral mucositis scale has helped in identifying affected children at an early stage and hence suggesting early intervention to manage pain and discomfort during episodes of oral mucositis. However, this study did not intend to assess or compare pain and discomfort management strategies for children with oral mucositis
In the first phase of implementing the combined ChIMES/WHO oral mucositis scale during the period of January–April 2010, the rate of compliance of its daily recording for all oncology inpatients was 41%. This compliance rate has improved to 87% during the second phase of the prospective study from May to July 2010.
Since the start of implementing the new hospital oral care protocol; the protocol was fully adopted by all children diagnosed with childhood cancer. Patients, parents, oncology staff, and dental staff found the new protocol easy to follow; this has resulted in high compliance rates of 95–100% among inpatients and outpatients.
The rate of referral of children diagnosed with childhood cancer to the department of pediatric dentistry increased from 53% during the retrospective study to 100% during the prospective study. A standardized referral system has been established so that all newly diagnosed cases of childhood cancer are referred to the dental department for an initial assessment. These referrals are now organized through a data manager in the oncology department who receives information about all newly diagnosed cancer patients.
Discussion
The retrospective and the prospective study designs were appropriate to understand the dynamics of the project and to logically and empirically implement the planned changes. Both designs have contributed positively to the implementation of the new hospital oral care protocol, improved referral rates to the department of pediatric dentistry, and appropriate recording of the incidence of oral mucositis for the inpatient population.
Reporting the old hospital oral care protocol in the retrospective study highlighted the inconsistencies in oral care management among inpatients. Patients/parents were receiving mixed messages from nursing, medical and dental staff on the oral care protocol that they should follow. Maintaining good compliance with the old hospital oral care protocol was very difficult due to its frequent use of different agents. The new hospital oral care protocol was made easy to follow by reducing the number and frequency of the agents used. The chlorhexidine mouthwash was included as part of the preventative protocol to help maintain a good oral hygiene, to prevent oral/dental diseases, but not to prevent or treat oral mucositis [28, 29]. The frequency of use of the new non-alcohol containing chlorhexidine mouthwash was reduced from four daily applications to twice daily. The use of the non-alcohol containing mouthwash has helped in reducing the discomfort caused by alcohol containing preparations making the use of mouthwash more acceptable for children. The new protocol has also eliminated the frequent use of antifungal agents and made their use restricted to specific patients based on the recommendation from the treating medical staff. The mixed messages about the frequency of tooth brushing from nursing and medical staff on the one hand, and from the dental staff on the other hand, were standardized in the new protocol. Patients are now asked to brush their teeth twice daily throughout their cancer treatment, unlike the old protocol, which discouraged brushing during episodes of neutropenia and thrombocytopenia. Concerns about possible significant bacteremia due to tooth brushing during periods of neutropenia were not fully justified. When the prevalence of bacteremia due to tooth brushing was compared to other oral hygiene practices and dental treatments in a consensus document [30], it was reported to range between 0 and 26% which was lower than that of chewing (17–51%) and dental extractions (51–85%) [30]. Poor oral health and hygiene can significantly contribute to the risk of bacteremia. The odds ratios for having bacteremia from high dental plaque and calculus scores were reported at 3.78 and 4.43 (95% CI and P values of 0.008 and 0.004, respectively) [31]. Such poor oral health will render the gums inflamed and easy to bleed subjecting the patient to the risk of developing bacteremia after tooth brushing (OR=7.96 at 95% CI, and P value of 0.015) [31]. Therefore, keeping an optimal oral health and hygiene by tooth brushing and the use of antimicrobial mouthwash becomes paramount.
This high level of compliance with the new hospital oral care protocol was achieved by its easiness to follow by patients and parents and by standardizing the outgoing messages from the hospital staff (nursing, medical, and dental). The compliance rate was kept high by providing constant reminders to patients by the nursing staff at the oncology ward and by the dental staff during the three monthly reviews.
Raising the referral rate of children diagnosed with childhood cancer from 53% during the retrospective study to 100% during the prospective study was a great achievement. It came about by mutual understanding and agreement between the staff in the oncology and the dental departments. Families were also happy because they felt that their children are being looked after comprehensively in one institute rather than having to seek oral care outside the hospital. This has allowed the creation of a dental home and proper dental management for this group of patients based on the guidelines of managing pediatric patients undergoing cancer treatment [32]. The initial and follow-up dental visits were very helpful in maintaining a good oral hygiene, preventing dental diseases, and providing dental care as soon as problems arise. These visits also helped in motivating patients and parents to follow the new hospital oral care protocol thus minimizing the need for interventions and at the same time reducing the risk of developing oral mucositis.
It was a large change from not having any scale to record oral mucositis for inpatients during the retrospective study to using an established scale in the prospective study. In the retrospective study, the recording of oral mucositis was based on clear signs and symptoms and was mainly recorded for the severe grades of mucositis. Recoding the incidence of the different grades of oral mucositis among inpatients was standardized by the use of the combined ChIMES/WHO oral mucositis scale stickers. Incorporating the daily recoding of the oral mucositis scale, for all inpatients, into the daily activities of the nursing staff was a big challenge. Issues, related to familiarization and compliance of the nursing staff, were addressed by frequent in-service presentations and follow up sessions. Appointing a clinical administrator to post the oral mucositis scale stickers in the medical records and including the recording of the mucositis scale in nursing handover checklist helped in increasing the compliance rate from 41% in the first phase to 87% in second phase of the prospective study. This however, will need to be monitored at different time intervals to insure an ongoing maintenance of this new hospital policy.
Conclusion
Mutual understanding and collaboration between the oncology and the dental departments in a hospital is crucial for standardizing patient care. This collaboration has lead to the adoption of a better hospital oral care protocol that was easy to follow by patients and parents. Furthermore, nursing staff, medical staff, and dental staff were able to convey the same message in regards to oral care. Moreover, the wide adoption of the new hospital oral care protocol was beneficial in its preventative effect against oral mucositis and oral diseases including dental decay. Finally, the adoption of an established oral mucositis scale for daily use for inpatients has helped in accurate recording of the incidence of oral mucositis which in turn has helped in identifying affected children at an early stage and thus has improved pain and discomfort management during episodes of oral mucositis. The use of a standardized oral mucositis scale will also provide an opportunity to carry out future research that focuses on understanding, preventing, and treating oral mucositis in children.
References
Fadda G, Campus G, Luglie P (2006) Risk factors for oral mucositis in paediatric oncology patients receiving alkylant chemotherapy. BMC Oral Health 6:13
Australian Institute of Health and Welfare (AIHW) (2009) A picture of Australia’a children. [PHE 112]. Canberra
Wogelius P, Dahllof G, Gorst-Rasmussen A, Sorensen HT, Rosthoj S, Poulsen S (2008) A population-based observational study of dental caries among survivors of childhood cancer. Pediatr Blood Cancer 50:1221–1226
Cheng KK, Molassiotis A, Chang AM (2002) An oral care protocol intervention to prevent chemotherapy-induced oral mucositis in paediatric cancer patients: a pilot study. Eur J Oncol Nurs 6:66–73
Cheng KK, Molassiotis A, Chang AM, Wai WC, Cheung SS (2001) Evaluation of an oral care protocol intervention in the prevention of chemotherapy-induced oral mucositis in paediatric cancer patients. Eur J Cancer 37:2056–2063
Bonnaure-Mallet M, Bunetel L, Tricot-Doleux S, Guerin J, Bergeron C, LeGall E (1998) Oral complications during treatment of malignant diseases in childhood: effects of tooth brushing. Eur J Cancer 34:1588–1591
Tomlinson D, Judd P, Hendershot E, Maloney AM, Sung L (2007) Measurement of oral mucositis in children: a review of the literature. Support Care Cancer 15:1251–1258
Sung L, Tomlinson GA, Greenberg ML, Koren G, Judd P, Ota S, Feldman BM (2007) Validation of the oral mucositis assessment scale in pediatric cancer. Pediatr Blood Cancer 49:149–153
Sonis ST, Elting LS, Keefe D, Peterson DE, Schubert M, Hauer-Jensen M, Bekele BN, Raber-Durlacher J, Donnelly JP, Rubenstein EB (2004) Perspectives on cancer therapy-induced mucosal injury: pathogenesis, measurement, epidemiology, and consequences for patients. Cancer 100:1995–2025
Cheng KK, Chang AM, Yuen MP (2004) Prevention of oral mucositis in paediatric patients treated with chemotherapy; a randomised crossover trial comparing two protocols of oral care. Eur J Cancer 40:1208–1216
Tomlinson D, Judd P, Hendershot E, Maloney AM, Sung L (2008) Establishing literature-based items for an oral mucositis assessment tool in children. J Pediatr Oncol Nurs 25:139–147
Chen CF, Wang RH, Cheng SN, Chang YC (2004) Assessment of chemotherapy-induced oral complications in children with cancer. J Pediatr Oncol Nurs 21:33–39
Levy-Polack MP, Sebelli P, Polack NL (1998) Incidence of oral complications and application of a preventive protocol in children with acute leukemia. Spec Care Dentist 18:189–193
Bhatt V, Vendrell N, Nau K, Crumb D, Roy V (2010) Implementation of a standardized protocol for prevention and management of oral mucositis in patients undergoing hematopoietic cell transplantation. J Oncol Pharm Pract 16:195–204
Hogan R (2009) Implementation of an oral care protocol and its effects on oral mucositis. J Pediatr Oncol Nurs 26:125–135
Yeager KA, Webster J, Crain M, Kasow J, McGuire DB (2000) Implementation of an oral care standard for leukemia and transplantation patients. Cancer Nurs 23:40–47
Buyle F, Vogelaers D, Peleman R, Van MG, Robays H (2010) Implementation of guidelines for sequential therapy with fluoroquinolones in a Belgian hospital. Pharm World Sci 32:404–410
Davis ED, Harwood K, Midgett L, Mabrey M, Lien LF (2005) Implementation of a new intravenous insulin method on intermediate-care units in hospitalized patients. Diabetes Educ 31(818–21):823
Goldberg PA, Siegel MD, Sherwin RS, Halickman JI, Lee M, Bailey VA, Lee SL, Dziura JD, Inzucchi SE (2004) Implementation of a safe and effective insulin infusion protocol in a medical intensive care unit. Diabetes Care 27:461–467
McCarthy MJ, Byrne G, Silverman SH (1998) The setting up and implementation of a venous thromboembolism prophylaxis policy in clinical hospital practice. J Eval Clin Pract 4:113–117
van Niekerk, A.C., Venter, D.J., & Boschmans, S.A. (2012) Implementation of intravenous to oral antibiotic switch therapy guidelines in the general medical wards of a tertiary-level hospital in South Africa. J Antimicrob. Chemother 67, 756–762
(2006) The use of fluorides in Australia: guidelines. Aust. Dent. J 51, 195–199
Anderson MH (2003) A review of the efficacy of chlorhexidine on dental caries and the caries infection. J Calif Dent Assoc 31:211–214
Houston S, Hougland P, Anderson JJ, LaRocco M, Kennedy V, Gentry LO (2002) Effectiveness of 0.12% chlorhexidine gluconate oral rinse in reducing prevalence of nosocomial pneumonia in patients undergoing heart surgery. Am J Crit Care 11:567–570
Jenson L, Budenz AW, Featherstone JD, Ramos-Gomez FJ, Spolsky VW, Young DA (2007) Clinical protocols for caries management by risk assessment. J Calif Dent Assoc 35:714–723
Tomlinson D, Gibson F, Treister N, Baggott C, Judd P, Hendershot E, Maloney AM, Doyle J, Feldman B, Sung L (2009) Designing an oral mucositis assessment instrument for use in children: generating items using a nominal group technique. Support Care Cancer 17:555–562
World Health Organization (WHO) (1979) Handbook for reporting results of cancer treatment. WHO, Geneva
Schaeken MJ, De Jong MH, Franken HC, van der Hoeven JS (1984) Effect of chlorhexidine and iodine on the composition of the human dental plaque flora. Caries Res 18:401–407
Keefe DM, Schubert MM, Elting LS, Sonis ST, Epstein JB, Raber-Durlacher JE, Migliorati CA, McGuire DB, Hutchins RD, Peterson DE (2007) Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer 109:820–831
Gutierrez JL, Bagan JV, Bascones A, Llamas R, Llena J, Morales A, Noguerol B, Planells P, Prieto J, Salmeron JI (2006) Consensus document on the use of antibiotic prophylaxis in dental surgery and procedures. Med Oral Patol Oral Cir Bucal 11:E188–E205
Lockhart PB, Brennan MT, Thornhill M, Michalowicz BS, Noll J, Bahrani-Mougeot FK, Sasser HC (2009) Poor oral hygiene as a risk factor for infective endocarditis-related bacteremia. J Am Dent Assoc 140:1238–1244
American Academy of Pediatric Dentistry (AAPD) (2008) Guideline on dental management of pediatric patients receiving chemotherapy, hematopoietic cell transplantation, and/or radiation. American Academy of Pediatric Dentistry (AAPD)
Acknowledgments
The authors are greatly thankful to the oncology department’s nursing and medical staff for their support and patience during the implementation process. Special thanks to Kate Turpin from Brookman ward at the Women’s and Children’s Hospital for her great collaboration throughout the study period.
Conflict of interest
None declared by all authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qutob, A.F., Allen, G., Gue, S. et al. Implementation of a hospital oral care protocol and recording of oral mucositis in children receiving cancer treatment. Support Care Cancer 21, 1113–1120 (2013). https://doi.org/10.1007/s00520-012-1633-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-012-1633-2