Abstract
High-altitude ascent imposes a unique cerebrovascular challenge due to two opposing blood gas chemostimuli. Specifically, hypoxia causes cerebral vasodilation, whereas respiratory-induced hypocapnia causes vasoconstriction. The conflicting nature of these two superimposed chemostimuli presents a challenge in quantifying cerebrovascular reactivity (CVR) in chronic hypoxia. During incremental ascent to 4240 m over 7 days in the Nepal Himalaya, we aimed to (a) characterize the relationship between arterial blood gas stimuli and anterior, posterior and global (g)CBF, (b) develop a novel index to quantify cerebral blood flow (CBF) in relation to conflicting steady-state chemostimuli, and (c) assess these relationships with cerebral oxygenation (rSO2). On rest days during ascent, participants underwent supine resting measures at 1045 m (baseline), 3440 m (day 3) and 4240 m (day 7). These measures included pressure of arterial (Pa)CO2, PaO2, arterial O2 saturation (SaO2; arterial blood draws), unilateral anterior, posterior and gCBF (duplex ultrasound; internal carotid artery [ICA] and vertebral artery [VA], gCBF [{ICA + VA} × 2], respectively) and rSO2 (near-infrared spectroscopy). We developed a novel stimulus index (SI), taking into account both chemostimuli (PaCO2/SaO2). Subsequently, CBF was indexed against the SI to assess steady-state cerebrovascular responsiveness (SS-CVR). When both competing chemostimuli are taken into account, (a) SS-CVR was significantly higher in ICA, VA and gCBF at 4240 m compared to lower altitudes, (b) delta SS-CVR with ascent (1045 m vs. 4240 m) was higher in ICA vs. VA, suggesting regional differences in CBF regulation, and (c) ICA SS-CVR was strongly and positively correlated (r = 0.79) with rSO2 at 4240 m.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In humans, cerebral blood flow (CBF) is tightly regulated to ensure adequate oxygen delivery to the brain, as cerebral oxygenation is essential to maintain physiological homeostasis and meet metabolic demands. Changes in CBF are predominantly controlled by alterations in vascular smooth muscle tone, which are directly influenced by various vasodilators and vasoconstrictors (Ainslie and Ogoh 2010). Smooth muscle contraction/relaxation is mediated by endogenous/paracrine substances (e.g., nitric oxide), which are activated/inactivated in response to stressors including alterations in perfusion pressure (Lu and Kassab 2011; Kim and Baek 2011), shear stress (Lu and Kassab 2011; Rubanyi et al. 1986; Sriram et al. 2016) and the partial pressure of arterial O2 (PaO2), arterial oxygen saturation (SaO2), PaCO2, and pH (Ainslie and Subudhi 2014; Willie et al. 2012; Willie et al. 2014a, b).
With ascent to high altitude, there is a reduction in barometric pressure, and consequently oxygen availability decreases. This hypobaric hypoxia, reflected in reductions of PaO2 and SaO2, invokes a suite of physiological responses, maintaining cerebral perfusion and oxygen delivery, including cardiovascular (e.g., an acute increase in cardiac output; Naeije 2010), hematological (decreased plasma volume and increased red cell mass; Pugh 1964; Windsor and Rodway 2007), renal (acid–base compensations; Ge et al. 2006; Krapf et al. 1991; Swenson 2016; Zouboules et al. 2018) and ventilatory responses (plasticity in the hypoxic ventilatory response, HVR; Dempsey and Forster 1982; Teppema and Dahan 2010).
The larger arteries in the neck that are responsible for cerebral perfusion, including the internal carotid arteries (ICA) and vertebral arteries (VA), and particularly their downstream arterioles, are responsive to arterial blood gas perturbations (Willie et al. 2012). What is important to consider, however, is that while the HVR functions to mitigate arterial hypoxemia, it also reduces PaCO2, resulting in chronic hypocapnia and respiratory alkalosis (Bernardi et al. 2006; Teppema and Dahan 2010; Zouboules et al. 2018). Therefore, high-altitude exposure imposes a unique cerebrovascular challenge due to opposing blood gas stimuli (i.e., hypoxia and hypocapnia), as hypoxia causes cerebral vasodilation but respiratory-induced hypocapnia causes cerebral vasoconstriction (Ainslie and Subudhi 2014; Brugniaux et al. 2007; Kety and Schmidt 1948; Norcliffe et al. 2005; Xu et al. 2012). The conflicting nature of these two superimposed chemostimuli presents a challenge in the assessment and quantification of CBF responsiveness to chronic hypoxia associated with incremental ascent to high altitude. An integrative quantitative model does not yet exist.
Previous laboratory studies have demonstrated regional (i.e., anterior vs. posterior) differences in CBF regulation, where there appears to be prioritization for the maintenance of blood flow and oxygen delivery to the posterior circulation at altitude (Ainslie and Subudhi 2014; Ogoh et al. 2013; Hoiland et al. 2017). However, what is consistently lacking from these studies and others is the consideration of PaCO2 as a factor in this differential blood flow pattern between the anterior and posterior circulations. Other studies have conversely demonstrated that during progressive ascent to 5050 m, anterior vs. posterior differences do not exist (Willie et al. 2014a, b). However, Willie et al. (2014a, b) only took into account the reductions in peripheral oxygen saturation, but not the concomitant hypocapnia, which may have had a braking effect on increases in CBF with ascent. In addition, these participants were taking prophylactic acetazolamide, most likely confounding the blood gas responses associated with incremental ascent due to relative metabolic acidosis (Willie et al. 2014a, b). Thus, whether or not anterior vs. posterior differences exist upon exposure to chronic hypoxia and concomitant hypocapnia is inconclusive to date. In addition, a practical way to assess and quantify regional CBF responses that take into account both competing chemostimuli (i.e., hypoxia and hypocapnia) is currently lacking.
Given these limitations and gaps in understanding, during incremental ascent to altitude, we aimed to (a) characterize the relationship between conflicting arterial blood gas stimuli with anterior (internal carotid), posterior (vertebral) and global (g)CBF (b) develop a novel index to track changes in CBF in relation to concomitant and countervailing chemostimuli and (c) determine whether anterior vs. posterior differences in CBF regulation exist in the steady state and (d) assess these relationships with regional (anterior) cerebral oxygenation (rSO2). We hypothesized that (a) steady-state cerebrovascular responsiveness (SS-CVR) would increase in anterior, posterior and global parameters during incremental ascent to altitude, (b) anterior vs. posterior differences would persist with ascent when hypocapnia was taken into account and (c) anterior cerebrovascular responses would be related to anterior cerebral oxygenation at high altitude.
Materials and methods
Participant recruitment and ethics
Sixteen participants were recruited for the study (nine females) from a large research expedition in the Nepal Himalaya. Inclusion criteria included adult participants over 18 years of age who planned to trek the entire ascent profile and those not taking acetazolamide prophylactically. Participants were recruited via verbal communication and provided written and informed consent prior to voluntary participation in the study. No pre-existing medical conditions were reported by participants and none had previously travelled to altitudes greater than 2500 m for at least one year prior to the expedition.
This study abided by the Canadian Government Tri-Council policy on research ethics with human participants (TCPS2) and conformed with the standards set by the latest revision of the Declaration of Helsinki, except for registration in a database. Ethical approval was received in advance through the Mount Royal University Human Research Ethics Board (Protocols 100,012 and 101,012), University of Alberta Health Research Ethics Board Biomedical Panel (Protocol 00,064,195) and was harmonized with the Nepal Health Research Council (Protocol 109–2017). Although this study took place in the context of a large research expedition to altitude, the specific study design, research question, participant recruitment and data collection were planned a priori. Specifically, the arterial blood gas and electrolyte values presented here are a subset of a previously published study on acid–base responses to incremental ascent (Zouboules et al. 2018). However, these acid–base values are ancillary to the present study on cerebral blood flow and cerebral oxygenation reported here.
Data collection
Ascent to high altitude
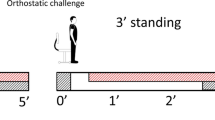
Baseline measurements were collected from 16 participants in Calgary (1045 m) prior to the departure to Nepal. Three days following arrival in Kathmandu (1400 m), they flew to Lukla (2840 m) where the trek to high altitude commenced. Consecutive measurements were obtained on rest days at 3440 m (day 3) and 4240 m (day 7) during incremental ascent, following one night at each altitude. Thus, participants avoided vigorous exercise and alcohol for at least 12 h prior to data collection and all data were collected on resting participants. In some metrics, there was a sample size decrease with ascent from n = 16 at baseline to n = 12 up to 4240 m due to difficulties in obtaining ABG and/or ultrasound measures, time constraints, illness and in one case a participant began taking acetazolamide due to the development of acute mountain sickness (see Table 1 for specific n).
Data acquisition
Data were measured continuously using an analog-to-digital data acquisition system (Powerlab/16SP ML880, ADInstruments (ADI), Colorado Springs, CO, USA). All data, except ICA and VA diameters, were analyzed offline using a commercially available software (Labchart V8; ADInstruments, Colorado Springs, CO, USA).
Heart rate and blood pressure
Following instrumentation, resting heart rate and blood pressure measurements were made during a 3-min resting baseline period. Specifically, instantaneous heart rate was measured using an electrocardiogram (FE 132 Bio Amp, ADInstruments, Colorado Springs, CO, USA; 60/period). Beat-to-beat blood pressure was measured using a finometer (Finometer Pro, Finapres Medical Systems, Amsterdam, Netherlands) calibrated for every participant using return to flow (RTF) function and three manual blood pressure measurements. MAP was calculated as the mean of the raw finometer envelope in Labchart. Heart rate and blood pressure data were averaged over the 3-min baseline period immediately prior to beginning CBF measurements to obtain the heart rate and mean arterial pressure (MAP) values from LabChart.
Arterial blood draws
Arterial blood samples were obtained from the radial artery by a trained and registered Respiratory Therapist (HEN) for partial pressure of arterial O2 [PaO2 (mmHg)], arterial oxygen saturation [SaO2 (%)], partial pressure of arterial CO2 [PaCO2 (mmHg)], arterial bicarbonate concentration [[HCO3−]a (mmol/L)], hematocrit (%), and arterial pH (pHa) (Abbott iSTAT, CG4 + and CHEM 8 + cartridges; Mississauga, Ontario, Canada; all samples subjected to thermal correction to 37 °C and atmospheric pressure calibration). Topical lidocaine was applied to all participants ~ 30 min prior to the blood draws. Arterial blood was drawn while participants were at rest, in supine position, for a minimum of 10 min. Samples were obtained between the hours of 08:00 and 16:00 on each of the data collection days.
Cerebral blood flow
CBF data were obtained from the ICA and VA by a trained and experienced sonographer using duplex ultrasound (MAJ). Following the 3-min baseline period in supine position at rest, cerebrovascular measurements began. Continuous unilateral blood velocity and diameter recordings were measured in the ICA and VA using a multi-frequency linear array transducer (6.0–13.0 MHz multi-frequency linear array probe, 12L-RS H40402LY, GE Healthcare, Wauwatosa, WI, USA) attached to a Duplex vascular ultrasound machine (Vivid q cardiovascular ultrasound system, GE Healthcare, Wauwatosa, WI, USA). The right ICA was measured first in all participants, and was located at least 2 cm distal to the carotid bifurcation. The right VA was then measured between C4 and C6, and was always measured at the same location within participants. The ICA and VA peak velocity envelopes were recorded into LabChart and averaged over 1 min following the initial baseline period. Subsequently, three vascular images of the ICA and VA diameters were taken in both systole and diastole, in three different cardiac cycles during the same analysis window as the mean velocity bin. Extracranial vascular images were stored for offline analysis to obtain ICA and VA diameters.
Cerebral oximetry
During the same measurement period as the CBF measures, a portable near-infrared spectroscopy (NIRS) system was utilized to measure regional cerebral oxygen saturation (rSO2; anterior only; see Bakker et al. 2012 for NIRS review; INVOS 5100 cerebral oximeter (Somanetics Corp, Troy, MI, USA). Prior to the application of the sensor, the forehead skin was cleaned. The sensor was positioned so that the medial margin of the sensor was at the midline of the forehead and the lower margin was 2 cm above the eyebrow (Hadolt and Litscher 2003). To minimize the effect of ambient light, the forehead was covered by a black opaque material, which was secured over the sensor by a black bandana. Cerebral oxygenation was assessed throughout a 3-min block every 5 s, which coincided with the CBF measurements, on the ipsilateral side as the ICA measurement. Mean rSO2 over the course of the 3-min supine rest was taken to represent resting regional cerebral oxygenation.
Data analysis
Arterial blood variables
Absolute values of PaO2, SaO2, PaCO2, [HCO3−]a, hematocrit and pHa were inputted, analyzed and plotted in Microsoft Excel. As CBF is linearly and directly proportional to PaCO2 (i.e., CBF ∝ PaCO2) and CBF is linearly and inversely proportional to SaO2 (i.e., CBF ∝ 1/SaO2), the combined influence of PaCO2 and SaO2 on CBF was assessed using a novel stimulus index (SI; see Bruce et al. 2016), which was calculated at each altitude using the following equation:
Cerebral blood flow (CBF) and steady-state cerebrovascular reactivity (SS-CVR)
Ultrasound images of the ICA and VA were analyzed offline by a trained sonographer to obtain the vessel diameters. Using the measured ICA and VA diameters, the average diameter of each vessel was calculated as
The cross-sectional area of each vessel was then calculated as
Flow in the right ICA and VA was calculated as
where CBF is the flow measured in the ICA or VA and v is the peak envelope velocity in the corresponding vessel.
Absolute values of ICA blood flow, VA blood flow and gCBF were analyzed and plotted accordingly, with gCBF calculated as
To track the responsiveness of the cerebrovasculature to changes in both the relevant chemostimuli (i.e., CO2 and O2) throughout ascent, an index termed steady-state cerebrovascular responsiveness (SS-CVR) was calculated as
where CBF was ICA blood flow and VA was blood flow or gCBF.
Cerebrovascular conductance (CVC) and steady-state cerebrovascular conductance reactivity (SS-CVCR)
In accordance with Ohm’s law, cerebrovascular conductance (CVC) was calculated as
where CBF was ICA blood flow and VA was blood flow or gCBF.
To assess the changes in vessel conductance in response to changes in both the chemostimuli (i.e., O2 and CO2) throughout ascent, an index termed steady-state cerebrovascular conductance reactivity (SS-CVCR) was created and calculated as
where conductance was CVCICA, CVCVA or gCVC.
Anterior vs. posterior differences
To assess if anterior vs. posterior differences existed between the ICA and VA during ascent, absolute deltas and percent changes at 4240 m compared to baseline (1045 m) were calculated and compared for CBF, SS-CVR, CVC and SS-CVCR.
Arterial oxygen content and delivery
Arterial oxygen content (CaO2) was calculated as
where 1.34 is the Hüfner number, or binding capacity of oxygen to hemoglobin, and 0.003 × PaO2 accounts for the net solubility of O2 per dL of blood (ml/dl).
where anterior, posterior or gCBF (ml/min) was multiplied by CaO2 (ml/dl) to calculate the cerebral oxygen delivery in ml/min.
Cerebral oximetry
Mean rSO2 values were input, analyzed and plotted in Excel. Relationships between CBFICA, SS-CVRICA, CVCICA and SS-CVCICA and rSO2 were assessed to determine their respective contributions to the maintenance of anterior cerebral oxygenation. The correlations were performed at 4240 m using only the ipsilateral and unilateral ICA, as the cerebral oximeter measured only unilateral anterior rSO2.
Statistical analysis
The final analysis included all available data at each altitude. A Shapiro–Wilk test was used to confirm normal distribution of variables. The Brown–Forsythe test was used as an equal variance test. One-way repeated-measures analysis of variance (ANOVA) tests were performed on the arterial blood, ancillary measures, CBF and cerebral oximetry data analyzed at different altitudes (Table 1). The ANOVA eliminated individuals who dropped out during ascent through list-wise deletion. The Student–Newman–Keuls post hoc test was used for multiple comparisons between the various altitudes, where necessary. A paired t test was performed between the absolute deltas and percent changes of the ICA and VA for CBF, SS-CVR, CVC and SS-CVCR. A Pearson correlation coefficient test was used to assess linear relationships between anterior DO2, CBFICA, SS-CVRICA, CVCICA and SS-CVCICA and rSO2. Values are reported as mean ± standard deviation (SD). Statistical significance was assumed when P < 0.05 (SigmaPlot v14, Systat, San Jose, CA, USA).
Results
Participants
The study included 16 adults (9 female) with a mean age of 24.7 ± 7.2 years and body mass index (BMI) of 24.1 ± 3.9 kg/m2. All 16 participants completed all baseline measurements in Calgary (1045 m).
Changes in arterial blood gas and electrolytes
As expected, PaO2, SaO2 and PaCO2 decreased significantly at both 3440 m and 4240 m compared to baseline at 1045 m (all P < 0.001). In addition, arterial bicarbonate ([HCO3−]a) decreased significantly at both altitudes compared to baseline, keeping pHa constant with ascent. Oxygen content was statistically lower at both 3440 m and 4240 m with ascent (P < 0.001). Oxygen delivery was statistically unchanged in anterior, posterior and global CBF with ascent (P = 0.067, P = 0.43 and P = 0.073, respectively). Figure 1a, b illustrates the decrease in PaCO2 and SaO2 with ascent; however, the SI shows no significant change with ascent (Fig. 1c; P = 0.07 at 4240 m compared to baseline).
Relationship between arterial blood gas variables with ascent. a Arterial partial pressure of CO2 (PaCO2; Torr). b Arterial saturation of O2 (SaO2; %). c Stimulus Index (SI; PaCO2/SaO2; a.u.). Black circles represent mean values and grey circles are individual data. Values reported for 1045 m (day 0), 3440 m (day 3) and 4240 m (day 7). *Difference in mean from baseline (1045 m), P < 0.05. †Difference in mean from previous altitude, P < 0.05
Changes in regional and global cerebral blood flow (CBF) with ascent
The mean diameter of the ICA was 0.48 ± 0.05 cm, 0.52 ± 0.06 cm and 0.51 ± 0.07 cm at 1045 m, 3440 m and 4240 m, respectively. There were no significant differences in the mean ICA diameter at either altitude compared to baseline. The mean diameter of the VA was 0.34 ± 0.07 cm, 0.34 ± 0.06 cm and 0.35 ± 0.05 cm at 1045 m, 3440 m and 4240 m, respectively. There were no significant differences in the mean VA diameter at either altitude compared to baseline.
Absolute values of mean anterior (ICA) CBF were calculated to be 262.8 ± 57.2 ml/min, 301.7 ± 101.6 ml/min and 344.6 ± 84.7 ml/min at 1045 m, 3440 m and 4240 m, respectively. Mean posterior (VA) CBF was 81.0 ± 38.6 ml/min, 90.9 ± 36.5 ml/min and 103.2 ± 41.8 ml/min at 1045 m, 3440 m and 4240 m, respectively. Mean gCBF was 699.7 ± 101.3 ml/min, 785.3 ± 186.6 ml/min and 906.0 ± 204.3 ml/min at 1045 m, 3440 m and 4240 m, respectively. Anterior (ICA), posterior (VA) and gCBF were significantly increased at 4240 m compared to baseline (all P = 0.02).
Mean anterior (ICA) steady-state cerebrovascular reactivity (SS-CVR) was calculated to be 753.8 ± 170.0, 874.8 ± 371.4 and 1081.1 ± 232.7 ml/min/SI at 1045 m, 3440 m and 4240 m, respectively. Mean posterior (VA) SS-CVR was 226.9 ± 109.5, 262.7 ± 98.0 and 334.7 ± 125.7 ml/min/SI at 1045 m, 3440 m and 4240 m, respectively. Mean global SS-CVR was 2005.6 ± 299.3, 2274.9 ± 762.3 and 2879.5 ± 489.8 ml/min/SI at 1045 m, 3440 m and 4240 m, respectively. Both regional and global SS-CVR were significantly increased at 4240 m compared to baseline (1045 m; all P < 0.01) and to the previous altitude of 3440 m (all P < 0.01).
Changes in cerebrovascular conductance (CVC) with ascent
Changes in regional and global cerebrovascular conductance (CVC) and steady-state cerebrovascular conductance reactivity (SS-CVCR) during incremental ascent are presented in Fig. 2. To take into account potential changes in MAP with ascent, mean anterior (ICA) CVC was calculated to be 2.9 ± 0.7, 3.4 ± 1.2 and 4.1 ± 1.0 ml/min/mmHg at 1045 m, 3440 m and 4240 m, respectively. Mean posterior (VA) CVC was 0.9 ± 0.5, 1.0 ± 0.5 and 1.2 ± 0.5 ml/min/mmHg at 1045 m, 3440 m and 4240 m, respectively. Mean global CVC was 7.7 ± 1.4, 8.8 ± 2.4 and 10.7 ± 2.5 ml/min/mmHg at 1045 m, 3440 m and 4240 m, respectively. Both regional and global CVC were significantly increased at 4240 m in comparison to baseline (all P < 0.02). Additionally, global CVC was significantly increased at 4240 m in comparison to the previous altitude at 3440 m (P = 0.04).
Changes in regional and global cerebral blood flow (CBF), steady-state cerebrovascular reactivity (SS-CVR), cerebrovascular conductance (CVC) and steady-state cerebrovascular conductance reactivity (SS-CVCR) with ascent. a Anterior (internal carotid artery; ICA; white), posterior (vertebral artery; VA; black) and global (g)CBF (grey). b ICA, VA and global steady-state cerebrovascular reactivity (SS-CVR). c ICA, VA and global CVC. d ICA, VA and global steady-state cerebrovascular conductance reactivity (SS-CVCR). All bar graphs illustrate mean values and the error bars represent the corresponding standard deviations. All graphs demonstrate an incremental ascent profile in which 1045 m, 3440 m and 4240 m correspond to day 0, 3 and 7 days of altitude exposure. *Significantly different from baseline (1045 m), P < 0.05. †Significantly different from previous altitude, P < 0.05
Mean anterior (ICA) SS-CVCR was determined to be 8.4 ± 2.3, 9.9 ± 4.4 and 12.8 ± 3.1 ml/min/mmHg/SI at 1045 m, 3440 m and 4240 m, respectively. Mean posterior (VA) SS-CVCR was 2.5 ± 1.3, 3.0 ± 1.3 and 4.0 ± 1.7 ml/min/mmHg/SI at 1045 m, 3440 m and 4240 m, respectively. Mean global SS-CVCR was 22.3 ± 4.8, 25.7 ± 9.4 and 34.1 ± 7.3 ml/min/mmHg/SI at 1045 m, 3440 m and 4240 m, respectively. Both regional and global SS-CVCR were significantly increased at 4240 m compared to baseline (all P < 0.01) and to the previous altitude at 3440 m (all P < 0.03).
Regional differences
Figure 3 demonstrates the absolute change and percent change in the ICA and VA metrics (CBF, SS-CVR, CVC and SS-CVCR) at 4240 m in comparison to baseline at 1045 m.
Assessing regional differences via absolute and percent change in cerebral blood flow (CBF), steady-state cerebrovascular reactivity (SS-CVR), cerebrovascular conductance (CVC) and steady-state cerebrovascular conductance reactivity (SS-CVCR) with ascent. Absolute values (delta) and percent change were calculated for the internal carotid artery (ICA) and the vertebral artery (VA) at 4240 m in comparison to baseline (1045 m). a Absolute values for mean ICA vs. VA CBF from baseline. b Percent change for mean CBF from baseline (ICA vs. VA). c Absolute values for mean ICA vs. VA SS-CVR from baseline. d Percent change for mean ICA vs. VA SS-CVR from baseline. e Absolute values for mean ICA vs. VA CVC from baseline. f Percent change for mean ICA vs. VA CVC from baseline. g Absolute values for mean ICA vs. VA SS-CVCR from baseline. h Percent change for mean ICA vs. VA SS-CVCR from baseline (ICA vs. VA). *Significantly different between mean ICA and mean VA, P < 0.05
With respect to CBF, ICA increased by 79.4 ± 92.8 ml/min (35.0 ± 36.5%) and VA increased by 18.4 ± 25.6 ml/min (29.6 ± 38.7%). There were no significant differences observed in the absolute change or percent increases between the two vessels (P = 0.053 and P = 0.5, respectively).
For SS-CVR, the ICA increased by 349.9 ± 231.5 (53.7 ± 41.4%), while the VA increased by 76.3 ± 62.2 (35.2 ± 37.7%). There was no significant difference observed in the percent increases in SS-CVR between the two vessels (P = 0.07). However, the absolute increase in SS-CVR for the ICA was significant larger than the increase observed in the VA (P < 0.01).
CVC of the ICA increased by 1.1 ± 1.2 (44.7 ± 47.5%), while CVC of the VA increased by 0.3 ± 0.3 (36.2 ± 43.4%). There was no significant difference observed in the percent increases between the two vessels (P = 0.5). However, the absolute increase in CVC for the ICA was significantly larger than the absolute increase of the CVC of the VA (P < 0.05).
SS-CVCR of the ICA increased by 4.6 ± 3.3 (65.5 ± 58.2%), while SS-CVCR of the VA increased by 1.0 ± 0.9 (41.6 ± 43.8%). There was no significant difference observed in the percent increases between the two vessels (P = 0.06). However, the absolute increase in SS-CVCR of the ICA was significantly higher than the absolute increase of the SS-CVCR for the VA (P < 0.05).
Arterial oxygen content, cerebral oxygen delivery and cerebral oxygen saturation
Figure 4 demonstrates changes and relationships in CaO2, DO2 and rSO2 with ascent. CaO2 was significantly decreased in comparison to baseline at both 3440 m and 4240 m (both P < 0.02). Anterior DO2 was not significantly changed across all altitudes (P = 0.067). Anterior rSO2 was significantly decreased in comparison to baseline at both 3440 m and 4240 m (both P < 0.01). However, there was no further significant decrease in rSO2 observed at 4240 m compared to the previous altitude of 3440 m (P = 0.18). There was a strong positive correlation between anterior DO2 and rSO2 at 4240 m (r = 0.85, P = 0.002).
Changes in arterial oxygen content, delivery and cerebral oxygenation with ascent. a Arterial oxygen content (CaO2; mL/dL), calculated from [Hb], PaO2 and SaO2 from radial artery blood draws (see Methods). b Anterior cerebral oxygen delivery (DO2; mL/min) calculated from CaO2 in a and anterior cerebral blood flow in Fig. 2a. c Measurement of anterior (rSO2) cerebral oxygenation (see “Materials and methods”). d Correlation between anterior DO2 and rSO2 at 4240 m (day 7 at altitude). Black circles represent mean values and grey circles are individual data. Values reported for 1045 m (day 0), 3440 m (day 3) and 4240 m (day 7). *Significantly different from baseline (1045 m), P < 0.05. For correlation in d, representative r, P and n values are reported in graph
Figure 5 illustrates correlations between rSO2 versus CBFICA, SS-CVRICA, CVCICA and SS-CVCRICA. Moderate to strong correlations were observed in all cases; however, correlations with the derived indices SS-CVR and SS-CVCR had stronger correlations compared to their corresponding cerebrovascular parameters, CBF and CVC, respectively. Specifically, Pearson correlation coefficients (r) were 0.64 (P = 0.02), 0.79 (P = 0.006), 0.69 (P = 0.01) and 0.73 (P = 0.02) for CBFICA, SS-CVRICA, CVCICA and SS-CVCICA, respectively.
Relationship between regional (anterior) cerebral oxygenation (rSO2) and metrics of anterior (ICA) CBF at 4240 m (day 7 at altitude). a rSO2 as a function of ICA CBF. b rSO2 as a function of ICA steady-state cerebrovascular responsiveness (SS-CVR). c rSO2 as a function of ICA cerebrovascular conductance (CVC). d rSO2 as a function of ICA steady-state cerebrovascular conductance reactivity (SS-CVCR). Respective correlation coefficients (r), P values and n reported on each panel
Discussion
During an incremental ascent to high altitude, we aimed to assess the changes in regional and global (g)CBF and cerebrovascular conductance (CVC) while taking into account the simultaneous and competing chemostimuli (i.e., hypoxia and hypocapnia) via the development of novel steady-state indices: steady-state cerebrovascular reactivity (SS-CVR) and steady-state cerebrovascular conductance reactivity (SS-CVCR). Additionally, we aimed to investigate the potential for regional differences between the ICA and VA during incremental ascent to moderate altitude. Lastly, we aimed to assess the relationship between our novel indices of CBF regulation on cerebral oxygenation (rSO2) at 4240 m, where participants were most hypoxic. The principal findings were as follows: (1) both regional and global CBF and SS-CVR were significantly increased at 4240 m compared to baseline while regional and global SS-CVR were also increased at 4240 m compared to 3440 m, (2) both regional and global CVC and SS-CVCR were significantly increased at 4240 m compared to baseline; however, a further significant increase was observed in global CVC, along with both regional and global SS-CVCR at 4240 m in comparison to the previous altitude of 3440 m (3) the potential for regional differences between the ICA and VA in all CBF metrics exist when analyzing the data in absolute terms; however, there are no significant differences when analyzing the data using percent change, and (4) both the derived indices, SS-CVR and SS-CVCR, exhibit stronger correlations with rSO2 compared to their original parameters, CBF and CVC, respectively.
Blood gas perturbations at altitude
As expected, we observed the development of hypoxia and hypocapnia with ascent, evidenced by arterial blood gas values, whereby PaCO2, PaO2 and SaO2 all significantly decreased during incremental ascent to 4240 m. With ascent to moderate altitude, barometric pressure is reduced, and consequently oxygen availability is also reduced. This hypobaric hypoxia stimulates oxygen-sensitive peripheral chemoreceptors found in the carotid bodies (Prabhakar 2000). Sensory chemoreceptors found within the carotid bodies detect the resultant decrease in arterial oxygen (PaO2) and synapse with neurons within the brain stem to increase ventilation and thus increase PaO2 levels (Dempsey et al. 2014), a phenomenon commonly referred to as the HVR (Dempsey and Forster 1982; Teppema and Dahan 2010). The HVR partially corrects PaO2 levels; however, a decrease in PaCO2 results, which decreases the sensitivity of both central and peripheral respiratory chemoreceptors. Thus, to increase PaO2 levels during ascent to altitude, the decreased central and peripheral chemoreceptor sensitivity must be countered, which is achieved by increasing the HVR sensitivity through carotid body plasticity (Dempsey et al. 2014). Together, the HVR increases PaO2 levels, but also results in decreased PaCO2 levels, known as hypoxic-induced hypocapnia (i.e., respiratory alkalosis). We used a stimulus index (SI), which was previously developed by Bruce et al. (2016) to quantify the magnitude of cerebrovascular reactivity in regional cerebral circulations during breath holding that takes into account both chemostimuli (PaCO2/SaO2). We found no significant change in the SI at either altitude (3440 m and 4240 m) compared to baseline (1045 m) when analyzing these ABG parameters, highlighting the competing nature of the two chemostimuli.
Cerebrovascular responses
Cerebral blood flow and cerebrovascular reactivity
The cerebral vasculature is highly responsive to changes in arterial blood gases and thus our study provides an advantage as we collected arterial blood gases, providing an accurate representation of the proximal stimulus that affects cerebrovascular changes with ascent. We assessed global CBF using two large conduit arteries in the neck, namely the ICA and VA. The ICA is responsible for anterior cerebral perfusion and contributes ~ 70% global cerebral blood flow (gCBF), whereas the VA is responsible for posterior cerebral perfusion and contributes ~ 30% of gCBF (Tymko et al. 2018; Willie et al. 2014a, b; Zarrinkoob et al. 2015).
It has been well established that increases in CBF reflect the severity of the hypoxic stimulus, which is achieved via arteriolar smooth muscle relaxation and vessel dilation (Hoiland et al. 2016). Specifically, hypoxia does not exert a substantial influence on CBF until reaching the steeper portion of the oxyhemoglobin dissociation curve in which PaO2 drops to < 60 mmHg (Willie et al. 2014a, b; Hoiland et al. 2016; Ainslie and Poulin 2004). This is often referred to as the “threshold phenomenon” in which the competing chemostimuli stabilize CBF, whereby the vasoconstrictive effect of hypocapnia counters the vasodilatory effects of hypoxia (Ainslie and Poulin 2004). In our study, we observed a decrease in SaO2 from 96.6 ± 1.5 at baseline to 85.2 ± 3.9 at 4240 m, with a corresponding PaO2 from 84.2 ± 8.4 mmHg at baseline to 49.0 ± 5.2 mmHg at 4240 m. Our observed decreases in SaO2 and PaO2 suggest we reached the hypoxic stimulus “threshold” at 4240 m, resulting in increased CBF, evidenced by a significant increase in anterior, posterior and gCBF at 4240 m compared to baseline at 1045 m. This finding parallels the previous literature in which CBF increases with ascent (Willie et al. 2012, 2014a, b, 2015; Faraci et al. 1987). However, the extent to which CBF increases with ascent (both regional and global) may differ compared to previous studies due to methodological differences, such as inducing isobaric hypoxia in the laboratory (e.g., Willie et al. 2012), along with the extensive inter-individual variability in time course and magnitude of CBF responses at altitude (Willie et al. 2014a, b).
We developed a novel index we term steady-state cerebrovascular reactivity (SS-CVR), which takes into account the simultaneous and competing chemostimuli present during ascent to altitude. Similar to CBF, we found a significant increase in both regional and global SS-CVR at 4240 m compared to baseline. However, we found a further significant increase in both regional and global SS-CVR at 4240 m compared to the previous altitude of 3440 m. Thus, our index may be a useful tool in assessing cerebrovascular acclimatization during incremental ascent to altitude.
Our index indicates, given the countervailing vasomotor influences of SaO2 and PaCO2, that there was no statistical change in the mean net cerebrovascular stimulus (i.e., SI) at either altitude compared to baseline (1045 m). As a result, changes in CBF may be due to alterations in cerebrovascular reactivity at altitude. Changes in both hypocapnic and hypoxic cerebrovascular reactivity have been observed at altitude (reviewed in Hoiland et al. 2018), but only limited data are available. Cerebrovascular hypoxic reactivity appears increased at altitude (Jensen et al. 1996), a finding corroborated by laboratory studies (Poulin et al. 2002). This increase in hypoxic reactivity could contribute to the increased SS-CVR observed in the present study. What appears less clear is how changes in hypocapnic reactivity may influence SS-CVR. Increases in or no change in hypocapnic reactivity has both been demonstrated following ascent to altitude (Flück et al. 2015). When indexed against hydrogen ion concentration, hypocapnic reactivity still appears unaltered (Willie et al. 2015). An elevated hypocapnic reactivity (i.e., greater vasoconstriction) could reduce the SS-CVR. However, even if hypocapnic reactivity was elevated in our participants, competing changes in hypoxic reactivity were of a great enough magnitude to increase the net SS-CVR. As it is the net vasomotor response, derived from the balance of hypoxic vasodilation and hypocapnic vasoconstriction that ultimately governs perfusion, our SS-CVR index provides utility in quantifying the cerebrovascular changes that determine cerebral oxygen homeostasis.
Cerebrovascular conductance and cerebrovascular conductance reactivity
CBF regulation is largely influenced by cerebrovascular resistance (Willie et al. 2014a, b), in which contraction of smooth muscle (i.e., vasoconstriction) increases resistance, while relaxation of smooth muscle (i.e., vasodilation) decreases resistance. It is widely accepted that the pial arterioles, located in the subarachnoid space, play a large role in modulating cerebrovascular resistance (Willie et al. 2014a, b). However, several animal models have demonstrated that the larger arteries in the neck (ICA and VA) may also play a key role in modulating cerebrovascular resistance (Faraci et al. 1987). Additionally, Lewis et al. (2014) found a significant increase in the arterial diameter of the ICA and VA in response to poikilocapnic hypoxia compared to breathing room air. In our study, we did not observe a significant increase in the arterial diameter of the ICA or VA at either altitude compared to baseline. We suggest the diameter of the ICA and VA are unchanged during incremental ascent due to the competing hypoxia and hypocapnia, whereby the vasodilatory effect of hypoxia is nullified by the vasoconstriction of hypocapnia. Thus, we suggest that although vasodilatory effects have been measured in the extracranial vessels (ICA and VA) during hypoxia-induced protocols (normobaric conditions), the same is not true for progressive ascent protocols (hypobaric conditions).
Furthermore, we assessed cerebrovascular conductance (CVC; inverse of resistance) and found significant increases in both regional and global CVC at 4240 m compared to baseline, suggesting cerebrovascular resistance decreases with ascent, enabling the vasodilatory effects associated with hypoxia. In addition, we found a significant increase of global CVC at 4240 m compared to the previous altitude of 3440 m.
Similar to our previous index (SS-CVR), we developed another novel index derived from CVC called steady-state cerebrovascular conductance reactivity (SS-CVCR), which also takes into account not only the competing and simultaneous chemostimuli present during ascent to altitude but also MAP by indexing CVC to the SI. Similar to SS-CVR, we found a significant increase in both anterior, posterior and global SS-CVCR at 4240 m compared to baseline, along with a further significant increase compared to the previous altitude of 3440 m, and thus may be another useful tool in assessing integrated cerebrovascular responses during ascent to altitude.
Regional (anterior vs. posterior) differences
An important physiological question that remains unanswered is whether or not regional differences in CBF exist in response to either acute or chronic hypoxia. Specifically, whether hypoxia elicits a greater response in either anterior perfusion to cortical areas (ICA) or posterior perfusion to the brain stem (VA) is unclear. Although a substantial number of studies have addressed this question (Willie et al. 2012; Ogoh et al. 2013; Hoiland et al. 2015; Binks et al. 2008), the findings remain inconclusive, likely due to methodological differences (e.g., absolute vs. relative quantification). Several laboratory-based studies utilizing an isocapnic hypoxia stimulus have found that cerebrovascular reactivity to hypoxia is greater in the posterior circulation compared to the anterior circulation, and suggest this may occur to maintain the vital homeostatic functions of the brainstem (Ainslie and Subudhi 2014; Ogoh et al. 2013; Binks et al. 2008). Limited data exist on volumetric flow during poikilocapnic (thus hypocapnic) normobaric hypoxia. Lewis et al. (2014) demonstrated that the posterior CBF (i.e., VA) response to hypoxia was greater than that of the anterior circulation (i.e., ICA). In addition to the greater posterior CBF response, Lewis et al. (2014) also demonstrated a higher relationship between VA and SaO2 than that of ICA and SaO2. This was interpreted to also support a greater posterior CBF reactivity to hypoxia. However, all of these studies employed a normobaric hypoxia-induced laboratory model, with those employing poikilocapnic hypoxia not considering the concomitant hypocapnia in their consideration of regional reactivity. When regional differences were assessed during incremental ascent to high altitude, Willie et al. (2014a, b) did not observe such regional differences when assessing regional differences using percent change. However, Willie et al. (2014a, b) only took into account the reductions in oxygen saturation, but not the concomitant hypocapnia, which may have had a braking effect on increases in CBF with ascent. In addition, these participants were taking prophylactic acetazolamide, which likely influenced the cerebrovascular responses observed (Willie et al. 2014a, b). Thus, our study is one of the first to investigate anterior vs. posterior differences in CBF during an incremental ascent profile to moderate altitude in the absence of any high-altitude prophylactic medication (e.g., acetazolamide), with the effects of both O2 and CO2 accounted for in quantification.
We assessed anterior vs. posterior differences in responses during ascent between the ICA and VA in the following four parameters: CBF, SS-CVR, CVC and SS-CVCR. These regional differences were assessed using both absolute change and percent change (1045–4240 m). Regarding CBF, we found no significant difference between the ICA and VA when analyzing the data using both absolute change and percent change, although the P value was at the statistical threshold for absolute ICA being larger (Fig. 3a; P = 0.053). However, the trend was consistent for SS-CVR, CVC and SS-CVCR in which the ICA demonstrated a significantly increased response compared to the VA when analyzing the data using absolute changes. No significant differences were found in any of the parameters when analyzing the data using relative changes (i.e., percent change), illustrating the importance of addressing quantification method in assessing physiological phenomenon.
Skow et al. (2013) reported similar results when assessing regional differences in cerebrovascular CO2 reactivity, whereby regional differences were observed when analyzed in absolute terms, yet absent when values were normalized to baseline values when analyzing in relative terms. The discrepancies between absolute and relative changes may contribute to the inconsistency in the literature regarding anterior vs. posterior differences in CBF regulation and thus highlight the importance in reporting both to draw consistent conclusions.
Our data suggest that differences between the ICA and VA may exist in which the ICA demonstrates an increased absolute response to hypobaric poikilocapnic hypoxia compared to the VA during incremental ascent. However, it appears that anterior vs. posterior differences may be time course dependent, whereby laboratory studies that induce acute normobaric hypoxia observe increased posterior (VA) cerebral perfusion to the brainstem. In addition, Subudhi et al. (2014) observed increased cerebral oxygen delivery in the VA compared to the ICA upon rapid ascent to 5260 m. The extent to which regional and global CBF responds to a hypoxic stimulus is not only dependent on the ascent profile, but is also dependent on time in regard to acute versus chronic exposure. For example, Lawley et al. (2017) demonstrated that CBF increases upon acute exposure to hypoxia (following 2 h of poikilocapnic normobaric hypoxia), yet both anterior and posterior CBF decreased following chronic exposure to hypoxia (following 10 h of poikilocapnic normobaric hypoxia). Thus, we conclude that detecting anterior vs. posterior differences in CBF regulation depends on whether the study utilizes an incremental or rapid ascent profile, takes into account competing chemostimuli and/or utilizes absolute vs. normalized qualification methods. However, future studies are needed to reconcile these discrepancies and to investigate the role anterior vs. posterior differences in CBF play during both incremental and rapid ascent profiles to further understand the time course dependency and the potential adaptive responses behind each.
Arterial oxygen content and cerebral oxygenation
As PaO2 dictates the driving force of oxygen into the tissue, it is often considered the primary stimulus for hypoxic cerebral vasodilation; however, it is becoming more apparent that CaO2 is the primary determinant of hypoxic vasodilation (Brown et al. 1985). This is likely due to deoxyhemoglobin-mediated signaling [reviewed in Hoiland et al. 2016] and is in agreement with the operation of this mechanism in the systemic circulation (Roach et al. 1999; Gonzalez-Alonso et al. 2001). Increased CBF in response to reductions in CaO2 at altitude occurs as a compensatory mechanism to maintain cerebral oxygen delivery (Ainslie and Subudhi 2014). Here, we found that increases in CBF were indeed of an adequate magnitude to offset the arterial hypoxemia and maintain constant cerebral oxygen delivery.
Modulation of CBF with ascent serves as a compensatory process to maintain adequate cerebral perfusion, as sufficient rSO2 is essential in maintaining physiological homeostasis. In our study, we found a significant decrease in rSO2 at both 3440 m and 4240 m compared to baseline. However, rSO2 was not different between 3440 and 4240 m, likely due to maintained DO2 (see Fig. 4b), as well as increases in CBF regulation, evidenced by the significant increase in SS-CVR at 4240 m compared to the previous altitude of 3440 m. The subsequent increase of SS-CVR at 4240 m reflects the further increase of CBF required to maintain rSO2.
We also assessed the relationship between rSO2 and various anterior cerebrovascular parameters: CBFICA, SS-CVRICA, CVCICA and SS-CVCRICA. Only anterior (ICA) cerebrovascular parameters were used to correlate with rSO2 because the device used to measure rSO2 was placed on the anterior region of the cerebrum, ipsilateral to the ICA ultrasound measurement. Moderate to strong correlations were observed in all cases. However, correlations with the derived indices, SS-CVR and SS-CVCR, provided stronger correlations compared than their corresponding cerebrovascular parameters, CBF and CVC, respectively. This is in contrast to previous studies using at altitude using cerebral blood velocity (e.g., Feddersen et al. 2015), where correlations between rSO2 and anterior CBV were not observed. This finding emphasizes the utility of our derived indices in assessing the maintenance of cerebral oxygenation during ascent to altitude, and potentially the differences between measuring velocity and volumetric flow. Previous studies have assessed cerebral oxygenation using the same Invos 5100 cerebral oximeter system (Feddersen et al. 2015), with similar values at comparable altitudes, and thus it appears to be a feasible tool in high-altitude hypoxia research.
Stimulus index validity
The aim of our novel indices, SS-CVR and SS-CVCR, was to more accurately quantify CBF regulation in terms of both competing chemostimuli (i.e., O2 and CO2). The basis of these indices is derived from a stimulus index (PaCO2/SaO2), which was developed and calculated in accordance to the relationship between PaCO2 and SaO2 to CBF. Specifically, PaCO2 is directly and linearly proportional to CBF (i.e., PaCO2 ∝ CBF) and SaO2 is inversely and linearly proportional to CBF (i.e., 1/SaO2 ∝ CBF), and thus the combined influence of PaCO2 and SaO2 on CBF can be assessed using the stimulus index. We also calculated SI as H+/CaO2 (data not shown), and found no differences in the utility of these two expressions of CO2 and O2, likely given that (a) pH was unchanged with ascent due to metabolic compensation (see Table 1) and CaO2 showed the same trends as SaO2 (see Fig. 4a compared to Fig. 1b).
Not only can the stimulus index be validated theoretically, but also has been used in a previous study by Bruce et al. (2016) in which the stimulus index was used to quantify the magnitude of regional cerebrovascular reactivity during breath holding. In agreement with Bruce et al. (2016), we suggest the utility of SI lies in its ability to take into account both CO2 and O2 and the counteracting influences they exert on the net CBF when both variables are changing simultaneously. In addition, previous reports from our group have utilized the SI in assessing steady-state chemoreflex drive in laboratory and high-altitude hypoxia (Pfoh et al. 2017; Bruce et al. 2018).
Significance and future directions
The Sagarmatha National Park, where the Everest Base Camp trek is located, is visited by ~ 45,000 trekkers per year (Sagarmatha National Park Office 2017). High-altitude trekking and climbing is becoming increasingly popular and thus it is necessary to continue to gain further understanding regarding the integrated responses to incremental hypoxia in healthy lowlanders. Our incremental ascent model represents a “real world” ascent profile that is applicable to large numbers of trekkers, many of whom experience acute mountain sickness, pulmonary edema, and cerebral edema.
Furthermore, investigating the cerebrovasculature in response to various arterial blood gases stimuli is extremely important, as these gases represent the actual cerebrovascular chemostimuli, as opposed to more distal metrics of end-tidal gases and/or peripheral oxygen saturation. Incremental ascent to high altitude is an appropriate model to investigate the acute and chronic cerebrovascular effects of reduced O2 availability and provides insight into the various physiological responses and compensations required to maintain cerebral oxygenation with incremental reductions in oxygen.
Conclusions
Incremental ascent to moderate altitude imposes a unique cerebrovascular challenge due to the presentation of two simultaneous but countervailing chemostimuli, specifically hypoxia and hypocapnia. Our study aimed to characterize anterior, posterior and global CBF and CVC using arterial blood gas measurements during incremental ascent to moderate altitude. We developed two novel indices, steady-state cerebrovascular reactivity (SS-CVR) and steady-state cerebrovascular conductance reactivity (SS-CVCR), that take into account both competing chemostimuli (i.e., O2 and CO2) and serve to track cerebrovascular changes in response to incremental and chronic hypobaric hypoxic exposure. The principal findings of our study were as follows (1) anterior, posterior and global CBF, SS-CVR, CVC and SS-CVCR were significantly increased at 4240 m compared to baseline. However, further significant increases were observed in regional and global SS-CVR and SS-CVCR at 4240 m in comparison to the previous altitude of 3440 m; (2) the potential for anterior vs. posterior differences between the ICA and VA exists (ICA are larger) when assessing responses in absolute terms; however, there are no significant differences in relative (%-change) terms; (3) both derived indices SS-CVR and SS-CVCR exhibit stronger correlations with rSO2 compared to their original parameters, CBF and CVC, respectively. Our novel indices may have important utility in tracking cerebrovascular responses to acute concomitant hypoxia and hypocapnia in lab or fieldwork at altitude.
Abbreviations
- ABG:
-
Arterial blood gas
- CaO2 :
-
Arterial oxygen content
- CVC:
-
Cerebrovascular conductance
- CBF:
-
Cerebral blood flow
- CVR:
-
Cerebrovascular reactivity
- CBV:
-
Cerebral blood velocity
- DO2 :
-
Cerebral oxygen delivery
- gCBF:
-
Global cerebral blood flow
- ICA:
-
Internal carotid artery
- PaCO2 :
-
Pressure or arterial carbon dioxide
- PaO2 :
-
Pressure of arterial oxygen
- rSO2 :
-
Regional cerebral oxygen saturation
- SaO2 :
-
Arterial oxygen saturation
- SI:
-
Stimulus index (PaCO2/SaO2)
- SS-CVR:
-
Steady-state cerebrovascular reactivity
- SS-CVCR:
-
Steady-state cerebrovascular conductance reactivity
- VA:
-
Vertebral artery
References
Ainslie PN, Ogoh S (2010) Regulation of cerebral blood flow in mammals during chronic hypoxia: a matter of balance. Exp Physiol 95:251–262
Ainslie PN, Poulin MJ (2004) Ventilatory, cerebrovascular, and cardiovascular interactions in acute hypoxia: regulation by carbon dioxide. J Appl Physiol 97:149–159
Ainslie PN, Subudhi A (2014) cerebral blood flow at high altitude. High Alt Med Biol 15:133–140
Ainslie PN, Shaw AD, Smith KJ, Willie CK, Ikeda K, Graham J, Macleod DB (2014) Stability of cerebral metabolism and substrate availability in humans during hypoxia and hyperoxia. Clin Sci (Lond) 126(9):661–670
Bakker A, Smith B, Ainslie PN, Smith K (2012). Near-infrared spectroscopy, applied aspects of ultrasonography in humans. In: Philip A (ed) Near-infrared spectroscopy. ISBN: 978-953-51-0522-0, InTech. https://www.intechopen.com/books/applied-aspects-of-ultrasonography-in-humans/near-infrared-spectroscopy. Accessed 1 Mar 2019
Bernardi L, Schneider A, Pomidori L, Paolucci E, Cogo A (2006) Hypoxic ventilatory response in successful extreme altitude climbers. Eur Respir J 27:165–171
Binks A, Cunningham V, Adams L, Banzett R (2008) Gray matter blood flow change is unevenly distributed during moderate isocapnic hypoxia in humans. J Appl Physiol 104:212–217
Brown M, Wade J, Marshall J (1985) Fundamental importance of arterial oxygen content in the regulation of cerebral blood flow in man. Brain 108:81–93
Bruce CD, Steinback CD, Chauhan U, Pfoh J, Abrosimova M, Vanden Berg ER, Skow R, Davenport M, Day TA (2016) Quantifying cerebrovascular reactivity in anterior and posterior cerebral circulations during voluntary breath holding. Exp Physiol 101:1517–1527
Bruce CD, Saran G, Pfoh JR, Leacy JK, Zouboules SM, Mann CR, Peltonen JDB, Linares AM, Chiew AE, O’Halloran KD, Sherpa MT, Day TA (2018) What is the point of the peak? assessing steady-state respiratory chemoreflex drive in high altitude field studies. In: Gauda E, Monteiro M, Prabhakar N, Wyatt C, Schultz H (eds) Arterial chemoreceptors. Advances in experimental medicine and biology, vol 1071, chapter 2. Springer, Cham, pp 13–23
Brugniaux J, Hodges A, Hanly P, Poulin M (2007) Cerebrovascular responses to altitude. Respir Physiol Neurobiol 158:212–223
Chernecky CC, Berger BJ (2004) Laboratory tests & diagnostic procedures. Elsevier Inc., Philadelphia
Dempsey JA, Forster HV (1982) Mediation of ventilatory adaptations. Physiol Rev 62:262–346
Dempsey JA, Powell FL, Bisgard GE, Blain GM, Poulin MJ, Smith CA (2014) Role of chemoreception in cardiorespiratory acclimatization to, and deacclimatization from, hypoxia. J Appl Physiol 116:858–866
Faraci F, Heistad D, Mayhan W (1987) Role of large arteries in regulation of blood flow to brain stem in cats. J Physiol 387:115–123
Feddersen B, Neupane P, Thanbichler F, Hadolt I, Sattelmeyer V, Pfefferkorn T, Waanders R, Noachtar S, Ausserer H (2015) Regional differences in the cerebral blood flow velocity response to hypobaric hypoxia at high altitudes. J Cereb Blood Flow Metab 35:1846–1851
Flück D, Siebenmann C, Keiser S, Cathomen A, Lundby C (2015) Cerebrovascular reactivity is increased with acclimatization to 3,454 M altitude. J Cereb Blood Flow Metab 35:1323–1330
Ge R, Babb TG, Sivieri M, Resaland GK, Karlsen T, Stray-Gundersen J, Levine BD (2006) Urine acid–base compensation at simulated moderate altitude. High Alt Med Biol 7:64–71
Gonzalez-Alonso J, Richardson R, Saltin B (2001) Exercising skeletal muscle blood flow in humans responds to reduction in arterial oxyhaemoglobin, but not to altered free oxygen. J Physiol 530:331–341
Grocott M, Martin D, Levett D, McMorrow R, Windsor J, Montgomery H (2009) Arterial blood gases and oxygen content in climbers on mount everest. N Engl J Med 360:140–149
Hadolt I, Litscher G (2003) Noninvasive assessment of cerebral oxygenation during high altitude trekking in the Nepal Himalayas (2850–5600 m). Neurol Res 25:183–188
Hoiland R, Ainslie P, Wildfong K, Smith K, Bain A, Willie C, Foster G, Monteleone B, Day T (2015) Indomethacin-induced impairment of regional cerebrovascular reactivity: implications for respiratory control. J Physiol 593:1291–1306
Hoiland R, Bain R, Rieger M, Bailey D, Ainslie P (2016) Hypoxemia, oxygen content, and the regulation of cerebral blood flow. Am J Physiol Regul Integr Comp Physiol 310:R398–413
Hoiland R, Smith K, Carter H, Lewis N, Tymko M, Wildfong K, Bain A, Green D, Ainslie P (2017) Shear-mediated dilation of the internal carotid artery occurs independent of hypercapnia. Am J Physiol Circ Physiol 313:H24–H31
Hoiland RL, Howe CA, Coombs GB, Ainslie PN (2018) Ventilatory and cerebrovascular regulation and integration at high-altitude. Clin Auton Res 28(4):423–435
Jensen J, Sperling B, Severinghaus J, Lassen N (1996) Augmented hypoxic cerebral vasodilation in men during 5 days at 3,810 m altitude. J Appl Physiol 80:1214–1218
Kety S, Schmidt C (1948) The effects of altered arterial tensions of carbon dioxide and oxygen on cerebral blood flow and cerebral oxygen consumption of normal young men. J Clin Invest 27:484–492
Kim J, Baek S (2011) Circumferential variations of mechanical behavior of the porcine thoracic aorta during the inflation test. J Biomech 44:1941–1947
Krapf R, Beeler I, Hertner D, Hulter HN (1991) Chronic respiratory alkalosis. The effect of sustained hyperventilation on renal regulation of acid-base equilibrium. N Engl J Med 324(20):1394–1401
Lawley J, Macdonald J, Oliver S, Mullins P (2017) Unexpected reductions in regional cerebral perfusion during prolonged hypoxia. J Physiol 595:935–947
Lewis N, Messinger L, Monteleone B, Ainslie P (2014) Effect of acute hypoxia on regional cerebral blood flow: effect of sympathetic nerve activity. J Appl Physiol 116:1189–1196
Lu D, Kassab G (2011) Role of shear stress and stretch in vascular mechanobiology. J R Soc Interface 8:1379–1385
Naeije R (2010) Physiological adaptation of the cardiovascular system to high altitude. Prog Cardiovasc Dis 52:456–466
Norcliffe L, Rivera-Ch M, Claydon V, Moore J, Leon-Velarde F, Appenzeller O, Hainsworth R (2005) Cerebrovascular responses to hypoxia and hypocapnia in high-altitude dwellers. J Physiol 566:287–294
Ogoh S, Sato K, Nakahara H, Okazaki K, Subudhi A, Miyamoto T (2013) Effect of acute hypoxia on blood flow in vertebral and internal carotid arteries. Exp Physiol 98:692–698
Pfoh JR, Steinback CD, Vanden Berg ER, Bruce CD, Day TA (2017) Assessing chemoreflexes and oxygenation in the context of acute hypoxia: implications for field studies. Respir Physiol Neurobiol 246:67–75
Poulin M, Fatemian M, Tansley J, O’Connor D, Robbins P (2002) Changes in cerebral blood flow during and after 48 h of both isocapnic and poikilocapnic hypoxia in humans. Exp Physiol 87:633–642
Prabhakar N (2000) Oxygen sensing by the carotid body chemoreceptors. J Appl Physiol 88:2287–2295
Pugh L (1964) Blood volume and haemoglobin concentration at altitudes above 18,000 ft. (5500m). J Physiol 170:344–354
Roach R, Koskolou M, Calbet J, Saltin B (1999) Arterial O2 content and tension in regulation of cardiac output and leg blood flow during exercise in humans. Am J Physiol 276:H438–H445
Rubanyi G, Romero J, Vanhoutte P (1986) Flow-induced release of endothelium-derived relaxing factor. Am J Physiol 250:H1145–H1149
Sagarmatha National Park Office (2017) Sagarmatha National Park fact sheet. Sagarmatha National Park Office, Namche Bazaar
Skow R, MacKay C, Tymko M, Willie C, Smith K, Ainslie P, Day T (2013) Differential cerebrovascular CO2 reactivity in anterior and posterior cerebral circulations. Respir Physiol Neurobiol 189:76–86
Sriram K, Laughlin J, Rangamani P, Tartakovsky D (2016) Shear-induced nitric oxide production by endothelial cells. Biophys J 111:208–221
Subudhi A, Fan L, Evero O, Bourdillon N, Kayser B, Julian C, Lovering A, Roach R (2014) AltitudeOmics: effect of ascent and acclimatization to 5260 m on regional cerebral oxygen delivery. Exp Physiol 99:772–781
Swenson ER (2016) Hypoxia and its acid–base consequences: from mountains to malignancy. Adv Exp Med Biol 903:301–323
Teppema L, Dahan A (2010) The ventilatory response to hypoxia in mammals: mechanisms, measurement, and analysis. Physiol Rev 90:675–754
Tymko M, Ainslie P, Smith K (2018) Evaluating the methods used for measuring cerebral blood flow at rest and during exercise in humans. Eur J Appl Physiol 118:1527–1538
Willie C, Macleod D, Shaw A, Smith K, Tzeng Y, Eves D, Ikeda K, Graham J, Lewis C, Day T, Ainslie P (2012) Regional brain blood flow in man during acute changes in arterial blood gases. J Physiol 590:3261–3275
Willie C, Smith K, Day T, Ray L, Lewis N, Bakker A, Macleod D, Ainslie P (2014a) Regional cerebral blood flow in humans at high altitude: gradual ascent and 2 wk at 5,050 m. J Appl Physiol 116:905–910
Willie C, Tzeng Y, Fisher J, Ainslie P (2014b) Integrative regulation of human brain blood flow. J Physiol 592:841–859
Willie C, MacLeod D, Smith K, Lewis N, Foster G, Ikeda K, Hoiland R, Ainslie P (2015) The contribution of arterial blood gases in cerebral blood flow regulation and fuel utilization in man at high altitude. J Cereb Blood Flow Metab 35:873–881
Windsor J, Rodway G (2007) Heights and haematology: the story of haemoglobin at altitude. Postgrad Med J 83:148–151
Xu F, Liu P, Pascual J, Xiao G, Lu H (2012) Effect of hypoxia and hyperoxia on cerebral blood flow, blood oxygenation, and oxidative metabolism. J Cereb Blood Flow Metab 32:1909–1918
Zarrinkoob L, Ambarki K, Wåhlin A, Birgander R, Eklund A, Malm J (2015) Blood flow distribution in cerebral arteries. J Cereb Blood Flow Metab 35:648–654
Zouboules SM, Lafave HC, O’Halloran KD, Brutseart TD, Nysten HE, Nysten CE, Steinback CD, Sherpa MT, Day TA (2018) Renal reactivity: acid-base compensation during incremental ascent to high altitude. J Physiol 596(24):6191–6203
Acknowledgements
We gratefully acknowledge the time and effort of our research participants and our Sherpa guide team. The principal investigator (TAD) dedicates this manuscript to the memory of Dr. Christopher Willie.
Funding
Financial support for this work was provided by (a) Natural Sciences and Engineering Research Council of Canada (NSERC) Undergraduate Student Research Assistantship (SZ, HL); (b) Alberta Innovates Health Solution Summer studentship (CN); (c) Government of Alberta Student Temporary Employment Program (SZ), and NSERC Discovery grants (TAD; RGPIN-2016-04915; CDS RGPIN-2015-06637).
Author information
Authors and Affiliations
Contributions
HCL: data analysis, intellectual contribution, first draft of manuscript, and manuscript editing; SMZ: data analysis and manuscript editing; MAJ, GMP, JLR, PO, TDB, HEN, and CEN: data collection, manuscript editing; CDS, intellectual contribution, assistance with ethics, and manuscript editing; RLH: intellectual contribution and manuscript editing, MTS: Nepalese collaboration, assistance with ethics in Nepal, and manuscript editing; TAD: study design, expedition organizer, ethical clearance, funding, data analysis, intellectual contribution, and manuscript editing. All listed co-authors approved the final version of the manuscript, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved, all persons designated as authors qualify for authorship, and all those who qualify for authorship are listed.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Additional information
Communicated by Guido Ferretti.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lafave, H.C., Zouboules, S.M., James, M.A. et al. Steady-state cerebral blood flow regulation at altitude: interaction between oxygen and carbon dioxide. Eur J Appl Physiol 119, 2529–2544 (2019). https://doi.org/10.1007/s00421-019-04206-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-019-04206-6