Abstract
Purpose
Primary graft dysfunction still represents a major challenge in liver transplantation. We herein studied in an isolated rat liver perfusion model whether a multidrug donor preconditioning (MDDP) can not only reduce but also completely prevent cold ischemia–reperfusion injury.
Methods
MDDP included curcumin, simvastatin, N-acetylcysteine, erythropoietin, pentoxyphylline, melatonin, glycine, and methylprednisolone. Postischemic reperfusion was performed after 24 h cold storage in histidine–tryptophan–ketoglutarate solution with 37°C Krebs Henseleit bicarbonate buffer.
Results
Cold hepatic ischemia–reperfusion resulted in a massive K+ release, protein loss, and aspartate aminotransferase, alanine aminotransferase, and lactate dehydrogenase elevation. This was associated with increased malondialdehyde formation, enhanced tumor necrosis factor-alpha and interleukin-6 production, pronounced leukocytic tissue infiltration, and apoptotic cell death.
Conclusions
MDDP abolished the inflammation response and was capable of completely preventing the manifestation of parenchymal injury. Thus, MDDP potentiates the protective effects reported after single-drug donor preconditioning and may therefore be an interesting approach to improve the outcome in clinical liver transplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the successful use of polyvalent organ preservation solutions, such as histidine–tryptophan–ketoglutarate (HTK) and University of Wisconsin (UW), preservation and reperfusion injury still represents a major challenge in liver transplantation [1]. The organ injury, induced by cold ischemia and warm reperfusion, is initiated by sinusoidal lining cell damage and can lead to primary liver graft dysfunction (PLGD). In fact, PLGD significantly contributes to the morbidity and mortality among liver transplant recipients [2, 3]. The incidence of PLGD after liver transplantation ranges between 4.6% and 14.6% [3, 4]. In view of the worldwide donor organ shortage, modified preservation solutions have been established to further reduce ischemia–reperfusion (I/R) injury [1, 5, 6].
Donor organ preconditioning (DOP) is an additive approach for donor liver protection and is thought to attenuate I/R injury after transplantation [7–9]. Basically, the achievement of DOP is attributed to the fact that drugs are applied under physiological conditions which guarantee adequate amounts of energy-rich phosphates necessary for the intracellular drug uptake [10, 11]. In contrast, addition of drugs into the preservation solution is thought to be disadvantageous because the amount of energy-rich phosphates during preservation is restricted and the additional consumption of the already limited amount of energy-rich phosphates may further affect the quality of the preserved organ [12].
The established preconditioning procedures include either short-term or long-term DOP protocols. Long-term protocols, as described for Kupffer cell modulation or doxorubicin-induced heat shock protein 72 expression [13, 14], may not be transferred to clinical routine due to the limited practicability in organ harvesting.
In contrast, short-term DOP protocols with different single drugs, such as curcumin, pentoxifylline, simvastatin, N-acetylcysteine, erythropoietin, melatonin, glycine, or methylprednisolone, have shown promising results. Curcumin [15], which is a yellow-orange dye extracted from the spice turmeric, has demonstrated protection in a rat model of warm hepatic I/R, which was associated with the control of heat shock proteins, anti-oxidative enzymes, and apoptotic cell death.
Pentoxifylline is a methylxanthine derivate and phosphodiesterase inhibitor, commonly used for the treatment of peripheral vascular diseases. Nishizawa et al. [7] demonstrated in a donor pretreatment experiment in rat livers that pentoxifylline suppresses Kupffer cell activation and decreases I/R injury [7, 16].
Simvastatin [8] is an inhibitor of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, which is the rate-limiting hepatic enzyme responsible for converting HMG-CoA to mevalonate, a precursor of sterols including cholesterol. Inhibition of HMG-CoA reductase lowers the amount of mevalonate and subsequently reduces cholesterol levels in hepatic cells [17].
N-Acetylcysteine (NAC) is a thiol-containing compound that serves as a glutathione precursor [9]. It also can serve directly as a scavenger of oxygen-derived free radicals [18]. Glutathione is known to act as a cellular antioxidant [18]. Liver I/R injury is associated with the depletion of hepatic GSH stores [18].
Erythropoietin is an endogenous hormone produced by interstitial fibroblasts in the kidney and in the fetal liver. It is a potent stimulator of bone marrow activity and increases red cell production [19]. The properties of EPO in protecting from I/R injury, however, may include anti-oxidative and anti-apoptotic effects and may also involve the downregulation of tumor necrosis factor (TNF)-alpha production and the stimulation of eNOS expression [20–22].
Melatonin (N-acetyl-5-methoxy-tryptamine) is a lipophilic indoleamine product secreted by the pineal gland. Melatonin and its metabolites are potent anti-oxidants that are well tolerated and non-toxic [23]. Melatonin has been reported to reduce hepatocellular damage after warm I/R [24] and to improve liver function after cold storage and reperfusion [24–26].
Glycine, a non-essential amino acid, has been shown to successfully reduce cold I/R injury in the liver [27]. It acts in cold ischemia by attenuating Kupffer cell activation, which results in a significant reduction of TNF-alpha release [27].
The first reports on protective effects of steroids on liver ischemia were published in 1975 by Santiago Delpin and Figueroa [28]. They described that methylprednisolone applied before hepatic occlusion results in an increased animal survival and a reduced liver damage when compared with non-treated, ischemic controls [28]. Of interest, methylprednisolone did not affect hepatic protein synthesis during ischemia but restored it more effectively during reperfusion. The mechanisms of action are still not fully understood. It is assumed that methylprednisolone can protect the cell membrane by stabilization of the lysosomal membrane or inhibit circulating toxic substances liberated from the liver during ischemia [29]. In addition, it may lower I/R injury by attenuating the preservation-induced Kupffer cell damage [30].
In the experimental setting, these short-term single-drug donor preconditioning procedures have shown various degrees of attenuation of cold or warm hepatic I/R injury [7–9, 15, 16, 21, 24–27, 30–32]. With the interest to further enhance protection from I/R injury in cold liver preservation and reperfusion, we herein studied with the use of an isolated rat liver perfusion model whether multidrug donor preconditioning (MDDP), including curcumin, pentoxifylline, simvastatin, N-acetylcysteine, erythropoietin, melatonin, glycine, and methylprednisolone, is capable of not only reducing but also completely preventing manifestation of cold hepatic I/R injury.
Material and methods
Animals
A total of Sprague–Dawley rats of either sex with a body weight of 280–330 g were used. The animals were housed in single cages at 22°C with a 12:12-h dark–light cycle and were kept on standard laboratory chow and water ad libitum. The experiments were performed according to the National Institutes of Health Guide for Care and Use of Laboratory Animals (NIH publication 86-23, revised 1985) and were approved by the local animal care committee.
Liver procurement
Rats were anesthetized with pentobarbital sodium (50 mg/kg body weight (bw) i.p.; Narcoren, Merial, Hallbergmoos, Germany). A tracheotomy was performed to facilitate spontaneous respiration. After laparotomy, the common bile duct was cannulated and bile was collected for 20 min to assess baseline values. After systemic anticoagulation with 500 iU heparin, livers were flushed with 100 mL of 4°C HTK solution (Custodiol®, Köhler Chemie, Alsbach-Hähnlein, Germany) via an aortic catheter with a pressure of 90 cm H2O. Livers were then immediately harvested, weighed, and stored in 4°C HTK solution.
Isolated liver perfusion
After 24 h cold storage, livers were reperfused for 60 min through the portal vein in a non-recirculating system [33]. Perfusion was performed with freshly prepared Krebs–Henseleit bicarbonate buffer saturated with carbogen at a flow rate of 2 mL/min g liver tissue using a pulsatile perfusion pump (beta/4, ProMinent, Heidelberg, Germany). Throughout the reperfusion period, portal venous pressure was measured continuously. Samples of the effluent fluid were collected after 1, 30, and 60 min via an infrahepatic vena cava catheter for analysis of alanine transaminase (ALAT), aspartate transaminase (ASAT), and lactate dehydrogenase (LDH) activities as well as for determination of potassium (K+), malondialdehyde (MDA), and total protein (TP).
Bile was collected in 30-min intervals over 60 min to measure liver excretory function. Moreover, perfusate samples were withdrawn from the portal inflow and the infrahepatic cava outflow after 1, 30, and 60 min for analysis of pH.
Sampling and assays
Bile volume was measured and standardized per gram of liver wet weight (microliters per minute gram liver tissue). LDH, ALAT, and ASAT activities were analyzed in perfusate samples by means of standard spectrophotometric techniques. K+, pH, and blood gases were measured by a blood gas and electrolyte analyzer (Rapidlab 855, Bayer Health Care, Fernwald, Germany). Plasma TNF-alpha and interleukin-6 (IL-6) were determined by an enzyme-linked immunosorbent assay (ELISA) according to the manufacturer’s instructions (R&D Systems, Wiesbaden Nordenstadt, Germany). At the end of cold storage and after postischemic reperfusion, liver tissue was sampled for histology and Western blot analysis.
MDA analysis
Oxidative stress was ascertained by the formation of MDA (DigiScan, Asys Hitech, Deelux Labortechnik, Gödendorf, Germany). MDA was determined spectrophotometrically. One volume of the tissue sample was mixed with 10 vol of a solution of 10% (w/v) trichloroacetic acid, 0.375% (w/v) thiobarbituric acid, and 0.25 M hydrochloric acid, and the mixture was heated for 10 min in a boiling water bath. After cooling, the flocculent precipitate was removed by centrifugation at 1,000×g for 15 min. Absorbance was measured at 550 nm. Thiobarbituric acid reaction species in concentrations from 0 to 100 μmol were used to establish the standard curve.
Histology and immunohistochemistry
For analysis of hepatocellular vacuolization, cellular stress response and apoptotic cell death liver tissue was fixed for 2 to 3 days in 4% formalin and embedded in paraffin. Five-micrometer sections were cut from paraffin-embedded tissue blocks and stained with hematoxylin–eosin. Cytoplasmic vacuolization of hepatocytes was scored in 20 high-power fields by a semi-quantitative score from 0 to 4, with none = 0, minimal (<10% hepatocytes) = 1, mild (10–25% hepatocytes) = 2, moderate (25–50% hepatocytes) = 3, and severe (>50% hepatocytes) = 4.
To study leukocytic tissue infiltration, neutrophils were stained by the AS-D chloroacetate esterase (CAE) technique. Cells were identified by positive staining and morphology. CAE-positive cells were counted within 20 consecutive high-power fields (×40 objective, 0.65 numeric aperture) and are given in percent of all cells visible.
To study the amount of apoptotic cell death, cleaved caspase-3 was stained using indirect immunoperoxidase techniques [34]. Therefore, deparaffinized sections were incubated with 3% H2O2 and 2% goat normal serum to block endogenous peroxidases and unspecific binding sites. A rabbit polyclonal anti-cleaved caspase-3 antibody (1:50, Cell Signaling Technology, Frankfurt, Germany) was used as primary antibody. A biotinylated goat anti-rabbit immunoglobulin antibody served as secondary antibody for streptavidin–biotin complex peroxidase staining (LSAB 2 System HRP, DakoCytomation). 3,3′-Diaminobenzidine (DakoCytomation) served as chromogen. Sections were counterstained with Hemalaun. The number of apoptotic cells was counted and is expressed in percent of all cells within 15 consecutive high-power fields.
Western blot analysis
For whole protein extracts and Western blot analysis of caspase-3, liver tissue was homogenized in lysis buffer (10 mM Tris, pH 7.5, 10 mM NaCl, 0.1 mM ethylenediaminetetraacetic acid, 0.5% Triton-X 100, 0.02% NaN3, 0.2 mM phenylmethylsulfonyl fluoride), incubated for 30 min on ice, and centrifuged for another 30 min at 16,000×g at 4°C. The supernatant was saved as whole protein fraction. Prior to use, a protease inhibitor cocktail (1:100 v/v, Sigma) was added to the buffer. Protein concentrations were determined using the Lowry assay with bovine serum albumin as standard.
Equal amounts of protein per lane (30 μg of whole liver lysate) were separated discontinuously on 10% sodium dodecyl sulfate polyacrylamide gels and transferred to a polyvinyldifluoride membrane (BioRad, Munich, Germany). After blockade of non-specific binding sites, membranes were incubated for 2 h at room temperature with rabbit polyclonal anti-cleaved caspase-3 antibodies (1:800, Cell Signaling Technology, Frankfurt, Germany). This was followed by a secondary peroxidase-conjugated donkey anti-rabbit IgG antibody (1:5,000, Amersham Pharmacia Biotech, Freiburg, Germany). Protein expression was visualized using luminol-enhanced chemiluminescence and exposure of the membrane to a blue light-sensitive autoradiography film (Hyperfilm ECL, Amersham Pharmacia Biotech). Signals were assessed densitometrically and normalized to the β-actin signals (mouse monoclonal anti-β-actin antibody, 1:5,000) to correct unequal loading.
MDDP protocol
MDDP was initiated 30 min before starting the cold perfusion with HTK solution for organ harvesting by applying 50 mg/kg bw curcumin (Sigma Aldrich Chemie Holding GmbH, Taufkirchen, Germany) in 0.33 ml DMSO1 and 5 mg/kg bw simvastatin (SimvaHEXAL®, Hexal AG, Holzkirchen, Germany) in 0.67 ml 100% ethanol [4] intragastrically using a 0.45 × 13-mm cannula (Table 1).
MDDP additionally included the intraperitoneal application of 150 mg/kg bw N-acetylcysteine (Fluimucil®, Pierre Fabre Pharma, Freiburg, Germany) in 1.67 ml NaCl 0.9% [5], 3,000 IU/kg bw erythropoietin (Epoetin alfa HEXAL®, Hexal AG, Holzkirchen, Germany) [6–8], 50 mg/kg bw pentoxyphylline (Trental®, Sanofi-Aventis, Frankfurt, Germany) in 2.67 ml NaCl 0.9% [2, 3], and 10 mg/kg bw melatonin (Sigma Aldrich Chemie Holding GmbH, Taufkirchen, Germany) in 0.67 ml ethanol 20% [9, 10] 30 min before cold perfusion (Table 1).
MDDP was finally completed by intravenous injection of 100 mg/kg bw (300 mM) glycine in 1.67 ml NaCl 0.9% [11] and 5 mg/kg bw methylprednisolone (Urbason®, Sanofi-Aventis, Frankfurt, Germany) in 1.67 ml NaCl 0.9% [12, 13] through the portal vein 10 min before cold HTK perfusion (Table 1).
Experimental protocol
A total of 24 animals were divided into three groups. In the preconditioning group (MDDP; n = 8), rats underwent the MDDP protocol before liver perfusion with 4°C cold HTK solution. In the ischemia–reperfusion group (I/R; n = 8), animals received 2.0 mL vehicle (0.9% NaCl) 10 min before liver perfusion with 4°C cold HTK solution. Livers of animals of those two groups were stored for 24 h in 4°C HTK solution. In sham-operated controls, untreated livers were perfused with 4°C cold HTK solution and were reperfused directly after harvest in the isolated liver perfusion setup.
Statistics
All data are expressed as mean ± SD. After proving the assumption of normality and homogeneity of variance across groups, differences between groups were calculated by a one-way analysis of variance (ANOVA) followed by an pairwise Dunnett post hoc test using the statistical software package SigmaStat (Jandel Scientific, San Rafael, CA, USA). Overall statistical significance was set at p < 0.05.
Results
Reperfusion-associated tissue injury
Potassium and total protein concentrations in the effluent fluid were measured as indicators of cell membrane integrity. Loss of cell membrane integrity is indicated by an increase of potassium and total protein in the effluent fluid. I/R induced a significant increase of K+ (11.62 ± 3.35 mmol/L) and TP (5.11 ± 2.72 g/L) in the first effluent at 1 min reperfusion when compared to sham controls (8.08 ± 1.46 mmol/L and 3.00 ± 2.32 g/L, p < 0.05). Of interest, MDDP completely prevented this increase in K+ (7.82 ± 0.52 mmol/L) and TP (1.40 ± 0.50 g/L), as indicated by levels similar to that of sham controls (p < 0.05). After 60 min reperfusion, potassium and protein release of all livers exposed to cold storage were found in the range of non-ischemic controls (5.73–5.86 mmol/L and 0.08–0.12 g/L). Analysis of pH did not reveal substantial differences between the three groups studied (data not shown).
Analysis of ASAT, ALAT, and LDH, serving as indicators of parenchymal cell death, revealed a 5- to 10-fold increase in the first effluent after cold I/R compared to sham controls (Table 2). MDDP could almost completely prevent this increase of hepatocellular enzyme release, presenting with values not significantly different from that of sham controls (Table 2). After 30 and 60 min of reperfusion, enzyme levels were found slightly higher in both I/R and I/R-MDDP livers compared to controls; however, these differences did not prove to be statistically significant (Table 2).
Bile flow was used as an indicator of liver excretory function. After 60 min reperfusion, sham controls showed a bile flow of 0.23 ± 0.17 μL/g tissue min. In contrast, I/R livers showed a reduced value of 0.17 ± 0.16 μL/g tissue min, although this reduction did not proof to be statistically significant (ANOVA: p = 0.679). MDDP before I/R was capable of restoring bile flow to 0.22 ± 0.13 μL/g tissue min.
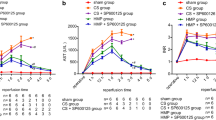
Cytokine release
The release of the pro-inflammatory chemokines TNF-alpha and IL-6 into the effluent during postischemic reperfusion was analyzed by ELISA. The 24-h cold storage caused significantly increased TNF-alpha and IL-6 concentrations in the first effluent at 1 min, which remained elevated over the entire 60-min period of reperfusion (Fig. 1). Of interest, at 1 min reperfusion, MDDP could completely prevent the increase of TNF-alpha and significantly reduce the amount of IL-6 release (263 ± 158 vs. 435 ± 297 pg/mL). Also, at 60 min of reperfusion, the cytokine measurements in the effluent of I/R-MDDP livers still revealed negligible values (Fig. 1; IL-6, 31 ± 21 pg/mL) not significantly different from those of sham controls (Fig. 1; IL-6, 10.07 ± 14.25 pg/mL).
Tumor necrosis factor-alpha concentration (TNF-alpha) of the effluent after 1 min (a) and 60 min (b) reperfusion of livers exposed to 24 h cold storage in 4°C HTK. Donor animals underwent short-term multidrug donor preconditioning (MDDP) or received saline pretreatment (I/R). Livers from untreated animals which were not exposed to 24 h cold storage served as sham controls (Sham). Data are given as means ± SD (n = 8 in each group); # p < 0.05 vs. Sham, *p < 0.05 vs. I/R
Lipid peroxidation
MDA formation was measured as an indicator of lipid peroxidation and membrane disintegration. In the first effluent at 1 min reperfusion, I/R livers showed an almost 5-fold increase of MDA concentration compared to sham controls, which remained elevated until the end of the 60-min observation period (Fig. 2). Application of the MDDP protocol before 24 h cold ischemic storage was successful to completely prevent the increase of MDA over the entire postischemic reperfusion period (Fig. 2).
Malondialdehyde concentration (MDA) of the effluent after 1 min (a) and 60 min (b) reperfusion of livers exposed to 24 h cold storage in 4°C HTK. Donor animals underwent short-term multidrug donor preconditioning (MDDP) or received saline pretreatment (I/R). Livers from untreated animals which were not exposed to 24 h cold storage served as sham controls (Sham). Data are given as means ± SD (n = 8 in each group); # p < 0.05 vs. Sham, *p < 0.05 vs. I/R
Leukocyte recruitment
After 60 min reperfusion, saline-treated I/R livers showed a markedly elevated number of transmigrated leukocytes. Pretreatment of livers according to the MDDP protocol before 24 h storage in HTK was capable of completely abrogating the I/R-induced increase in leukocyte transmigration (Fig. 3).
Leukocyte infiltration (a–d, chloroacetate esterase staining) after 60 min reperfusion of livers exposed to 24 h cold storage in 4°C HTK. Donor animals underwent short-term multidrug donor preconditioning (MDDP; c) or received saline pretreatment (I/R; b). Livers from untreated animals which were not exposed to 24 h cold storage served as sham controls (Sham; a). Data are given as means ± SD (n = 4 in each group); # p < 0.05 vs. Sham, *p < 0.05 vs. I/R. Magnification (a–c), ×120
Histomorphology and apoptotic cell death
Hematoxylin–eosin-stained tissue sections showed a dramatic increase of vacuolization of hepatocytes after I/R when compared to sham controls, indicating hypoxic parenchymal injury. MDDP was capable of significantly reducing vacuolization. Although the score of vacuolization after MDDP was still higher than that of sham controls, this difference did not prove to be statistically significant (Fig. 4).
Cytoplasmic hepatocellular vacuolization (a–d, hematoxylin–eosin staining) after 60 min reperfusion of livers exposed to 24 h cold storage in 4°C HTK. Donor animals underwent short-term multidrug donor preconditioning (MDDP; c) or received saline pretreatment (I/R; b). Livers from untreated animals which were not exposed to 24 h cold storage served as sham controls (Sham; a). Data are given as means ± SD (n = 4 in each group); # p < 0.05 vs. Sham, *p < 0.05 vs. I/R. Magnification (a–c), ×120
In addition, immunohistochemistry and Western blots showed a significant increase of cleaved caspase-3 expression in saline-treated I/R livers when compared with sham controls. Of interest, MDDP before 24 h cold storage completely abolished the increase of cleaved caspase-3, indicating prevention of apoptotic cell death (Fig. 5).
Cleaved caspase-3 expression (a–d immunohistochemistry; e, f Western blot) after 60 min reperfusion in livers exposed to 24 h cold storage in 4°C HTK. Donor animals underwent short-term multidrug donor preconditioning (MDDP; c) or received saline pretreatment (I/R; b). Livers from untreated animals which were not exposed to 24 h cold storage served as sham controls (Sham; a). Data are given as means ± SD (n = 4 in each group); # p < 0.05 vs. Sham, *p < 0.05 vs. I/R. Magnification (a–c), ×120
Discussion
The major finding of the present study is that short-term MDDP of 24-h cold-stored livers almost completely prevents manifestation of postischemic reperfusion injury. This protection is provided by the anti-oxidative, anti-inflammatory, and anti-apoptotic actions of MDDP.
For our experiments on cold I/R, we have chosen the isolated rat liver perfusion model and a cold ischemia time of 24 h with organ storage in HTK. These conditions did prove appropriate to induce a marked postischemic injury after 60 min reperfusion, presenting with the entire plethora of well-known mechanisms of I/R injury, including oxygen radical production, pro-inflammatory cytokine release, neutrophilic infiltration, and apoptotic and necrotic cell death. Thus, the model and the cold ischemic exposure time have to be considered adequate to mimic severe cold I/R injury in liver transplantation and, accordingly, to study protective actions of MDDP.
The compounds included in the MDDP protocol may have differently contributed to the protection from IR injury. The anti-inflammatory modes of action of curcumin may have caused the MDDP-associated prevention MDA formation and caspase-3 activation, observed in the present study.
Pentoxifylline is known to be capable of not only inhibiting TNF-alpha production in hepatic I/R [16] but also of reducing leukocyte recruitment and apoptotic cell death within the postischemic microvasculature [35, 36]. These actions of pentoxifylline may have abrogated the TNF-alpha release, the leukocyte infiltration, and the apoptotic cell death, observed in I/R livers after application of the MDDP protocol. TNF-alpha and related cytokines are key players in different pathways, as they can exert both pro-apoptotic and anti-apoptotic actions on hepatocytes. They may contribute to I/R-induced inflammation and injury; however, they are also involved in liver regeneration. However, in hepatic I/R, Colletti et al. [37] and others could demonstrate that inhibition of TNF-alpha is effective to significantly reduce I/R injury, indicating a deleterious role of this pro-inflammatory cytokine on postischemic organ integrity. In the present study, we observed an increase in TNF-alpha and intrahepatic leukocyte recruitment in the non-treated I/R controls. This increased leukocytic inflammation may not be considered a reperfusion-associated event but is rather due to the surgical manipulation before organ flush and harvest. This view is based on previous studies, demonstrating TNF-alpha-mediated Kupffer cell activation due to mechanical organ manipulation during liver surgery [38].
Statins have been shown to suppress inflammation and proliferation in vascular endothelial and smooth muscle cells [8, 39] and to reduce I/R injury in the liver [8] and the kidney [40]. Of interest, the pleiotropic actions of statins are not related to its lipid-lowering mechanism but rather caused by their anti-oxidative properties [17, 41], their inhibitory action on leukocyte adhesion [42, 43], and their modulatory function on the microcirculation [42, 44]. These statin actions may have contributed to the prevention of I/R injury observed in the present study after MDDP application.
Previous studies have shown that the administration of NAC recovers liver glutathione stores and that glutathione replenishment during postischemic reperfusion attenuates hepatic I/R injury [18]. Thus, NAC can be used successfully for pharmacological preconditioning in hepatic I/R [9]. Beside its anti-oxidative properties, the protection from I/R injury by NAC may additionally be due to its anti-inflammatory action, reducing pro-inflammatory cytokine production and leukocyte aggregation [45, 46].
EPO has been shown to protect from I/R injury by its anti-oxidative and anti-apoptotic properties, involving the downregulation of TNF-alpha production and the stimulation of eNOS expression [20–22]. These actions of EPO can reduce leukocyte adherence and improve the microcirculation by vasodilation [47, 48] and thus may represent the mechanisms how EPO has contributed to the abrogation of I/R injury by MDDP.
Melatonin exerts its anti-oxidative actions by increasing the activity of superoxide dismutase and glutathione peroxidase after I/R, thereby decreasing MDA accumulation in postischemic hepatic tissue [23, 26]. Thus, melatonin within the MDDP protocol may have contributed to the prevention of reperfusion injury by abrogating the oxygen radical actions and thus the MDA accumulation. Of interest, melatonin enhances mitochondrial performance and attenuates hepatic I/R injury also by improving the balance between nitric oxide and endothelin [25]. These results indicate the pleiotropic nature of melatonin and suggest that other mechanisms of action than anti-oxidative properties may also contribute to the MDDP-mediated protection in I/R injury.
Glycine has been shown to act in cold ischemia by attenuating Kupffer cell activation, resulting in a significant reduction of TNF-alpha release [27]. Glycine is also capable of preventing sinusoidal endothelial cell apoptosis after hepatic I/R [49, 50]. Thus, the reduced TNF-alpha release and the lack of increase of cleaved caspase-3 expression observed after MDDP may be caused by the action of glycine.
UW and HTK solution have been shown successful in protecting livers from preservation injury [51]. The two solutions consist of a considerable number of substances, which all have been shown capable of attenuating preservation and I/R injury [51]. Recent studies have shown that preconditioning of the donor by distinct drugs is capable of additionally improving protection from postischemic liver injury [7–9, 15, 16, 21, 24–27, 30–32]. Accordingly, preconditioning is discussed as a promising adjunct to improve outcome of organ preservation and transplantation [8, 27, 30, 32]. With the aim to achieve the best possible organ protection by adjunct preconditioning, we included those drugs in our MDDP protocol, which have been shown in previous single-drug preconditioning studies to be successful in attenuating postischemic liver injury. These substances provide protection be exerting anti-oxidative, anti-inflammatory, and anti-apoptotic actions, or may even be characterized by a pleiotropic action profile [52], such as simvastatin [42], glycine [53, 54], erythropoietin [55], and methylprednisolone [56]. The data of the present study now indicate that MDDP is capable of almost completely preventing cold I/R injury. However, we cannot distinguish whether this protection is caused by the distinct action of just one of the drugs or by the combination of different drugs. Thus, although we cannot provide detailed information on the individual contribution of each of the substances, we conclude that MDDP, similar as has been reported for UW or HTK solution, represents an approach in which multiple ingredients may be effective in improving organ quality after storage.
Taken together, short-term pharmacological preconditioning can be an effective, clinically applicable adjunct to improve organ preservation. All substances included in our MDDP protocol have been shown in previous studies to be effective in reducing liver injury after I/R. Of interest, MDDP was able to completely prevent hepatic reperfusion injury despite the prolonged period of 24 h cold storage in HTK. Although the nature and the effects of the used substances have been studied extensively, the mechanisms by which they act in combination with each other remains to be determined. Nonetheless, the fact that MDDP completely abrogated the I/R-associated oxygen radical production, cytokine response, neutrophilic infiltration, and apoptotic cell death should make it an interesting tool to be studied in liver transplantation.
Abbreviations
- ALAT:
-
Alanine aminotransferase
- ASAT:
-
Aspartate aminotransferase
- EPO:
-
Erythropoietin
- GLDH:
-
Glutamate dehydrogenase
- GSH:
-
Glutathione
- HTK:
-
Histidine–tryptophan–ketoglutarate
- IL:
-
Interleukin
- I/R:
-
Ischemia–reperfusion
- K+ :
-
Potassium
- KHB:
-
Krebs–Henseleit bicarbonate buffer
- LDH:
-
lactate dehydrogenase
- MDA:
-
Malondialdehyde
- MDDP:
-
Short-term multidrug donor preconditioning
- Na+ :
-
Sodium
- NAC:
-
Acetylcysteine
- PTX:
-
Pentoxifylline
- PLGD:
-
Primary liver graft dysfunction
- ROS:
-
Reactive oxygen species
- ST:
-
Simvastatin
- TP:
-
Total protein
- TNF:
-
Tumor necrosis factor
- UW:
-
University of Wisconsin
References
Franco-Gou R, Mosbah IB, Serafin A, Abdennebi HB, Roselló-Catafau J, Peralta C (2007) New preservation strategies for preventing liver grafts against cold ischemia reperfusion injury. J Gastroenterol Hepatol 22:1120–1126
McKeown CMB, Edwards V, Phillips MJ, Harvey PRC, Petrunka CN, Strasberg SM (1988) Sinusoidal lining cell damage: the critical injury in cold preservation of liver allografts in the rat. Transplantation 46:178–191
Jain A, Reyes J, Kashyap R, Dodson SF, Demetris AJ, Ruppert K et al (2000) Long-term survival after liver transplantation in 4, 000 consecutive patients at a single center. Ann Surg 232:490–500
Schrem H, Till N, Becker T, Bektas H, Manns MP, Strassburg CP et al (2008) Long-term results after liver transplantation. Chirurg 79:121–129
Fukuda C, Kollmar O, Schäfer T, Tian YH, Schilling MK (2002) Anionic polysaccharides. A class of substances with hepatoprotective and antiadhesive properties in rat liver preservation. Transpl Int 15:17–23
Hata K, Tolba RH, Wei L, Doorschodt BM, Büttner R, Yamamoto Y et al (2007) Impact of polysol, a newly developed preservation solution, on cold storage of steatotic rat livers. Liver Transplant 13:114–121
Nishizawa H, Egawa H, Inomata Y, Uemoto S, Asonuma K, Kiuchi T et al (1997) Efficiency of pentoxifylline in donor pretreatment in rat liver transplantation. J Surg Res 72:170–176
Lai IR, Chang KJ, Tsai HW, Chen CF (2008) Pharmacological preconditioning with simvastatin protects liver from ischemia–reperfusion injury by heme oxygenase-1 induction. Transplantation 85:732–738
Montero EF, Quireze C Jr, d'Oliveira DM (2005) Bile duct exclusion from selective vascular inflow occlusion in rat liver: role of ischemic preconditioning and N-acetylcysteine on hepatic reperfusion injury. Transplant Proc 37:425–427
Sandker GW, Slooff MJ, Groothuis GM (1992) Drug transport, viability and morphology of isolated rat hepatocytes preserved for 24 hours in University of Wisconsin solution. Biochem Pharmacol 43:1479–1485
Schilling M, Tian YH, Büchler MW (1998) Effect of temperature on hepatic and renal uptake of components from University of Wisconsin solution. Transplantation 65:989–992
Ainscow EK, Brand MD (1999) Internal regulation of ATP turnover, glycolysis and oxidative phosphorylation in rat hepatocytes. Eur J Biochem 266:737–749
Chen H, Yu YY, Zhang MJ, Deng XX, Yang WP, Ji J et al (2004) Protective effect of doxorubicin induced heat shock protein 72 on cold preservation injury of rat livers. World J Gastroenterol 10:1375–1378
Rentsch M, Puellmann K, Sirek S, Iesalnieks I, Kienle K, Mueller T et al (2005) Benefit of Kupffer cell modulation with glycine versus Kupffer cell depletion after liver transplantation in the rat: effects on postischemic reperfusion injury, apoptotic cell death graft regeneration and survival. Transpl Int 18:1079–1089
Shen SQ, Zhang Y, Xiang JJ, Xiong CL (2007) Protective effect of curcumin against liver warm ischemia/reperfusion injury in rat model is associated with regulation of heat shock protein and antioxidant enzymes. World J Gastroenterol 13:1953–1961
El-Ghoneimi A, Cursio R, Schmid-Alliana A, Tovey M, Lasfar A, Michiels JF et al (2007) Pentoxifylline inhibits liver expression of tumor necrosis factor alpha mRNA following normothermic ischemia–reperfusion. HPB (Oxf) 9:112–119
Yeung AC, Tsao P (2002) Statin therapy: beyond cholesterol lowering and antiinflammatory effects. Circulation 105:2937–2938
Nagasaki H, Nakano H, Boudjema K, Jaeck D, Alexandre E, Baek Y et al (1998) Efficacy of preconditioning with N-acetylcysteine against reperfusion injury after prolonged cold ischaemia in rats liver in which glutathione had been reduced by buthionine sulphoximine. Eur J Surg 164:139–146
Pérez-Ruixo JJ, Krzyzanski W, Hing J (2008) Pharmacodynamic analysis of recombinant human erythropoietin effect on reticulocyte production rate and age distribution in healthy subjects. Clin Pharmacokinet 47:399–415
Lindenblatt N, Menger MD, Klar E, Vollmar B (2007) Darbepoetin-alpha does not promote microvascular thrombus formation in mice: role of eNOS-dependent protection through platelet and endothelial cell deactivation. Arterioscler Thromb Vasc Biol 27:1191–1198
Johnson DW, Pat B, Vesey DA, Guan Z, Endre Z, Gobe GC (2006) Delayed administration of darbepoetin or erythropoietin protects against ischemic acute renal injury and failure. Kidney Int 69:1806–1813
Sepodes B, Maio R, Pinto R, Sharples E, Oliveira P, McDonald M et al (2006) Recombinant human erythropoietin protects the liver from hepatic ischemia–reperfusion injury in the rat. Transpl Int 19:919–926
Korkmaz A, Reiter RJ, Topal T, Manchester LC, Oter S, Tan DX (2009) Melatonin: an established antioxidant worthy of use in clinical trials. Mol Med 15:43–50
Kim SH, Lee SM (2008) Cytoprotective effects of melatonin against necrosis and apoptosis induced by ischemia/reperfusion injury in rat liver. J Pineal Res 44:165–171
Zhang WH, Li JY, Zhou Y (2006) Melatonin abates liver ischemia/reperfusion injury by improving the balance between nitric oxide and endothelin. Hepatobiliary Pancreat Dis Int 5:574–579
Freitas I, Bertone V, Guarnaschelli C, Ferrigno A, Boncompagni E, Rizzo V et al (2006) In situ demonstration of improvement of liver mitochondria function by melatonin after cold ischemia. In Vivo 20:229–237
Duenschede F, Westermann S, Riegler N, Miesner I, Erbes K, Ewald P et al (2006) Different protection mechanisms after pretreatment with glycine or alpha-lipoic acid in a rat model of warm hepatic ischemia. Eur Surg Res 38:503–512
Santiago Delpín EA, Figueroa I, López R, Vázquez J (1975) Protective effect of steroids on liver ischemia. Am Surg 41:683–685
Wang Y, Mathews WR, Guido DM, Jaeschke H (1996) The 21-aminosteroid tirilazad mesylate protects against liver injury via membrane stabilization not inhibition of lipid peroxidation. J Pharmacol Exp Ther 277:714–720
Chimalakonda AP, Mehvar R (2003) Effects of duration of ischemia and donor pretreatment with methylprednisolone or its macromolecular prodrug on the disposition of indocyanine green in cold-preserved rat livers. Pharm Res 20:1001–1008
Schmeding M, Neumann UP, Boas-Knoop S, Spinelli A, Neuhaus P (2007) Erythropoietin reduces ischemia–reperfusion injury in the rat liver. Eur Surg Res 39:189–197
Glanemann M, Strenziok R, Kuntze R, Münchow S, Dikopoulos N, Lippek F et al (2004) Ischemic preconditioning and methylprednisolone both equally reduce hepatic ischemia/reperfusion injury. Surgery 135:203–214
Moussavian MR, Kollmar O, Schmidt M, Scheuer C, Wagner M, Slotta JE et al (2009) Amiodarone pretreatment of organ donors exerts anti-oxidative protection but induces excretory dysfunction in liver preservation and reperfusion. Liver Transplant 15:763–775
El-Gibaly AM, Scheuer C, Menger MD, Vollmar B (2004) Improvement of rat liver graft quality by pifithrin-alpha-mediated inhibition of hepatocyte necrapoptosis. Hepatology 39:1553–1562
Rüdiger HA, Clavien PA (2002) Tumor necrosis factor alpha, but not Fas, mediates hepatocellular apoptosis in the murine ischemic liver. Gastroenterology 122:202–210
Müller JM, Vollmar B, Menger MD (1997) Pentoxifylline reduces venular leukocyte adherence (“reflow paradox”) but not microvascular “no reflow” in hepatic ischemia/reperfusion. J Surg Res 71:1–6
Colletti LM, Remick DG, Burtch GD, Kunkel SL, Strieter RM, Campbell DA Jr (1990) Role of tumor necrosis factor-alpha in the pathophysiologic alterations after hepatic ischemia/reperfusion injury in the rat. J Clin Invest 85:1936–1943
Schemmer P, Schoonhoven R, Swenberg JA, Bunzendahl H, Thurman RG (1998) Gentle in situ liver manipulation during organ harvest decreases survival after rat liver transplantation: role of Kupffer cells. Transplantation 65:1015–1020
Horimoto H, Nakai Y, Nakahara K, Nomura Y, Mieno S, Sasaki S (2002) HMG-CoA reductase inhibitor cerivastatin prolonged rat cardiac allograft survival by blocking intercellular signals. J Heart Lung Transplant 21:440–445
Inman SR, Davis NA, Olson KM, Lukaszek VA (2003) Simvastatin attenuates renal ischemia/reperfusion injury in rats administered cyclosporine A. Am J Med Sci 326:117–121
Lefer DJ (2002) Statins as potent antiinflammatory drugs. Circulation 106:2041–2042
Dold S, Laschke MW, Lavasani S, Menger MD, Jeppsson B, Thorlacius H (2009) Simvastatin protects against cholestasis-induced liver injury. Br J Pharmacol 156:466–474
Schramm R, Menger MD, Harder Y, Schmits R, Adam O, Weitz-Schmidt G et al (2007) Statins inhibit lymphocyte homing to peripheral lymph nodes. Immunology 120:315–324
Tokunaga T, Ikegami T, Yoshizumi T, Imura S, Morine Y, Shinohara H et al (2008) Beneficial effects of fluvastatin on liver microcirculation and regeneration after massive hepatectomy in rats. Dig Dis Sci 53:2989–2994
Zhang SJ, Ma TW, Ma XX, Gou JJ, Shi JH, Guo WZ (2006) Protective effects of N-acetylcysteine on brain-dead rat liver. Hepatobiliary Pancreat Dis Int 5:428–431
Koeppel TA, Lehmann TG, Thies JC, Gehrcke R, Gebhard MM, Herfarth C et al (1996) Impact of N-acetylcysteine on the hepatic microcirculation after orthotopic liver transplantation. Transplantation 61:1397–1402
Gao X, Xu X, Belmadani S, Park Y, Tang Z, Feldman AM et al (2007) TNF-alpha contributes to endothelial dysfunction by upregulating arginase in ischemia/reperfusion injury. Arterioscler Thromb Vasc Biol 27:1269–1275
Chan BP, Reichert WM, Truskey GA (2004) Effect of streptavidin–biotin on endothelial vasoregulation and leukocyte adhesion. Biomaterials 25:3951–3961
Zhang SJ, Shi JH, Tang Z, Wu Y, Chen S (2005) Protective effects of glycine pretreatment on brain-death donor liver. Hepatobiliary Pancreat Dis Int 4:37–40
Jacob T, Ascher E, Hingorani A, Kallakuri S (2003) Glycine prevents the induction of apoptosis attributed to mesenteric ischemia/reperfusion injury in a rat model. Surgery 134:457–466
Mühlbacher F, Langer F, Mittermayer C (1999) Preservation solutions for transplantation. Transplant Proc 31:2069–2070
Menger MD, Vollmar B (2007) Pathomechanisms of ischemia–reperfusion injury as the basis for novel preventive strategies. Transplant Proc 39:485–488
Moussavian MR, Slotta JE, Kollmar O, Menger MD, Gronow G, Schilling MK (2008) Post-hypoxic cellular disintegration in glycine-preserved renal tubules is attenuated by hydroxyl radical scavengers and iron chelators. Langenbecks Arch Surg 393:303–310
Moussavian MR, Slotta JE, Kollmar O, Menger MD, Schilling MK, Gronow G (2007) Hemoglobin induces cytotoxic damage of glycine-preserved renal tubules. Transpl Int 20:884–894
Le Minh K, Klemm K, Abshagen K, Eipel C, Menger MD, Vollmar B (2007) Attenuation of inflammation and apoptosis by pre- and posttreatment of darbepoetin-alpha in acute liver failure of mice. Am J Pathol 170:1954–1963
Seehofer D, Neumann UP, Schirmeier A, Carter J, Cho SY, Lederer A et al (2008) Synergistic effect of erythropoietin but not G-CSF in combination with curcumin on impaired liver regeneration in rats. Langenbecks Arch Surg 393:325–332
Acknowledgment
We appreciate the excellent technical assistance of Janine Becker and Elisabeth Gluding.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moussavian, M.R., Scheuer, C., Schmidt, M. et al. Multidrug donor preconditioning prevents cold liver preservation and reperfusion injury. Langenbecks Arch Surg 396, 231–241 (2011). https://doi.org/10.1007/s00423-010-0668-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-010-0668-4