Abstract
Abnormal swallowing, dysphagia, is a potentially fatal symptom in Parkinson’s disease (PD) and is characterized by frequent silent aspiration, an unrecognized risk of suffocation and aspiration pneumonia. Several studies have reported that the injection of apomorphine, a dopamine agonist, alleviated dysphagia in some patients with PD. The effects of other antiparkinson medications against dysphagia remain controversial. Rotigotine is another dopamine agonist with non-oral administration, i.e., a transdermal patch. Its noninvasiveness seems to render this medicine even more suitable than apomorphine for dysphasic patients. However, no direct evidence has been reported. In the present retrospective open-label study, we for the first time objectively showed that rotigotine improved swallowing on videofluoroscopic examination in dysphagic patients with PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) affects voluntary and involuntary movements, including swallowing. Abnormal swallowing, dysphagia, is a potentially fatal symptom in PD as well as in other neurodegenerative diseases [1–3] and is characterized by frequent silent aspiration, an unrecognized risk of suffocation and aspiration pneumonia [4]. The effects of antiparkinson medications on dysphagia remain controversial [5], but several studies have reported that apomorphine, a dopamine agonist, alleviated dysphagia in some patients with PD [6]. Notably, this medicine improved involuntary pharyngeal functions evaluated by pharyngeal transit duration (PTD) [6]. Apomorphine is suitable for dysphagic patients because it is injected subcutaneously and is thus not affected by dysphagia, but requires invasive procedures, including repeated subcutaneous punctures for transient use or an operation to embed a syringe pump for continuous use.
Rotigotine is another dopamine agonist with non-oral administration, i.e., a transdermal patch [7]. Its noninvasiveness seems to render this medicine even more suitable than apomorphine for dysphasic patients. However, no direct evidence that rotigotine is effective against dysphagia has been reported. In contrast, an extensive literature search identified only one study reporting that rotigotine was effective against parkinsonism but not dysphagia in a patient who had PD with severe esophageal cancer-related dysphagia [8]. In the present open-label study, we objectively showed that rotigotine improved swallowing on videofluoroscopic (VF) examination in dysphagic patients with PD.
Patients and Methods
Patients
We retrospectively studied six consecutive patients with PD (4 men and 2 women, age 75 ± 6 years, mean ± SD) who complained of symptoms probably caused by dysphagia, such as swallowing difficulty, drooling, coughing after swallowing, or aspiration pneumonia (Table 1). The mean body weight was 50 kg. All patients were given a clinical diagnosis of PD by board-certified neurologists in accordance with the UK Parkinson’s disease Society Brain Bank Clinical Diagnostic Criteria. No patient had received antiparkinson medication until this study; all patients were thus drug-naïve.
VF Examinations
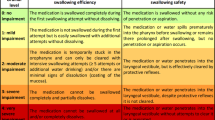
VF was performed according to a previously described method, with slight modification [9, 10]. Briefly, a diluted solution of barium (5 ml) was swallowed twice. If the swallowing problem was not very severe as indicated by the procedure and rating scales described below, a concentrated solution of barium was then swallowed once; the amount was not restricted, and the subject was requested to swallow as usual to detect swallowing problems encountered in daily life. Worse scores were obtained on each swallow according to the scales described below. Six grams of barium mixed with jelly was then swallowed. The results of VF were evaluated according to a Japanese scale established by the Japanese Society of Dysphagia Rehabilitation, already reported several times in the English-language literature (please see supplemental Table 1 and videos for details), as well as according to the Dysphagia Outcome and Severity Scale (DOSS) [2, 3, 10]. The following VF variables were assessed according to the Japanese scale: lip closure, bolus formation, and bolus transport during the oral phase and constriction of the pharynx, elevation of the larynx, bolus stasis at the valleculae and pyriform sinus, and aspiration during the pharyngeal phase. A three-point scale was used to semi-quantify each variable in a series of VF: 3 (normal), 2 (disturbed), and 1 (severely disturbed). When the Japanese scale was used, the oral phase (3 = severely affected and 9 = normal) and the pharyngeal phase (4 = severely affected and 12 = normal) were separately evaluated, and the values were summed to derive the total score. DOSS (1 = severely affected and 7 = normal) is more widely used internationally, but the oral and pharyngeal phases cannot be separately evaluated. One speech language pathologist and one neurologist who were blinded to all clinical details independently scored the results for each patient. Both had more than 10 years of experience in swallowing evaluation. More than 90 % of the point scores were matched between the initial evaluators. If there was any discrepancy, three additional neurologists who were also experts in swallowing evaluation and disorders decided which score was appropriate.
PTD was calculated from the time of arrival of the bolus head (5 ml of barium) at the ramus of the mandible until the time that the tail of the bolus passed through the upper esophageal sphincter, as described previously [6]. PTD was also measured in six healthy controls (age 60 ± 24 years).
Evaluation of Parkinsonism
Parkinsonism was evaluated according to the Hoehn–Yahr grade and the United Parkinson’s Disease Rating Scale (UPDRS), Part III (UPDRS-III, motor examination). All patients were evaluated before and 1–2 weeks after starting treatment with 2 mg/day of rotigotine (the patch contains 4.5 mg rotigotine, but only 2 mg/day is absorbed). Two of the six patients initially had jaw tremor. This study was approved by the Institutional Review Board of Kinki University. All patients enrolled in this study gave written informed consent.
Results
Improvement in Swallowing Function
Clinically, dysphagia-related symptoms completely disappeared in all patients (Table 1). Swallowing function as evaluated by the Japanese scale on VF examinations improved significantly in all patients tested (Fig. 1). For example, the videos 1 and 2 showed the improvement of swallowing by rotigotine in Patient 1 (see also the result of the VF scores in supplemental Table 1). The improvement was found during both the oral and pharyngeal phases in the six patients. The pre-treatment PTD (1.07 ± 0.38 s) in the six patients with PD was significantly longer than that in the controls (0.65 ± 0.38 s, p < 0.05, Mann–Whitney U test). After treatment, however, the PTD was significantly shortened (0.84 ± 0.22 s, p < 0.05, Wilcoxon signed-rank test) and did not differ significantly from the control value (p = 0.08, Mann–Whitney U test). The scores of DOSS increased slightly, indicating improved swallowing function, but not significantly.
Swallowing function in six patients with Parkinson disease before (pre) and after (post) application of a rotigotine transdermal patch. The videofluoroscopic (VF) examinations revealed significant improvements (p < 0.05, Wilcoxon signed-rank test) in the total scores, scores during the oral and pharyngeal phases, and pharyngeal transit duration (PTD). The Dysphagia Outcome and Severity Scale (DOSS) scores improved slightly, but not significantly
Improvements in Parkinsonism as Evaluated by Hoehn–Yahr Grade and UPDRS-III
Parkinsonism improved in all patients according to the UPDRS-III score, with no significant change in Hoehn–Yahr grade. The changes in the UPDRS-III score were not significantly associated with the changes in VF scores, PTD, or DOSS.
Discussion
Our open-label study in 6 patients showed that swallowing functions on VF evaluations were significantly improved by application of a rotigotine transdermal patch, with the disappearance of their dysphagia-related symptoms. Accumulating evidence suggests that antiparkinson medications improve swallowing during the oral phase, characterized mainly by voluntary movements [5]. The reduced UPDRS-III scores in our study also supported an improvement in voluntary movements affected by parkinsonism. In addition, our results showed that rotigotine improved the scores during the pharyngeal phase, associated mainly with sequential reflexes of striatal muscles. Moreover, PTD improved in all patients. The DOSS score also improved slightly, but not significantly. This is feasible because DOSS may be less sensitive than the Japanese scale evaluations, as in spinocerebellar ataxias [2]. Our results are supported by the findings of a previous study showing that the pharyngeal phase of swallowing was improved by the dopamine agonist apomorphine [11]. Furthermore, levodopa also considerably improved pharyngeal functions on videoendoscopic evaluation in a previously reported patient with PD [12]. We thus speculate that central dopaminergic stimulation also facilitates the pharyngeal phase as well as the oral phase and thereby improved swallowing function in our patients.
Surprisingly, only an initial dose of rotigotine (2 mg/day) improved both voluntary movements and swallowing function. A small dose was effective in some population of patients with PD. A reported clinical trial showed that even 2 mg/day seemed to reduce parkinsonism with the extent equivalent to that for 4 mg/day until 2 weeks [13]. Another study for early PD with the protocol that allowed to increase the dosage of rotigotine to 6 mg/day demonstrated that about 3 % of patients remained to receive 2 mg/day [14]. Although the precise reason for the good response to rotigotine in our patients remains unclear, one plausible reason may include a racial difference in body weight between the previous studies and ours; patients with larger weight generally need larger doses for the same effect. In a reported clinical trial in the US, the mean body weight was 81 kg [14], while that in this study in Japan was only 50 kg (62 % of that in the US). Another racial factor might include skin permeability, as reported in other medicines [15]. One can speculate the attribution of a “placebo effect” to the observed good response since this was an open-label study. However, the extent of placebo effects is about 2–4 points on average of UPDRS-III [16]. Thus, the improvement in our patients surpassed the previously reported placebo effect. In addition, swallowing function was evaluated by an objective method (VF examination), which might minimize placebo effects. A small dose of rotigotine may therefore have exerted beneficial effects in some population of patients with PD, such as those having dysphagia, though firm conclusions must await future placebo-controlled studies.
The mechanism by which apomorphine in previous studies and rotigotine in the present study exerted beneficial effects on swallowing functions remains unestablished, but the high specificities of these drugs to dopamine receptor subtypes might be related to such effects. Apomorphine has a stronger affinity to the D1 receptor (pKi = 6.43) than ropinirole (pKi < 5.0) or pramipexole (pKi < 5.0), currently the most widely used antiparkinson agents. Rotigotine has an even higher affinity (pKi = 7.08) than apomorphine. Mice lacking the dopamine D1 receptor showed abnormal motor activities and feeding problems [17]. Guinea pigs treated with a specific D1 inhibitor had impaired swallowing function [18]. These findings might be related to the good response of dysphasia to apomorphine and rotigotine.
We should note that dopaminergic treatments could not completely resolve impairment during the pharyngeal phases of swallowing in the present and previous studies. Mechanisms that underlie possible limitations of dopaminergic treatments include the fact that α-synuclein pathology in PD has been reported to extend to non-dopamine neurons, such as the sensory branches of the vagal and glossopharyngeal nerves innervating the pharynx and peripheral motor nerves innervating pharyngeal muscles [19, 20]. Future treatments might target such neurons.
In conclusion, our study showed for the first time to our knowledge that rotigotine significantly improved swallowing function as evaluated by an objective VF examination in dysphagic patients with PD.
References
Muller J, Wenning GK, Verny M, McKee A, Chaudhuri KR, Jellinger K, Poewe W, Litvan I. Progression of dysarthria and dysphagia in postmortem-confirmed parkinsonian disorders. Arch Neurol. 2001;58:259–64.
Isono C, Hirano M, Sakamoto H, Ueno S, Kusunoki S, Nakamura Y. Differences in dysphagia between spinocerebellar ataxia type 3 and type 6. Dysphagia. 2013;28:413–8.
Higo R, Nito T, Tayama N. Swallowing function in patients with multiple-system atrophy with a clinical predominance of cerebellar symptoms (MSA-C). Eur Arch Otorhinolaryngol. 2005;262:646–50.
Troche MS, Brandimore AE, Okun MS, Davenport PW, Hegland KW. Decreased cough sensitivity and aspiration in Parkinson disease. Chest. 2014;146:1294–9.
Melo A, Monteiro L. Swallowing improvement after levodopa treatment in idiopathic Parkinson’s disease: lack of evidence. Parkinsonism Relat Disord. 2013;19:279–81.
Tison F, Wiart L, Guatterie M, Fouillet N, Lozano V, Henry P, Barat M. Effects of central dopaminergic stimulation by apomorphine on swallowing disorders in Parkinson’s disease. Mov Disord. 1996;11:729–32.
Jankovic J, Watts RL, Martin W, Boroojerdi B. Transdermal rotigotine: double-blind, placebo-controlled trial in Parkinson disease. Arch Neurol. 2007;64:676–82.
LeWitt PA, Lyons KE, Pahwa R. Advanced Parkinson disease treated with rotigotine transdermal system: PREFER Study. Neurology. 2007;68:1262–7.
Longemann JA. Evaluation and treatment of swallowing disorders. San Diego: College-Hill Press; 1983.
O’Neil KH, Purdy M, Falk J, Gallo L. The dysphagia outcome and severity scale. Dysphagia. 1999;14:139–45.
Hunter PC, Crameri J, Austin S, Woodward MC, Hughes AJ. Response of parkinsonian swallowing dysfunction to dopaminergic stimulation. J Neurol Neurosurg Psychiatry. 1997;63:579–83.
Warnecke T, Hamacher C, Oelenberg S, Dziewas R. Off and on state assessment of swallowing function in Parkinson’s disease. Parkinsonism Relat Disord. 2014;20:1033–4.
Poewe W, Luessi F. Clinical studies with transdermal rotigotine in early Parkinson’s disease. Neurology. 2005;65:S11–4.
Watts RL, Jankovic J, Waters C, Rajput A, Boroojerdi B, Rao J. Randomized, blind, controlled trial of transdermal rotigotine in early Parkinson disease. Neurology. 2007;68:272–6.
Gean CJ, Tur E, Maibach HI, Guy RH. Cutaneous responses to topical methyl nicotinate in black, oriental, and caucasian subjects. Arch Dermatol Res. 1989;281:95–8.
Giladi N, Boroojerdi B, Korczyn AD, Burn DJ, Clarke CE, Schapira AH. Rotigotine transdermal patch in early Parkinson’s disease: a randomized, double-blind, controlled study versus placebo and ropinirole. Mov Disord. 2007;22:2398–404.
Xu M, Moratalla R, Gold LH, Hiroi N, Koob GF, Graybiel AM, Tonegawa S. Dopamine D1 receptor mutant mice are deficient in striatal expression of dynorphin and in dopamine-mediated behavioral responses. Cell. 1994;79:729–42.
Jia YX, Sekizawa K, Ohrui T, Nakayama K, Sasaki H. Dopamine D1 receptor antagonist inhibits swallowing reflex in guinea pigs. Am J Physiol. 1998;274:R76–80.
Mu L, Sobotka S, Chen J, Su H, Sanders I, Nyirenda T, Adler CH, Shill HA, Caviness JN, Samanta JE, Sue LI, Beach TG. Parkinson disease affects peripheral sensory nerves in the pharynx. J Neuropathol Exp Neurol. 2013;72:614–23.
Mu L, Sobotka S, Chen J, Su H, Sanders I, Adler CH, Shill HA, Caviness JN, Samanta JE, Beach TG. Alpha-synuclein pathology and axonal degeneration of the peripheral motor nerves innervating pharyngeal muscles in Parkinson disease. J Neuropathol Exp Neurol. 2013;72:119–29.
Conflict of interest
Makito Hirano received travel expenses and honoraria for lectures from Ono, Otsuka, and Takeda Pharmaceuticals. This study was partly supported by Grants-in-Aids for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (25461297 to MH) and by a University Research Grant from Kinki University (KD03 to MH). Chiharu Isono, Shuichi Ueno, Hikaru Sakamoto, Susumu Kusunoki, and Yusaku Nakamura report no conflict of interest (COI), as confirmed by the institutional COI committee.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
455_2015_9622_MOESM1_ESM.tif
The results of the videofluoroscopic (VF) examinations of Patient 1 before (video 1) and after (video 2) treatment with rotigotine (2 mg/day) for 1 week. Video 1 showed that bolus formation and transportation during the oral phase were impaired possibly because of tremorous movements of the tongue and pharynx. The constriction of pharynx and elevation of larynx during pharyngeal phase were impaired with large amounts of bolus stasis at the valleculae and the pyriform sinus. Frequent and modest pharyngeal penetration and more importantly silent aspiration were observed. Video 2 showed that tremorous movement disappeared with normalization of his swallowing function during the oral phase. The constriction of pharynx and elevation of larynx during pharyngeal phase remained impaired with large amounts of bolus stasis at the valleculae and the pyriform sinus. However, the frequency and extent of pharyngeal penetration reduced, with no aspiration observed. Supplementary material 1 (TIFF 3987 kb)
Rights and permissions
About this article
Cite this article
Hirano, M., Isono, C., Sakamoto, H. et al. Rotigotine Transdermal Patch Improves Swallowing in Dysphagic Patients with Parkinson’s Disease. Dysphagia 30, 452–456 (2015). https://doi.org/10.1007/s00455-015-9622-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-015-9622-5