Abstract
Dysphagia associated with Parkinson’s disease (PD) affects the mortality and quality of life of patients with PD. Avoiding aspiration and maintaining swallowing ability are among the concerns regarding PD care. Therefore, we developed a swallowing supplement for easier swallowing and tolerability in patients with PD. Thirty patients with PD and 50 healthy controls were enrolled and their swallowing function measured using the videofluoroscopic swallowing study (VFSS) and several dysphagia scales. The Unified Parkinson’s Disease Rating Scale motor scores, Hoehn and Yahr stage, and levodopa doses were evaluated in patients with PD. The VFSS and survey were used to assess the viscosity, color, taste, nutrition, safety, and tolerability of the swallowing supplement. The MMSE score, serum albumin, and hemoglobin levels, and oral conditions were worse in the PD group than in the control group. Compared with controls, patients with PD had significantly lower total and sub-item scores of the swallowing quality of life (swal-QoL). Using commercialized yogurt, the pharyngeal delay time (PDT) and the modified penetration aspiration scale were higher in the PD group than in the control group. The swallowing supplement significantly shortened the PDT and pharyngeal transit time (PTT). Moreover, compared with commercialized yogurt, it improved pharyngeal wall coating, PTT, and aspiration in the videofluoroscopic dysphagia subscales. The survey scores were above average to good in the “easy swallowing” and “pharyngeal residual sense” items and tolerable in the remaining 6 preference items. This swallowing supplement could prevent aspiration and dysphagia complications in patients with PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dysphagia is a very common but difficult Parkinson’s disease (PD) symptom to treat [1]. Its reported prevalence varies across studies since it depends on the age, PD subtype, disease severity, and cognition status [1,2,3]. Dysphagia is significantly associated with aspiration pneumonia, which is the highest mortality cause in patients with PD [4], and thus significantly affects their quality of life [1]. Pathophysiology underlying PD-associated dysphagia remains unclear. Reduced cortical activation and severe cognitive dysfunction are negatively associated with swallowing ability [5]. Additionally, neuronal death in the substantia nigra pars compacta and dysfunction of the swallowing central pattern generator located in the medulla might cause dysphagia in PD [5, 6]. Therefore, cortical function, as well as the interaction between the basal ganglia and brainstem, could affect swallowing function modulation. Moreover, PD-associated dysphagia could be reported in early-stage PD and is not always associated with PD severity [7]. The definite dysphagia cause and its effective treatments currently remain unclear; moreover, conventional dopaminergic treatment and deep brain stimulation are ineffective in improving dysphagia in patients with PD [8, 9]. Therefore, non-dopaminergic systems could play a crucial role in dysphagia [10]. There have been few reports regarding PD-associated dysphagia even in the early disease stages; moreover, functional swallowing disability mostly involves the oral swallowing phase [11, 12]. Most studies on PD-associated dysphagia have assessed the dysphagia risk or analyzed factors associated with dysphagia [13]. However, it is more important to prevent aspiration and maintain swallowing ability in patients with PD. Generally, swallowing rehabilitation, as well as behavioral and electrophysiological treatments, has been attempted in patients with dysphagia [14]. However, insufficient foods have been developed for alleviating swallowing disorders. This study aimed to develop elderly friendly swallowing supplements that are easier to swallow than commercialized yogurt. Furthermore, we aimed to evaluate the safety and tolerability of our swallowing supplements in patients with PD compared with age-matched healthy controls.
Methods
Participants
We enrolled 30 patients with PD who regularly visited the movement disorder clinic without changing of medication within 8 weeks, as well as 50 age-matched healthy controls. All the patients with PD lacked a history of uncomfortable dysphagia and aspiration. Most patients with PD are unaware of their swallowing impairment [15]; therefore, the term “symptomless dysphagia” was employed for patients unaware of their swallowing impairment revealed by an objective swallowing test. Furthermore, we used the term “presbyphagia” for elderly healthy controls to differentiate them from patients with PD [16]. We excluded participants with neurological diseases, head and neck cancer, and diagnosed dementia. We assessed cognitive status in both groups using the Mini-Mental State Examination (MMSE). Furthermore, a movement disorder specialist (E.O) assessed the disease status using the Hoehn and Yahr (H&Y) stage, the Unified Parkinson’s Disease Rating Scale-III, disease duration, and levodopa equivalent dose in the PD group. Furthermore, we excluded patients with dysphagia, which is affected by the status of PD medication. This study was approved by the ethics committee of Chungnam National University Hospital. All the participants provided informed consent before data collection.
Swallowing analysis
Videofluoroscopic swallowing studies
We used the videofluoroscopic swallowing studies (VFSS) as an objective measurement tool since it is the gold standard for evaluating PD-related dysphagia [1, 17]. VFSS was performed in a medication on state. Moreover, we simultaneously video-recorded at 30 frames per second (INFINITT PACS video) to analyze dysphagia patterns (FLEXAVISION; Shimadzu Corp., Kyoto, Japan). The participants were seated upright in the fluoroscopy chair. Subsequently, each participant was required to swallow 5 bolus types as follows: rice porridge, yogurt (Dongwon Co., Seoul, Korea), water (Jeju Province Developmental Co., Jeju, Korea) 2.5 cc, water 5 cc, and steamed rice in that order. The boluses were administered using a tablespoon mixed at a 1:1 ratio with a contrast medium. All VFSS images were viewed in the lateral plane, which included the lips anteriorly to the vertebrae posteriorly, as well as the soft palate superiorly to the sixth cervical vertebra inferiorly. The VFSS was immediately discontinued in case of aspiration due to chocking from any boluses were noticed or the participants complained of dyspnea. A wall suction was equipped in a fluoroscopy room and a physician closely monitored vital signs during the entire examination time.
Analysis of swallowing physiology
Two skilled physiatrists analyzed the video files under the supervision of an aspiration rehabilitation specialist (S.A). The physiatrists counted the number of frames and determined the time (seconds) taken during each swallowing phase. The oral transit time (OTT) was defined as the time taken for the main bolus in the oral cavity to start moving to the posterior until the bolus head reached the lower edge of the mandibular ramus. The pharyngeal transit time (PTT) was defined as the time from the head of the main bolus reaching the lower edge of the mandibular ramus to the bolus tail passing through the cricopharyngeal region approximately 1 cm below the true vocal folds. The pharyngeal delay time (PDT) is a PTT component defined as the time from the bolus head arriving at the lower edge of the mandibular ramus to triggering of the pharyngeal swallow. Temporal data were acquired through analysis of the bolus position in the oropharynx as previously defined [18]. The videofluoroscopic dysphagia scale (VDS), which developed by Hahn et al., was measured. This scale is expressed as a score out of 100 and comprehensively reflects the findings of the videofluoroscopy test [19]. A skilled rehabilitation physician performed VDS scoring for each participant.
Functional measurement of swallowing
The modified penetration aspiration scale (mPAS) and the American Speech-Language-Hearing Association National Outcome Measurement System (ASHA-NOMS) describe the swallowing abilities with higher ASHA-NOMS scores indicating improved swallowing function [20]. The mPAS is a revised PAS version that evaluates airway invasion severity based on the level of swallowing materials (levels 1 to 5). Penetration and aspiration refer to the materials not passing and passing below the vocal cord level, respectively. Higher mPAS scores indicate decreased swallowing function [21]. One skilled rehabilitation physician performed scoring for each participant.
Swallowing supplement
The viscosity of the swallowing supplement was a spoon thick, which is most frequently used for the dysphagia test given the convenience of controlling the bolus speed, pharyngeal residue clearance, and penetration or aspiration [22]. The swallowing supplement was developed by the Korea Food Research Institute (KFRI) as a probiotic thickened liquid containing 5% lipid nanoparticle carrier with 200 ppm of vitamin D3 and vitamin E. It has similar texture and smell as commercialized plain yogurt with a color of bright white yellow and overall sweet taste.
Questionnaire and survey for the swallowing supplement
We assessed oral health-related quality of life using the Geriatric Oral Health Assessment Index (GOHAI) and swallowing quality of life (swal-QoL) questionnaires. The GOHAI is a 12-item questionnaire that consists of three positive and nine negative items for assessing oral health in elderly individuals. Here, participants selected one of five responses to the 12 questions to indicate whether oral discomfort occurred during the previous 3 months [23]. The 6-point scale was adapted to a 3-point scale. The coding of the three positive items was reversed since a high GOHAI score indicates low impairment. As a result, the score of the GOHAI scale ranged from 12 to 36 with a higher total score indicating a higher oral health index [23]. The swal-QoL was developed to assess the quality of life of patients with swallowing disorders [24, 25]. It comprises of 44 questions evaluating 11 QOL domains (burden, eating duration, eating desire, symptom frequency, food selection, communication, fear, mental health, social functioning, sleep, and fatigue). The possible responses are “strongly agree” (1 point), “agree” (2 points), “neutral (3 points), “disagree” (4 points), and “strongly disagree” (5 points). The score for each domain was calculated by adding the points of the responses to its questions with the score being positively associated with the quality of life. After the videofluoroscopic study, the participants underwent a survey and ate the swallowing supplement. The survey assessed “convenience to swallow”; “residual sense after swallowing”; and 6 preference items, including appearance, flavor, taste, texture, overall preference, and purchase intent.
Statistical analysis
Independent t tests were used for between-group comparisons of each demographic variable, swallowing measurement, and questionnaire. Pearson’s correlation coefficient analysis was performed within the patient group to examine the relationships between nutritional status and swallowing function. Statistical analyses were performed using SPSS ver. 21.0 software (IBM Company, Armonk, NY, USA) with the significance level set at P value < 0.05.
Results
Demographics and clinical characteristics
Table 1 presents the demographics, clinical characteristics, and oral conditions of participants in both groups. There was no between-group difference in muscle and fat mass, as well as body mass index. However, there were significantly lower albumin and hemoglobin levels in the PD group than in the control group. Compared with the control group, the PD group had significantly lower cognitive status as measured using the MMSE score. Furthermore, compared with the control group, the PD showed decreased overall dental condition, sensory and motor tongue function, and salivation.
Between-group comparison of swallowing function
Compared with the control group, the PD group had significantly lower total VDS scores and sub-scores regarding the oral stage, including bolus formation, mastication, premature bolus loss, and oral transit time. Furthermore, compared with the control group, the PD group had significantly impaired vallecular residue, pyriform sinus residue, and aspiration and penetration of the pharyngeal stage (Fig. 1). Between-group comparisons of the OTT, PDT, and PTT for the general diet were performed with adjustment for sex and age. Compared with the control group, the PD group had a significantly impaired PDT (P < 0.05). However, there was no significant between-group difference in the mPAS score for 5 food types (Fig. 1). The mean ASHA-NOMS was 5.83 ± 1.12 and 6.72 ± 0.54 in the PD and control groups, respectively, with the between-group difference being significant (data was not shown).
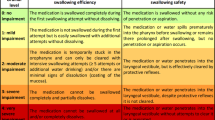
The percentage of subject who showed abnormal findings in the items of videofluoroscopic dysphagia scale (VDS) (upper), swallowing physiology including oral transit time (OTT), pharyngeal delay time (PDT), and pharyngeal transit time (PTT), and modified penetration aspiration scale (mPAS) with commercial yogurt between healthy controls and PD patients
Swallowing supplements in patients with PD
Table 2 shows the comparison of swallowing function using the VFSS between commercialized plain yogurt and swallowing supplement in patients with PD. There was no significant between-diet difference in the mPAS score. However, the PDT and PTT were significantly shorter with the swallowing supplement than with the commercialized plain yogurt (P = 0.000, 0.009, respectively). The OTT showed a tendency to shorten with swallowing supplement; however, there was no significant between-diet difference. The total VDS score was lower with swallowing supplements than with commercialized yogurt. In the VDS sub-score, the pharyngeal wall coating, PTT, and aspiration showed a significant improvement with swallowing supplement (P = 0.000, 0.001, 0.032; respectively).
Survey for the swallowing supplement
All the patients with PD underwent a survey for the newly developed swallowing supplement after finishing the swallowing evaluation. In a preference survey, most patients with PD selected a high score for “easy to swallow” and above-average to good scores for the “pharyngeal residual sense.” Moreover, the preferential survey of the six items, including appearance, flavor, taste, texture, overall preference, and purchase intent (range: 0~4.5) scored an average of ≥ 3. The texture score was the highest (average > 4) followed by the overall preference (average > 3.5) (Fig. 2).
Questionnaire for oral health and swallowing QOL
The total GOHAI scores, which are comprised of 12 sub-items, were significantly lower in the PD group than in the healthy control group (P < 0.000) (Table 3). In the swal-QoL questionnaire, the total score and scores of 8 sub-items, except the “food selection” sub-item, were significantly lower in the PD group than in the control group (Table 4).
Discussion
We found that patients with PD and healthy controls preferred or could tolerate newly developed swallowing supplements compared with commercialized yogurt. Furthermore, about 30% of the included patients with PD presented “symptomless dysphagia,” which was revealed by penetration/aspiration and moderate vallecular residue degree seen in the VFSS. Therefore, “symptomless dysphagia” is prevalent among early-stage patients with PD where there is a potential risk of progressing to symptomatic dysphagia. Kalf et al. [2] reported that a high percentage of early-stage patients with PD without subjective dysphagia presented objective swallowing dysfunctions, including abnormal VFSS findings. Swallowing dysfunction could be involved in the preclinical or early PD stage [26] as a bottom-up progression of α-synuclein pathology according to the Braak hypothesis [27]. However, we could not perform a detailed analysis of this specific patient group and compare it with those without dysphagia in the VFSS. Patients with PD described feeling “something seems to be hanging inside the neck” or “sticky swallowing.” Most of these patients were examined in the department of otorhinolaryngology or pulmonology; however, there were no true pharyngeal or respiratory problems. These patients received more clinical attention and further evaluation using proper swallowing measurement tools was needed.
Dysphagia prevalence in the elderly (presbyphagia) remains unclear; however, it has been estimated to be approximately 15% [28]. PD-related dysphagia is more frequent than dysphagia in elderly person and the oral stage mostly disturbed [1, 11]. The oral phase of swallowing was associated with trouble with swallowing initiation in patients with PD. Compared with the control group, the PD group showed greater disruption bolus formation, mastication and premature bolus loss in the oral phase. These findings could be attributed to impaired oral conditions; decreased tongue sensory and motor function in patients with PD. The oral phase of swallowing is under the voluntary controls of the mouth, tongue, and neck muscles [11]. Therefore, disharmony between the mouth and surrounding muscles caused by bradykinesia and rigidity in patients with PD could have oral effects. This hypokinetic dysphagia has been reported to respond to dopaminergic treatment unlike the other swallowing stage in PD [29].
In addition, dysfunction of the pharyngeal phase, including delayed PDT, as well as increased residual material and aspiration, was observed in the PD group than in the control group. Delayed PDT is indicative of slower triggering of the pharyngeal motor response and laryngeal elevation. We speculated that somatosensory deficits in the pharyngeal wall and a reduced rate of spontaneous swallowing increased the residue in the pyriform sinus [11, 30]. Regarding the dysfunction of the oral and pharyngeal phases, the swallowing reflex is controlled by the swallowing pattern generator (SPG), which is associated with the nucleus tractus solitarius (NTS) [31]. The NTS, which is interconnected with neural circuits, are involved in oral, pharyngeal, and esophageal swallowing stages. The pharyngeal striated muscle is innervated by the nucleus ambiguous; moreover, the dorsal vagal motor nucleus innervates the lower pharynx and esophageal muscles [31, 32]. Therefore, degeneration of the dorsal vagal nucleus could disrupt both the pharyngeal and esophageal phases.
We compared the swallowing function between commercialized yogurt and swallowing supplement in patients with PD to determine whether the swallowing supplement allowed safe swallowing. Subsequently, we assessed factors regarding nutrition, flavor, texture, and convenience with respect to the patient’s needs. We had to consider the various cases of PD-associated dysphagia since it can be caused by PD medication, disease severity, and PD progression. Taken together, it is best to modulate swallowing supplements as individualized therapy; however, this is difficult due to the various characteristics of swallowing supplements, including mass production and commercialization. Various diets for dysphagia have already been commercialized in liquid, gelatin, and powder forms for use in place of food, nutrient, and meal replacement (www.diaphagia-diet.com). However, the development of these dysphagia diets did not involve an objective evaluation of the swallowing function as performed in our study. Furthermore, these diets were developed for general dysphagia regardless of the disease type. The National Dysphagia Diet Task Force redefined the international standardized terminology and definitions for texture-modified foods and liquids for individuals with dysphagia [33]. In addition, it recommended standardized therapies for dysphagia management, including three different levels of food textures and four types of liquids suitable for patients with mild to severe degree dysphagia. The levels for solid foods include ground/pure (level 1), mechanical soft/chopped (level 2), and regular/advanced (level 3) while the four thickness liquid levels are thin, nectar thick, honey-thick, and spoon thick [33]. Our swallowing supplement was similar spoon thick, which was formulated with the Korean dining culture considered where spoons and chopsticks are used. Moreover, we considered the color and texture where the color was bright white yellow and the texture was non-clumpy and soft like pudding; however, it was not sticky. VDS analysis with commercialized yogurt showed that the PD group had more delayed PDT, as well as increased residue and coating around the pharynx, compared with the control group. However, our swallowing supplement significantly shortened the PDT and PTT, as well as improved aspiration and pharyngeal wall coating compared with commercialized yogurt. This indicates that the texture of the swallowing supplement should allow light swallowing based on low surface friction coefficient, as well as moderate viscosity without stickiness. The odor of the swallowing supplement is not a significant factor since hyposmia and anosmia are common early non-motor PD symptoms [34]. The nutrition composition of swallowing supplement is as important as its safety aspects. Since the indication of the swallowing supplement could alter between an own and additive meal depending on its nutritional composition, we developed it as a thickened liquid to allow both uses.
Recently, other than in terms of nutrients, the market of functional food has grown among elderly individuals and according to consumer needs. Functional food was shown to have physiological benefits and to decrease the risk of chronic and neurodegenerative diseases, including PD [35]. Moreover, using nutraceuticals derived from natural sources has been reported to support the beneficial roles in PD prevention as antioxidants, anti-apoptosis, and mitochondrial homeostasis [36]. However, the nutrients of our swallowing supplement lacked protective and disease-modifying effects; rather, it was composed of the daily recommended essential nutrition for elderly individuals. Subsequent addition of the features of functional food and nutraceuticals to our swallowing supplement could improve its prevention of neurodegenerative disease and attenuation of PD-related health problems. Our swallowing supplement has good portability given the possibility of disposable individual packaging.
Initially, it is important to decide when patients with PD use swallowing supplements. Self-awareness of dysarthria progression or the use of a self-report questionnaire for patients with PD provided the initial dysphagia clues. The swallowing disturbance questionnaire (SDQ) and non-motor symptoms questionnaire (NMSQ) are generally used for PD-related dysphagia [37, 38]. However, it is difficult to administer the SDQ to participants unaware of swallowing disturbances even though it is an accurate and sensitive tool for identifying swallowing disturbance [37]. In addition, SDQ scores are affected by medication on and off states, as well as mood symptoms, including anxiety in patients with PD. The NMSQ is a useful clinical tool for screening non-motor problems; however, dysphagia is a PD motor symptom. Consequently, we used the GOHAI, which is regarded as the most comprehensive assessment tool for measuring oral health-related quality of life [23]. Furthermore, the GOHAI evaluates the highly prevalent dental diseases that affect swallowing in elderly people [23]. In addition, the swal-QoL specifically evaluates the impact caused by changes in quality of life for swallowing [25]. With respect to quality of life, it is useful to differentiate swallowing in healthy adults with dysphagia from that involving various diseases [39]. We observed that patients with PD obtained lower scores in all domains of the swal-QoL than healthy controls. Consequently, the burden for swallowing was high in patients with PD, which resulted in a reduced swal-QoL. To address the possible inconsistency between subjective awareness and objective dysphagia measurement, we performed confirmation VFSS analysis [40]. The VFSS is a widely used tool for objectively evaluating swallowing function and allowing visualization of the structure and dynamics of the swallowing process. We quantitatively measured functional dysphagia through video-fluoroscopy, which could comprehensively reflect swallowing functions.
PD-related dysphagia can be predicted by various clinical indicators, including the H&Y stage, body mass index < 20 kg/m2, drooling, dysarthria, cognitive impairment, and gait disturbance [1, 8, 9, 41]. The advanced PD stage involves more dysphagia symptoms with high levodopa treatment not improving dysphagia symptoms. This refutes the suggestion that the non-dopaminergic pathway is involved in PD-related dysphagia [10]. The non-dopaminergic pathways, including the central cholinergic system, are involved in dysphagia, cognition, and gait difficulty. Brainstem cholinergic systems have been implicated in the pharyngeal and esophageal stages of swallowing and in generating rhythmic or propulsive esophageal motility [42]. Taken together, the swallowing supplements decreased the aspiration frequency and reduced aspiration pneumonia. The optimal degrees of viscous and elastic components of texture-modified food have been suggested to affect the resulting findings [43].
Our findings should be carefully considered. First, our sample size was insufficient for comparing the advantages of our swallowing supplement. Second, there were no significant between-group differences in the swallow physiology of general diets except PDT. This could be attributed to differences in the PD stage. Third, there was a significant between-group difference in cognitive status, which could have a confounding effect on swallowing dysfunction since the cholinergic pathway affects dysphagia in patients with PD [44].
In conclusion, we found that several patients with PD presented “symptomless dysphagia” upon VFSS evaluation. In addition, our swallowing supplement was easier to swallow than a general diet and tolerable to patients with PD. This elderly friendly swallowing supplement could contribute toward reducing the chance of aspiration and dysphagia complications in patients with PD.
References
Suttrup I, Warnecke T (2016) Dysphagia in Parkinson’s disease. Dysphagia 31:24–32
Kalf JG, de Swart BJ, Bloem BR, Munneke M (2012) Prevalence of oropharyngeal dysphagia in Parkinson’s disease: a meta-analysis. Parkinsonism Relat Disord 18:311–315
Kim JS, Youn J, Suh MK, Kim TE, Chin J, Park S, Cho JW (2015) Cognitive and motor aspects of Parkinson’s disease associated with dysphagia. Can J Neurol Sci 42:395–400
Williams-Gray CH, Mason SL, Evans JR, Foltynie T, Brayne C, Robbins TW, Barker RA (2013) The CamPaIGN study of Parkinson’s disease: 10-year outlook in an incident population-based cohort. J Neurol Neurosurg Psychiatry 84:1258–1264
Suntrup S, Teismann I, Bejer J, Suttrup I, Winkels M, Mehler D, Pantev C, Dziewas R, Warnecke T (2013) Evidence for adaptive cortical changes in swallowing in Parkinson’s disease. Brain 136:726–738
Regan J, Walshe M, Tobin WO (2010) Immediate effects of thermal-tactile stimulation on timing of swallow in idiopathic Parkinson’s disease. Dysphagia 25:207–215
Han M, Ohnishi H, Nonaka M, Yamauchi R, Hozuki T, Hayashi T, Saitoh M, Hisahara S, Imai T, Shimohama S, Mori M (2011) Relationship between dysphagia and depressive states in patients with Parkinson’s disease. Parkinsonism Relat Disord 17:437–439
Menezes C, Melo A (2009) Does levodopa improve swallowing dysfunction in Parkinson’s disease patients? J Clin Pharm Ther 34:673–676
Troche MS, Brandimore AE, Foote KD, Okun MS (2013) Swallowing and deep brain stimulation in Parkinson’s disease: a systematic review. Parkinsonism Relat Disord 19:783–788
Przuntek H (2000) Non-dopaminergic therapy in Parkinson’s disease. J Neurol 247 Suppl 2:II 19–II 24
Potulska A, Friedman A, Królicki L, Spychala A (2003) Swallowing disorders in Parkinson’s disease. Parkinsonism Relat Disord 9:349–353
Ali GN, Wallace KL, Schwartz R, DeCarle DJ, Zagami AS, Cook IJ (1996) Mechanisms of oral-pharyngeal dysphagia in patients with Parkinson’s disease. Gastroenterology 110:383–392
Ding X, Gao J, Xie C, Xiong B, Wu S, Cen Z, Lou Y, Lou D, Xie F, Luo W (2018) Prevalence and clinical correlation of dysphagia in Parkinson disease: a study on Chinese patients. Eur J Clin Nutr 72:82–86
van Hooren MR, Baijens LW, Voskuilen S, Oosterloo M, Kremer B (2014) Treatment effects for dysphagia in Parkinson’s disease: a systematic review. Parkinsonism Relat Disord 20:800–807
Maier F, Prigatano GP (2017) Impaired self-awareness of motor disturbances in Parkinson’s disease. Arch Clin Neuropsychol 32:802–809
Namasivayam-MacDonald AM, Riquelme LF (2019) Presbyphagia to dysphagia: multiple perspectives and strategies for quality care of older adults. Semin Speech Lang 40:227–242
Braun T, Juenemann M, Viard M, Meyer M, Fuest S, Reuter I, Kaps M, Prosiegel M et al (2018) What is the value of fibre-endoscopic evaluation of swallowing (FEES) in neurological patients? A cross-sectional hospital-based registry study. BMJ Open 8:e019016
Lafer M, Achlatis S, Lazarus C, Fang Y, Branski RC, Amin MR (2013) Temporal measurements of deglutition in dynamic magnetic resonance imaging versus videofluoroscopy. Ann Otol Rhinol Laryngol 122:748–753
Han TR, Paik NJ, Park JW, Kwon BS (2008) The prediction of persistent dysphagia beyond six months after stroke. Dysphagia 23:59–64
Mullen R, Schooling T (2010) The national outcomes measurement system for pediatric speech-language pathology. Lang Speech Hear Serv Sch 41:44–60
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL (1996) A penetration-aspiration scale. Dysphagia 11:93–98
Cichero JA, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, Duivestein J, Kayashita J (2017) Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: The IDDSI framework. Dysphagia 32:293–314
Atchison KA, Dolan TA (1990) Development of the Geriatric Oral Health Assessment Index. J Dent Educ 54:680–687
McHorney CA, Robbins J, Lomax K, Rosenbek JC, Chignell K, Kramer KE, Bricker DE (2002) The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia 17:97–114
Leow LP, Huckabee ML, Anderson T, Beckert L (2010) The impact of dysphagia on quality of life in ageing and Parkinson’s disease as measured by the swallowing quality of life (SWAL-QOL) questionnaire. Dysphagia 25:216–220
Pflug C, Bihler M, Emich K, Niessen A, Nienstedt JC, Flügel T, Koseki JC, Plaetke R (2018) Critical dysphagia is common in Parkinson disease and occurs even in early stages: a prospective cohort study. Dysphagia 33:41–50
Braak H, Del Tredici K, Rüb U, Vos RA, Jansen Steur EA, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Sura L, Madhavan A, Carnaby G, Crary MA (2012) Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging 7:287–298
Hunter PC, Crameri J, Austin S, Woodward MC, Hughes AJ (1997) Response of parkinsonian swallowing dysfunction to dopaminergic stimulation. J Neurol Neurosurg Psychiatry 63:579–583
Mu L, Sobotka S, Chen J, Su H, Sanders I, Adler CH, Shill HA, Caviness JN (2012) Altered pharyngeal muscles in Parkinson disease. J Neuropathol Exp Neurol 71:520–530
Jean A (2001) Brain stem control of swallowing: neuronal network and cellular mechanisms. Physiol Rev 81:929–969
Bao X, Wiedner EB, Altschuler SM (1995) Transsynaptic localization of pharyngeal premotor neurons in rat. Brain Res 696:246–249
Cichero JA, Steele C, Duivestein J, Clavé P, Chen J, Kayashita J, Dantas R, Lecko C (2013) The need for international terminology and definitions for texture-modified foods and thickened liquids used in dysphagia management: foundations of a global initiative. Curr Phys Med Rehabil Rep 1:280–291
Fullard ME, Morley JF, Duda JE (2017) Olfactory dysfunction as an early biomarker in Parkinson’s disease. Neurosci Bull 33:515–525
Vella MN, Stratton LM, Sheeshka J, Duncan AM (2014) Functional food awareness and perceptions in relation to information sources in older adults. Nutr J 13:44
Cencic A, Chingwaru W (2010) The role of functional foods, nutraceuticals, and food supplements in intestinal health. Nutrients 2:611–625
Manor Y, Giladi N, Cohen A, Fliss DM, Cohen JT (2007) Validation of a swallowing disturbance questionnaire for detecting dysphagia in patients with Parkinson’s disease. Mov Disord 22:1917–1921
Romenets SR, Wolfson C, Galatas C, Pelletier A, Altman R, Wadup L, Postuma RB (2012) Validation of the non-motor symptoms questionnaire (NMS-Quest). Parkinsonism Relat Disord 18:54–58
Carneiro D, das Graças Wanderley de Sales Coriolano M, Belo LR, de Marcos Rabelo AR, Asano AG, Lins OG (2014) Quality of life related to swallowing in Parkinson’s disease. Dysphagia 29:578–582
Ertekin C (2014) Electrophysiological evaluation of oropharyngeal dysphagia in Parkinson’s disease. J Mov Disord 7:31–56
Lam K, Lam FK, Lau KK, Chan YK, Kan EY, Woo J, Wong FK, Ko A (2007) Simple clinical tests may predict severe oropharyngeal dysphagia in Parkinson’s disease. Mov Disord 22:640–644
Grinberg LT, Rueb U, Alho AT, Heinsen H (2010) Brainstem pathology and non-motor symptoms in PD. J Neurol Sci 289:81–88
Sukkar SG, Maggi N, Travalca Cupillo B, Ruggiero C (2018) Optimizing texture modified foods for oro-pharyngeal dysphagia: a difficult but possible target? Front Nutr 5:68
Lee KD, Koo JH, Song SH, Jo KD, Lee MK, Jang W (2015) Central cholinergic dysfunction could be associated with oropharyngeal dysphagia in early Parkinson’s disease. J Neural Transm (Vienna) 122:1553–1561
Acknowledgments
The authors gratefully acknowledge the members of the Division of Neurology, Department of Rehabilitation, Chungnam National University College of Medicine for their assistance and suggestions.
Funding
This study was supported by a grant from the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (2015R1C1A1A01055923), Korean Health Technology R&D Project (HI10C2020, HI3C1990), and Ministry of Health & Welfare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Oh, E., Jee, S., Kim, B.K. et al. A new swallowing supplement for dysphagia in patients with Parkinson’s disease. Neurol Sci 42, 1949–1958 (2021). https://doi.org/10.1007/s10072-020-04730-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04730-w