Abstract
Goals of work
Recently, 6 cycles of R-CHOP-14 have been recommended as the reference standard regimen for the treatment of elderly patients with diffuse large B-cell lymphoma (DLBCL). Pegfilgrastim has been shown to facilitate dose-dense chemotherapy schedules with a single administration per chemotherapy cycle. The aims of this study were to evaluate the use of pegfilgrastim in combination with the R-CHOP-14 regimen in a homogenous group of previously untreated elderly patients with DLBCL and to assess the pharmacokinetics of pegfilgrastim within this patient population.
Materials and methods
Ten patients with DLBCL between 60 and 80 years of age received a single subcutaneous injection of 6 mg pegfilgrastim 24 h after administration of R-CHOP chemoimmunotherapy, which was repeated for 6 to 8 cycles in two-weekly intervals. A total of 348 blood samples were collected. Pegfilgrastim plasma levels and absolute neutrophil counts were measured every other day during the first treatment cycle and twice weekly during all consecutive cycles.
Main results
Sixty-three of 72 cycles (87.5%) could be delivered on time and at the planned dose. Median absolute neutrophil nadir was 0.32 g/l on day 9. Grade 3/4 granulocytopenia occurred in all patients. Febrile neutropenia occurred in two patients. Plasma levels of pegfilgrastim remained elevated during the neutropenic phase. At the start of hematologic recovery, plasma concentrations of pegfilgrastim decreased rapidly to baseline levels. Median pegfilgrastim trough plasma level was 0.43 ng/ml on the day preceding the next application.
Conclusions
A single fixed dose of 6 mg of pegfilgrastim given once per cycle of R-CHOP-14 is effective in supporting neutrophil recovery to allow two-weekly drug administration in previously untreated elderly patients with DLBCL. However, close monitoring for infectious complications is mandatory in this patient population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its first description in 1976, the three-weekly CHOP-21 regimen (cyclophosphamide, doxorubicin, vincristine, and prednisone) has been the standard treatment of diffuse large B-cell lymphoma (DLBCL) for a quarter century [7, 18]. During the last few years, two distinct approaches have likewise led to a substantial improvement in the treatment of this disease. First, the addition of rituximab, a chimeric anti-CD20 monoclonal antibody, to the classical CHOP-21 regimen significantly improved results with regard to overall remission rates, progression-free survival, and overall survival in elderly as well as younger low-risk patients with DLBCL [6, 11, 23]. Secondly, by shortening the interval between CHOP cycles from 21 to 14 days with the use of granulocyte colony-stimulating factors (G-CSF), similar improvements have been achieved [21]. The recently presented interim results of a large randomized trial comparing 6 and 8 cycles of CHOP-14 each with or without rituximab showed a highly significant improvement with regard to time to treatment failure (p < 0.001) for the combined treatment groups [22].
To allow for timely application of the CHOP-14 regimen, patients treated within the mentioned studies received daily filgrastim from day 4 to day 13 of each two-week cycle. However, in all these studies, rituximab was not added to CHOP, and no information could be obtained on the CHOP-14 toxicity profile in the presence of the antibody. To date, only one retrospective analysis has been published on the feasibility and toxicity of the R-CHOP-14 in combination with daily filgrastim [12].
Within the last few years, several studies have demonstrated that pegfilgrastim, the pegylated form of filgrastim, stimulates granulocytopoiesis as efficiently as filgrastim and that a single fixed dose of 6 mg per cycle of pegfilgrastim is as safe and well tolerated as standard daily filgrastim administration in the management of chemotherapy-induced neutropenia [8, 9, 14, 17, 27].
Recently, an Italian group for the first time reported on the feasibility and toxicity of the R-CHOP-14 regimen with support of pegfilgrastim administered at the standard fixed dose of 6 mg per cycle in patients with DLBCL [4]. However, in this study, patients of all age groups were included, and no pharmacokinetic data of pegfilgrastim in use with the R-CHOP-14 regimen were provided.
In our trial, we have prospectively investigated the use of pegfilgrastim in a homogenous population of elderly patients with newly diagnosed, biopsy-proven DLBCL treated with the R-CHOP-14 regimen. Special focus has been given to pegfilgrastim plasma levels in relation to absolute neutrophil counts to allow for more detailed evaluation of pegfilgrastim pharmacokinetics within this group of patients.
Materials and methods
Patients
Patients were eligible for this prospective, oligocentric phase II study if they had previously untreated, biopsy-confirmed DLBCL according to the World Health Organization (WHO) classification and were between 60 and 80 years of age [13]. For the subgroup of the first ten consecutive patients, a detailed evaluation of pegfilgrastim plasma levels in relation to neutrophil counts was integrated as an accompanying pharmacological part of the protocol. This is a report on the completed analysis focusing on feasibility, toxicity, and pharmacokinetics of the R-CHOP-14 regimen supported by pegfilgrastim.
All disease stages (I–IV) according to Ann Arbor criteria and all International Prognostic Index scores were included [1]. Patients had to have a performance status of 0–2 according to the Eastern Cooperative Oncology Group scale. CD-20 expression of tumor cells must have been demonstrated by immunohistochemistry. All patients gave informed written consent. The study complied with all the provisions of the Declaration of Helsinki and was approved by the local ethics review committee. Patients were enrolled in three centers.
Patients with marked impairment of cardiac, pulmonary, hepatic, or renal function, bone marrow involvement with more than 25% lymphoma cells, initial white blood cell count (WBC) less than 2.5 × 109/l, initial platelet count less than 80 × 109/l, or inability to comply with study requirements were excluded.
All patients had mandatory baseline examinations that included clinical examination, laboratory tests, chest radiograph, computed tomography of chest and abdomen, and a bone marrow biopsy. Study enrollment started in June 2004.
Treatment
All patients initially received a “prephase” treatment consisting of a single intravenous (i.v.) injection of 1 mg vincristine on day −7 and 100 mg prednisone given orally for 7 days. The R-CHOP-14 regimen consisted of rituximab (375 mg/m2) on day 1, followed on day 2 by cyclophosphamide (750 mg/m2 intravenously), doxorubicin (50 mg/m2 intravenously), vincristine (2 mg intravenously), and prednisone (100 mg orally) given on days 2 to 6 for a total of 8 cycles. Pegfilgrastim (Neulasta®, Amgen, Thousand Oaks, CA, USA) was given on day 3, 24 h after CHOP chemotherapy, in a single subcutaneous dose of 6 mg. Darbepoetin alfa (Aranesp®, Amgen, Thousand Oaks, CA, USA) was started in patients with a hemoglobin value <11 g/dl at a dose of 300 μg subcutaneously every 2 weeks.
The next chemotherapy cycle was scheduled for day 15 after recovery of WBC (>2.5 × 109/l) and platelet count (>80 × 109/l). If recovery was not achieved, blood counts were repeated 3 days later and, if necessary, 7 days later. The dosages of cyclophosphamide and doxorubicin were reduced by 25% if WBC and platelet count recovery exceeded 1 week, or by 50% if the delay was longer than 2 weeks.
Patients with initial bulky disease (defined as lymphoma masses or conglomerates with a diameter >7.5 cm) received radiotherapy (36 Gy) to these areas irrespective of the result of chemotherapy. Radiotherapy was recommended at the same dose to extranodal sites of disease whenever feasible. Central nervous system prophylaxis was recommended only for patients with bone marrow involvement, testicular involvement, or lymph-node involvement in the cranial region and consisted of 15 mg methotrexate given intrathecally on days 1 and 5 of the first two chemotherapy cycles.
Pharmacokinetic data and toxicity
A complete blood count (cbc) was performed on days 1, 3, 5, 7, 9, 11, and 13 of the first therapy cycle and on days 1, 3, 7, and 11 of all consecutive cycles. Ten-milliliter EDTA samples for pharmacokinetic analysis of pegfilgrastim plasma levels were collected in parallel with blood samples for cbc during all treatment cycles. EDTA plasma tubes were immediately centrifuged at 3,000 rpm for 10 min; plasma was then separated and stored in a plain tube at −20°C. Pegfilgrastim plasma levels were measured at CellTrend GmbH Laboratory, Luckenwalde, Germany. Plasma samples were analyzed using standard curves constructed with pegfilgrastim by a commercially available G-CSF enzyme-linked immunosorbent assay (Quantikine, R&D Systems) that does not distinguish pegfilgrastim or filgrastim from endogenous G-CSF.
Adverse events reported by the patient or observed by the treating physician were coded on case report forms according to WHO grades. Incidence of febrile neutropenia, depth of neutrophil nadir, and time to neutrophil recovery [absolute neutrophil count (ANC) ≥2.0 × 109/l) were assessed, as was the requirement for i.v. antibiotic administration or hospitalization.
Relative dose intensity (RDI) of the CHOP-14 combination was calculated according to Hryniuk and Bush [15].
Statistical analysis
All statistical calculations were carried out using SPSS 11.0.1 software for Windows, Version 11.0.1©, SPSS, and Microsoft® Excel 2003.
Pharmacokinetic parameters were estimated using WinNonLin Version 4.01 (Pharsight, Pharsight, Mountain View, CA 94041-1530, USA) and standard noncompartmental methods. For calculation of the maximum observed plasma concentration (C max), time of C max (T max), terminal half-life (T1/2), area under the plasma concentration time curve from time zero to infinity \({\left( {AUC_{{{\left( {0 - \infty } \right)}}} } \right)},\) and apparent serum clearance after subcutaneous administration of dose (CL/F), pegfilgrastim plasma values from the first treatment cycle were used because of more closely timed collection of blood samples as specified in the protocol.
Results
Feasibility
Patients were enrolled between June 2004 and September 2005. Median age was 73.4 years (range 59–80). As a protocol violation, one patient was included at the age of 59 years. Seven patients were men.
Of the 72 cycles documented, 63 (87.5%) were delivered on time at the planned dose. Therapy was delayed on nine occasions (12.5%); 2 cycles (2.8%) were postponed because of delayed hematopoietic recovery, six (8.3%) because of nonhematologic toxicity, and 1 cycle (1.4%) was delayed on the patient’s request. The length of treatment delays was 1 week in 7 cycles. Postponement of treatment for 4 days and 3 weeks was necessary in another 2 cycles, respectively. In consideration of frequency and length of all treatment delays, the average RDI for all patients was 93.2% for all chemoimmunotherapeutic drugs. Of note, all treatment delays occurred in patients older than 70 years of age.
All patients completed the intended minimum of six planned treatment cycles. In four patients, the seventh and eighth treatment cycles were omitted due to achievement of a CR after the fourth cycle in three patients and due to toxicity concerns in one patient.
Toxicity
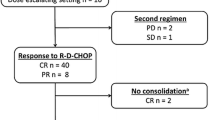
All 72 cycles were evaluable for toxicity. Incidences of severe hematologic and nonhematologic toxicities (WHO grade 3 or 4) are shown in Table 1. Grade 3 and grade 4 neutropenia occurred in 20 and 80% of patients, respectively. Figure 1 illustrates the median ANCs, with interquartile ranges, at given days over all cycles. The highest median ANC value was observed on day 4, while the nadir ANC was invariably observed on day 9 (7 days after CHOP application). The median time of recovery to ANCs >0.5 and >2.0 × 109/l was on days 10 and 11, respectively (8 and 9 days from the day of chemotherapy administration, respectively).
Median serum pegfilgrastim plasma levels (dotted line) and absolute neutrophil count (ANC) (solid line) after a single 6-mg pegfilgrastim injection 24 h after chemotherapy. Error bars show interquartile ranges. Solid lines show EC 50 and EC 20 concentrations of pegfilgrastim plasma levels (=pegfilgrastim concentration that produces half maximum and 20% stimulation of granulopoiesis, respectively)
Grade 3 and grade 4 thrombocytopenia occurred in one patient each. No bleeding complications occurred. Severe anemia requiring transfusion developed in five of ten patients. Darbepoetin alpha was administered to all patients by protocol.
Febrile neutropenia was defined as fever ≥38.2°C and an ANC <1.0 × 109/l. Based on analysis of the laboratory and body-temperature data, neutropenic fever developed on three occasions (4.2% of cycles) in two patients (20%), and the median duration of neutropenic fever was 1.5 days (range: 1–2 days).
Hospitalization for i.v. antibiotic administration was necessary in two patients. One patient was admitted due to severe diarrhea (WHO grade IV) requiring i.v. antibiotics and fluid replacement. In the other patient, Pneumocystis jiroveci pneumonia was diagnosed requiring i.v. antibiotic therapy with cotrimoxazole. Both patients had ANC >1.0 × 109/l at the time of admission.
Pegfilgrastim plasma levels
Median pegfilgrastim plasma levels were highest on the day after subcutaneous administration (day 4). Levels remained elevated throughout the neutropenic phase until neutrophil recovery; on the day of neutrophil nadir (day 9), pegfilgrastim levels were 10.62 ng/ml (Fig. 1). A rapid decline of pegfilgrastim levels was observed after neutrophil recovery with values falling below 2.0 ng/ml on day 13. On day 2 of the following cycle, i.e., on the day of the next CHOP application, pegfilgrastim plasma levels were down to baseline values with a median trough level of 0.43 ng/ml. No accumulation of the drug was observed in subsequent cycles. Terminal plasma half-time was 35.2 h. Detailed pharmacokinetic data are given in Table 2.
Discussion
This is a report on feasibility, toxicity, and pharmacokinetic data of once per cycle pegfilgrastim use in a homogenous cohort of elderly patients with previously untreated, biopsy-proven DLBCL treated with the R-CHOP-14 regimen.
Feasibility
The comparability of once per cycle pegfilgrastim and daily filgrastim has consistently been demonstrated in several randomized clinical trials. A first randomized trial was able to show that a single injection of pegfilgrastim 100 μg/kg per cycle was as safe and effective as daily injections of filgrastim 5 μg kg−1 day−1 in reducing neutropenia and its complications in patients with high-risk stage-II or stage-III/IV breast cancer, who received 4 cycles of doxorubicin and docetaxel chemotherapy in a three-weekly regimen [14]. In contrast to this weight-adopted dose and with the aim of further increasing the ease of dosing, another randomized trial confirmed in a similar patient population that a single fixed dose of 6 mg pegfilgrastim was comparable to multiple daily injections of filgrastim in supporting neutrophil recovery after myelosuppressive chemotherapy independent of patient weight [9]. In a pooled analysis of both trials, the incidence of febrile neutropenia, rates of hospitalization, and i.v. anti-infective use was lower with pegfilgrastim than with filgrastim [25].
Data from five small clinical trials have focused on the use of pegfilgrastim in patients treated for non-Hodgkin’s lymphoma (NHL). In a randomized phase-II study, a single weight-adjusted subcutaneous injection of pegfilgrastim (100 μg/kg) per chemotherapy cycle was compared with daily subcutaneous injections of filgrastim 5 μg/kg in 66 patients receiving salvage chemotherapy with the ESHAP regimen (etoposide, methylprednisolone, cisplatin, and cytarabine) for relapsed or refractory Hodgkin’s lymphoma or NHL [27]. The incidence of grade 4 neutropenia as well as the mean duration of grade 4 neutropenia was similar in both groups. The results for the two groups were also not significantly different for febrile neutropenia, neutrophil profile, time to neutrophil recovery, or toxicity profile. Another randomized phase-II trial compared two doses of single administration pegfilgrastim (60 and 100 μg/kg) with daily doses of filgrastim (5 μg kg−1 day−1) or no cytokine treatment after standard CHOP-21 in elderly NHL patients [10]. In an intent-to-treat analysis, the outcomes were similar in the pegfilgrastim (100 μg/kg) and filgrastim groups with respect to the duration of grade 4 neutropenia. Pegfilgrastim as hematopoietic support for the CHOP regimen—again without the addition of rituximab—has been evaluated in another small trial including 29 patients [8]. In this study, pharmacokinetic data were assessed and will be discussed below. Recently, the MD Anderson Cancer Center has published a small trial investigating a salvage regimen composed of paclitaxel and topotecan in relapsed aggressive NHL patients using pegfilgrastim support [24]. In fact, only one full paper has been published so far reporting on pegfilgrastim support for dose-dense R-CHOP-14 in DLBCL [4]. In this phase-II study, a single pegfilgrastim dose of 6 mg per cycle allowed on time delivery of therapy in 92% of cycles. In the experience of the authors, delays due to severe neutropenia occurred in a minimal percentage of cycles (3%) and affected a low fraction of patients.
The results of our trial compare very well with the reported data from the other mentioned trials on pegfilgrastim use in NHL patients. Of all 72 documented cycles, 63 (87.5%) were delivered on time at the planned full dose. Taking into account the length and frequency of all treatment delays, we were able to calculate an average RDI of 93.2% for all patients. These data are virtually identical with the trial of Brusamolino et al. [4]. However, it has to be considered that our patients were much older than in the Italian trial and thus more susceptible to increased toxicities. In fact, all toxicity-related treatment delays without exception occurred in the patients older than 70 years of age. In contrast, in the patients younger than 70 years of age, all cycles were given at the planned doses and intervals.
Toxicity
Concerning toxicity, the incidence of febrile neutropenia of 4.2% of cycles in our trial is similar as the reported rate of 4.0% of cycles in the Italian trial or the 3.7% of the retrospective study from the Memorial Sloan–Kettering Cancer Center evaluating the CHOP-14 regimen with adjunct filgrastim [4, 12]. Thus, both trials, as well as our own study, demonstrate that the addition of rituximab does not significantly modify the toxicity profile of dose-dense CHOP-14 supported by prophylactic G-CSF.
With regard to severe infections, the Italian trial reported on 6% of patients presenting with P. jiroveci pneumonia in the absence of routine cotrimoxazole prophylaxis (n = 50). Similarly, one of our ten patients also experienced microbiologically proven infection with P. jiroveci [4]. Therefore, we would follow the recommendation of routine cotrimoxazole prophylaxis made by the authors of this trial although other groups did not report on a higher incidence of this complication with the R-CHOP-14 regimen. However, these reports are yet available as abstracts only [22].
The aspect of age
It is well known from several trials that hematologic toxicity is increased in elderly patients (>65 years) and that age is an independent predictor of developing febrile neutropenia, leading to chemotherapy dose reductions or delays [5, 16, 20, 26]. As a consequence, the likelihood of receiving the full schedule of chemotherapy on time decreases with age. The clinical importance of this is demonstrated by the fact that reducing dose intensity either by reducing the dose or extending the interval between treatment cycles can compromise the efficacy of chemotherapy and thus negatively influence the outcome [19, 21].
It has to be kept in mind that the median age for DLBCL is 64 years, and thus a majority of all patients fall in the age group included in our trial [2]. Due to age restrictions in many treatment protocols, elderly patients are generally underrepresented in clinical trials. Of note, patients included in the trial of Brusamolino et al. [4] ranged from 22 to 70 years with a median age of 55 years. Only 32% of patients were older than 60 years. Therefore, our trial—although small in size—contributes to the evidence for the safe and efficient use of pegfilgrastim as adjunct to this well-established chemoimmunotherapy regimen in this particular patient population.
Pharmacokinetic data
By the addition of a 20-kDa linear polyethylene glycol molecule to the N-terminal methionine residue of the filgrastim molecule, the resulting pegylated molecule has approximately doubled its molecular weight (39 kDa) [3, 17]. The greater molecular size results in a reduced renal clearance of the drug; therefore, neutrophil-mediated clearance becomes the predominant route of elimination. This clearance is saturable and involves internalization and metabolism of the pegfilgrastim/G-CSF receptor complex within the neutrophil. Thus, elimination of the drug decreases when the ANC is low. This explains the characteristic pharmacokinetic profile of the drug, which has appropriately been described as “patient specific” and “self-regulating,” because drug elimination depends on each patient’s unique neutrophil recovery. As a result, serum levels of pegfilgrastim are maintained during the neutrophil nadir and rapidly decline at the onset of neutrophil recovery after myelosuppressive chemotherapy.
In our analysis, we could confirm this self-regulation process within the R-CHOP-14 regimen. Plasma concentrations reached a maximum of 24 h after pegfilgrastim application. On day 9, when the nadir of the ANC was reached, median plasma levels were 10.6 ng/ml, thereby still exceeding a concentration of 8 ng/ml, which has been defined as the pegfilgrastim concentration that produces half-maximum stimulation of granulopoiesis (=EC 50) [28, 29]. After day 9, a rapid decline parallels granulocyte recovery: pegfilgrastim levels in our study fell below 2 ng/ml on day 13. This threshold is considered as the lowest pegfilgrastim concentration being able to elicit meaningful granulopoiesis (=EC 20). Pegfilgrastim concentration reached baseline levels on the day before the next application (0.43 ng/ml). Median terminal plasma half-time in our series has been calculated as 35.2 h. This result is well in line with the reported 33–42 h in other series [3, 8, 17].
Summary
In conclusion, our results confirm that a single dose of pegfilgrastim per chemotherapy cycle allows dose-dense application of the R-CHOP-14 regimen in DLBCL, facilitating on time delivery of therapy in 87.5% of cycles and an RDI of 93.2%. Thus, our results confirm the supportive capacity of pegfilgrastim in the dose-dense R-CHOP-14 regimen in a homogenous elderly patient population at high risk for increased hematologic toxicity and infectious complications. In view of the two episodes of febrile neutropenia and two admissions for i.v. antibiotic therapy, close monitoring for infectious complications is mandatory. Plasma levels of pegfilgrastim remained high until the day of granulocyte recovery and decreased to baseline levels before the next application.
References
The International Non-Hodgkin’s Lymphoma Prognostic Factors Project (1993) A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med 329:987–994
The Non-Hodgkin’s Lymphoma Classification Project (1997) A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin’s lymphoma. Blood 89:3909–3918
Biganzoli L, Untch M, Skacel T, Pico JL (2004) Neulasta (pegfilgrastim): a once-per-cycle option for the management of chemotherapy-induced neutropenia. Semin Oncol 31:27–34
Brusamolino E, Rusconi C, Montalbetti L, Gargantini L, Uziel L, Pinotti G, Fava S, Rigacci L, Pagnucco G, Pascutto C, Morra E, Lazzarino M (2006) Dose-dense R-CHOP-14 supported by pegfilgrastim in patients with diffuse large B-cell lymphoma: a phase II study of feasibility and toxicity. Haematologica 91:496–502
Chrischilles E, Delgado DJ, Stolshek BS, Lawless G, Fridman M, Carter WB (2002) Impact of age and colony-stimulating factor use on hospital length of stay for febrile neutropenia in CHOP-treated non-Hodgkin’s lymphoma. Cancer Control 9:203–211
Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, Morel P, Van Den Neste E, Salles G, Gaulard P, Reyes F, Lederlin P, Gisselbrecht C (2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346:235–242
Fisher RI, Gaynor ER, Dahlberg S, Oken MM, Grogan TM, Mize EM, Glick JH, Coltman CA Jr, Miller TP (1993) Comparison of a standard regimen (CHOP) with three intensive chemotherapy regimens for advanced non-Hodgkin’s lymphoma. N Engl J Med 328:1002–1006
George S, Yunus F, Case D, Yang BB, Hackett J, Shogan JE, Meza LA, Neumann TA, Liang BC (2003) Fixed-dose pegfilgrastim is safe and allows neutrophil recovery in patients with non-Hodgkin’s lymphoma. Leuk Lymphoma 44:1691–1696
Green MD, Koelbl H, Baselga J, Galid A, Guillem V, Gascon P, Siena S, Lalisang RI, Samonigg H, Clemens MR, Zani V, Liang BC, Renwick J, Piccart MJ (2003) A randomized double-blind multicenter phase III study of fixed-dose single-administration pegfilgrastim versus daily filgrastim in patients receiving myelosuppressive chemotherapy. Ann Oncol 14:29–35
Grigg A, Solal-Celigny P, Hoskin P, Taylor K, McMillan A, Forstpointner R, Bacon P, Renwick J, Hiddemann W (2003) Open-label, randomized study of pegfilgrastim vs. daily filgrastim as an adjunct to chemotherapy in elderly patients with non-Hodgkin’s lymphoma. Leuk Lymphoma 44:1503–1508
Habermann TM, Weller EA, Morrison VA, Gascoyne RD, Cassileth PA, Cohn JB, Dakhil SR, Woda B, Fisher RI, Peterson BA, Horning SJ (2006) Rituximab-CHOP versus CHOP alone or with maintenance rituximab in older patients with diffuse large B-cell lymphoma. J Clin Oncol 24:3121–3127
Halaas JL, Moskowitz CH, Horwitz S, Portlock C, Noy A, Straus D, O’Connor OA, Yahalom J, Zelenetz AD (2005) R-CHOP-14 in patients with diffuse large B-cell lymphoma: feasibility and preliminary efficacy. Leuk Lymphoma 46:541–547
Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J, Lister TA, Bloomfield CD (1999) World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee meeting—Airlie House, Virginia, November 1997. J Clin Oncol 17:3835–3849
Holmes FA, O’Shaughnessy JA, Vukelja S, Jones SE, Shogan J, Savin M, Glaspy J, Moore M, Meza L, Wiznitzer I, Neumann TA, Hill LR, Liang BC (2002) Blinded, randomized, multicenter study to evaluate single administration pegfilgrastim once per cycle versus daily filgrastim as an adjunct to chemotherapy in patients with high-risk stage II or stage III/IV breast cancer. J Clin Oncol 20:727–731
Hryniuk W, Bush H (1984) The importance of dose intensity in chemotherapy of metastatic breast cancer. J Clin Oncol 2:1281–1288
Jacobson JO, Grossbard M, Shulman LN, Neuberg D (2000) CHOP chemotherapy with preemptive granulocyte colony-stimulating factor in elderly patients with aggressive non-Hodgkin’s lymphoma: a dose-intensity analysis. Clin Lymphoma 1:211–217; discussion 218
Johnston E, Crawford J, Blackwell S, Bjurstrom T, Lockbaum P, Roskos L, Yang BB, Gardner S, Miller-Messana MA, Shoemaker D, Garst J, Schwab G (2000) Randomized, dose-escalation study of SD/01 compared with daily filgrastim in patients receiving chemotherapy. J Clin Oncol 18:2522–2528
McKelvey EM, Gottlieb JA, Wilson HE, Haut A, Talley RW, Stephens R, Lane M, Gamble JF, Jones SE, Grozea PN, Gutterman J, Coltman C, Moon TE (1976) Hydroxyldaunomycin (Adriamycin) combination chemotherapy in malignant lymphoma. Cancer 38:1484–1493
Meyer RM, Browman GP, Samosh ML, Benger AM, Bryant-Lukosius D, Wilson WE, Frank GL, Leber BF, Sternbach MS, Foster GA et al (1995) Randomized phase II comparison of standard CHOP with weekly CHOP in elderly patients with non-Hodgkin’s lymphoma. J Clin Oncol 13:2386–2393
Morrison VA, Picozzi V, Scott S, Pohlman B, Dickman E, Lee M, Lawless G, Kerr R, Caggiano V, Delgado D, Fridman M, Ford J, Carter WB (2001) The impact of age on delivered dose intensity and hospitalizations for febrile neutropenia in patients with intermediate-grade non-Hodgkin’s lymphoma receiving initial CHOP chemotherapy: a risk factor analysis. Clin Lymphoma 2:47–56
Pfreundschuh M, Trumper L, Kloess M, Schmits R, Feller AC, Rube C, Rudolph C, Reiser M, Hossfeld DK, Eimermacher H, Hasenclever D, Schmitz N, Loeffler M (2004) Two-weekly or 3-weekly CHOP chemotherapy with or without etoposide for the treatment of elderly patients with aggressive lymphomas: results of the NHL-B2 trial of the DSHNHL. Blood 104:634–641
Pfreundschuh M, Kloess M, Schmits R, Zeynalova S, Lengfelder E, Franke A, Steinhauer H, Reiser M, Clemens M, Nickenig C, de Wit M, Hoffmann M, Mertelsmann R, Metzner B, Ho A, Truemper L, Eimermacher H, Mergenthaler H, Liersch R, Duehrsen U, Balleisen L, Hartmann F, Poeschel V, Schmitz N, Loeffler M (2005) Six, not eight cycles of bi-weekly CHOP with rituximab (R-CHOP-14) is the preferred treatment for elderly patients with diffuse large B-cell lymphoma (DLBCL): results of the RICOVER-60 trial of the German High-Grade non-Hodgkin Lymphoma Study Group (DSHNHL). Blood 106:13
Pfreundschuh M, Trumper L, Osterborg A, Pettengell R, Trneny M, Imrie K, Ma D, Gill D, Walewski J, Zinzani PL, Stahel R, Kvaloy S, Shpilberg O, Jaeger U, Hansen M, Lehtinen T, Lopez-Guillermo A, Corrado C, Scheliga A, Milpied N, Mendila M, Rashford M, Kuhnt E, Loeffler M (2006) CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large-B-cell lymphoma: a randomised controlled trial by the MabThera International Trial (MInT) Group. Lancet Oncol 7:379–391
Pro B, Fayad L, McLaughlin P, Romaguera J, Hagemeister FB, Rodriguez MA, Goy A, Loyer E, Younes A (2006) Pegfilgrastim administered in a single fixed dose is effective in inducing neutrophil count recovery after paclitaxel and topotecan chemotherapy in patients with relapsed aggressive non-Hodgkin’s lymphoma. Leuk Lymphoma 47:481–485
Siena S, Piccart MJ, Holmes FA, Glaspy J, Hackett J, Renwick JJ (2003) A combined analysis of two pivotal randomized trials of a single dose of pegfilgrastim per chemotherapy cycle and daily Filgrastim in patients with stage II–IV breast cancer. Oncol Rep 10:715–724
Vose JM, Armitage JO, Weisenburger DD, Bierman PJ, Sorensen S, Hutchins M, Moravec DF, Howe D, Dowling MD, Mailliard J et al (1988) The importance of age in survival of patients treated with chemotherapy for aggressive non-Hodgkin’s lymphoma. J Clin Oncol 6:1838–1844
Vose JM, Crump M, Lazarus H, Emmanouilides C, Schenkein D, Moore J, Frankel S, Flinn I, Lovelace W, Hackett J, Liang BC (2003) Randomized, multicenter, open-label study of pegfilgrastim compared with daily filgrastim after chemotherapy for lymphoma. J Clin Oncol 21:514–519
Yang BB, Hill R, Hollifield A, Green M, Holmes FA, Sheridan WP, Baynes RD (2003) Pegfilgrastim serum concentrations on the twelfth day after dosing are unlikely to stimulate granulopoiesis: a retrospective analysis of 6 clinical trials in a variety of cancer populations. Blood 102:1918
Yang BB, Lum P, Renwick J, Liang B, Neumann T, Nguyen S, Roskos L (2000) Pharmacokinetic rationale for a fixed-dose regimen of a sustained-duration form of filgrastim in cancer patients. Blood 96:157b
Acknowledgments
Our special thanks go to the employees of the hematology laboratory of the Department of Internal Medicine I, University of Bonn, Mrs. Lange, Mrs. Schenkel, and Mrs. Leufgens, for their exemplary assistance and support with regard to blood sample collection. Likewise, we also thank the employees of CellTrend GmbH, Luckenwalde, for their accurate and prompt work on pegfilgrastim plasma level measurements. Finally, we want to thank Dr. T. Sauerbruch, Bonn, and Stefanie Baumgartner, Zurich, Switzerland, for carefully reading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mey, U.J.M., Maier, A., Schmidt-Wolf, I.G.H. et al. Pegfilgrastim as hematopoietic support for dose-dense chemoimmunotherapy with R-CHOP-14 as first-line therapy in elderly patients with diffuse large B cell lymphoma. Support Care Cancer 15, 877–884 (2007). https://doi.org/10.1007/s00520-006-0201-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-006-0201-z