Abstract
We investigated the swallowing function of 21 patients with multiple system atrophy with a clinical predominance of cerebellar symptoms (MSA-C) by videofluoroscopy (VF). Twenty-six VF examinations were performed at various time points, and they were divided into three groups according to the duration following disease onset: Group A had 1 to 3 years following disease onset (the early stage of the disease), group B had 4 to 6 years following disease onset (the middle stage of the disease), and group C had more than 7 years following disease onset (the late stage of the disease). Swallowing function in the oral phase became gradually disturbed over the progression of MSA. Delayed bolus transport from the oral cavity to the pharynx was already seen in 50% of the patients in group A, and it was seen in more than 85% of the patients in group C. Bolus holding in the oral cavity was slightly disturbed in group A, but it was seen in 57% of the patients in group C. Our study shows that parkinsonism is related to swallowing dysfunction in MSA, but cerebellar dysfunction also affects coordination of the tongue; bolus transport in the oral cavity was disturbed in the early stage of disease. Progression of cerebellar dysfunction and overlapped parkinsonism will worsen tongue movement, and in the late stage of the disease, swallowing function of the oral phase (bolus transport and bolus holding) was remarkably disturbed. Swallowing function in the pharyngeal phase was not significantly correlated to the duration of the disease; however, our study showed that swallowing function in the pharyngeal phase was not assessed fully by VF examination in MSA-C only. Combination with other examinations, such as manometry and electromyography, may be useful, especially in the late stage of the disease. In addition, an analysis concerning the relationship between aspiration seen on VF examination and a history of aspiration pneumonia in MSA-C patients suggested that the sensory system at the larynx and trachea should also be assessed in patients in the late stage of MSA-C.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple system atrophy (MSA), a progressive neurodegenerative disorder of unknown etiology, is considered a general pathological term, which was defined by Graham and Oppenheimer [5]. MSA shows various clinical aspects, such as cerebellar ataxia, parkinsonism, autonomic nervous system failure and pyramidal signs. According to these aspects, MSA had previously been described in three ways: as olivopontocerebellar atrophy (OPCA), as striatonigral degeneration (SND) and as Shy-Drager syndrome (SDS). However, Wenning et al. [12] recently proposed avoiding the term “MSA of the SDS type.” In addition to the basic fact that almost all MSA patients suffer from some degree of autonomic dysfunction, the patient in Shy and Drager’s case [11] developed parkinsonism and cerebellar signs, and showed pathology of both SND and OPCA. Based on a clinicopathological analysis, diagnostic criteria were proposed by a Consensus Conference in 1998 [4]: MSA-C, with a clinical predominance of cerebellar symptoms, and MSA-P, with a clinical predominance of parkinsonism. The Consensus Conference put forward that the term Shy Drager syndrome had been widely misused and was no longer useful [4].
Dysphagia is the most critical complication of MSA and is closely related to patient prognosis [9]. Evaluation and appropriate treatment of patients suffering from dysphagia might prevent or delay complications, such as aspiration pneumonia, and thereby improve quality of life and increase survival time [9]; however, swallowing function of patients with MSA has not been well reported.
We previously reported on the swallowing function of MSA patients, evaluated by videofluoroscopy (VF) and manometry [6]. Abnormal findings in VF were generally consistent with those in Parkinson’s disease. As a result, the oral phase of swallowing was most involved. Delayed bolus transport from the oral cavity to the pharynx was the most common disturbance found (72.7%), followed by disturbance of bolus holding in the oral cavity (48.5%). In the pharyngeal phase, slowing of upward relocation of the larynx was also found in 39.3% of the patients. Insufficient constriction of the pharynx, bolus stasis at the pyriform sinus (PS) and impaired UES opening were not commonly found [6]. These results imply that swallowing function in MSA patients might be more influenced by parkinsonism than cerebellar dysfunction, and that parkinsonism mainly affects the oral phase of swallowing. From these facts, it is reasonable to think that MSA-P patients suffer from dysphagia, caused by parkinsonism, beginning in the early stage of the disease. However, MSA-C patients also complain of dysphagia in the early stage of the disease [8], although they do not always show parkinsonism in the early stage of the disease. In MSA-C patients, how cerebellar dysfunction influences swallowing function and how swallowing dysfunction will advance over progression of the disease, with cerebellar dysfunction progressing and parkinsonism overlapping, are unsolved problems. The aim of this study was to evaluate swallowing function using VF in MSA-C patients over the progression of the disease and to elucidate how swallowing dysfunction advances in MSA-C.
Patients and methods
Twenty-one patients diagnosed as having MSA-C at the Department of Neurology in our institute were referred to our swallowing and speech clinic for evaluation of swallowing function. All of them were sporadic cases and showed negative molecular genetic evidence. The clinical subtype of MSA was classified according to the “Consensus statement on the diagnosis of multiple system atrophy,” defined by Gilman et al. [4], and all of the cases were diagnosed as having probable MSA-C. They were divided into three groups according to the duration following disease onset (Table 1): Group A had 1 to 3 years following disease onset (the early stage of the disease), group B had 4 to 6 years following disease onset (the middle stage of the disease), and group C had more than 7 years following disease onset (the late stage of the disease).
These 21 patients with MSA-C were investigated by videofluoroscopy (VF). VF was performed from once to several times, at various time points. Seventeen patients received one examination each, while other patients received VF evaluation several times (twice in three patients; three times in one). In total, 26 VF examinations were performed at various time points over the progression of the disease. Appropriate and safe bolus textures (thin liquid or semisolid) and bolus volumes (1 ml, 3 ml, 5 ml, or self-regulated) were used in each patient. As contrast medium, a 140%/v barium mixture was routinely used, but a water-soluble contrast medium (Omnipaque 300, Daiichi Pharmaceutical Co., Ltd., Tokyo) was given when a risk of aspiration was suspected. The assessment parameters in VF are set as follows: bolus transport from the mouth to the pharynx, bolus holding in the oral cavity, pharyngeal constriction, laryngeal elevation, bolus stasis at the PS, upper esophageal sphincter (UES) opening and aspiration. A three-point scale was used to quantify each parameter: 0 (normal), 1 (slightly disturbed) and 2 (disturbed). A history of aspiration pneumonia was ascertained from the patients’ records. Informed consent was obtained from each patient, and they were treated according to the Declaration of Helsinki.
Alterations in the assessment parameters on VF examination among groups A, B and C were analyzed using Spearman’s rank correlation. Statistical significance was defined as P <0.05.
Results
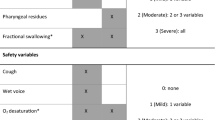
Figure 1 shows the videofluoroscopic findings of groups A, B and C. Delayed bolus transport from the oral cavity to the pharynx was already seen in 50% of the patients in group A (1 to 3 years following disease onset, the early stage of the disease), and it was seen in more than 85% of the patients in group C (more than 7 years following disease onset, the late stage of the disease). Bolus holding in the oral cavity was slightly disturbed in group A, but it was seen in 57% of the patients in group C. Parameters of VF examination in the oral phase worsen over the progression of the disease. Spearman’s rank correlation showed that bolus holding in the oral cavity was significantly correlated to the duration of the disease ( P =0.0495). Bolus transport from the oral cavity to the pharynx was not significantly correlated to the duration of the disease ( P =0.0581), but it tended to worsen over the progression of the disease.
In the pharyngeal phase, all parameters on VF examination showed only slight disturbances in group A. In group B, slowing of upward relocation of the larynx was found in 36% of the patients. Bolus stasis at the PS was not seen in group A, but it was found in about 30% of the patients in group B. Disturbances in the pharyngeal phase seen in group C were generally similar to those in group B, but no abnormality was found concerning UES opening in group C. UES opening was relatively well maintained through all stages of the disease. Spearman’s rank correlation showed that none of the parameters on VF examination in the pharyngeal phase (pharyngeal constriction, laryngeal elevation, bolus stasis at the PS and UES opening) were significantly correlated to the duration of the disease.
A history of aspiration pneumonia was seen in 12.5% of the patients in group A, in 0% of the patients in group B and in 42.9% of the patients in group C (Table 2). Aspiration pneumonia was seen more in group C than in group A or B. By Spearman’s rank correlation, no significant correlation was seen between aspiration (a parameter on VF examination in the pharyngeal phase) and a history of aspiration pneumonia.
Discussion
This study showed that swallowing function in the oral phase became gradually disturbed over the progression of MSA-C. Delayed bolus transport from the oral cavity to the pharynx is already disturbed in the early stage of the disease, in which parkinsonism has less influence on swallowing than in the middle and late stages of the disease. Disturbed coordination of tongue movement by cerebellar dysfunction causes delayed bolus transport in the early stage of the disease. Progression of cerebellar dysfunction and overlapped parkinsonism (tremor and/or bradykinesia) may worsen tongue movement, and in the late stage of the disease, more than 85% of these patients suffer from delayed bolus transport from the oral cavity to the pharynx. In contrast, bolus holding in the oral cavity was not very disturbed in the early stage of the disease, and it worsened in the middle and late stages of the disease. This result suggests that parkinsonism is more related to the ability to hold a bolus than cerebellar dysfunction is.
Cerebellar dysfunction does not severely influence pharyngeal swallowing in the early stage of the disease. In the middle and late stages of the disease, laryngeal elevation and pharyngeal constriction were disturbed in 30–40% of the patients. The cause of these can be assumed to be dysfunction of the suprahyoid muscles and thyropharyngeal muscle, which are regulated by somatic nerves, such as the hypoglossal, facial, mandibular and vagus nerves. Poor regulation by somatic nerves, caused by extrapyramidal symptoms, and latent weakness of the suprahyoid muscles and thyropharyngeal muscle, may lead to pharyngeal swallowing dysfunction.
Kurita et al. divided MSA-C patients into two groups (group I: patients with less than 4 years’ duration of the disease; group II: patients with more than 5 years’ duration of the disease), and evaluated swallowing function using VF and manometry [8]. They found that 83.3% of the patients in group II suffered from incomplete UES relaxation, compared to only 22.2% of the patients in group I [8]. In another report, Kurita et al. investigated 13 patients with OPCA (MSA-C), and 5 of them showed incomplete relaxation of the UES [7]. They discussed that patients with more than 5 years’ duration of OPCA (MSA-C) tended to show incomplete relaxation of the UES [7, 8]. We also reported incomplete UES relaxation in 60% of patients with more than 5 years’ duration of MSA-C [6]. These reports suggest that UES function is also affected by duration of MSA, especially after more than 5 years’ duration of the disease. However, VF can only assess opening of the UES, which is different from relaxation of the UES [2]. In this study, UES opening was almost maintained at normal function in all stages of the disease (Fig. 1). VF is the most reliable evaluation tool for swallowing, but it cannot fully evaluate changes of the swallowing status in MSA-C. We recommend use of other examination methods, such as manometry and electromyography (EMG), together with VF, to evaluate swallowing function in MSA-C.
Few of our patients showed aspiration on VF examination, even in groups B and C, while group C had the largest number with a history of aspiration pneumonia (42.9%). The discrepancy between the rate of aspiration seen on VF examination and a history of aspiration pneumonia suggested that patients might be at risk for aspiration pneumonia even though aspiration is not found on VF examination. Since symptoms of MSA vary and change from one point in time to another, MSA patients, without showing aspiration on VF examination, may aspirate critically when in poor condition. Or, since swallowing on VF examination is done on demand under a specific condition different from when food is eaten normally in daily life, the patients might be more concentrated on swallowing during VF examination. In addition, the ability to protect the airway is quite an important factor for aspiration pneumonia. Patients might not be at risk for aspiration pneumonia if they can cough out an aspirated bolus. To appropriately evaluate silent aspiration, the sensory system at the larynx and trachea, which protects the airway from bolus aspiration, should also be assessed, in patients in group C, many of whom had a history of aspiration pneumonia. Flexible endoscopic evaluation of swallowing with sensory testing (FEESST), as described by Aviv et al., is useful for sensory testing of the larynx [3]. The cough test is also useful to assess the protective ability of the airway system [1, 10]. These examinations will be useful to prevent MSA-C patients from aspiration pneumonia.
Conclusion
We performed 26 VF examinations on MSA-C patients at various time points and assessed changes of swallowing functions in MSA-C over the duration of the disease. Swallowing function in the oral phase became gradually disturbed with the progression of MSA. Cerebellar dysfunction affects bolus transport from the oral cavity to the pharynx in the early stage of the disease. Progression of cerebellar dysfunction and overlapped parkinsonism will worsen tongue movement, and in the late stage of the disease, swallowing function in the oral phase (bolus transport and bolus holding) was remarkably disturbed. Swallowing function in the pharyngeal phase was not significantly correlated to the duration of the disease, but our study also showed that swallowing function in the pharyngeal phase was not assessed fully by only VF examination in MSA-C. The combination of other examinations, such as manometry and EMG, together with VF, may be useful, especially in the late stage of the disease. We also emphasize that an assessment of the sensory system at the larynx and trachea is important and should also be done in patients in the late stage of MSA-C.
References
Addington WR, Stephens RE, Gilliland KA (1999) Assessing the laryngeal cough reflex and the risk of developing pneumonia after stroke: an interhospital comparison. Stroke 30:1203–1207
Ali GA, Wallace KL, Schwartz R, DeCarle DJ, Zagami AS, Cook IJ (1996) Mechanisms of oral-pharyngeal dysphasia in patients with parkinson’s disease. Gastroenterology 110:383–392
Aviv JE, Kaplan ST, Thomson JE, Spitzer J, Diamond B, Close LG (2000) The safety of flexible endoscopic evaluation of swallowing with sensory testing (FEESST): an analysis of 500 consecutive evaluations. Dysphagia 15:39–44
Gilman S, Low PA, Quinn N, Albanese A, Ben-Shlomo Y, Fowler CJ, Kaufmann H, Klockgether T, Lang AE, Lantos PL, Litvan I, Mathias CJ, Oliver E, Robertson D, Schatz I, Wenning GK (1999) Consensus statement on the diagnosis of multiple system atrophy. J Neurol Sci 163:94–98
Graham JG, Oppenheimer DR (1969) Orthostatic hypotension and nicotine sensitivity in a case of multiple system atrophy. J Neurol Neurosurg Psychiatry 32:28–34
Higo R, Tayama N, Watanabe T, Nitou T, Ugawa Y (2003) Videofluoroscopic and manometric evaluation of swallowing function in patients with multiple system atrophy. Ann Otol Rhinol Laryngol 112:630–636
Kurihara K, Kita K, Hirayama K, Hara T, Toyama M (1990) Dysphagia in olivopontocerebellar atrophy. Clin Neurol 30:146–150
Kurihara K, Kita K, Hirayama K, Hara T (1993) Dysphagia in multiple system atrophy—radiological and manometric study. Clin Neurol 33:271–277
Muller J, Wenning GK, Verny M, McKee A, Chaudhuri KR, Jellinger K, Poewe W, Litvan I (2001) Progression of dysarthria and dysphagia in postmortem-confirmed parkinsonian disorders. Arch Neurol 58:259–264
Nakajoh K, Nakagawa T, Sekizawa K, Matsui T, Arai H, Sasaki H (2000) Relation between incidence of pneumonia and protective reflexes in post-stroke patients with oral or tube feeding. J Intern Med 247:39–42
Shy GM, Drager GA (1960) A neurological syndrome associated with orthostatic hypotension. Arch Neurol 2:511–527
Wenning GK, Ben-Shlomo Y, Magalhaes M, Daniel SE, Quinn NP (1994) Clinical features and natural history of multiple system atrophy. An analysis of 100 cases. Brain 117:835–845
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Higo, R., Nito, T. & Tayama, N. Swallowing function in patients with multiple-system atrophy with a clinical predominance of cerebellar symptoms (MSA-C). Eur Arch Otorhinolaryngol 262, 646–650 (2005). https://doi.org/10.1007/s00405-004-0883-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-004-0883-0