Abstract
As we continue to understand more about the complex mechanism of growth, a plethora of novel therapies have recently been developed that aim to address barriers and optimize efficacy. This review aims to explore these novel therapies and provide a succinct review based on the latest clinical studies in order to introduce clinicians to therapies that will soon constitute the future in the field of short stature.
Conclusion: The review focuses on long-acting growth hormone formulations, a novel growth hormone oral secretagogue, novel treatments for children with achondroplasia, and targeted therapies for rare forms of skeletal dysplasias.
What is Known: • Recombinant human growth hormone has been the mainstay of treatment for children with short stature for years. • Such therapy is not always effective based on the underlying diagnosis (e.g achondroplasia, Turner syndrome). Compliance with daily injections is challenging and can directly affect efficacy. | |
What is New: • Recent development of long-acting growth hormone regimens and oral secretagogues can overcome some of these barriers, however several limitations need to be taken into consideration. • Newer therapies for achondroplasia, and other rare forms of skeletal dysplasias introduce us to a new era of targeted therapies for children with short stature. Clinicians ought to be aware of pitfalls and caveats before introducing these novel therapies to every day practice. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recombinant human growth hormone (GH) has been the mainstay of treatment for children with short stature for decades. Since it first became available in 1985, it has been used in millions of children with short stature for a variety of indications. However, this therapy comes with various limitations. One of the major caveats to using GH over the years is that in many instances, it is used for indications where the primary growth defect is not attributable to GH deficiency, such as Turner Syndrome or Noonan Syndrome. In these cases, GH is used as a non-specific growth promoting agent due to the absence of alternative targeted treatments. Additionally, the need for daily injections to achieve steady state and maximum efficacy often creates a significant barrier to families and frequently compromises adherence. As we have come to better understand the complex mechanisms of growth in the recent years, there has been a recent rise in development of novel therapies for short stature that aim to enhance growth in more targeted ways as opposed to purely maximizing levels of GH. In an effort to increase patient adherence, simplify drug delivery, and ease the burden of daily injections, several new medications with longer half-lives have been recently developed that can have similar outcomes with weekly instead of daily injections. This review article aims to explore these novel therapeutic advances in growth disorders and provide a summary of the major newer drug classes in the field of growth.
Methods
We conducted a thorough search of the literature on novel therapies for short stature in children. Our search was mainly focused on the electronic databases of PubMed, using the keywords: “GH”, “weekly GH”, “growth in Achondroplasia”, “Vosoritide”, “trans-con CNP”, “infigratinib”, “LUM201”, “Burosumab”, “carbamazepine”, and “Asfotase alfa”. We attempted to identify the most relevant studies published in the last 5 to 10 years. The bibliographies of related articles were also reviewed to identify other relevant references for inclusion in our study. Additionally, we reviewed data from ongoing clinical trials that were published directly at the pharmaceutical’s webpages and have not yet been published in peer-reviewed medical literature.
Results
Long acting GH (LAGH) formulations
Since therapy with recombinant human GH became (rhGH) readily available in the 1980s, it has revolutionized the field of growth and has shown great benefits in most cases. However, multiple studies have shown that commitment to daily injections poses a major barrier to long-term adherence resulting in compromised outcomes with suboptimal linear growth [1, 2]. This is particularly important when it comes to treating children with growth disorders as long-term commitment to therapy is required, and often times, compliance worsens over time. Several treatment burden questionnaires have been developed, highlighting these limitations [3], and the need for alternative regimens. In that light, long-acting formulations have been developed and recently approved hoping to address these concerns.
Somatrogon (MOD40-23, Ngenla) is one of the long-acting rhGH formulations that consists of the same amino acid sequence as rhGH with the addition of the C-terminal peptide (CTP). CTP is derived from human chorionic gonadotropin, and it was previously used to create long-acting follicular stimulating hormone (FSH) and erythropoietin formulations with great success [4, 5]. Somatrogon was first studied in adults with GH deficiency and was shown to have a very favorable safety profile while maintaining insulin-like growth factor-1 (IGF-1) levels within the normal range [6]. Data from the phase 2 clinical trial in a pediatric population showed a dose dependent effect of somatrogon when compared to daily somatropin, with a dose of 0.66 mg/kg/week demonstrating similar efficacy to daily rhGH administration. This dose elicited similar mean height velocity (HV) and gain in height SDS while maintaining an acceptable safety profile [7]. Subsequently, a 12-month open-label, multicenter, randomized, active-controlled, parallel group phase 3 study was published as a non-inferiority study to daily rhGH [8]. This study involved 224 pre-pubertal children that were all treated under the diagnosis of GH deficiency and had not been previously exposed to GH therapy. There was 1:1 randomization to receive somatrogon at a dose of 0.66 mg/kg/week or somatropin 0.034 mg/kg/day for 12 months, followed by an open-label extension on somatrogon. Inclusion criteria included an annualized HV below the 25th percentile, IGF-1 values ≤ −1 SD, and a confirmed diagnosis of GH deficiency based on stimulation testing as opposed to an absolute height cut-off. GH deficiency was confirmed after completion of 2 different growth hormone stimulation tests with the cut-off for failure set as peak GH ≤ 10 ng/mL. In this study, the first-year HV in the weekly somatrogon group was found to be non-inferior to daily somatrogon, regardless of age, sex, or peak GH levels. Mean annual HV was 10.1 cm/year in the somatrogon vs 9.78 cm/year in the somatropin group (95% CI for the difference: −0.24, 0.89). There was also no difference in degree of bone maturation. The incidence of adverse events was similar in the two groups; however, treatment-emergent AEs (TEAE) for injection site erythema, pruritus and pain were > 5% more common in the somatrogon group (39.4% vs 25.25), while one subject had to withdraw from the study due to injection site induration. Mean IGF-1 levels were also monitored, and 26 subjects were found to have IGF-1 levels > 2 SD in the somatrogon group vs 3 in the somatotropin group. However, in the majority of the cases, that was due to inappropriate timing of sample collection, within the first 2–3 days of administering the dose which represents the peak IGF-1 levels. As we will discuss later, this is a an extremely important point of consideration when it comes to monitoring drug and IGF-1 levels in patients receiving long-acting GH formulations. Nevertheless, a total of 12 patients did require dose reduction for IGF-1 SD levels > 2. There were no differences in metabolic effects between the two medications, and although somatrogon was associated with a higher incidence of anti-drug antibodies (ADA), this was not clinically significant in terms of drug safety or efficacy (i.e., growth rate). There was no difference in adherence between the two groups, although this is in the setting of a closely monitored clinical trial. Tolerability was very high in both groups, which is also supported by > 95% enrollment in the open-label enrollment after completion of the 12-month period [9].
Another long-acting GH molecule that has also been recently studied is lonapegsomatropin (Skytrofa). Lonapegsomatropin uses a different mechanism than somatrogon to prolong half-life by attaching a methoxy polyethylene glycol carrier via a cleavable linker to intact GH [10]. In a study of 161 GH-naïve, pre-pubertal children with GH deficiency, the subjects were randomized 1:2 to received standard of care daily somatropin (0.34 mg/kg/day) vs weekly lonapegsomatropin (0.24 mg/kg/week). Similar inclusion criteria were used as above, including peak GH ≤ 10 on 2 stimulation tests; however, in this study, height SD ≤ −2 and delayed bone age by ≥ 6 months were required. Patients were followed for a year. This study confirmed non-inferiority and additionally showed statistical superiority of lonapegsomatropin over somatropin in HV, with mean annualized HV of 11.2 cm/year in the lonapegsomatropin group vs 10.3 cm/year in the somatropin group (p = 0.009). The greater HV in the lonapegsomatropin arm was confirmed in all subgroup analyses and became evident after week 26. The estimated average IGF-1 SD in the lonapegsomatropin group was higher than the somatropin group (+0.72 vs −0.02, respectively) and reached the target range of 0–2 SD faster. In this study, they used estimated average IGF-1 SD levels to assess overall systemic exposure which was defined based on non-linear mixed effect population pharmacodynamic modeling from the phase 2 study [10]. IGF-1 SD > 2 was rarely exceeded in both groups; however, it was more common in lonapegsomatropin group (7.6% vs 3.65). One subject also required dose reduction for asymptomatic SD > 3. Both groups had very similar safety and tolerability profiles. Degree of bone age advancement, anti-hGH antibody production, and metabolic effects were the same, too. Nevertheless, a single obese patient with GH deficiency was recently reported with severe acute hyperglycemia after starting lonapegsomatropin. Hyperglycemia correlated with the anticipated peak GH level times, and it has been proposed that perhaps lower starting doses should be considered for patients with pre-disposition to diabetes mellitus or metabolic syndrome [11].
Somapacitan (Sogroya) is another LAGH regimen that is rhGH with a single point mutation which is attached to a small terminal fatty acid with non-covalent albumin-biding properties. Binding to albumin delays elimination therefore increasing half-life. Data from the randomized, open-label phase 3 trial were recently published [12]. They enrolled 200 pre-pubertal, GH naïve children with GHD, height SD < −2 SD, IGF-1 < −1 SD, and HV below the 25th percentile. They were randomized 2:1 to receive somapacitan 0.16 mg/kg/week vs daily GH 0.034 mg/kg/day for a year, followed by a 3-year safety extension during which all subjects were on somapacitan. They used peak to trough IGF-1 levels and population pharmacokinetics/pharmacodynamics (PK/PD) modeling to derive a weekly IGF-1 average. HV at the end of the study was very similar in both groups (11.2 cm/year in somapacitan vs 11.7 cm/year for somatropin). Interestingly, it was thought that somapacitan may lead to a higher HV based on the phase 2 data (12.9 cm/year vs 11.4 cm/year), although this difference was not statistically significant at the time [13] and similar HV at years 2, 3, and 4 [12] overall continue to affirm non-inferiority. Both groups had very similar mean IGF-1 SD values with no statistically significant difference for change of baseline to week 52. Peak IGF-1 levels were found to be ≥ 2 SD more frequently in the somapacitan group (27.3% vs 0.4%); however, no such difference was noted when measuring trough levels of the weekly regimen. Frequency of consecutive measurements ≥ 2 SD was similar in both groups (3.8% vs 2.9%), and only a single participant in both groups had to have dose reduction for that reason (0.8% somapacitan vs 1.4% somatropin). These cases were not associated with higher incidence of adverse events. Bone age advancement, metabolic profiles, and neutralizing antibodies were again similar in both groups. Importantly, this study also compared treatment burden questionnaires for both patients and caregivers that favored weekly somapacitan in all domains. Interestingly though, this difference was not as pronounced at year 4, based on data recently published from the phase 2 trial, although based on a much smaller study population of 50 patients [12, 13]. Safety profiles were again reported to be similar at the 4-year period.
LAGH regimens were first developed to address issues with patient’s satisfaction and poor compliance that also inevitably affect outcomes. However, in all these studies, the adherence rates were very similar (which are not unexpected in a controlled clinical study setting), yet in some cases, they proved superiority in outcomes and HV, indicating that there might be additional benefits to LAGH other than pure compliance. Authors have proposed that this is due to increased engagement of the GH receptors at the level of the growth plates. This is also supported by higher mean IGF-1 levels, often identified in the LAGH products, which can suggest preservation of biological balance between direct GH and indirect IGF-1 effect [14,15,16]. However, this has not come without concerns. Apart from being a surrogate for efficacy, IGF-1 has been used over the years to monitor safety too. Since the effect of LAGH at the growth plate is not fully known or hard to quantify, standard clinical guidance over the years has recommended using circulating IGF-1 as a proxy for safety with the goal of maintaining IGF-1 SD range between −2 and +2 and avoiding persistent supraphysiologic elevation [17, 18]. Of note though, transient spikes beyond this point have not been shown to raise a safety concern [19, 20]. This is particularly important when it comes to monitoring these new LAGH agents since their pharmacokinetics are completely different than the classic daily rhGH that most clinicians are familiar using and monitoring. Once-weekly injections are expected to cause peaks and troughs over the weekly dosing interval. One must keep this in mind when timing blood draws and using results to make dose adjustments [18]. All of the above LAGH exhibit similar patterns of pharmacokinetics with peak GH value occurring about 12 h and peak IGF-1 at 48 h post-dose. Mean IGF-1 and IGF-1 SD is achieved more closely at approximately 96 h (4 days) post-dose although there is interindividual variability, therefore clinicians need to be aware of this natural course to time labs drawn accordingly [10, 12, 21].
Although it is important to understand these timeframes, we acknowledge that this is not necessarily practical in real-world practice. Additionally, it is believed that the average IGF-1 level is more clinically relevant to represent overall exposure rather than isolated measurements. For that reason, Zhegning et al. recently published a pharmacokinetic/pharmacodynamic (PK/PD)-generated prediction model based on data from two randomized open-label trials with lonapegsomatropin to estimate mean IGF-1 value and mean IGF-1 SD value based on a random measurement [21]. This study provided prediction error models and means or ratios that can be used to calculate average IGF-1 and IGF-1 SD, respectively. It also confirmed that, generally, the prediction errors are at the minimum when samples are taken between days 2.5 and 5, whereas the largest errors occur closer to days 0 and 7. The sampling time for IGF-1 to coincide as much as possible with average levels is around day 4.5, with peak being at 2 to 2.5 days.
New therapies in achondroplasia
Achondroplasia is an autosomal dominant genetic disorder that is caused by a gain of function mutation in the fibroblast growth factor receptor 3 (FGFR3). FGFR3 is one of the major receptors that negatively regulates growth by inhibiting production of extracellular matrix, decreasing chondrocyte proliferation while increasing hypertrophic differentiation. In achondroplasia, this increased FGFR3 signaling leads to disruption of fibroblast ossification with distinct clinical features of short stature with rhizomelia (short proximal long bones), relative macrocephaly, distinct facial features (flat nasal bridge, midface hypoplasia), and a normal torso length [22]. In addition to short stature, achondroplasia can lead to a variety of medical complications including foramen magnum stenosis, hydrocephalus, obstructive sleep apnea, hydrocephalus, limb bowing, and spinal stenosis. Limb lengthening was one of the first interventions ever developed to increase height in patients with achondroplasia; however, this can often have significant complications and even increase disease burden. In recent years, newer medications have been developed that can instead augment growth via a targeted precision medication therapy [23]. The first class of these medications for children with achondroplasia is analogs of C-type natriuretic peptide (CNP). CNP is an important peptide involved in the MAPK growth cascade (mitogen-activated growth cascade). In brief, CNP acts through its receptor at the chondrocyte cell membrane to convert GTP to cGMP, eventually resulting in downstream inhibition of the MAPK pathway, thereby promoting the arrested chondrocyte differentiation and proliferation. Two major analogs in this category include vosoritide and TransCon CNP.
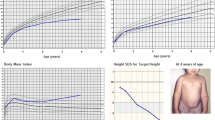
Vosoritide is a small CNP analog with a longer half-life than endogenous CNP due to a modification which makes it resistant to degradation. Vosoritide is administered via daily subcutaneous injection. Animal studies in wild-type mice and monkeys as well as knock-in mice with FGFR3 activating mutations mimicking achondroplasia showed increased long bone growth as well as improvement in phenotypic findings of skeletal dysplasia [24, 25]. This eventually led to a phase 2 study in 35 children with achondroplasia to explore optimum dosing as well as its safety profile [26]. Results from this study revealed that higher doses (15 and 30 mcg/kg/day) achieved the maximum response in HV, while maintaining a benign safety profile (most commonly reported adverse events were skin irritation and transient drop in blood pressure). Following this, a phase 3, randomized double-blind placebo control trial was conducted that included 121 children with achondroplasia (ages 5–18 years old) with 1:1 randomization to receive vosoritide 15 mcg/kg/day vs placebo. The study compared annualized HV after 52 weeks of treatment [27, 28]. Results showed a 1.57 cm/year height difference between the two groups (95% CI [1.22–1.93], two-sided p < 0.0001). There were no differences in adverse events reported between the two groups, and no drug-related serious adverse events were reported. The 2-year mark in the open-label, phase 3 extension study also confirmed similar results. Fifty-eight participants from the vosoritide group that remained on the study showed sustained HV at the end of the 2-year extension period, while the 61 participants from the placebo group that crossed over to vosoritide treatment exhibited an increased annual HV that resembled the initial effect noticed in the phase 3 trial. Height Z-scores increased by +0.44 (95% CI: 0.25 to 0.63), and interestingly, there was also a statistically significant decrease in upper to lower body segment ratio (−0.55, 95% CI: −0.09 to −0.01) at 2 years indicating a change not only in growth but also in the body disproportion due to the underlying skeletal dysplasia. Vosoritide is now approved for use in children with achondroplasia in the USA, Europe, Australia, and parts of Asia.
The second CNP agent, that is currently under investigation, is TransCon CNP, which consists of a CNP analog that is conjugated to a polyethylene glycol carrier module as a cleavable linker and therefore prolongs this action of CNP by inhibiting its degradation by neutral-endopeptidase proteolysis. This is the same technology used to make lonapegsomatropin. Initial studies in mice and monkeys showed prolonged CNP half-life (from 2–3 min, up to 90 h post-TransCon CNP), with increased growth. Mouse models with achondroplasia also showed increased growth, and results were comparable to the vosoritide studies [23, 27]. Safety and pharmacodynamic data from the phase 1 clinical trial by Breinholt et al. showed that TransCon CNP was very well tolerated with no serious adverse events or treatment discontinuation [28]. The pharmacokinetic analysis indicated that once a week dosing would be appropriate with a sustained and satisfactory increase in CNP levels in both urine and plasma. There is now an ongoing phase 2 double-blind, randomized, placebo-controlled trial in pre-pubertal children with achondroplasia, aiming to obtain more insight in pharmacokinetics, minimum effective dose, and safety profile. Preliminary results presented by the company showed an increase in annualized HV at the 100 µg/kg/week dose when compared to placebo (5.42 vs 4.35 cm/year, p = 0.02). The medication was well tolerated with no discontinuation or treatment-related serious adverse events [29].
Infigratinib is an oral tyrosine kinase inhibitor (TKI) specific for FGFR1-3 that counteracts FGFR3 hyperactivity by inhibiting its phosphorylation and therefore downstream signaling. It has recently been studied in mouse models with achondroplasia and showed increased growth which was also more pronounced compared to vosoritide-treated mice [30]. There is currently an ongoing phase 2, open-label clinical trial aiming to investigate the safety profile and pharmacokinetics of infigratinib in children with achondroplasia [31]. Preliminary results were presented at the Endocrine Society annual meeting and report a mean increase of annualized HV that reached 3.38 cm/year at the 0.25 mg/kg/day dose. No major AE have been reported to date [32].
LUM-201
Ibutamoren, also known as LUM-201, is an oral GH secretagogue that is designed to increase endogenous GH release and pulsatility. It acts by stimulating ghrelin receptors, thereby increasing GH releasing hormone (GHRH) as well as suppressing somatostatin secretion in the hypothalamus. One of its major advantages is that it is an oral medication as compared to subcutaneous growth hormone. When it was first studied in a healthy adult population, results were very promising [33]; however, when applied to pediatric population with GH deficiency, only a small subset of patients had a considerable response [34].
In hindsight, it is thought that the study population selection for this initial study was suboptimal as it included patient populations that would have been expected to fail, e.g., hypothalamic-pituitary disorders that lack the ability to increase hypothalamic GHRH secretion. However, a post-hoc analysis was later performed in an effort to identify characteristics of the patients that did respond. This analysis led to the creation of a pre-treatment model designed to help predict those with the potential to respond to treatment. This model is based on the individual patient’s peak GH response after a single LUM-201 dose as well as on their baseline IGF-1 level. The model is called a Predictive Enrichment Marker (PEM) [35]. Based on their results, maximum sensitivity (0.92), specificity (0.5), and predictive accuracy (0.71) of the PEM test were achieved for subjects that had a peak GH level of ≥ 5 ng/ml, which further increased when also taking into account baseline IGF-1 levels, with the cut-off being 30 ng/ml. PEM-positive subjects were taller at baseline, had less delayed bone ages with higher IGF-1, and overall deemed to have a more mild to moderate GHD compared to PEM-negative subjects. In PEM-positive individuals, the post-hoc analysis showed that LUM-201 was statistically similar to rhGH in terms of annualized HV. Additionally, there seems to be a dose dependent effect; therefore, it was speculated that higher doses than the 0.8 mg/kg/day used in the initial study may lead to improved outcomes with LUM-201. No major adverse events were reported apart from increased appetite that can also be considered as beneficial during catch up growth. Lastly, it has been suggested that LUM-201 can possibly be used as an additional stimulator when performing GH stimulation test as it elicits a more robust peak when compared to the standard regimens (arginine, glucagon, L-dopa) and with much fewer side effects [35, 36]. Additional research is needed on the utility of LUM-201 as a diagnostic agent.
There is currently an open-label phase 2 clinical trial investigating the effects of LUM-201 at higher than the previously studied doses (0.8–3.2 mg/kg/day vs 0.4–0.8 mg/kg/day used in initial studies) in treatment-naive pre-pubertal children with mild growth hormone deficiency. Preliminary data suggest that there is no significant difference in the outcomes between 1.6 and 3.2 mg/kg/day groups, and both doses helped to increase GH and IGF-1 amplitude as well as HV. The preliminary data show HV in the range that is expected when compared to historically treated GH patients with similar clinical characteristics [37].
Burosumab
Understanding the underlying disease pathophysiology led to development of a targeted therapy for X-linked hypophosphatemia (XLH), a rare skeletal disorder due to variants in the phosphate-regulating endopeptidase homologue on the X chromosome (PHEX). Deficiency of PHEX causes an increase in fibroblast growth factor 23 (FGF23) leading to chronic hypophosphatemia by renal phosphate wasting and decreased in 1,25-dihydroxyvitamin D (1,25(OH)2D) leading to decreased intestinal phosphate absorption and renal phosphate reabsorption. In children, XLH causes rickets, skeletal deformities, impaired growth, muscle weakness, and dental abscess. Conventional treatment for children with XLH includes high doses of oral phosphate multiple times a day and active vitamin D (calcitriol); however, complications such as hyperparathyroidism and nephrocalcinosis may persist. There is also known poor tolerance and compliance of conventional treatment, but even those with coherence, there has been shown linear growth failure in 25–40% of children [38, 39]. Burosumab is a fully human monoclonal antibody, given via subcutaneous injection every 2 weeks, that targets excess FGF23 activity of XLH. This leads to increased renal phosphate reabsorption, intestinal phosphate absorption, and 1,25(OH)2D activity. The clinical trials showed improved outcome in rickets, lower limb deformities, and growth [40]. In the phase 3 study of burosumab vs conventional treatment, linear growth was modestly increased after 64 weeks with standing height Z-score difference of 0.14(p = 0.05) [41]. Burosumab was first approved for clinical use in 2018, since then, clinical experiences have reported that there was also reduction in number of abscesses, reduce risk of fractures, and improvement in pain [38, 42].
Asfotase alfa
Hypophosphatasia (HPP) is a rare metabolic skeletal disorder caused by tissue-non-specific alkaline phosphatase (TNSALP) gene leading to low serum alkaline phosphatase (ALP) activity. Low TNSALP leads to extracellular accumulation of mainly its substrates inorganic pyrophosphate (PPi) and pyridoxal 5′-phosphate (PLP). Increased extracellular PPi impairs skeletal mineralization. The clinical spectrum varies for autosomal dominant and recessive forms. A novel enzyme replacement therapy, asfotase alfa, specifically targets mineralized tissues in HPP [43]. Manifestations in the infantile and childhood HPP include poor growth and skeletal deformities. Asfotase alfa showed generalized increase in height/weight Z-score in the phase 2 open-label study [44]. The most common side effect has been injection site reactions, including erythema, hypertrophy, and atrophy with minimal severe adverse events and no deaths [45]. It is approved for use in the USA, Canada, and European Union for childhood onset (perinatal-, infantile-, and juvenile-onset) hypophosphatasia.
Carbamazepine for metaphyseal chondrodysplasia Schmid type
With increasing knowledge of the underlying pathophysiology of skeletal dysplasias, a number of efforts are underway to develop precision medicines targeted at the specific underlying defect. One approach is to attempt to repurpose existing drugs as opposed to developing completely novel therapies. Mutations in type X collagen cause a short-limbed dwarfism called metaphyseal chondrodysplasia type Schmid (MCDS). In this disease process, mutant collagen X proteins become misfolded and accumulate within the hypertrophic chondrocytes, usually due to a missense mutation, causing growth plate disruption. This ultimately alters its differentiation programming causing decreased VEGF and increased hypertrophic zone width with growth arrest. Carbamazepine (CBZ) is a medication classically used as anti-convulsant that has an autophagy-stimulating effect and has been used in the past in other diseases, e.g., to prevent liver cirrhosis in patients with alpha1-antitrypsin deficiency due to misfolded protein accumulation [46]. Similarly, it has been proposed that CBZ can help reduce endoplasmic reticulum (ER) stress in MCDS via promoting intracellular degradation through autophagy and/or proteasomal degradation depending of the causative mutation and therefore improve growth [47]. Studies in mice with Col10a1 p.N617K mutation showed that CBZ treatment can be beneficial in limiting chondrocyte hypertrophy and reducing ER stress with lower stress markers (Bip and Atf4), thus overall promoting growth. Mice that received treatment achieved 1.25 to 1.44-fold increase in limb length as well as improved features of skeletal dysplasia on histological examination. Similarly, encouraging data regarding growth have been found even in mice with a pre-mature stop codon mutation, where typically there is no absolute chondrocyte expansion [47]. There is now an ongoing clinical trial of CMZ in patients with MCDS which will test this hypothesis in humans [48].
Discussion/conclusion
With the advancements in genetics, we continue to obtain a deeper understanding of the complex mechanisms of growth. While rhGH has been the mainstay of treatment of short stature for years, there has recently been a significant expansion in the field of novel therapies that will soon change the way clinicians approach treatment. All three of the LAGH agents mentioned above (somapacitan, somatrogon, lonapegsomatropin) are now approved for use in children with GH deficiency; therefore, understanding their mechanisms of action, safety profiles, caveats, and pitfalls is essential. Unfortunately, it remains impossible at the moment to directly compare the results of these similar, yet substantially different agents, via existing data from phase 3 trials. Future studies directly comparing these agents would be helpful. Additionally, it is important to note that all the above clinical trials only include children with GH deficiency, which in most cases is defined as peak GH level of < 10 ng/ml. Whether this is truly sufficient and accurate to diagnose, GH deficiency has long been a highly controversial point in the literature [49] and therefore needs to be taken into consideration when applied in clinical practice. Ongoing and future studies will test these LAGH preparations in non-GH deficient indications. Lastly, antibody formation was something commonly seen in LAGH studies, and although this was not associated with less efficacy or more side effects, some speculate that it can have an unpredictable effect in the setting of long-term use. Additionally, the long-term metabolic effects of LAGH are not known and one should be cautious in counseling about the potential for long-term metabolic and cardiovascular risk [50]. At the same time, there continues to be an ongoing exploration of non-injectable agents, like LUM-201; however, studies are still at a preliminary stage. Importantly, it has now become evident that approach to short stature should be tailored to the specific underlying pathology rather than one-size-fits-all mentality. An example of that is the use of burosumab in children with hypophosphatemic rickets. Similarly, there has been a major improvement in the field of skeletal dysplasias, with recent addition of novel therapies including vosoritide that is current approved for use in children with achondroplasia in multiple countries. Although absolute HV with vosoritide is found to be less than with rhGH for growth hormone deficiency, the increase in HV in children with achondroplasia appears to be sustained over multiple years which may lead to a clinically significant effect on final height. Nevertheless, we still do not know the full effect of vosoritide on important medical comorbidities such as foramen magnum stenosis, spinal stenosis, or body disproportion. Ongoing studied will shed light on these issues in the future. Targeted approaches are developed for other skeletal dysplasias too, including MCDS. One of the barriers to care for newer therapies is the burden of cost. Nonetheless, as the model of personized medicine is expanding in many fields, it will eventually also become standard of care when it comes to approaching short stature.
References
Mohseni S, Heydari Z, Qorbani M, Radfar M (2018) Adherence to growth hormone therapy in children and its potential barriers. J Pediatr Endocrinol Metab 31:13–20
Aydın BK, Aycan Z, Sıklar Z et al (2014) Adherence to growth hormone therapy: results of a multicenter study. Endocr Pract 20:46–51
Brod M, Højbjerre L, Alolga SL, Beck JF, Wilkinson L, Rasmussen MH (2017) Understanding treatment burden for children treated for growth hormone deficiency. Patient 10:653–666
Fares FA, Suganuma N, Nishimori K, LaPolt PS, Hsueh AJ, Boime I (1992) Design of a long-acting follitropin agonist by fusing the C-terminal sequence of the chorionic gonadotropin beta subunit to the follitropin beta subunit. Proc Natl Acad Sci USA 89:4304–4308
Fares F, Havron A, Fima E (2011) Designing a long acting erythropoietin by fusing three carboxyl-terminal peptides of human chorionic gonadotropin β subunit to the N-terminal and C-terminal coding sequence. Int J Cell Biol 2011:275063
Strasburger CJ, Vanuga P, Payer J et al (2017) MOD-4023, a long-acting carboxy-terminal peptide-modified human growth hormone: results of a Phase 2 study in growth hormone-deficient adults. Eur J Endocrinol 176:283–294
Zelinska N, Iotova V, Skorodok J et al (2017) Long-acting C-terminal peptide-modified hGH (MOD-4023): results of a safety and dose-finding study in GHD children. J Clin Endocrinol Metab 102:1578–1587
Deal CL, Steelman J, Vlachopapadopoulou E et al (2022) Efficacy and safety of weekly somatrogon vs daily somatropin in children with growth hormone deficiency: a phase 3 study. J Clin Endocrinol Metab 107:e2717–e2728
Zadik Z, Zelinska N, Iotova V et al (2023) An open-label extension of a phase 2 dose-finding study of once-weekly somatrogon vs. once-daily Genotropin in children with short stature due to growth hormone deficiency: results following 5 years of treatment. J Pediatr Endocrinol Metab 36:261–9
Thornton PS, Maniatis AK, Aghajanova E et al (2021) Weekly lonapegsomatropin in treatment-naïve children with growth hormone deficiency: the phase 3 height trial. J Clin Endocrinol Metab 106:3184–3195
Alkhatib EH, Dauber A, Estrada DE, Majidi S (2023) Weekly growth hormone (lonapegsomatropin) causes severe transient hyperglycemia in a child with obesity. Horm Res Paediatr 1–5
Sävendahl L, Battelino T, Rasmussen MH et al (2023) Weekly somapacitan in GH deficiency: 4-year efficacy, safety and treatment/disease burden results from REAL 3. J Clin Endocrinol Metab
Sävendahl L, Battelino T, Brod M et al (2020) Once-weekly somapacitan vs daily GH in children with GH deficiency: results from a randomized phase 2 trial. J Clin Endocrinol Metab 105:e1847–e1861
Jørgensen JO, Møller N, Lauritzen T, Alberti KG, Orskov H, Christiansen JS (1990) Evening versus morning injections of growth hormone (GH) in GH-deficient patients: effects on 24-hour patterns of circulating hormones and metabolites. J Clin Endocrinol Metab 70:207–214
Laursen T, Møller J, Jørgensen JO, Orskov H, Christiansen JS (1996) Bioavailability and bioactivity of intravenous vs subcutaneous infusion of growth hormone in GH-deficient patients. Clin Endocrinol (Oxf) 45:333–339
Jørgensen JO, Møller N, Lauritzen T, Christiansen JS (1990) Pulsatile versus continuous intravenous administration of growth hormone (GH) in GH-deficient patients: effects on circulating insulin-like growth factor-I and metabolic indices. J Clin Endocrinol Metab 70:1616–1623
Allen DB, Backeljauw P, Bidlingmaier M et al (2016) GH safety workshop position paper: a critical appraisal of recombinant human GH therapy in children and adults. Eur J Endocrinol 174:P1-9
Johannsson G, Bidlingmaier M, Biller BMK et al (2018) Growth Hormone Research Society perspective on biomarkers of GH action in children and adults. Endocr Connect 7:R126–R134
Yuen KCJ, Miller BS, Boguszewski CL, Hoffman AR (2021) Usefulness and potential pitfalls of long-acting growth hormone analogs. Front Endocrinol (Lausanne) 12:637209
Pampanini V, Deodati A, Inzaghi E, Cianfarani S (2022) Long-acting growth hormone preparations and their use in children with growth hormone deficiency. Horm Res Paediatr
Lin Z, Shu AD, Bach M, Miller BS, Rogol AD (2022) Average IGF-1 Prediction for once-weekly lonapegsomatropin in children with growth hormone deficiency. J Endocr Soc 6:bvab168
Hoover-Fong J, Scott CI, Jones MC (2020) Health supervision for people with achondroplasia. Pediatrics 145
Merchant NDA Shedding light: novel therapies for common disorders. Achondroplasia and growth disorders Accepted.
Wendt DJ, Dvorak-Ewell M, Bullens S et al (2015) Neutral endopeptidase-resistant C-type natriuretic peptide variant represents a new therapeutic approach for treatment of fibroblast growth factor receptor 3-related dwarfism. J Pharmacol Exp Ther 353:132–149
Lorget F, Kaci N, Peng J et al (2012) Evaluation of the therapeutic potential of a CNP analog in a Fgfr3 mouse model recapitulating achondroplasia. Am J Hum Genet 91:1108–1114
Savarirayan R, Irving M, Bacino CA et al (2019) C-type natriuretic peptide analogue therapy in children with achondroplasia. N Engl J Med 381:25–35
Breinholt VM, Rasmussen CE, Mygind PH et al (2019) TransCon CNP, a sustained-release C-type natriuretic peptide prodrug, a potentially safe and efficacious new therapeutic modality for the treatment of comorbidities associated with fibroblast growth factor receptor 3-related skeletal dysplasias. J Pharmacol Exp Ther 370:459–471
Breinholt VM, Mygind PH, Christoffersen ED et al (2022) Phase 1 safety, tolerability, pharmacokinetics and pharmacodynamics results of a long-acting C-type natriuretic peptide prodrug. TransCon CNP Br J Clin Pharmacol 88:4763–4772
TransCon™CNP ACcomplisHTrial Topline Results. https://investors.ascendispharma.com/static-files/44b24b0c-f83d-48fa-aaef-9bdb768999d3
Komla-Ebri D, Dambroise E, Kramer I et al (2016) Tyrosine kinase inhibitor NVP-BGJ398 functionally improves FGFR3-related dwarfism in mouse model. J Clin Invest 126:1871–1884
Savarirayan R, De Bergua JM, Arundel P et al (2022) Infigratinib in children with achondroplasia: the PROPEL and PROPEL 2 studies. Ther Adv Musculoskelet Dis 14:1759720x221084848
PROPEL2 topline results (2023) https://investor.bridgebio.com/static-files/25c6cab1-cbec-4c6-96a6-067367e8e170
Nass R, Pezzoli SS, Oliveri MC et al (2008) Effects of an oral ghrelin mimetic on body composition and clinical outcomes in healthy older adults: a randomized trial. Ann Intern Med 149:601–611
Codner E, Cassorla F, Tiulpakov AN et al (2001) Effects of oral administration of ibutamoren mesylate, a nonpeptide growth hormone secretagogue, on the growth hormone-insulin-like growth factor I axis in growth hormone-deficient children. Clin Pharmacol Ther 70:91–98
Bright GM, Do MT, McKew JC, Blum WF, Thorner MO (2021) Development of a predictive enrichment marker for the oral GH secretagogue LUM-201 in pediatric growth hormone deficiency. J Endocr Soc 5:bvab030
Bright GM, Thorner MO (2022) A GH secretagogue receptor agonist (LUM-201) elicits greater GH responses than standard GH secretagogues in subjects of a pediatric GH deficiency trial. Horm Res Paediatr 95:76–81
Dauber A (2023) Growth response of oral LUM-201 in OraGrowtH210 and OraGrowtH212 trials in idiopathic pediatric growth hormone deficiency (iPGHD): combined analysis interim analysis data. ENDO Chicago
Seefried L, Duplan MB, Briot K et al (2023) Anticipated effects of burosumab treatment on long-term clinical sequelae in XLH: expert perspectives. Front Endocrinol (Lausanne) 14:1211426
Linglart A, Biosse-Duplan M, Briot K et al (2014) Therapeutic management of hypophosphatemic rickets from infancy to adulthood. Endocr Connect 3(1):R13-30
Ward LM, Glorieux FH, Whyte MP et al (2022) Effect of burosumab compared with conventional therapy on younger vs older children with X-linked hypophosphatemia. J Clin Endocrinol Metab 107:e3241–e3253
Imel EA, Glorieux FH, Whyte MP et al (2019) Burosumab versus conventional therapy in children with X-linked hypophosphataemia: a randomised, active-controlled, open-label, phase 3 trial. Lancet 393:2416–2427
Gadion M, Hervé A, Herrou J et al (2022) Burosumab and dental abscesses in children with X-linked hypophosphatemia. JBMR Plus 6(11):e10672
Whyte MP, Simmons JH, Moseley S et al (2019) Asfotase alfa for infants and young children with hypophosphatasia: 7 year outcomes of a single-arm, open-label, phase 2 extension trial. Lancet Diabetes Endocrinol 7:93–105
Hofmann CE, Harmatz P, Vockley J et al (2019) Efficacy and safety of asfotase alfa in infants and young children with hypophosphatasia: a phase 2 open-label study. J Clin Endocrinol Metab 104:2735–2747
Kishnani PS, Rockman-Greenberg C, Rauch F et al (2019) Five-year efficacy and safety of asfotase alfa therapy for adults and adolescents with hypophosphatasia. Bone 121:149–162
Hidvegi T, Ewing M, Hale P et al (2010) An autophagy-enhancing drug promotes degradation of mutant alpha1-antitrypsin Z and reduces hepatic fibrosis. Science 329:229–232
Mullan LA, Mularczyk EJ, Kung LH et al (2017) Increased intracellular proteolysis reduces disease severity in an ER stress-associated dwarfism. J Clin Invest 127:3861–3865
MCDS Therapy EU Horizon (2020) Project at https://mcds-therapy.eu/
Kamoun C, Hawkes CP, Grimberg A (2021) Provocative growth hormone testing in children: how did we get here and where do we go now? J Pediatr Endocrinol Metab 34(6):679–696
Tidblad A, Bottai M, Kieler H et al (2021) Association of childhood growth hormone treatment with long-term cardiovascular morbidity. JAMA Pediatr 175(2):e205199
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception of this review article. Literature search was conducted by DG, and reviewed by AD. The first draft of the manuscript was written by DG and NM, and was edited and reviewed by AD. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Galetaki, D.M., Merchant, N. & Dauber, A. Novel therapies for growth disorders. Eur J Pediatr 183, 1121–1128 (2024). https://doi.org/10.1007/s00431-023-05239-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05239-y