Abstract
Purpose
Paclitaxel is associated with both an acute pain syndrome (P-APS) and chronic chemotherapy-induced peripheral neuropathy (CIPN). Given that extensive animal data suggest that minocycline may prevent chemotherapy-induced neurotoxicity, the purpose of this pilot study was to investigate the efficacy of minocycline for the prevention of CIPN and the P-APS.
Methods
Patients with breast cancer were enrolled prior to initiating neoadjuvant or adjuvant weekly paclitaxel for 12 weeks and were randomized to receive minocycline 200 mg on day 1 followed by 100 mg twice daily or a matching placebo. Patients completed (1) an acute pain syndrome questionnaire daily during chemotherapy to measure P-APS and (2) the EORTC QLQ-CIPN20 questionnaire at baseline, prior to each dose of paclitaxel, and monthly for 6 months post treatment, to measure CIPN.
Results
Forty-seven patients were randomized. There were no remarkable differences noted between the minocycline and placebo groups for the overall sensory neuropathy score of the EORTC QLQ-CIPN20 or its individual components, which evaluate tingling, numbness and shooting/burning pain in hands and feet. However, patients taking minocycline had a significant reduction in the daily average pain score attributed to P-APS (p = 0.02). Not only were no increased toxicities reported with minocycline, but there was a significant reduction in fatigue (p = 0.02).
Conclusions
Results of this pilot study do not support the use of minocycline to prevent CIPN, but suggest that it may reduce P-APS and decrease fatigue; further study of the impact of this agent on those endpoints may be warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paclitaxel is a chemotherapeutic agent widely employed against a variety of both early stage and advanced epithelial malignancies. One of the most frequent and troubling toxicities associated with its use is chemotherapy-induced peripheral neuropathy (CIPN), characterized by numbness, tingling, and shooting/burning pain, usually starting in the hands and feet. These symptoms may appear in the first several weeks of therapy and become more common and severe over time with continued exposure to the drug. While the symptoms of paclitaxel-induced CIPN tend to improve after paclitaxel is discontinued, in some patients, symptoms persist for years after completing chemotherapy. Paclitaxel is also associated with a syndrome of sub-acute aches and pain, often referred to as myalgias and arthalgias, which has been labeled as the paclitaxel-acute pain syndrome (P-APS). The pain often starts 1–2 days after the paclitaxel infusion, with the median duration of 4–5 days. The pain is usually located in the back, hips, shoulders, thighs, legs, and feet and, at times, radiates down the legs, arms, or back. Based on its clinical characteristics, as well as animal studies that demonstrated nerve injury within 24 h after receipt of a clinically appropriate dose of paclitaxel [1], it has been hypothesized that P-APS is a form of acute neurotoxicity and not due to effects of the drug on muscles or joints. To further support its neurotoxic mechanism, patients with severe P-APS tend to be at increased risk for developing chronic CIPN [2, 3].
Many agents have been studied for the prevention of CIPN, but, unfortunately, none have any proven benefit [4]. While there has been less investigation of agents for the prevention of P-APS, glutamine has been studied, with negative results [5]. More recently, a study was performed using pregabalin for the prevention of paclitaxel-associated neuropathy. This study included 46 patients who were randomly assigned to receive 75 mg of pregabalin or placebo twice daily while receiving weekly paclitaxel (80 mg/m2) for 12 weeks. The investigators found no substantial reduction in the development of symptoms of P-APS or chronic neuropathy with this agent [6]. Therefore, further investigation is needed to try to identify agents that may have efficacy for the prevention of P-APS and CIPN.
Minocycline is a second-generation tetracycline derivative, traditionally used as an antibiotic and an anti-inflammatory drug. It effectively crosses the blood-brain barrier and has been shown to have neuroprotective properties in experimental animal models of neurological injury and neurodegenerative disease [7, 8]. Minocycline has also been found to have possible benefit in human studies of acute stroke and spinal cord injury [9, 10]. This drug has been investigated for the prevention of neuropathic pain in multiple experimental animal models, including models of nerve injury, peripheral nerve inflammation, and diabetic neuropathic pain [11,12,13,14,15,16,17,18,19]. The proposed mechanism by which minocycline may reduce neuropathic pain is by inhibition of spinal microglia activation, reducing the production of pro-inflammatory cytokines, thereby lessening nerve injury [20]. In addition, it is proposed that administration of minocycline may decrease cytokine production and inflammation in the dorsal root ganglion (DRG). It may be that the analgesic effects of minocycline are related to inhibition of Na+ channels in primary afferent neurons [21].
Five studies using experimental animal models have investigated minocycline for the prevention of paclitaxel-induced neurotoxicity, each demonstrating positive results [22,23,24,25,26]. In one rat study, animals that were pretreated with minocycline had significantly attenuated paclitaxel-evoked allodynia at days 4 and 12, with a trend toward improvement as early as day 2. In addition, it appeared that minocycline inhibited the increase in the number of ATF3 (activating transcription factor 3)-positive cells in the DRG on days 4 and 12 [24]. In another study, rats treated with paclitaxel and minocycline were noted to have reduced levels of paclitaxel-induced mechanical hyperalgesia, measured as the mechanical withdrawal threshold to the application of von Frey filaments to the hind paws, compared to animals treated with paclitaxel alone. In addition, minocycline prevented paclitaxel-induced thermal hyperalgesia, measured as the withdrawal latency to radiant heat. Reductions in mechanical hyperalgesia and thermal hyperalgesia were noted as early as 1 day after treatment. It was proposed that the immunomodulatory effects of minocycline were primarily responsible for these changes [23]. An additional animal study involved administration of minocycline 72 h prior to the first injection of paclitaxel. It was noted that paclitaxel-induced the activation of spinal astrocytes, recognized by an increase in GFAP (glial fibrillary acidic protein) expression in the spinal dorsal horn, as early as 4 h after the first injection of paclitaxel. Systemic prophylaxis with minocycline prevented activation of astrocytes and downregulation of glial glutamate transporters in the spinal dorsal horn induced by paclitaxel. [26] Furthermore, since paclitaxel has clearly been shown to increase sensory neurons responses to TRPV1 (transient receptor potential vanilloid 1) by activation of toll-like receptor 4 (TLR4), minocycline-induced effects on pain signaling could result from suppression of TLR4 neuronal activation [27].
Based on these above noted data, the current study was developed to attempt to provide pilot data regarding the potential role of minocycline for the prevention of P-APS as well as paclitaxel-induced neuropathy, to support, hopefully, the conduct of a larger phase III placebo-controlled trial.
Methods
The current study was a multi-centric, randomized, double-blinded, pilot trial. Inclusion criteria included a diagnosis of breast cancer, age ≥18 years, ECOG performance 0 or 1, and life expectancy >6 months. All of the participants were scheduled to receive weekly paclitaxel at a dose of 80 mg/m2 in the adjuvant or neoadjuvant setting for a planned course of 12 weeks without any other concurrent cytotoxic chemotherapy; concurrent trastuzumab and/or other antibody and/or small molecule treatments, except for PARP (poly adenosine diphosphate ribose polymerase) inhibitors, was allowed. Participants needed to have the ability to complete questionnaires by themselves or with assistance and the ability to provide informed written consent. Exclusion criteria included pregnant or nursing women, previous diagnosis of diabetic or other peripheral neuropathy, fibromyalgia, prior exposure to neurotoxic chemotherapy or a history of allergic or other adverse reactions to tetracycline or minocycline.
Patients were randomized to either the placebo or minocycline arm. Patients on the active therapy arm received 200 mg of minocycline (two 100 mg capsules) on day one followed by 100 mg twice daily until the 12 weeks of chemotherapy were completed, while the control group received matching placebos. Treatment was stopped 1 week after the last planned paclitaxel dose. Patients were instructed to use 500 mg of acetaminophen every 6 h and/or 5 mg of oxycodone every 1–2 h as needed for breakthrough pain associated with the P-APS.
At the time of registration, patients had a history and physical examination and completed a pre-treatment 9-item questionnaire that addressed 1) the presence of symptoms related to baseline pain and 2) potential minocycline toxicities.
P-APS symptoms were measured by asking patients to keep a daily symptom log, comprising of 10 items regarding pain symptoms and the use of pain medications on days 2–7 following each paclitaxel dose. These items asked about aches and pain attributed to the paclitaxel treatments. A 15-question summary questionnaire regarding symptom quality, location, alleviating/aggravating factors, and medication use was administered on the eighth day following each paclitaxel dose (typically the day when the patient returned for her next dose of treatment). These instruments were those used to define this syndrome in previous publications [2, 3, 28]. CIPN was measured using the European Organization for Research and Treatment of Cancer Quality-of-Life (EORTC QLQ-CIPN20) questionnaire, which was completed at baseline, prior to each dose of paclitaxel and then monthly, following completion of paclitaxel treatment, for 6 months. The EORTC QLQ-CIPN20 is a 20-item self-report questionnaire that contains nine items assessing sensory function, eight items assessing motor function, and three items assessing autonomic function. Items are scored from 1 to 4 with 1 representing “not at all” and 4 representing “very much.” The EORTC QLQ-CIPN20 has been tested in cancer patients receiving a variety of chemotherapy agents and has been shown to be reliable, valid, and responsive to change. Cronbach’s alpha coefficients for the three subscales are 0.82, 0.73, and 0.76, respectively [29, 30]. Adverse events were monitored with the patient questionnaires, noted above, as well as with the physician-reported National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE) version 4.0.
The primary goals of this trial were to obtain pilot data regarding the possible effect of minocycline on the prevention of paclitaxel-induced CIPN and P-APS. An additional goal was to look at the potential toxicities of minocycline in this setting. To accomplish the goals of this trial, a variety of endpoints were utilized in an exploratory fashion. Pain scores and other continuous variables were converted to a 0–100 scale, where 100 = best possible quality of life. Area under the curve (AUC) for the entire course of treatment was calculated for worst, least, and average pain, as well as for the EORTC QLQ-CIPN20. Demographics, clinical data, and adverse events were summarized using descriptive statistics. Pain scores (maximum, average, and least), EORTC QLQ-CIPN20 scores, and AUCs between the two groups were compared using a Wilcoxon rank-sum test. Opioid and non-prescription drug use, adverse events, and other categorical variables were compared using chi-square or Fisher exact tests. Patients with missing data were excluded from analysis of associated endpoints.
Results
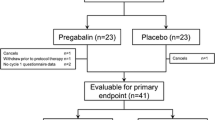
This study accrued 47 patients between 11/21/2014 and 7/21/2015, from 13 individual sites. Two patients canceled and were not evaluable for primary endpoint analyses. Baseline demographics were balanced among the remaining 45 patients (22 on the minocycline arm and 23 on the placebo arm). All patients were females with mean age of 54.9 (standard deviation of 10.9). Of these 45 patients, 2 patients did not complete their booklets at their baseline and 1 patient did not complete a booklet for the duration of the study.
Paclitaxel acute pain syndrome
There was a significant difference in the daily average AUC pain score attributed to P-APS, favoring minocycline (median 96.0 vs 84.3; p = 0.02), and also a trend toward improvement in the daily worst pain AUC score over the 12 cycles (median 94.9 vs 83.0, p = 0.06), although no difference was apparent during the first cycle (week) of treatment (Fig. 1). In addition, patients in the minocycline group reported that their P-APS aches and pains were less distressing compared to the placebo group (median 84.6 vs 68.9 p = 0.02; Fig. 2), and there was a trend toward less use of opioid pain medications for control of P-APS during cycle one (0 vs 23%, p = 0.05) and in other cycles (27.3 vs 52.2%, p = 0.09) (Fig. 3). One patient did not answer any of these pain questions at baseline, and one patient did not answer their average pain question at baseline. These patients were excluded from this analysis.
Chemotherapy-induced peripheral neurotoxicity
Despite the decrease in P-APS associated with minocycline use, there was no substantial difference in the overall EORTC QLQ-CIPN20 sensory subscale between minocycline and placebo (Fig. 4), nor any difference in reported tingling, numbness, or shooting/burning pain during treatment or for 6 months following treatment (Fig. 5). Three patients, for whom we either did not have baseline neuropathy scores (n = 1) or post-baseline scores (n = 2), are excluded from this analysis.
EORTC QLQ-CIPN20 selected individual item scores during treatment and over 6-month follow-up for tingling fingers/hands (a), tingling toes/feet (b), numbness fingers/hands (c), numbness of toes/feet (d), shooting burning pain of fingers/hands (e), and shooting burning pain of toe/feet (f). Higher scores represent fewer symptoms
Minocycline toxicity evaluation
Dizziness, fatigue, headache, skin discoloration, and tooth discoloration toxicities were evaluated, with no findings to suggest that minocycline increased any of these symptoms. In fact, patients who received minocycline reported significantly less fatigue (median AUC 76.7 vs 59.0, p = 0.02; Fig. 6).
Discussion
Data from the current study suggest, but do not prove, that minocycline decreases P-APS symptoms, as patients who received minocycline had lower daily average pain scores, reported less distress from aches and pains after paclitaxel, and tended to take less opioid medications. Symptoms of P-APS have been reported in up to 71% of patients being treated with paclitaxel at doses of 70 to 90 mg/m2 weekly and 88% of those receiving doses of at least 175 mg/m2 every 2 to 4 weeks [2, 3]. The discomfort associated with this syndrome can be distressing for patients and treatment with opioid medications has been reported for 12–20% of patients receiving weekly paclitaxel and up to 41% who received every 3 week paclitaxel [2, 3]. No agent has previously been shown to decrease this acute pain syndrome, although analgesics appear to alleviate it.
Given that this trial supports the possibility that minocycline might decrease this problem, it is reasonable to consider possible mechanisms for this effect. It may be related to the ability of minocycline to inhibit activation of microglia, reducing production of pro-inflammatory cytokines [20]. It may also be related to its ability to prevent the loss of intra-epidermal nerve fibers (IENFs) and interruption of macrophage responses [22, 24]. Finally, the protection against P-APS may be related to prevention of astrocyte activation and downregulation of glial glutamate transporters [26]. It is interesting to note that while there was no suggestion of a difference in P-APS symptoms in cycle 1, differences in symptoms become apparent with later cycles. Due to logistical reasons, minocycline in the current study was not given prior to the first day of chemotherapy. In contrast, in many of the animal studies, minocycline was given 24–72 h prior to the first dose paclitaxel [22, 24, 26]. The current data suggest that minocycline might be more effective against week 1 P-APS if started 1–3 days prior to the first dose of paclitaxel.
In contrast to the positive findings of the acute pain syndrome, the results of this trial do not support the conduct of a larger trial to test whether minocycline can reduce paclitaxel-induced peripheral neuropathy. As previous studies have demonstrated a potential relationship between the severity of P-APS symptoms and subsequent development of CIPN [2, 3], it is reasonable to consider why minocycline appears to prevent P-APS but not CIPN. The animal studies described above primarily investigated the ability of minocycline to reduce short-term nerve damage induced by paclitaxel. Perhaps those findings, like P-APS, are more related to acute nerve inflammation and injury, which can be attenuated by minocycline, while CIPN may be more a function of paclitaxel-induced microtubule dysfunction causing temporary, and sometimes permanent, damage to sensory neurons and their myelin sheaths, especially of the long axons extending to and from the patient’s distal extremities.
The findings of the current trial are consistent with a previous study of minocycline for the prevention of bortezomib-induced neurotoxicity, the preliminary results from which have been reported [31]. A phase II randomized placebo-controlled trial of minocycline vs. placebo, administered during induction therapy with bortezomib for multiple myeloma, was conducted at MD Anderson to assess its impact on the development of peripheral neuropathy. With about 40 evaluable patients, there was no evidence that minocycline reduced physician-judged neuropathy or improved fingertip touch perception. While numbness from baseline to week 10 was about half as prominent in patients receiving minocycline, this was not a statistically significant difference. Two other MD Anderson trials have been developed to assess the ability of minocycline to reduce neuropathy, including another trial in multiple myeloma, similar to the previous one but focusing on patients receiving maintenance therapy, which has completed accrual, and a trial in patients with colorectal cancer to determine whether minocycline can decrease neuropathy in patients receiving oxaliplatin.
An interesting finding from our study was the positive effect of minocycline on treatment-related fatigue. While the observed improvement in fatigue over the 12 weeks of treatment was a surprise to the study team, this is consistent with data from a study reported at ASCO 2016 which investigated minocycline for the prevention of symptoms in patients with non-small-cell lung cancer undergoing concurrent chemoradiation therapy [32]. In that trial, patients were randomized to receive minocycline (100 mg twice daily) or a placebo over the course of chemoradiation therapy. With 40 evaluable patients (19 minocycline, 21 placebo), AUCs for fatigue over 12 weeks were significantly lower in the minocycline group (odds ratio 0.65, p = 0.03). A fatigue-moderating effect of minocycline has also been observed in animal models. One study used a mouse model to discriminate between two components of cancer-related fatigue: loss of muscle mass and altered mood/motivation. Minocycline administration reduced depressive-like behavior and improved grip strength without altering muscle mass. It also reduced tumor-induced expression of IL-1 β (interleukin-1 beta), a marker of neuroinflammation [33]. Another study used a mouse model to explore the role of minocycline and licofelone for chronic fatigue stress. In this study, mice were put on a running wheel apparatus for 6-min test sessions daily for 21 days, which normally produces a fatigue-like condition. Pre-treatment with either licofelone or minocycline significantly attenuated fatigue-like behavior and oxidative damage, and restored mitochondrial enzyme complex activities; licofelone and minocycline used together seemed to potentiate their individual fatigue-protective effects [34].
It could be considered a weakness of our study that we enrolled only patients receiving weekly paclitaxel at 80 mg/m2, as opposed to those receiving doses of 175 mg/m2 or higher every 2–3 weeks, since patients receiving higher dose of paclitaxel are more likely to experience severe symptoms of P-APS [2, 3] and therefore might show greater benefit from a treatment that reduces this symptom. We also studied only patients being treated for breast cancer and enrolled only women. This design was chosen because the lower dose weekly schedule is the one most commonly employed in treating early stage breast cancer; a subsequent study could be designed specifically to assess the efficacy of minocycline at preventing or reducing P-APS and fatigue in patients receiving higher doses of paclitaxel and in other malignancies for which paclitaxel is commonly employed. Another potential weakness may be that the minocycline was not started in advance of the first dose of paclitaxel.
While the results of this study do not support conducting a large, phase III trial of minocycline for the prevention of CIPN, they do support further investigation of the effect of minocycline on P-APS and the potential utility of minocycline for decreasing chemotherapy-related fatigue.
References
Peters CM et al (2007) An evolving cellular pathology occurs in dorsal root ganglia, peripheral nerve and spinal cord following intravenous administration of paclitaxel in the rat. Brain Res 1168:46–59
Loprinzi CL et al (2011) Natural history of paclitaxel-associated acute pain syndrome: prospective cohort study NCCTG N08C1. J Clin Oncol 29(11):1472–1478
Reeves BN, Dakhil SR, Sloan JA, Wolf SL, Burger KN, Kamal A, Le-Lindqwister NA, Soori GS,Jaslowski AJ, Kelaghan J, Novotny PJ, Lachance DH, Loprinzi CL (2012) Further data supporting that paclitaxel-associated acute pain syndrome is associated with development of peripheral neuropathy: north central cancer treatment group trial N08C1. Cancer
Hershman DL et al (2014) Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 32(18):1941–1967
Jacobson SD et al (2003) Glutamine does not prevent paclitaxel-associated myalgias and arthralgias. J Support Oncol 1(4):274–278
Shinde SS et al (2016) Can pregabalin prevent paclitaxel-associated neuropathy?—an ACCRU pilot trial. Support Care Cancer 24(2):547–553
Plane JM et al (2010) Prospects for minocycline neuroprotection. Arch Neurol 67(12):1442–1448
Yong VW et al (2004) The promise of minocycline in neurology. Lancet Neurol 3(12):744–751
Casha S, Zygun D, McGowan D, Yong VW, Hurlbert JR (2009) Neuroprotection with minocycline after spinal cord injury: results of a double blind, randomized, controlled pilot study. Neurosurgery 65(2):410–411
Lampl Y et al (2007) Minocycline treatment in acute stroke: an open-label, evaluator-blinded study. Neurology 69(14):1404–1410
Cho IH et al (2006) Systemic administration of minocycline inhibits formalin-induced inflammatory pain in rat. Brain Res 1072(1):208–214
LeBlanc BW et al (2011) Minocycline injection in the ventral posterolateral thalamus reverses microglial reactivity and thermal hyperalgesia secondary to sciatic neuropathy. Neurosci Lett 498(2):138–142
Ledeboer A et al (2005) Minocycline attenuates mechanical allodynia and proinflammatory cytokine expression in rat models of pain facilitation. Pain 115(1–2):71–83
Marchand F et al (2009) Effects of etanercept and minocycline in a rat model of spinal cord injury. Eur J Pain 13(7):673–681
Mika J et al (2010) Minocycline reduces the injury-induced expression of prodynorphin and pronociceptin in the dorsal root ganglion in a rat model of neuropathic pain. Neuroscience 165(4):1420–1428
Pabreja K et al (2011) Minocycline attenuates the development of diabetic neuropathic pain: possible anti-inflammatory and anti-oxidant mechanisms. Eur J Pharmacol 661(1–3):15–21
Padi SS, Kulkarni SK (2008) Minocycline prevents the development of neuropathic pain, but not acute pain: possible anti-inflammatory and antioxidant mechanisms. Eur J Pharmacol 601(1–3):79–87
Raghavendra V, Tanga F, DeLeo JA (2003) Inhibition of microglial activation attenuates the development but not existing hypersensitivity in a rat model of neuropathy. J Pharmacol Exp Ther 306(2):624–630
Stirling DP et al (2004) Minocycline treatment reduces delayed oligodendrocyte death, attenuates axonal dieback, and improves functional outcome after spinal cord injury. J Neurosci 24(9):2182–2190
Mei XP et al (2011) Post-injury administration of minocycline: an effective treatment for nerve-injury induced neuropathic pain. Neurosci Res 70(3):305–312
Kim TH et al (2011) Effects of minocycline on Na+ currents in rat dorsal root ganglion neurons. Brain Res 1370:34–42
Boyette-Davis J et al (2011) Intraepidermal nerve fiber loss corresponds to the development of taxol-induced hyperalgesia and can be prevented by treatment with minocycline. Pain 152(2):308–313
Cata JP, Weng HR, Dougherty PM (2008) The effects of thalidomide and minocycline on taxol-induced hyperalgesia in rats. Brain Res 1229:100–110
Liu CC et al (2010) Prevention of paclitaxel-induced allodynia by minocycline: effect on loss of peripheral nerve fibers and infiltration of macrophages in rats. Mol Pain 6:76
Masocha W (2014) Paclitaxel-induced hyposensitivity to nociceptive chemical stimulation in mice can be prevented by treatment with minocycline. Sci Rep 4:6719
Zhang H, Yoon SY, Dougherty PM (2012) Evidence that spinal astrocytes but not microglia contribute to the pathogenesis of paclitaxel-induced painful neuropathy. J Pain
Li Y et al (2015) The cancer chemotherapeutic paclitaxel increases human and rodent sensory neuron responses to TRPV1 by activation of TLR4. J Neurosci 35(39):13487–13500
Loprinzi CL et al (2007) The paclitaxel acute pain syndrome: sensitization of nociceptors as the putative mechanism. Cancer J 13(6):399–403
Lavoie Smith EM et al (2013) Assessing patient-reported peripheral neuropathy: the reliability and validity of the European Organization for Research and Treatment of Cancer QLQ-CIPN20 Questionnaire. Qual Life Res 22(10):2787–2799
Postma TJ et al (2005) The development of an EORTC quality of life questionnaire to assess chemotherapy-induced peripheral neuropathy: the QLQ-CIPN20. Eur J Cancer 41(8):1135–1139
Thomas SK, Mendoza T, Dougherty PM, Williams L, Wang XS, Prasad S, Shah ND, Weber D, Wang M, Orlowski RZ, Giralt S, Cleeland C (2014) A phase 2 trial of minocycline versus placebo to prevent neuropathy in patients (pts) with multiple myeloma (MM). J Clin Oncol 32(15 Suppl):Abstract # e20669
Cleeland CS, Shi Q, Wang XS, Mendoza TR, Williams LA, Liao ZX (2016) Minocycline to reduce chemoradiation-related fatigue in patients with non-small cell lung cancer: A phase II randomized trial. J Clin Oncol 34(suppl; abstr 10017):2016
Norden DM et al (2015) Tumor growth increases neuroinflammation, fatigue and depressive-like behavior prior to alterations in muscle function. Brain Behav Immun 43:76–85
Kumar A et al (2012) Potential role of licofelone, minocycline and their combination against chronic fatigue stress induced behavioral, biochemical and mitochondrial alterations in mice. Pharmacol Rep 64(5):1105–1115
Acknowledgements
This trial was supported by the Breast Cancer Research Foundation and by the Altru Health Foundation and the University of North Dakota Athletics Department.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
An abstract, related to the data in this manuscript, was presented and published in 2016.
Rights and permissions
About this article
Cite this article
Pachman, D.R., Dockter, T., Zekan, P.J. et al. A pilot study of minocycline for the prevention of paclitaxel-associated neuropathy: ACCRU study RU221408I. Support Care Cancer 25, 3407–3416 (2017). https://doi.org/10.1007/s00520-017-3760-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3760-2