Abstract
Background
The advantages of laparoscopic appendectomy did not meet the same acceptance in the setting of perforated appendicitis as in uncomplicated appendicitis in the general surgical community. The aim of this study was to compare the clinical outcome of laparoscopic and open appendectomy in perforating appendicitis.
Methods
A randomized controlled study was conducted on 126 patients presenting with perforated appendicitis. Sixty patients were subjected to laparoscopic appendectomy (LA) and 66 patients underwent traditional open appendectomy (OA).
Results
65 (51.6%) patients were female, and 61 (48.4%) patients were male in whom the mean age was 37.6 + 8.5 years. A significant difference was calculated in the domains of postoperative pain, less need for analgesics, hospital stay, and return to daily activities. The mean operative time was shorter in OA 94 ± 10.4 min than LA 120.6 ± 17.7 min. No statistically significant difference between both groups was detected as regard occurrence of intra-abdominal collection.
Conclusion
In view of its clinical outcomes, laparoscopy should be considered in the context of perforated appendicitis. The possibility of intra-abdominal collection should not be a barrier against the widespread practice of this surgical procedure amidst laparoscopic surgeons if adequate precautions are employed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obstruction of the appendiceal lumen leads to rapid distension of the appendix because of its small luminal capacity and a dramatic rise of the intraluminal pressure [1]. Once the pressure exceeds 85 mmHg, thrombosis of the venules and impairment of lymphatic drainage occur, continued arteriolar inflow provokes vascular congestion, and engorgement of the appendix becomes more manifest. Mucosa becomes hypoxic and begins to ulcerate resulting in deficiency of the mucosal defenses, allowing invasion of the appendiceal wall by intraluminal bacteria [2].
If untreated, the inflamed appendix eventually perforates, especially if the condition is accompanied by appendiceal fecoliths, with periappendiceal abscess formation [2]. The rate of perforation in acute appendicitis has been estimated between 20 and 30% [3]. On clinical basis, a classic triad of pain, vomiting, and fever was demonstrated in one study in 76% of patients [4].
Perforated appendicitis (PA) is associated with increased morbidity rates and longer hospital stay. In the same time, open surgery has its inherent problems such as surgical site infection (SSI), wound dehiscence, and incisional hernia. Therefore, seeking a minimally invasive access is warranted given the well-documented benefits of laparoscopic surgery in uncomplicated appendicitis [5,6,7].
Despite the progress in laparoscopic equipment, intra-abdominal abscess (IAA) remains a common problem that general surgeons face after surgery for PA. A higher incidence of IAA formation was reported with laparoscopic appendectomy (LA), especially for PA, which prevented LA from being a standard procedure for PA [8, 9]. Intra-abdominal abscess prolongs hospital stay and increases readmission rate, in addition to the need for a subsequent drainage procedure and antibiotic treatment [8, 10, 11].
On literature review, most studies were retrospective thus liable to selection bias and included heterogenous groups of patients. We hypothesized that LA is superior to open appendectomy (OA) in patients with PA. The aim of this study was to compare the outcome of LA versus OA in patients with PA regarding operative time, morbidity, hospital stay, and time to resume normal activities.
Study design
This randomized controlled trial included patients with PA. This study was done at Alexandria Main University hospital and Medical Research Institute hospital, Petroleum hospital and Mabaret Alasafra hospitals, Alexandria, Egypt, in the period from January 2013 to April 2018. The study protocol was approved by the ethical committee of our institutions. All patients with evidence of appendicular perforation (severe right iliac fossa pain, tenderness, rebound tenderness, rigidity, fever, leukocytosis more than 15000/mm3 and turbid peri-appendicular collection by ultrasonography (US) or computed tomography (CT)) were included; this corresponds to grades III and IV laparoscopic grading system by Gomes et al. published in 2015 [12]. Patients with appendicular mass/well-defined abscess unfit for laparoscopic surgery and those who refused to participate were excluded. Informed consent was obtained from all participants and approved by the ethics committee of our institutions.
Sample size calculation
Using PASS program version 12 for sample size calculation, the minimum sample size required is 120 patients at 20% prevalence of PA and 0.07 error at 80% power and 5% level of significance.
Sampling technique and randomization
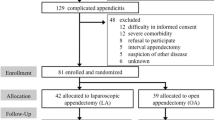
182 consecutive patients with PA were randomly selected; 42 patients were excluded, five did not receive allocated intervention because of equipment failure and nine lost to follow-up leaving finally, 126 patients to be eligible in our study (Fig. 1).
Patients with PA were randomly categorized into two groups using the closed envelope method:
-
1.
A study group who underwent laparoscopic appendectomy (LA, n = 60).
-
2.
A control group who underwent conventional open appendectomy (OA, n = 66).
Surgical technique
All included patients received a preoperative intravenous dose of two grams 3rd-generation cephalosporins (ceftriaxone) and metronidazole were given and continued for 3–5 days.
Laparoscopic appendectomy
LA was executed under the three-trocar protocol. After induction of low-pressure pneumoperitoneum at 10–12 mmHg by open Hasson method, a 10-mm umbilical port was used for the camera followed by a 5-mm port in the suprapubic area and finally a 10-mm trocar in left iliac fossa. Trendlenberg’s position with a slight tilt to the left was adopted. An initial evaluation of different abdominal quadrants was performed.
Pus was immediately aspirated to prevent bacterial dissemination and a sample sent for culture sensitivity. Monopolar diathermy was used for adhesiolysis and then to separate the mesoappendix with clipping of appendiceal artery. Three consecutive extracorporeal Roader knots were then applied on the base of appendix followed by scissor cutting of appendix. If the base was gangrenous, trimming of the gangrenous part or even partial caecal excision and suture repair was done. The infected specimen was retrieved from the left iliac fossa trocar enclosed in a prepared glove.
The right iliac fossa is repeatedly irrigated by warmed saline in the supine position that was then suctioned till it became clear. In localized periappendicular pus, one to two pelvic drains were inserted according to surgeon discretion. In diffuse peritonitis with pus dissemination all over the abdomen, four tube drains were left: two in the pelvis, one in Morison’s pouch, and one in the left subphrenic space emerging from the two port sites in the suprapubic and left iliac regions.
Open appendectomy
OA was performed via a lower midline or extended McBurney’s incision. The operation was performed by the standard technique with ligation/division of the mesoappendix including the appendicular artery followed by ligation/division of the appendix at its base. No purse string suture was used to invert the stump. Adhesions were cautiously divided. Suction irrigation of pus till it became clear and drain(s) was inserted through a separate stab incision the same as LA. Wound was closed primarily in layers. Absorbable sutures (polyglactin 2/0) for the peritoneum, non-absorbable (polypropylene 2/0) sutures for external oblique sheath. Skin was closed primarily with interrupted non-absorbable sutures.
Postoperative care and follow-up
Ketorolac ampoules were given intravenously on patient demand. Pain severity was assessed every 12 h in the first two postoperative days by the visual analogue score (VAS) from zero to ten (where zero represent no pain and ten represent the most severe pain), and the average number was used for analysis. The primary outcome was the postoperative complications. The secondary outcomes included the operative time, rate of conversion to open approach, resumption of oral intake, length of hospital stay, and return to normal daily activities.
Wound-related complications were reported when the wound showed redness, discharge (pus or blood) or dehiscence necessitating suture removal or frequent dressing. Infection was confirmed by positive culture results. Ileus was defined as progressive abdominal distension and sluggish peristalsis after 3 days from the operation. Intra-abdominal fluid collection demonstrated by US/CT accompanied by fever and ileus was considered IAA (Fig. 2) that were classified according to the Clavien–Dindo classification [13] as groups IIIa (CT-targeted drain) and IIIb (re-operation).
Patients were discharged on an oral antibiotic for a week and scheduled for follow-up at 1, 2, and 4 weeks after discharge from hospital and upon discovery of abnormal bulge at the site of wound(s).
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 20 software (SPSS, Inc., Chicago, IL, USA).
Qualitative data were described using number and percent. Categorical variables of both groups were expressed by number and percent and compared using the Chi square (X2) test. Quantitative values of both groups were expressed by mean and standard deviation (X ± 2SD) and compared using the independent t test after data exploration using Kolmogorov–Smirnov test. Z test was used to compare two proportions. All tests were done at 5% level of significance. Calculation of the risk estimates as relative risk (RR), absolute risk reduction (ARR), relative risk reduction (RRR), and number needed to treat (NNT) were done.
Results
This randomized controlled trial was conducted on 126 patients with perforated appendicitis (Fig. 1). The mean age was 37.6 ± 8.5 years ranging from 16 to 60 years. Sixty-five (51.6%) patients were females, and 61 (48.4%) patients were males. After randomization, 60 (47.6%) patients underwent LA while 66 (52.4%) patients were subjected to OA and served as controls. All operations were performed by the same surgical team. Both groups were comparable as regard demographic data, body mass index (BMI), and American society of anesthesiology (ASA) score (Table 1).
Operative data and postoperative outcomes are displayed in Table 2. A statistically significant difference in favor of laparoscopic approach was observed in the fields of postoperative pain, use of ketorolac, time of drain removal, hospital stay, return to normal daily activities, and wound-related complications. On the other hand, OA had a statistically significant shorter operative time.
In LA group, five patients (8.3%) were converted to OA. Causes of conversion included wide area of peri-appendicular caecal gangrene in two patients, a large ileal injury in another case and excessive bleeding occurred in two cases as there was extensive adhesions and during adhesiolysis, excessive bleeding occurred (around 1 l) from the mesentery and omentum with failed trials to control so, conversion was done to control bleeding upon the recommendation of our anesthetist. No intra-operative complications were noted in OA patients.
Regarding postoperative complications (Table 3), ileus and wound-related complications were found to be higher in OA while IAA and chest infection were higher in LA but statistically insignificant. Three cases of incisional hernia were encountered in the 2nd and 3rd postoperative months in OA. No mortality was recorded in either group.
Ten patients developed IAA (seven in LA and three in OA). Six abscesses were detected during the same hospital stay and four abscesses after patient discharge and were re-admitted. These collections were situated in the pelvis (n = 6) (Fig. 2), in the subhepatic space (n = 2) and in between bowel loops (n = 2). In all cases, broad spectrum antibiotic was started, and interventional radiology consulted for possible ultrasound-guided percutaneous aspiration that was performed in six cases when the abscess was larger than 5 cc. Intestinal leakage was not recorded in any of the patients.
Risk estimates (Table 4) revealed that OA increased the risk of some complications as ileus (1.8 times risk than those treated with LA). Also, the risk of wound infection and incisional hernia is increased in OA 2.7 and 9 times, respectively. Also, we needed to treat 8 patients with LA to prevent one patient from developing ileus after OA (NNT = 8). We needed to treat seven and 22 patients in OA to prevent one patient from developing wound infection and incisional hernia, respectively.
Discussion
There are traditional myths among general surgeon not to perform LA in patients with PA. Worries about the technical demand, high conversion rate, difficulty in managing the appendiceal stump and high rate if postoperative IAA led to preference of open approach in such cases [14]. To answer these queries, this study was conducted to evaluate the postoperative consequences of LA in patients with PA as compared to control group of OA through a prospective double-blinded randomized controlled trial.
In the literature, the term “complicated appendicitis” needs more clarification as different complications such as abscess, mass and peritonitis can ensue for which different management should be followed. All patients in the current study had perforated appendicitis resulting in localized or generalized peritonitis confirmed radiologically by US or CT.
It is unknown exactly when the first LA for PA in adults was performed. Wullstein et al. [15] in 2001 were the first to prove the feasibility of LA in complicated appendicitis and Towfigh et al. [16] published the first prospective study in 2006. The safety and feasibility of Laparoscopic appendectomy in PA were confirmed by many authors [11, 14, 17,18,19,20,21,22] and even recommended by some [15, 23] to be the standard approach in the background of PA.
In the present study, the operating time was statistically longer in the LA group. Adhesions to surrounding omentum and bowel form rapidly in a host defense to localize the inflammatory process caused by perforation. While dissection of these adhesions is straightforward in open surgery, a longer operative time in laparoscopy related to positioning of patient, narrow space, and the difficulty in proper instrument positioning to free these adhesions is required [11, 17]. A marked reduction in operative time was recorded between early and late cases after improvement in the learning curve, but still longer than the open approach. There is consensus that operative time is related to surgical skill and learning curve [11, 17, 22] accounting for different reports between authors in this aspect.
As our financial resources are limited, we successfully employed hand-made Roeder’s knots to ligate the appendicular stump. Perforation at the base was managed by trimming of the edges and direct closure with laparoscopic absorbable stitches. In two patients, the base and surrounding caecal wall were gangrenous, the operation was converted to OA and ileo-cecostomy was performed. In the beginning of this century, some authors [24, 25] recommended endoscopic staplers to minimize appendicular stump disruption that required 12-mm trocar and marked rise in operative costs. Katsuno et al. [19] employed commercial endoloops and used staplers selectively in difficult cases with perforation or inflammation at the base.
In contrast to the general belief that conversion depends on the surgeon experience, we think that intra-operative situations are the main reason to convert. Five patients (8.3%) were converted due to difficulties related to the disease state itself despite surgeons’ experience. The conversion rate in the literature ranges from zero to 47% [18, 19, 22,23,24,25,26,27,28]. Galli et al. [21] explored all suspected cases of PA laparoscopically according to hospital’s policy and selected easy cases only to be completed laparoscopically leading to high conversion rate.
Postoperative pain was assessed by VAS score and patient requirement of ketorolac sodium ampoules which are effective and cheap analgesic. Furthermore, to diminish shoulder pain from residual gas irritation, suction of CO2 from the right subphrenic space and low-pressure pneumoperitoneum [29] were executed in all cases in addition to minimal tissue handling and trauma, which also contributes to reducing pain sensation [28]. Our findings proved a significant advantage of LA in this issue. Similar findings were reported with opioid-combined analgesics as the oral opioid Pentazosine and diclofenac sodium suppositories by Fukami et al. [18], Pethidine IM with oral loxoprofen sodium used by Katsuno et al. [19] showing less analgesic requirement after LA.
Our data are consistent with published studies [4, 10, 11, 14, 17,18,19,20,21,22, 24, 26, 30, 31] emphasizing the perceived value of LA in wound related complications notably infections in favor of the protective endobag preventing contact between the infected appendix with the external wound. Extraction in prepared glove was as effective as endobag in decreasing SSI. Taguchi et al. [10] and Edwards et al. [32] showed that using a wound protection system in OA resulted in no difference in SSI between LA and OA in PA. The alternative is to leave wounds open for free drainage, thus reducing SSI. Low-cost endobags made from a surgical glove were used by some authors and offered the same advantages as the commercial endobags [26].
No statistical significance in the incidence of IAA was found between both groups. Certain operative considerations were taken in mind to lower the incidence of IAA: Firstly, low-pressure pneumoperitoneum limits bacterial translocations to blood stream [33, 34]. Secondly, suction of pus immediately at the start of procedure. Thirdly, complete adhesiolysis, to avoid missing pockets of pus. Fourthly, suction irrigation to wash out infected fluid till clear aspirate and finally adequate drainage by multiple drains. Some surgeons may disagree with multiple drains, but we found it useful in decreasing IAA. Asarias et al. [8] stated that IAA is fivefold more common with complicated appendicitis and considered increasing age as a predictive factor. Horvath et al. [17] blamed the use of Roeder knot, excessive irrigation and the Trendlenberg’s position for the higher incidence of IAA after LA in PA, while Gupta et al. [35] accused aggressive manipulation of infected appendix and excessive irrigation to increase infectious complications. In contrast, Piskun et al. [24] and Reid et al. [36] believed that IAAs have several determinants and their development is based on the magnitude of intra-abdominal inflammation rather than a specific technical issue during excision a perforated appendix.
Convenient amount of irrigation fluid was utilized in our cases, providing as little amount as necessary under direct vision then suctioned, and this maneuver was repeated till clear fluid was retrieved. Indeed, the significance of irrigation as a causative agent for IAA is controversial; Moore et al. [37] and Yau et al. [20] suggested that irrigation increases IAA. On the other hand, others [9, 10, 38] concluded that there is no difference between irrigation and suction alone in IAA formation.
Patients in LA were discharged from hospital 2 days earlier than their counter group. This finding agrees with most publications [11, 14, 16, 18,19,20,21, 23, 30, 39] and could be attributed to less infectious complications, which oblige patients to stay longer in hospital. In contrast most American/European groups would discharge patients sooner but prolongation of the hospital stays in the current study occurred in some cases due to complications such as ileus, chest infection, IAA, wound complications; although most of them could be managed on outpatient basis, it is related to cultural reasons, educational level of the patients and their relatives and medicolegal causes.
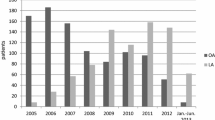
The study design conferred no selection bias as both groups were consistent regarding demographic data, a firm definition of PA and operations were done by the same surgical team in each hospital with high experience in laparoscopic surgery performing more than 20 LA per year.
Conclusion
LA is superior to OA in PA in terms of less wound-related complications, better pain score and less need for analgesics, shorter hospital stay, and earlier return to normal activities. Based on these findings, laparoscopy should be considered in the context of PA. The possibility of IAA should not be a barrier against the widespread practice of this surgical procedure amidst laparoscopic surgeons if adequate precautions are employed.
References
Teixeira PG, Demetriades D (2013) Appendicitis: changing perspectives. Adv Surg 47:119–140
Petroianu AVBT (2016) Pathophysiology of acute appendicitis. JSM Gastroenterol Hepatol 4(3):1062–1066
Hale DA, Molloy M, Pearl RH, Schutt DC, Jaques DP (1997) Appendectomy: a contemporary appraisal. Ann Surg 225(3):252–261
Khiria LS, Ardhnari R, Mohan N, Kumar P, Nambiar R (2011) Laparoscopic appendicectomy for complicated appendicitis: is it safe and justified?: a retrospective analysis. Surg Laparosc Endosc Percutan Tech 21(3):142–145
Katkhouda N, Mason RJ, Towfigh S, Gevorgyan A, Essani R (2005) Laparoscopic versus open appendectomy: a prospective randomized double-blind study. Ann Surg 242(3):439–448
Milewczyk M, Michalik M, Ciesielski M (2003) A prospective, randomized, unicenter study comparing laparoscopic and open treatments of acute appendicitis. Surg Endosc 17(7):1023–1028
Kehagias I, Karamanakos SN, Panagiotopoulos S, Panagopoulos K, Kalfarentzos F (2008) Laparoscopic versus open appendectomy: which way to go? World J Gastroenterol 14(31):4909–4914
Asarias JR, Schlussel AT, Cafasso DE, Carlson TL, Kasprenski MC, Washington EN et al (2011) Incidence of postoperative intraabdominal abscesses in open versus laparoscopic appendectomies. Surg Endosc 25(8):2678–2683
Yeom S, Kim MS, Park S, Son T, Jung YY, Lee SA et al (2014) Comparison of the outcomes of laparoscopic and open approaches in the treatment of periappendiceal abscess diagnosed by radiologic investigation. J Laparoendosc Adv Surg Tech A 24(11):762–769
Taguchi Y, Komatsu S, Sakamoto E, Norimizu S, Shingu Y, Hasegawa H (2016) Laparoscopic versus open surgery for complicated appendicitis in adults: a randomized controlled trial. Surg Endosc 30(5):1705–1712
Yu MC, Feng YJ, Wang W, Fan W, Cheng HT, Xu J (2017) Is laparoscopic appendectomy feasible for complicated appendicitis? a systematic review and meta-analysis. Int J Surg 40:187–197
Gomes CA, Sartelli M, Di Saverio S, Ansaloni L, Catena F, Coccolini F et al (2015) Acute appendicitis: proposal of a new comprehensive grading system based on clinical, imaging and laparoscopic findings. World J Emerg Surg 10:60
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Lin HF, Wu JM, Tseng LM, Chen KH, Huang SH, Lai IR (2006) Laparoscopic versus open appendectomy for perforated appendicitis. J Gastrointest Surg 10(6):906–910
Wullstein C, Barkhausen S, Gross E (2001) Results of laparoscopic vs. conventional appendectomy in complicated appendicitis. Dis Colon Rectum 44(11):1700–1705
Towfigh S, Chen F, Mason R, Katkhouda N, Chan L, Berne T (2006) Laparoscopic appendectomy significantly reduces length of stay for perforated appendicitis. Surg Endosc 20(3):495–499
Horvath P, Lange J, Bachmann R, Struller F, Konigsrainer A, Zdichavsky M (2017) Comparison of clinical outcome of laparoscopic versus open appendectomy for complicated appendicitis. Surg Endosc 31(1):199–205
Fukami Y, Hasegawa H, Sakamoto E, Komatsu S, Hiromatsu T (2007) Value of laparoscopic appendectomy in perforated appendicitis. World J Surg 31(1):93–97
Katsuno G, Nagakari K, Yoshikawa S, Sugiyama K, Fukunaga M (2009) Laparoscopic appendectomy for complicated appendicitis: a comparison with open appendectomy. World J Surg 33(2):208–214
Yau KK, Siu WT, Tang CN, Yang GP, Li MK (2007) Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg 205(1):60–65
Galli R, Banz V, Fenner H, Metzger J (2013) Laparoscopic approach in perforated appendicitis: increased incidence of surgical site infection? Surg Endosc 27(8):2928–2933
Lim SG, Ahn EJ, Kim SY, Chung IY, Park JM, Park SH et al (2011) A clinical comparison of laparoscopic versus open appendectomy for complicated appendicitis. J Korean Soc Coloproctol 27(6):293–297
Tiwari MM, Reynoso JF, Tsang AW, Oleynikov D (2011) Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg 254(6):927–932
Piskun G, Kozik D, Rajpal S, Shaftan G, Fogler R (2001) Comparison of laparoscopic, open, and converted appendectomy for perforated appendicitis. Surg Endosc 15(7):660–662
Stoltzing H, Thon K (2000) Perforated appendicitis: is laparoscopic operation advisable? Dig Surg 17(6):610–616
Kirshtein B, Bayme M, Domchik S, Mizrahi S, Lantsberg L (2007) Complicated appendicitis: laparoscopic or conventional surgery? World J Surg 31(4):744–749
Dimitriou I, Reckmann B, Nephuth O, Betzler M (2013) Single institution’s experience in laparoscopic appendectomy as a suitable therapy for complicated appendicitis. Langenbecks Arch Surg 398(1):147–152
Sauerland S, Jaschinski T, Neugebauer EA (2010) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 6(10):001546
Ge B, Zhao H, Chen Q, Jin W, Liu L, Huang Q (2014) A randomized comparison of gasless laparoscopic appendectomy and conventional laparoscopic appendectomy. World J Emerg Surg 9(1):3
Garg CP, Vaidya BB, Chengalath MM (2009) Efficacy of laparoscopy in complicated appendicitis. Int J Surg 7(3):250–252
Markides G, Subar D, Riyad K (2010) Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg 34(9):2026–2040
Edwards JP, Ho AL, Tee MC, Dixon E, Ball CG (2012) Wound protectors reduce surgical site infection: a meta-analysis of randomized controlled trials. Ann Surg 256(1):53–59
Evasovich MR, Clark TC, Horattas MC, Holda S, Treen L (1996) Does pneumoperitoneum during laparoscopy increase bacterial translocation? Surg Endosc 10(12):1176–1179
Gurtner GC, Robertson CS, Chung SC, Ling TK, Ip SM, Li AK (1995) Effect of carbon dioxide pneumoperitoneum on bacteraemia and endotoxaemia in an animal model of peritonitis. Br J Surg 82(6):844–848
Gupta R, Sample C, Bamehriz F, Birch DW (2006) Infectious complications following laparoscopic appendectomy. Can J Surg 49(6):397–400
Reid RI, Dobbs BR, Frizelle FA (1999) Risk factors for post-appendicectomy intra-abdominal abscess. Aust N Z J Surg 69(5):373–374
Moore CB, Smith RS, Herbertson R, Toevs C (2011) Does use of intraoperative irrigation with open or laparoscopic appendectomy reduce post-operative intra-abdominal abscess? Am Surg 77(1):78–80
St Peter SD, Adibe OO, Iqbal CW, Fike FB, Sharp SW, Juang D et al (2012) Irrigation versus suction alone during laparoscopic appendectomy for perforated appendicitis: a prospective randomized trial. Ann Surg 256(4):581–585
Tuggle KR, Ortega G, Bolorunduro OB, Oyetunji TA, Alexander R, Turner PL et al (2010) Laparoscopic versus open appendectomy in complicated appendicitis: a review of the NSQIP database. J Surg Res 163(2):225–228
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ahmed Talha, Hany El-Haddad, Abd-Elhamid Ghazal and Gihan Shehata have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Talha, A., El-Haddad, H., Ghazal, AE. et al. Laparoscopic versus open appendectomy for perforated appendicitis in adults: randomized clinical trial. Surg Endosc 34, 907–914 (2020). https://doi.org/10.1007/s00464-019-06847-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06847-2