Abstract
Purpose
Although laparoscopic appendectomy (LA) for acute appendicitis (AA) is widely performed, the value of LA for the treatment of complicated appendicitis (CA) is still controversially discussed.
Methods
In a retrospective study, we analyzed the clinical records of 404 patients who underwent LA or conversion (intention-to-treat group) or open appendectomy (OA) for AA or CA at the Alfried Krupp Hospital Essen-Rüttenscheid, Germany between January 2007 and December 2010.
Results
AA was treated in 64.2 % by LA and in 35.8 % by OA; the LA-to-OA conversion rate amounts to 3.7 %. CA was treated in 56 % by LA and in 44 % by OA. The LA-to-OA conversion rate here is 13.1 %, and compared to AA, it is significantly (P < 0.01) higher. Comparing LA with OA in both patient groups, we find no significant difference in the overall complication rate, the rate of postoperative intraabdominal abscesses and postoperative ileus. However, in both patient groups, the wound infection rate was significantly lower in patients who had undergone LA (AA P < 0.05 versus CA P < 0.01). In contrast to patients suffering from AA, patients with CA needed significantly less resurgery when treated by LA as compared to OA (P < 0.001). While the duration of surgery for the treatment of AA and CA was similar, the hospitalization time was significantly shorter with LA than with OA (AA P < 0.05 versus CA P < 0.001).
Conclusions
The data suggest that LA is advantageous not only in the treatment of AA, but also in the therapy of CA. Thus, LA may become a proper and safe routine method if performed by an experienced surgeon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute appendicitis is the most common cause of surgical abdomen and immediate surgical treatment is associated with a decreased morbidity and mortality [1]. The average current incidence of acute appendicitis is about 100 per 100,000 person-years in Europe, North America, and Australia [2, 3]. Clearly, lower incidences are observed in other countries like Thailand, New Guinea, and among the black population of South Africa [4–6]. The incidence of perforated appendicitis is about 20–30 per 100,000 person-years [7]. About 180,000 patients undergo an appendectomy in Germany every year [2]. The exact rate of laparoscopic appendectomies is unknown. For example, in 2006, for the first time, more than half of the appendectomies were performed laparoscopically in the state of Bavaria, Germany [8].
Complicated appendicitis is defined by perforation, abscess, or peritonitis [9]. Patients with a complicated appendicitis frequently show systemic signs of infection. While children and older patients show a significantly increased risk of perforation, women have a significantly lower rate of perforation in case of acute appendicitis [10]. Delay in diagnosis and surgical therapy can be regarded as the predominant cause of appendicular perforation [11]. The complication rate after appendectomy is mainly correlated with appendicular perforation as tenfold increases of the complication rate have been reported in the case of appendicular perforation [11, 12]. Even nowadays, people belonging to high-risk groups including very young patients, old patients, and patients with a suppressed immune system or patients with comorbidities die from acute and especially from complicated appendicitis [13].
Early surgical therapy is the only generally accepted concept in the treatment of acute appendicitis and can be performed by laparoscopic appendectomy (LA) or open appendectomy (OA) [14]. In a current meta-analysis with more than 5,000 patients, Sauerland et al. report significantly less wound infections, reduced postoperative pain, shorter hospitalization times, and earlier return to normal activity after LA as compared to OA [15]. However, in this study, laparoscopic surgery is associated with an increased incidence of intraabdominal abscesses and a longer duration of surgery [15]. Another meta-analysis by Aziz et al. including 6,477 children relates LA to OA in a pediatric population and also indicates significantly less wound infections, less postoperative ileus, and shorter hospitalization times after LA [16]. In the same study, no increased postoperative intraabdominal abscess rate or longer duration of surgery was reported after LA [16]. Regarding cost and hospitalization time, patients older than 65 years, patients with comorbidities, and those with complicated appendicitis appear to benefit the most from a laparoscopic approach [13]. Moreover, hospital mortality does not differ significantly between LA and OA in this study [13].
Although LA is known to be advantageous for the treatment of acute appendicitis, its value for the treatment of complicated appendicitis remains to be discussed controversially. Especially the reported rate of postoperative intraabdominal abscesses diverges widely in different studies comparing LA versus OA in complicated appendicitis [9, 17–24; Table 1]. Here, we retrospectively compare the clinical records of 404 patients that underwent LA or OA because of acute or complicated appendicitis. We analyze and discuss the suitability of both methods for the treatment of complicated appendicitis.
Methods
We retrospectively analyzed the clinical records of 404 patients who underwent LA or conversion (intention-to-treat group) or OA for acute appendicitis or complicated appendicitis at the Alfried Krupp Hospital Essen-Rüttenscheid, Germany, between January 2007 and December 2010. Every appendectomy (LA or OA) was treated by an attending surgeon or by a surgical resident in presence of an attending surgeon. The performed surgical procedure (LA or OA) depended on the laparoscopic experience of the surgeon or of the assisting attending surgeon. Laparoscopically experienced surgeons treated all patients irrespectively of the preoperative findings by LA while laparoscopically unexperienced surgeons always applied OA. LA was performed using Endo-GIAs for securing the appendicular stump and Endo-bags for extraction. Complicated appendicitis is defined by perforation, abscess, or peritonitis. For every patient from the complicated appendicitis group, the diagnosis was confirmed by histopathological findings. Here, we compare LA versus OA with respect to general parameters like age and gender as well as with respect to specific parameters like complications (i.e., wound infection rate, postoperative intraabdominal abscess rate, and postoperative ileus), necessity of resurgery, duration of surgery, hospitalization time, postoperative necessity of intensive care treatment, and mortality.
Data are expressed as percentages or mean ± SD. Box–whisker plots show minimum, 25th percentile, median, 75th percentile, and maximum. Differences between two groups are compared by the Student’s two-tailed t test. Discrete data are analyzed with the two-sided chi-square test. Statistical analysis is performed using the software SPSS 15.0 and differences were considered as significant at levels of P < 0.05.
Results
Age and gender in all patient groups
In the overall group, the average age was 34.9 ± 16.9 years. The average age of patients with acute appendicitis was 26.6 ± 9.2 years, which was significantly (P < 0.001) lower as the average age of patients with a complicated appendicitis (49.1 ± 18.4 years). Patients in the overall group (31.9 ± 13.1 years in LA/conversion versus 39.6 ± 20.8 years in OA, P < 0.001) and in the complicated appendicitis group (42.6 ± 14.2 years in LA/conversion versus 57.4 ± 19.8 years in OA, P < 0.001) who underwent LA/conversion were significantly younger than patients who underwent OA. In the acute appendicitis group, there was no significant difference between LA and OA with respect to the average patient age (26.6 ± 8.2 years in LA/conversion versus 26.3 ± 8.2 years in OA, not significant [n.s.]).
Altogether, there are significantly more male than female patients included in the study (188 women, 216 men, P < 0.01). The gender distribution in the acute appendicitis group was 114 women/140 men (P < 0.05) and 74 women/76 men in the complicated appendicitis group (n.s.). Within the overall group, 131 women and 116 men underwent LA/conversion while OA was performed with 57 women and 100 men. Regarding acute appendicitis, 92 women and 71 men were treated by LA/conversion, whereas 22 women and 69 men were treated by OA (P < 0.001). Thus, women with an acute appendicitis underwent LA/conversion significantly more often while OA was the predominant treatment in the male patient group. Finally, regarding complicated appendicitis, there was no significant difference in the gender distribution between LA/conversion (39 women/45 men) and OA (35 women/31 men).
Overall group
Acute appendicitis (254/404, 62.9 %) or complicated appendicitis (150/404, 37.1 %) was treated by LA/conversion in 247 (61.1 %) cases. The conversion rate in the overall group was 6.9 % (17/247, intention-to-treat group). One hundred fifty-seven (38.9 %) patients were treated by OA. In the overall group, 207 (207/404, 51.3 %) patients were treated by a surgical resident (in presence of an attending surgeon) and 197 (197/404, 48.7 %) patients were treated by an attending surgeon. Regarding the kind of surgery, there is no statistical difference with respect to the experience of the operating surgeon: for LA/conversion (surgical resident 116/247 [47.0 %] versus attending surgeon 131/247 [53.0 %], n.s.) compared to OA (surgical resident 91/157 [58.0 %] versus attending surgeon 66/157 [42.0 %], n.s.). The total complication rate was significantly lower for LA/conversion compared to OA (LA/conversion 22/247 [8.9 %] versus OA 28/157 [17.8 %], P < 0.01, Fig. 1a). There is no significant difference in the rate of postoperative intraabdominal abscesses (LA/conversion 6/247 [2.4 %] versus OA 4/157 [2.5 %], n.s., Fig. 1b) or in the postoperative ileus rate (LA/conversion 8/247 [3.2 %] versus OA 5/157 [3.2 %], n.s., Fig. 1d). The wound infection rate (LA/conversion 8/247 [3.2 %] versus OA 19/157 [12.1 %], P < 0.001, Fig. 1c) is significantly lower for patients treated by LA/conversion. Furthermore, there is no statistical difference regarding the necessity of resurgery (LA/conversion 7/247 [2.8 %] versus OA 9/157 [5.7 %], n.s., Fig. 2). Two patients (2/247 [0.8 %]) needed resurgery twice after LA. The duration of surgery (45.8 ± 16.3 min in LA/conversion versus 50.2 ± 22.1 min in OA, P < 0.05, Fig. 3a) and the hospitalization time (4.5 ± 1.5 days after LA/conversion versus 6.4 ± 4.5 days after OA, P < 0.001, Fig. 3b) were significantly shorter in LA/conversion. Differences in regard to intensive care treatment and mortality are described below.
a Overall complication rate, b postoperative intraabdominal abscess rate, c wound infection rate, and d postoperative ileus rate in the overall group and the acute and complicated appendicitis group for LA and OA (AA acute appendicitis, CA complicated appendicitis, LA laparoscopic appendectomy, OA open appendectomy, *P < 0.05, **P < 0.01, ***P < 0.001)
Acute appendicitis group
Acute appendicitis (n = 254) was treated by LA/conversion in 163 (64.2 %) cases. One hundred fifty-seven patients (61.8 %) underwent LA and six patients needed conversion (3.7 %, intention-to-treat group). Ninety-one (35.8 %) patients were treated by OA. One hundred thirty-nine (139/254, 54.7 %) patients were treated by a surgical resident (in presence of an attending surgeon) and 115 (115/254, 45.3 %) patients were treated by an attending surgeon. Regarding the kind of surgery in the acute appendicitis group, we find a slight bias with respect to the experience of the operating surgeon: while LA/conversion has been applied rather equally by the two mentioned categories of surgeons (surgical resident 78/163 [47.9 %] versus attending surgeon 85/163 [52.1 %], n.s.), OA seems to have been preferably applied by the surgical residents (surgical resident 61/91 [67.0 %] versus attending surgeon [33.0 %], P < 0.0001). Although this effect is formally statistically significant, we would like to qualify it by reminding the reader of the somewhat small sample size of the latter test of N = 91 patients. There is no significant difference in the total complication rate in this group (LA/conversion 9/163 [5.5 %] versus OA 10/91 [11.0 %], n.s., Fig. 1a). The rate of postoperative intraabdominal abscesses (LA/conversion 2/163 [1.2 %] versus OA 1/91 [1.1 %], n.s., Fig. 1b) and the rate of postoperative ileus (LA/conversion 2/163 [1.2 %] versus OA 1/91 [1.1 %], n.s., Fig. 1d) appear similar for LA and OA. The wound infection rate (LA/conversion 5/163 [3.1 %] versus OA 8/91 [8.8 %], P < 0.05, Fig. 1c) is found to be significantly lower for patients treated by LA/conversion. The necessity of resurgery in this group is rather low for both LA/conversion and OA (LA/conversion 2/163 [1.2 %] versus OA 2/91 [2.2 %], n.s., Fig. 2). In addition, we find a very similar duration of surgery for either method (43.1 ± 11.6 min in LA/conversion versus 44.9 ± 18.2 min in OA, P = 0.34, n.s., Fig. 3a). The hospitalization time was significantly shorter for LA/conversion (4.1 ± 1.4 days in LA/conversion versus 4.7 ± 2.4 days in OA, P < 0.05, Fig. 3b). Finally, no patient needed intensive care treatment and no case of death occurred in this group.
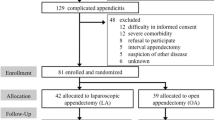
Complicated appendicitis group
Complicated appendicitis (n = 150) was treated by LA/conversion in 84 (56 %) cases. Seventy-three patients (48.7 %) underwent LA and 11 patients needed conversion (13.1 %, intention-to-treat group), whereas 66 (44 %) patients were treated by OA. Sixty-eight (68/150, 45.3 %) patients were treated by a surgical resident (in presence of an attending surgeon) and 82 (115/254, 54.7 %) patients were treated by an attending surgeon. Regarding the kind of surgery in the complicated appendicitis group, there are no hints for statistical differences with respect to the experience of the operating surgeon: for LA/conversion (surgical resident 38/84 [45.2 %] versus attending surgeon 46/84 [54.8 %], n.s.) compared to OA (surgical resident 30/66 [45.5 %] versus attending surgeon 36/66 [54.5 %], n.s.). Moreover, we find no significant difference in the total complication rate (LA/conversion 14/84 [16.7 %] versus OA 16/66 [24.2 %], n.s., Fig. 1a), the rate of postoperative intraabdominal abscesses (LA/conversion 4/84 [4.8 %] versus OA 3/66 [4.5 %], n.s., Fig. 1b), or the rate of postoperative ileus (LA/conversion 6/84 [7.1 %] versus OA 4/66 [6.1 %], n.s., Fig. 1d) between LA/conversion and OA. The wound infection rate (LA/conversion 3/84 [3.6 %] versus OA 11/66 [16.7 %], P < 0.01, Fig. 1c) and the resurgery rate (LA/conversion 4/84 [4.8 %] versus OA 7/66 [10.6 %], P < 0.01, Fig. 2) were significantly lower for patients treated via LA/conversion. Concerning the duration of surgery, we find no statistical difference between the two methods: 51.0 ± 22.1 min in LA/conversion versus 57.5 ± 24.5 min in OA (n.s., Fig. 3a). Hospitalization time is found to be significantly shorter for patients after LA/conversion (5.2 ± 1.5 days in LA/conversion versus 8.2 ± 5.5 days in OA, P < 0.001, Fig. 3b). However, four patients (6.1 %) needed intensive care treatment after OA, whereas no patient needed monitoring/intensive care treatment after LA/conversion. Finally, there is zero mortality in the LA/conversion group while one patient from the OA group deceased due to a severe sepsis after a prolonged postoperative intensive care treatment. One patient in the OA group had to be treated by an oncological right hemicolectomy due to a perforated incidental adenoid carcinoma.
Discussion
Although widely employed for the treatment of acute appendicitis, the role of LA for the therapy of complicated appendicitis is still under debate [9, 17–24]. In this work, we retrospectively analyzed the outcomes of 404 patients that underwent LA or OA because of acute appendicitis or complicated appendicitis. The acquired data do not show evidence of LA to being inferior to OA regarding the treatment of complicated appendicitis. Similarly to those patients with acute appendicitis, the patients with complicated appendicitis treated by LA showed significantly lower postoperative wound infection rates and shorter hospitalization time as compared to the OA group. In addition, no increased postoperative intraabdominal abscess rate was found for patients after LA in case of complicated appendicitis. We are discussing these results in more detail as follows.
The performed surgical procedure (LA or OA) depended on the laparoscopic experience of the surgeon or of the assisting consultant. Due to this, the rate of patients treated by OA was relatively high in both patient groups, that is, 44 % in the complicated appendicitis group and 35.8 % in the acute appendicitis group. Within the overall group and the complicated appendicitis group, we find no signs of a statistical difference regarding the kind of surgery with respect to the experience of the operating surgeon (surgical resident versus attending surgeon). However, within the group of patients that suffered from acute appendicitis, we found statistical hints of an asymmetry of the applied method with regard to the surgeons’ experience, that is, surgical residents, in contrast to attending surgeons, appear to have favored OA over LA/conversation in cases of acute appendicitis. Nevertheless, although this finding appears formally statistically significant within the analyzed patient group, it should be taken with a grain of salt since the sample size is limited (N = 91).
The rate of patients diagnosed with complicated appendicitis in this study is with 37.1 % higher than usually observed [7]. A reason for this may be the relatively high average age of 34.9 years (49.9 years in CA) in our patient collective [2]. Indeed, patients at the age of 45 years or older were reported to possess a significantly increased risk of perforation [10], which is accompanied by higher rates of complicated appendicitis. Li et al. have reported LA to OA conversion rates of 10 % for the treatment of acute appendicitis [25]. Regarding complicated appendicitis, this conversion rate fluctuates among 1.8–21.3 % [9, 17, 18, 20, 21]. Thus, in the present study, the conversion rate in acute appendicitis (3.7 %) is comparatively low while the significantly higher conversion rate in complicated appendicitis (13.1 %) lies within the range published in the literature.
It is well-known that patients with appendicitis undergoing LA show lower wound infection rates in comparison to OA treatments [15]. However, for these patients also, an increased incidence of postoperative intraabdominal abscesses has been reported in some studies limiting the LA-related beneficial outcomes [15]. The postoperative ileus rate after LA appears to be comparable [25] implying no advantage for one or the other method. Consistent with these studies, our patients showed significantly less wound infections and a similar postoperative ileus rate after LA as compared to OA (acute and complicated appendicitis). Remarkably, in the present study, we did not observe an OA-to-LA difference regarding the incidence of postoperative intraabdominal abscesses (acute and complicated appendicitis). These findings are in accordance with those studies also reporting similar rates of postoperative intraabdominal abscesses after LA compared with OA (see Table 1). Hence, our study raises further evidence that LA for both acute and complicated appendicitis combines the known advantages of minimally invasive surgery (e.g., lower wound infection rates) without necessarily being associated with the previously reported shortcomings (i.e., increased postoperative intraabdominal abscess rates).
In contrast to other groups reporting longer operation times for LA as compared to OA [15, 18, 21], in our study, the average duration of surgery was similar for both procedures (acute and complicated appendicitis). This discrepancy may be explained by the fact that all our LAs were performed employing Endo-GIAs for the appendicular stump management. Indeed, the use of Endo-GIAs for securing the appendicular stump during LA was shown to be more time-effective than the Endo-loop technique [26]. Patients treated by LA (acute and complicated appendicitis) displayed a significantly shorter hospitalization time as compared to OA—a result that is consistent with previous findings [15, 19, 20, 25]. In contrast to patients with acute appendicitis, patients with complicated appendicitis who were treated by LA needed significantly less resurgery compared to OA. Finally, patients with acute appendicitis needed resurgery significantly less often as compared to patients with complicated appendicitis regardless of the surgical procedure. This observation is consistent with the significantly lower rate of overall complications in acute appendicitis seen in this study.
Taken together, our observations raise further evidence for LA to be suitable not only for the treatment of acute, but also for the treatment of complicated appendicitis as the patients benefit from the known advantages of minimally invasive surgery without necessarily being at risk for increased postoperative intraabdominal abscess rates. Therefore, LA has the potential to become a safe routine method for the treatment of complicated appendicitis if performed by an experienced surgeon.
References
Wagner JM, McKinney WP, Carpenter JL (1996) Does this patient have appendicitis? JAMA 276(19):1589–1594
Ohmann C, Franke C, Kraemer M, Yang Q (2002) Status report on epidemiology of acute appendicitis. Chirurg 73(8):769–776
Körner H, Söreide JA, Pedersen EJ, Bru T, Söndenaa K, Vatten L (2001) Stability in incidence of acute appendicitis. A population-based longitudinal study. Dig Surg 18(1):61–66
Chatbanchai W, Hedley AJ, Ebrahim SB, Areemit S, Hoskyns EW, de Dombal FT (1989) Acute abdominal pain and appendicitis in north east Thailand. Paediatr Perinat Epidemiol 3(4):448–459
Foster HM, Webb SJ (1989) Appendicitis and appendicectomy in a Melanesian population. Br J Surg 76(4):368–369
Segal I, Paterson A, Walker AR (1986) Characteristics and occurrence of appendicitis in the black population in Johannesburg, South Africa. J Clin Gastroenterol 8(5):530–533
Kraemer M, Kremer K, Leppert R, Yang Q, Ohmann C, Fuchs KH (1999) Perforating appendicitis: is it a separate disease? Acute Abdominal Pain Study Group. Eur J Surg 165(5):473–480
Hermanek P (2007) Bayerische Arbeitsgemeinschaft für Qualitätssicherung in der stationären Versorgung (BAQ) Appendektomie, Jahresauswertung Modil 12/2, Bayern gesamt
Wullstein C, Barkhausen S, Gross E (2001) Results of laparoscopis vs. conventional appendectomy in complicated appendicitis. Dis Col Rectum 44(11):1700–1705
Hale DA, Molloy M, Pearl RH, Schutt DC, Jaques DP (1997) Appendectomy: a contemporary appraisal. Ann Surg 225(3):252–261
Bickell NA, Aufses AH Jr, Rojas M, Bodian C (2006) How time affects the risk of rupture in appendicitis. J Am Coll Surg 202(3):401–406
Kearney D, Cahill RA, O’Brien E, Kirwan WO, Redmond HP (2008) Influence of delays on perforation risk in adults with acute appendicitis. Dis Colon Rectum 51(12):1823–1827
Yeh CC, Wu SC, Liao CC, Su LT, Hsieh CH, Li TC (2011) Laparoscopic appendectomy for acute appendicitis is more favorable for patients with comorbidities, the elderly, and those with complicated appendicitis: a nationwide population-based study. Surg Endosc 25(9):2932–2942
Klempa I (2002) Current therapy of complicated appendicitis. Chirurg 73(8):799–804
Sauerland S, Jaschinski T, Neugebauer EA (2010) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev (10):CD001546
Aziz O, Athanasiou T, Tekkis PP, Purkayastha S, Haddow J, Malinovski V, Paraskeva P, Darzi A (2006) Laparoscopic versus open appendectomy in children: a meta-analysis. Ann Surg 243(1):17–27
Paik PS, Towson JA, Anthone GJ, Ortega AE, Simons AJ, Beart RW Jr (1997) Intra-abdominal abscesses following laparoscopic and open appendectomies. J Gastrointest Surg 1(2):188–192, discussion 192–3
Pokala N, Sadhasivam S, Kiran RP, Parithivel V (2007) Complicated appendicitis—is the laparoscopic approach appropriate? A comparative study with the open approach: outcome in a community hospital setting. Am Surg 73(8):737–741
Yau KK, Siu WT, Tang CN, Yang GP, Li MK (2007) Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg 205(1):60–65
Park HC, Yang DH, Lee BH (2009) The laparoscopic approach for perforated appendicitis, including cases complicated by abscess formation. J Laparoendosc Adv Surg Tech A 19(6):727–730
Garg CP, Vaidya BB, Chengalath MM (2009) Efficacy of laparoscopy in complicated appendicitis. Int J Surg 7(3):250–252
Asarias JR, Schlussel AT, Cafasso DE, Carlson TL, Kasprenski MC, Washington EN, Lustik MB, Yamamura MS, Matayoshi EZ, Zagorski SM (2011) Incidence of postoperative intraabdominal abscesses in open versus laparoscopic appendectomies. Surg Endosc 25(8):2678–2683
Cueto J, D’Allemagne B, Vázquez-Frias JA, Gomez S, Delgado F, Trullenque L, Fajardo R, Valencia S, Poggi L, Ballí J, Diaz J, González R, Mansur JH, Franklin ME (2006) Morbidity of laparoscopic surgery for complicated appendicitis: an international study. Surg Endosc 20(5):717–720
Katsuno G, Nagakari K, Yoshikawa S, Sugiyama K, Fukunaga M (2009) Laparoscopic appendectomy for complicated appendicitis: a comparison with open appendectomy. World J Surg 33(2):208–214
Li X, Zhang J, Sang L, Zhang W, Chu Z, Li X, Liu Y (2010) Laparoscopic versus conventional appendectomy—a meta-analysis of randomized controlled trials. BMC Gastroenterol 11(3):10–129
Sajid MS, Rimple J, Cheek E, Baig MK (2009) Use of endo-GIA versus endo-loop for securing the appendicular stump in laparoscopic appendicectomy: a systematic review. Surg Laparosc Endosc Percutan Tech 19(1):11–15
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dimitriou, I., Reckmann, B., Nephuth, O. et al. Single institution’s experience in laparoscopic appendectomy as a suitable therapy for complicated appendicitis. Langenbecks Arch Surg 398, 147–152 (2013). https://doi.org/10.1007/s00423-012-1035-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-012-1035-4