Abstract
With ascent to high altitude (HA), compensatory increases in cerebral blood flow and oxygen delivery must occur to preserve cerebral metabolism and consciousness. We hypothesized that this compensation in cerebral blood flow and oxygen delivery preserves tolerance to simulated hemorrhage (via lower body negative pressure, LBNP), such that tolerance is similar during sustained exposure to HA vs. low altitude (LA). Healthy humans (4F/4 M) participated in LBNP protocols to presyncope at LA (1130 m) and 5–7 days following ascent to HA (3800 m). Internal carotid artery (ICA) blood flow, cerebral delivery of oxygen (CDO2) through the ICA, and cerebral tissue oxygen saturation (ScO2) were determined. LBNP tolerance was similar between conditions (LA: 1276 ± 304 s vs. HA: 1208 ± 306 s; P = 0.58). Overall, ICA blood flow and CDO2 were elevated at HA vs. LA (P ≤ 0.01) and decreased with LBNP under both conditions (P < 0.0001), but there was no effect of altitude on ScO2 responses (P = 0.59). Thus, sustained exposure to hypobaric hypoxia did not negatively impact tolerance to simulated hemorrhage. These data demonstrate the robustness of compensatory physiological mechanisms that preserve human cerebral blood flow and oxygen delivery during sustained hypoxia, ensuring cerebral tissue metabolism and neuronal function is maintained.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trauma-induced hemorrhage can occur at high altitude (HA) from a variety of causes, including battlefield injuries, motorized vehicle accidents, air accidents, major falls, and avalanches if victims hit solid objects such as trees and rocks (Aguiar et al. 2017; Sheets et al. 2018; Boyd et al. 2009). Acute exposure to hypoxia reduces arterial oxygen content, resulting in compensatory increases in sympathetic activity (Weisbrod et al. 2001; Wilkins et al. 2008, 2006; Barioni et al. 2022), heart rate (Naeije et al. 1982; Richardson et al. 1967; van Helmond et al. 2018; Weisbrod et al. 2001; Wilkins et al. 2008, 2006), cardiac output (Naeije et al. 1982; Richardson et al. 1967; van Helmond et al. 2018), and hemoglobin concentration (via plasma volume contraction) (Siebenmann et al. 2015), and decreases in systemic vascular resistance (SVR; i.e., hypoxic vasodilation) (Naeije et al. 1982; Richardson et al. 1967; Rowell and Blackmon 1986; van Helmond et al. 2018; Weisbrod et al. 2001; Wilkins et al. 2008, 2006) to maintain adequate oxygen delivery to the tissues. The combined reduction in blood flow due to blood loss and decreased arterial oxygen content due to both blood loss and the hypoxic environment of HA, will ultimately limit oxygen delivery to vital organs and tissues, including the brain. Zhao et al. reported reduced survival (10% vs. 40%) and increased severity of organ injury following uncontrolled blood loss under acute hypobaric hypoxia conditions (atmospheric partial pressure of oxygen of 100 mmHg, ~ 4000 m) in a rodent model (Zhao et al. 2018). However, in humans, the effect of sustained hypoxia on tolerance to hemorrhage, and the cardiovascular and cerebrovascular responses to this stress are less clear.
Lower body negative pressure (LBNP) is a method used to induce central hypovolemia and simulate hemorrhage in heathy humans. LBNP has been validated against actual blood loss in humans (Johnson et al. 2014; Rickards et al. 2015) and non-human primates (Hinojosa-Laborde et al. 2014), and has been shown to induce similar cardiovascular responses. Investigators have assessed the cardiovascular responses to the combined effects of submaximal LBNP and acute normobaric hypoxia, and have demonstrated greater reductions in arterial pressure (Heistad and Wheeler 1970; van Helmond et al. 2018) and blunted compensatory increases in forearm vascular resistance (Heistad and Wheeler 1970; Rowell and Seals 1990) compared to normoxia (i.e., breathing room air). These data suggest that tolerance to simulated hemorrhage via LBNP may be reduced with exposure to acute hypoxia, although this question has not been directly assessed.
Another important consideration is the cerebrovascular responses that occur with exposure to hypoxia, and how these responses may impact tolerance to hemorrhage at HA. With acute inhalation of hypoxic gas mixtures (normobaric hypoxia), and during early stages of ascent to HA (hypobaric hypoxia), the cerebral vasculature dilates, reducing cerebral vascular resistance, and subsequently increasing cerebral blood flow (Ainslie et al. 2014; Kety and Schmidt 1948; Lafave et al. 2019; Willie et al. 2014). Several investigators have also measured cerebral blood flow over the course of acclimatization to HA (Severinghaus et al. 1966; Huang et al. 1987; Jensen et al. 1990; Lucas et al. 2011; Rupp et al. 2014; Willie et al. 2014). Severinghaus et al. (1966) were the first to report a ~ 24% increase in cerebral blood flow in humans on arrival at high altitude (6–12 h at 3810 m compared with sea level), and by days 3–5 cerebral blood flow was 13% higher than sea level (Severinghaus et al. 1966). Subsequent studies have demonstrated that cerebral blood flow reaches a peak about 2–3 days after arrival at HA and returns to sea-level values within ~ 1–3 weeks of HA exposure (Huang et al. 1987; Jensen et al. 1990; Lucas et al. 2011; Rupp et al. 2014). Importantly, cerebral oxygen delivery (CDO2) is well maintained throughout acclimatization due to the initial increases in cerebral blood flow, which compensate for the reduced arterial oxygen content. This is followed by increases in hemoglobin concentration via plasma volume contraction in the first few days, then an increase in total red blood cell volume (and increased hemoglobin mass), which increases oxygen carrying capacity with chronic HA exposure (weeks to months) (Siebenmann et al. 2017; Siebenmann et al. 2015). Based on these compensatory increases in cerebral blood flow that occur within the first week of exposure to HA-induced hypoxia, we hypothesized that tolerance to simulated hemorrhage (via application of LBNP) at HA would be similar to low altitude (LA) due to increased cerebral blood flow and oxygen delivery, and the subsequent preservation of cerebral tissue oxygenation.
Methods
Ethical approval
This study was part of a large multi-institutional high altitude research expedition to the Barcroft Research Laboratory (3800 m) in the White Mountains, California, USA in August 2019. The study abided by the Canadian Government Tri-Council policy on research ethics with humans. Ethical approval for all experimental protocols and procedures were approved through the University of Calgary Conjoint Human Research Ethics Board (#REB18-0374), the Mount Royal University Human Research Ethics Board (Protocol 101,879), and the North Texas Regional Institutional Review Board (IRB #2019–110 and IRB #2021–057) in accordance with the standards set forth in the Declaration of Helsinki, except for being registered in a database. All participants provided informed written and verbal consent prior to voluntary participation in the study.
Experimental design
Baseline testing was conducted at LA in Calgary, Alberta, Canada (1130 m). Participants then flew to Las Vegas, Nevada, USA (620 m) where they stayed for one night prior to rapid ascent by road (over 5–6 h) to HA at the Barcroft Research Laboratory. Participants resided at 3800 m for 10 days with the experimental testing taking place for this study on days 5–7. Data from the HA experiment (LBNP up to – 60 mmHg) have been reported in a related, but independent publication (Anderson et al. 2021), and the study outlined here is distinct and was planned a priori.
Participants
Participants were recruited from the research team, and they participated in multiple studies conducted during baseline testing in Calgary and during the 10 days at the Barcroft Research Laboratory. Prior to participation in this study, all participants lived at or below an altitude of 1130 m, and had not traveled to HA within the 6 months before the study. Eight healthy adults participated in two experimental study visits (one at LA and one at HA). All participants were non-smokers and free from known cardiovascular, respiratory, metabolic, or inflammatory diseases. Female participants underwent a urine pregnancy test immediately prior to each experimental session to confirm they were not pregnant. Menstrual cycle stage was not controlled due to the logistical constraints of an expedition study. Of the 4 female participants, 1 was taking oral contraceptives, and 3 were using intrauterine devices. All participants abstained from alcohol, caffeine, prescription and non-prescription drugs, herbal medications, and exercise for the 12-h before each experimental study visit. Experiments were performed throughout the day (approximately 7am–7 pm), but the two experimental sessions were performed at approximately the same time of day for each individual participant (i.e., always the morning or afternoon, within approximately 2 h of the previous experiment).
Instrumentation
Participants were positioned supine inside a LBNP chamber, straddling a bicycle seat, and with their waist (at the iliac crest) in line with the opening of the chamber. An airtight seal around the waist was achieved with heavy-duty plastic, and a neoprene band. All participants were instrumented for continuous measurement of heart rate (HR) via a standard lead II ECG configuration (shielded leads, cable, and amplifier, AD Instruments, Bella Vista, NSW, Australia), and beat-to-beat arterial pressure and stroke volume (SV) via finger photoplethysmography (Finometer, Finapres Medical Systems, Amsterdam, The Netherlands). Aortic diameter was measured using B-mode Doppler ultrasound (2–5 MHz 5C2 probe; Terason 3300, Teratech, Burlington, MA, USA) to correct the ModelFlow® SV measurements obtained from the Finometer. An oral- nasal cannula was placed in the nose and over the mouth for breath-by-breath measurement of respiration rate, partial pressure of end tidal CO2 (PETCO2), and partial pressure of end tidal O2 (PETO2) (ML206 Gas Analyzer, AD Instruments, Bella Vista, NSW, Australia). Cerebral blood velocity was recorded from a middle cerebral artery (MCAv) via transcranial Doppler ultrasound (2-MHz probe; ST3, Spencer Technologies, Seattle, WA). Interpretation of transcranial Doppler ultrasound measurements of cerebral blood velocity as an index of blood flow are limited by the assumption that the insonated cerebral vessel diameter remains constant. Accordingly, measurement of blood flow through the internal carotid artery (ICA) was also assessed (i.e., diameter and velocity). Duplex Doppler ultrasound (4–15 MHz 15L4 probe; Terason 3300, Teratech, Burlington, MA, USA) was used to measure ICA diameter and velocity continuously. Video recordings of the ultrasound measures were made using screen recording software (Camtasia, Techsmith Corp, MI, USA) and stored as AVI files for later analysis (see data analysis section for details). Oxy-hemoglobin, deoxy-hemoglobin, total hemoglobin concentration (THC; oxy-hemoglobin + deoxy-hemoglobin), and cerebral tissue oxygen saturation (ScO2; (oxy-hemoglobin/THC)*100) were measured or calculated from the frontal cortex via near infrared spectroscopy (OxiplexTS, ISS, Champaign-Urbana, IL). The MCAv, ICA blood flow, and cerebral oxygenation measurements were recorded from the right side of the head in all participants except for one, in whom the MCAv was measured on the left side of the head. Muscle tissue oxygen saturation (SmO2) was obtained from the flexor carpi ulnaris muscle of the forearm via near infrared spectroscopy (OxiplexTS, ISS, Champaign-Urbana, IL). Arterial oxygen saturation (SpO2) was monitored continuously via pulse oximetry (Nonin Onyx Vantage or Nonin 7500 FO, Nonin Medical Inc, MN, USA). Overnight, fasted finger capillary blood samples were collected on the morning of each experiment and were analyzed immediately for assessment of hemoglobin concentration ([Hb]) via a hemoglobinometer (Hemocue Hemoglobin System, Hb201 + with microcuvettes; Ängelholm, Sweden).
Protocol
Each participant completed a maximal LBNP test (i.e., to presyncope) at LA and HA. The protocol consisted of a 5-min baseline period, then application of LBNP to – 60 mmHg for 10-min, followed by decreases in chamber pressure every 5-min to – 70, – 80, – 90 and – 100 mmHg (Fig. 1A), or until the onset of specific termination criteria: (1) instantaneous systolic arterial pressure (SAP) below 80 mmHg; (2) sudden relative bradycardia, and/or; (3) voluntary termination due to subjective presyncopal symptoms such as gray-out, nausea, sweating, dizziness, blurred vision, or general discomfort (Kay and Rickards 2016; Kay et al. 2017). The chamber pressure was released immediately at the onset of one of these criteria, or upon reaching the end of 5-min at – 100 mmHg LBNP. Participants remained in the LBNP chamber for a 10-min recovery period.
Lower body negative pressure (LBNP) protocol (Panel A), consisting of a 5-min baseline period, then application of LBNP to – 60 mmHg for 10-min, followed by decreases in chamber pressure every 5-min to – 70, – 80, – 90 and – 100 mmHg, until pre-syncope. Tolerance time (in seconds; Panel B) to lower body negative pressure (LBNP) at low altitude (LA) and at high altitude (HA) in 8 participants. Stroke volume (SV; Panel C) was higher at HA (dashed line, open circles) compared with LA (solid line, closed circles), but decreased by a similar magnitude at both altitudes (Panel D). Mean ± SD and/or individual participant data (circles) are presented. *Denotes difference from baseline, P ≤ 0.001. †Denotes difference between LA and HA, P ≤ 0.06. A two-factor (time, altitude) linear mixed model analysis with Holm-corrected post hoc tests run on the least squared means (data in Panel C), and paired t-tests (data in Panels B and D) were used for analysis
Data analysis
Tolerance to LBNP was assessed by the total time to presyncope (in seconds). All continuous waveform data (e.g., ECG, arterial pressure, SV, MCAv, ScO2, SmO2, PETCO2, PETO2) were collected at 1000 Hz (LabChart, AD Instruments, Bella Vista, NSW, Australia) and analyzed offline via specialized software (WinCPRS, Absolute Aliens, Turku, Finland). R-waves from the ECG signal were detected to determine the time intervals of each cardiac cycle. Beat-to-beat SAP and diastolic arterial pressures (DAP) were then detected from the continuous arterial pressure tracings. Systolic and diastolic cerebral blood velocities were also detected and marked from the continuous MCAv tracings. Mean arterial pressure (MAP) and mean MCAv were automatically calculated as the area under the arterial pressure and cerebral blood velocity waveforms via the WinCPRS software. The final 1-min of the baseline period and the 1-min prior to presyncope (PS-1) were averaged for all time domain variables. Data for each participant were only included in the final analysis if they reached objective presyncopal criteria during PS-1 (defined as mean SAP ≤ 100 mmHg for the 1-min prior to presyncope, and/or minimum instantaneous SAP ≤ 90 mmHg within the 1-min prior to presyncope, and/or bradycardia ≥ 10 bpm within the 1-min prior to presyncope) as we have previously reported (Kay and Rickards 2016; Kay et al. 2017). All participants met these criteria, so were included in the analysis.
Oscillatory patterns of MAP and mean MCAv were determined via power spectral analysis. Data was made equidistant by interpolating linearly and resampling at 5 Hz, then passed through a low-pass filter with a cutoff frequency of 0.5 Hz. Five-minute data bins were fast Fourier transformed to obtain power spectra and are expressed as the integrated area within the very low frequency (VLF, 0.02–0.07 Hz) and low frequency (LF, 0.07–0.15 Hz) ranges. Coherence between MAP and mean MCAv in the VLF and LF ranges were calculated by dividing the squared cross-spectral densities of the two signals by the product of the individual autospectra. Transfer function phase and gain between MAP and mean MCAv were calculated only when coherence values were ≥ 0.5. The final 5-min of the baseline period and the 5-min prior to presyncope (PS-5) were averaged for all frequency domain variables.
Calculations
Cardiac output was calculated as the product of SV and HR; SVR was calculated as MAP divided by cardiac output. Simultaneous diameter and peak envelope blood velocity measurements from the ICA were obtained using specialized wall tracking software (Woodman et al. 2001). Mean blood velocity of the ICA was calculated as peak envelope blood velocity divided by 2 (Evans 1985). A minimum of 10 consecutive cardiac cycles were used to obtain ICA blood velocity and diameter during the last 5-min of each LBNP protocol stage, as per published guidelines (Thomas et al. 2015). These data were then used to calculate ICA blood flow using the following equation:
Arterial oxygen content (CaO2) was calculated by the following equation \(:\)
where [Hb] is the concentration of hemoglobin (g/dl), 1.36 is the oxygen carrying capacity of hemoglobin (ml/g), SpO2 is an index of arterial oxygen saturation, 0.003 is the percentage of oxygen dissolved in the blood, and PETO2 is used as a surrogate for PaO2 (Ainslie et al. 2014; Willie et al. 2012). CDO2 through the ICA was calculated from the following equation:
\(CD{O}_{2} =ICA\, Blood \,Flow* Ca{O}_{2}/ 100\) (Ainslie et al. 2014).
Statistical analysis
Time to presyncope and cardiovascular responses were compared between the LA and HA conditions for all participants. Absolute and percent change from baseline values are reported for the key variables of interest. Differences between altitude conditions at baseline, and all percent change from baseline values during LBNP were assessed using separate paired t-tests. Our primary outcome variables were assessed using a two-factor (LBNP stage, altitude) linear mixed model analysis with repeated measures from baseline to presyncope, followed by Holm corrected post-hoc tests (JMP Pro 12, SAS Institute, Cary, NC). Effect size statistics were also calculated (either partial eta-squared (η2) or Cohen’s d). Exact P values are reported for all comparisons allowing the reader to make their own judgments and interpretation of the results, rather than selecting an arbitrary threshold and the dichotomous use of the term “significant” (Curran-Everett and Benos 2004; Curran-Everett 2020). Unless otherwise stated, all data are presented as mean ± standard deviation (SD).
Results
Eight healthy human participants (4 males, 4 females; age, 30 ± 8 y; height, 173 ± 14 cm; weight, 74 ± 15 kg) completed the LBNP protocols to presyncope at LA and HA.
LBNP tolerance time
In all 16 LBNP experiments, participants reached objective presyncopal endpoints (defined as mean SAP ≤ 100 mmHg for the 1-min prior to presyncope, and/or minimum instantaneous SAP ≤ 90 mmHg within the 1-min prior to presyncope, and/or bradycardia ≥ 10 bpm within the 1-min prior to presyncope) as we have previously reported (Kay and Rickards 2016; Kay et al. 2017). As we hypothesized, LBNP tolerance time (assessed as time to presyncope) was similar between conditions (LA: 1276 ± 304 s vs. HA: 1208 ± 306 s, P = 0.58; Fig. 1B). The average maximal LBNP at presyncope was 78 ± 10 mmHg at LA and 75 ± 12 mmHg at HA (P = 0.56).
Central hemodynamic responses to presyncopal LBNP at LA and HA
Baseline hemodynamics are compared between altitude conditions in Table 1. Baseline heart rate, ICA blood flow, and Hb concentration were higher, while SV and SpO2 were lower at HA compared with LA (P ≤ 0.05; Table 1). Central hemodynamic responses to LBNP are presented in Table 2, and Fig. 1 (Panels C and D). Higher heart rates at HA (altitude effect, P < 0.001) resulted in lower SV at baseline and at presyncope compared with LA conditions (altitude effect, P < 0.01; Table 2). Consequently, there was no difference in cardiac output between altitudes (altitude effect, P = 0.71). SV, MAP, and cardiac output decreased in response to LBNP at both altitudes (LBNP effect, P < 0.0001), with similar relative responses at LA and HA (P ≥ 0.12; Fig. 1C and D; Table 2). In response to these reductions in central blood volume and arterial pressure with LBNP, HR increased at both altitudes (LBNP effect, P < 0.0001), with comparable relative changes from baseline to PS-1 (P = 0.71; Table 2). Similarly, SVR increased with presyncopal LBNP at both LA and HA (LBNP effect, P < 0.0001; Table 2), with comparable relative changes from baseline to PS-1 (P = 0.21; Table 2). SmO2 decreased with presyncopal LBNP at both LA and HA (LBNP effect, P < 0.01), with no difference in the relative changes from baseline to PS-1 between altitude conditions (P = 0.12; Table 2). Note that the SmO2 data was analyzed with only 6 participants due to loss of the signal during data collection in two participants.
Cerebral hemodynamic and oxygenation responses to LBNP at LA and HA
Cerebral hemodynamic and oxygenation responses to LBNP are presented in Table 3, and Figs. 2 and 3. MCAv data were analyzed from 7 participants, due to loss of the signal during data collection in one participant. Mean MCAv decreased from baseline with LBNP at both altitudes (LBNP effect, P < 0.0001), with no differences in either absolute (P = 0.35) or relative responses from baseline to PS-1 between altitude conditions (P = 0.77; Table 3). Overall, ICA diameter decreased with presyncopal LBNP (LBNP effect, P = 0.06), with no differences between altitude conditions in absolute or relative responses (P ≥ 0.27; Table 3). ICA velocity and blood flow were higher overall at HA vs. LA (Altitude effect, P ≤ 0.02), and decreased with presyncopal LBNP at both altitudes (LBNP effect, P < 0.0001), with comparable relative changes from baseline to PS-1 (P ≥ 0.79; Table 3; Fig. 2A; Fig. 2B). CaO2 was slightly higher at HA vs. LA (Altitude effect, P = 0.09), with a greater relative increase above baseline with LBNP at HA (P = 0.002; Table 3). CDO2 through the ICA was higher overall at HA vs. LA (Altitude effect, P < 0.01) and decreased with presyncopal LBNP at both altitudes (LBNP effect, P < 0.0001; Fig. 2C), but there was no difference in the relative response from baseline to PS-1 between the altitude conditions (P = 0.47; Fig. 2D). ScO2 data were analyzed from 7 participants, due to loss of the signal during data collection in one participant. There was no effect of altitude on ScO2 (Altitude Effect, P = 0.59; Fig. 3A), with similar relative decreases from baseline to PS-1 between altitude conditions (P = 0.38; Fig. 3B). Respiratory rates were higher overall at HA vs. LA (Altitude effect, P = 0.03) and increased slightly with presyncopal LBNP (LBNP effect, P = 0.08); however, there were no differences in the relative increase in respiration rates between altitudes during LBNP (P = 0.54; Table 3). This relative hyperventilation at HA and in response to LBNP was reflected in lower PETCO2 values under each of these conditions (Table 3). At both baseline and with LBNP, PETO2 and SpO2 were lower at HA vs. LA (P ≤ 0.01). With LBNP, PETO2 increased at both altitudes (LBNP effect, P ≤ 0.0001), with similar relative responses (P = 0.78; Table 3); SpO2 did not change with LBNP (LBNP effect, P = 0.49; Table 3).
Internal carotid artery (ICA) blood flow (Panel A) decreased at low altitude (solid line, closed circle) and high altitude (dashed line, open circle) during lower body negative pressure (LBNP) to presyncope (PS-1). While ICA blood flow was higher at HA baseline, the magnitude of change was similar with LBNP at both altitudes (Panel B). Cerebral delivery of oxygen (Panel C) was higher at high altitude (dashed line, open circle) vs. low altitude (solid line, closed circle) at baseline and at pre-syncope (PS-1) but decreased by the same magnitude at both altitudes (Panel D). Mean ± SD and/or individual participant data (circles) are presented. *Denotes difference from baseline, P ≤ 0.003. †Denotes difference between low and high altitude, P ≤ 0.09. A two-factor (time, altitude) linear mixed model analysis with Holm-corrected post hoc tests run on the least squared means (data in Panels A and C), and paired t-tests (data in Panels B and D) were used for analysis
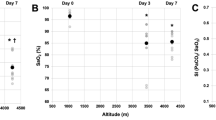
Cerebral oxygen saturation (Panel A) decreased at low altitude (solid line, closed circle) and high altitude (solid line, open circle) during lower body negative pressure (LBNP), but there was no difference between altitude conditions in either absolute or relative responses (Panel B). Mean ± SD and/or individual participant data (circles) are presented. A two-factor (time, altitude) linear mixed model analysis with Holm-corrected post hoc tests run on the least squared means (data in Panel A), and paired t-tests (data in Panel B) were used for analysis
Frequency domain responses to LBNP
The LF and VLF power spectral density data are presented in Table 4. Again, mean MCAv data were analyzed with 7 participants due to loss of the MCAv signal during data collection in one participant. MAP LF power was higher overall at HA vs. LA (Altitude effect, P = 0.01), and increased with presyncopal LBNP (LBNP effect, P < 0.01). In comparison, mean MCAv LF power was also higher overall at HA compared to LA (Altitude effect, P = 0.08), but did not change with LBNP (LBNP effect, P = 0.20). On average, LF coherence between MAP-mean MCAv was ≥ 0.5 at baseline and throughout presyncopal LBNP and was not different between LA and HA (Altitude effect, P = 0.29). However, due to low coherence (< 0.5) between signals during presyncopal LBNP for some participants, MAP-mean MCAv LF phase and gain data were analyzed with just 5 participants (Table 4). LF MAP-mean MCAv phase increased, and gain decreased in response to presyncopal LBNP at LA and HA (LBNP effect, P ≤ 0.01), with no differences between altitudes (Altitude effect, P ≥ 0.31).
VLF power for MAP and mean MCAv did not change with presyncopal LBNP at either LA or HA (LBNP effect, P ≥ 0.16), and there was no effect of altitude (Altitude effect, P ≥ 0.35). VLF coherence between MAP-mean MCAv was < 0.5 at baseline and during presyncopal LBNP, however, and only increased with presyncopal LBNP at HA (P = 0.02; Table 4). Due to this low coherence between MAP and mean MCAv in the VLF range, phase and gain were not calculated.
Discussion
We assessed the effect of sustained hypobaric hypoxia on tolerance to simulated hemorrhage in young healthy adult humans, and the cardiovascular and cerebrovascular responses to this combined physiological stress. The main findings of our study suggest that the sustained hypoxia experienced with ascent to high altitude (3800 m) does not affect tolerance to simulated hemorrhage (via maximal LBNP) in young healthy adults, which may be due to 1) a similar magnitude of central hypovolemia and subsequent cardiovascular reflex responses at low and high altitude, and/or, 2) compensatory increases in cerebral blood flow and subsequent maintenance of oxygen delivery to the cerebral tissues, resulting in the preservation of cerebral tissue oxygen saturation.
In previous studies, cardiovascular responses to the combination of acute normobaric hypoxia and simulated hemorrhage using submaximal LBNP have been explored (Heistad and Wheeler 1970; Rowell and Seals 1990; van Helmond et al. 2018). Acute normobaric hypoxia (inspired O2 ranged between 10 and 15%, equivalent to altitudes between 2700 and 5800 m) during submaximal LBNP resulted in greater decreases in arterial pressure (Heistad and Wheeler 1970; van Helmond et al. 2018) and attenuated increases in forearm vascular resistance (Heistad and Wheeler 1970; Rowell and Seals 1990) when compared to the normoxic condition. Additionally, Van Helmond et al. (2018) reported that acute exposure to hypoxia at rest resulted in reduced systemic vascular resistance, and lower tolerance to LBNP (van Helmond et al. 2018). These data suggest that tolerance to simulated hemorrhage may be reduced during acute hypoxia due to a greater hypotensive response, facilitated by hypoxic vasodilation (Naeije et al. 1982; Richardson et al. 1967; Rowell and Blackmon 1986; van Helmond et al. 2018; Weisbrod et al. 2001; Wilkins et al. 2008, 2006).
Our current findings are contrary to this literature, as we report similar tolerance and cardiovascular reflex responses to simulated hemorrhage at high and low altitude. We observed similar relative decreases in stroke volume (our index of central hypovolemia) and arterial pressure with maximal LBNP across altitudes, with no differences in the reflex increases in heart rate and systemic vascular resistance. There are some important methodological differences between these studies, however, which may account for the observed discrepancies. While we utilized a maximal, presyncopal limited LBNP protocol, the aforementioned studies examined the hemodynamic responses to submaximal LBNP with variations in the magnitude and timing of each LBNP stage. Additionally, the method of inducing hypoxia (normobaric vs. hypobaric) and duration of hypoxia exposure (acute vs. sustained) may influence the hemodynamic responses to simulated hemorrhagic stress (Millet and Debevec 2020; Millet et al. 2012). Accordingly, it is difficult to compare the results of studies where both the hypoxic stress (method and duration) and magnitude of central hypovolemia are different.
High altitude exposure is associated with compensatory changes in physiological function resulting from the reduction in atmospheric PO2 that leads to a decrease in arterial oxygen content. Acute physiological responses include increases in heart rate, cardiac output, ventilation, and hemoglobin concentration to preserve arterial oxygen content and sustain adequate oxygen delivery to the vital tissues during acclimatization (Bartsch and Gibbs 2007; Hoiland et al. 2018; Naeije 2010; Siebenmann et al. 2015). After a few days of acclimatization there is a reduction in plasma volume that contributes to an initial increase in hemoglobin concentration, prior to the onset of erythropoiesis; this elevation in hemoglobin concentration assists in restoration of arterial oxygen content, to account for the reduction in oxygen availability (Schlittler et al. 2021; Siebenmann et al. 2017). Additionally, during initial exposure to high altitude, hypoxic vasodilation tends to override sympathetic vasoconstriction in the peripheral circulation, resulting in an unchanged or slightly decreased arterial pressure (Bartsch and Gibbs 2007), so perfusion of the vital organs is maintained relatively constant.
The combined hypotension and hypocapnia induced by the simulated hemorrhage of LBNP, eventually leads to a decrease in cerebral blood flow and oxygen delivery, and the onset of presyncope (Rickards 2015). Accordingly, hemorrhage poses an additional challenge to cardiovascular and cerebrovascular compensatory mechanisms at HA, due to the combined reductions in both blood flow (due to hemorrhage) and arterial oxygen content (due to both hemorrhage and the hypoxic environment). To compensate for the reduced oxygen availability at HA, the cerebral blood vessels dilate, subsequently increasing blood flow to maintain oxygen delivery to the cerebral tissues (Hoiland et al. 2016). Indeed, in the current study, we observed an increase in ICA blood flow (our index of cerebral blood inflow) at HA, which increased delivery of oxygen to the tissues and preserved cerebral oxygen saturation. However, the increase in ICA blood flow was primarily due to an increase in blood velocity rather than dilation of the ICA. Interesting, this increase in ICA blood velocity and blood flow did not translate into an increase in MCAv (an index of intracranial blood flow) as expected. This may be due to dilation of intracranial cerebral blood vessels that may not occur in the extra cranial vessels. Indeed, Willie et al. (2014) demonstrated increases in MCA blood flow following 8 days at an altitude of 5050 m, which was due to increases in MCA diameter only, as velocity did not change (Willie et al. 2014). Unfortunately, MCA diameter was not assessed in the current study, so we are unable to definitively determine if MCA dilation was responsible for the stability of MCAv.
These findings suggest that adequate compensatory responses occurred to maintain oxygen delivery to the cerebral tissues during the combined stress of central hypovolemia (simulating hemorrhage) and sustained hypoxia. Interestingly, this contradicts findings from Zhao et al. (2018) who demonstrated in a rat model, that 2 days of hypoxia (atmospheric PO2 of 100 mmHg) combined with uncontrolled blood loss worsened the decreased oxygen supply, leading to more severe tissue injury (brain, lung, liver, kidney), and lower survival rate compared with the control condition (Zhao et al. 2018). This disparity may be due to the more severe blood loss protocol used for the rats (~ 30 ml/kg) compared with our study (~ 18 ml/kg at -70 mmHg LBNP (Hinojosa-Laborde et al. 2014)), the more acute phase of hypoxia exposure, and potential species differences. Further investigation is required to assess the magnitude of actual blood loss and/or hypoxia required to impair oxygen delivery and cerebral tissue oxygenation in humans.
Methodological considerations
There are several methodological considerations that must be taken into account when interpreting the findings of this study. First, we did not examine physiological responses to simulated hemorrhage and hypoxia during the early phase of HA acclimatization (days 1–3). As such, our findings cannot be generalized to all stages of HA exposure. In particular, at the time of testing, arterial oxygen content had returned to similar values as observed at LA. Therefore, the compensatory increase in oxygen delivery to the cerebral tissues and preservation of cerebral oxygen saturation that we observed at days 5–7, may have been attenuated during days 1–3, possibly leading to reduced tolerance to simulated hemorrhage.
As with most HA research expeditions, our participants were engaged in a number of other physiological studies for the duration of the LA and HA exposures, without the washout periods often employed in more controlled laboratory studies. As such, we cannot discount the confounding effects on our outcomes from these other physiological stimuli (such as tests of neurovascular coupling, variations in inspired O2 and CO2, voluntary breathing holding, cold pressor test, hand-grip exercise, post-exercise cuff occlusion). Despite this limitation, the results of our study were robust from both a physiological and statistical perspective.
In a related issue, we were not able to control the time of day of our experiments between participants, as we had a short time window to complete our studies. However, we were able to control for time of day within each participant for the two experiments. As blood samples were collected in the morning (in the supine posture) for all participants for assessment of hemoglobin concentration, some were not time-synced with their experiments. While hemoglobin concentrations can vary based on time of day and body position, both experiments were performed at the same time of day within each participant (i.e., the same time interval from the hemoglobin measurements), and they were always supine. Although increases in hemoglobin mass in response to HA exposure (around 3000 m) occur relatively slowly, with only small increases within the first 14 days (Rasmussen et al. 2013), altitude-induced dehydration cannot be excluded as a factor for increasing hemoglobin concentration.
Lastly, it is important to recognize that cerebral NIRS measures a mixed sample volume consisting of approximately 75% venous, 20% capillary, and 5% arterial blood (Pollard et al. 1996; Subudhi et al. 2011). Consequently, our measurement of cerebral oxygen saturation is influenced by both the delivery of oxygen through the blood to the cerebral tissue, and the extraction of oxygen from the blood into the tissue. Therefore, since cerebral oxygen delivery was elevated at HA compared to LA, we can assume that preservation of cerebral oxygen saturation is the result of greater delivery and not necessarily greater extraction of oxygen by the tissues. However, direct measurements of cerebral oxygen extraction and metabolism are needed to fully understand the physiological mechanisms underpinning these findings.
Conclusion
In summary, sustained (5–7 days) exposure to hypobaric hypoxia at an altitude of 3800 m does not affect tolerance to simulated hemorrhage in young healthy adults. This finding may be due to the similar cardiovascular reflex responses to central hypovolemia, and/or the compensatory increases in cerebral blood flow and oxygen delivery that resulted in the preservation of cerebral tissue oxygenation in response to sustained hypoxia. Further research is needed during the acute (minutes to hours) and chronic (weeks to months) phases of HA exposure to fully elucidate the effects of hypobaric hypoxia on tolerance to trauma-induced hemorrhage.
References
Aguiar M, Stolzer A, Boyd DD (2017) Rates and causes of accidents for general aviation aircraft operating in a mountainous and high elevation terrain environment. Accid Anal Prev 107:195–201. https://doi.org/10.1016/j.aap.2017.03.017
Ainslie PN, Shaw AD, Smith KJ, Willie CK, Ikeda K, Graham J, Macleod DB (2014) Stability of cerebral metabolism and substrate availability in humans during hypoxia and hyperoxia. Clin Sci (lond) 126(9):661–670. https://doi.org/10.1042/CS20130343
Anderson GK, Rosenberg AJ, Barnes HJ, Bird J, Pentz B, Byman BRM, Jendzjowsky N, Wilson RJA, Day TA, Rickards CA (2021) Peaks and valleys: oscillatory cerebral blood flow at high altitude protects cerebral tissue oxygenation. Physiol Meas 42:064005. https://doi.org/10.1088/1361-6579/ac0593
Barioni NO, Derakhshan F, Tenorio Lopes L, Onimaru H, Roy A, McDonald F, Scheibli E, Baghdadwala MI, Heidari N, Bharadia M, Ikeda K, Yazawa I, Okada Y, Harris MB, Dutschmann M, Wilson RJA (2022) Novel oxygen sensing mechanism in the spinal cord involved in cardiorespiratory responses to hypoxia. Sci Adv 8(12):eabm1444. https://doi.org/10.1126/sciadv.abm1444
Bartsch P, Gibbs JS (2007) Effect of altitude on the heart and the lungs. Circulation 116(19):2191–2202. https://doi.org/10.1161/CIRCULATIONAHA.106.650796
Boyd J, Haegeli P, Abu-Laban RB, Shuster M, Butt JC (2009) Patterns of death among avalanche fatalities: a 21-year review. CMAJ 180(5):507–512. https://doi.org/10.1503/cmaj.081327
Curran-Everett D (2020) Evolution in statistics: P values, statistical significance, kayaks, and walking trees. Adv Physiol Educ 44(2):221–224. https://doi.org/10.1152/advan.00054.2020
Curran-Everett D, Benos DJ (2004) Guidelines for reporting statistics in journals published by the American physiological society. Am J Physiol 287:R247-249. https://doi.org/10.1152/ajpregu.00346.2004
Evans DH (1985) On the measurement of the mean velocity of blood flow over the cardiac cycle using Doppler ultrasound. Ultrasound Med Biol 11(5):735–741. https://doi.org/10.1016/0301-5629(85)90107-3
Heistad DD, Wheeler RC (1970) Effect of acute hypoxia on vascular responsiveness in man. I. Responsiveness to lower body negative pressure and ice on the forehead. II. Responses to norepinephrine and angiotensin. 3. Effect of hypoxia and hypocapnia. J Clin Invest 49(6):1252–1265. https://doi.org/10.1172/JCI106338
Hinojosa-Laborde C, Shade RE, Muniz GW, Bauer C, Goei KA, Pidcoke HF, Chung KK, Cap AP, Convertino VA (2014) Validation of lower body negative pressure as an experimental model of hemorrhage. J Appl Physiol 116(4):406–415. https://doi.org/10.1152/japplphysiol.00640.2013
Hoiland RL, Bain AR, Rieger MG, Bailey DM, Ainslie PN (2016) Hypoxemia, oxygen content, and the regulation of cerebral blood flow. Am J Physiol Regul Integr Comp Physiol 310(5):R398-413. https://doi.org/10.1152/ajpregu.00270.2015
Hoiland RL, Howe CA, Coombs GB, Ainslie PN (2018) Ventilatory and cerebrovascular regulation and integration at high-altitude. Clin Auton Res 28(4):423–435. https://doi.org/10.1007/s10286-018-0522-2
Huang SY, Moore LG, McCullough RE, McCullough RG, Micco AJ, Fulco C, Cymerman A, Manco-Johnson M, Weil JV, Reeves JT (1987) Internal carotid and vertebral arterial flow velocity in men at high altitude. J Appl Physiol 63(1):395–400. https://doi.org/10.1152/jappl.1987.63.1.395
Jensen JB, Wright AD, Lassen NA, Harvey TC, Winterborn MH, Raichle ME, Bradwell AR (1990) Cerebral blood flow in acute mountain sickness. J Appl Physiol 69(2):430–433. https://doi.org/10.1152/jappl.1990.69.2.430
Johnson BD, van Helmond N, Curry TB, van Buskirk CM, Convertino VA, Joyner MJ (2014) Reductions in central venous pressure by lower body negative pressure or blood loss elicit similar hemodynamic responses. J Appl Physiol 117(2):131–141. https://doi.org/10.1152/japplphysiol.00070.2014
Kay VL, Rickards CA (2016) The role of cerebral oxygenation and regional cerebral blood flow on tolerance to central hypovolemia. Am J Physiol Regul Integr Comp Physiol 310(4):R375-383. https://doi.org/10.1152/ajpregu.00367.2015
Kay VL, Sprick JD, Rickards CA (2017) Cerebral oxygenation and regional cerebral perfusion responses with resistance breathing during central hypovolemia. Am J Physiol Regul Integr Comp Physiol 313(2):R132–R139. https://doi.org/10.1152/ajpregu.00385.2016
Kety SS, Schmidt CF (1948) The effects of altered arterial tensions of carbon dioxide and oxygen on cerebral blood flow and cerebral oxygen consumption of normal young men. J Clin Invest 27(4):484–492. https://doi.org/10.1172/JCI101995
Lafave HC, Zouboules SM, James MA, Purdy GM, Rees JL, Steinback CD, Ondrus P, Brutsaert TD, Nysten HE, Nysten CE, Hoiland RL, Sherpa MT, Day TA (2019) Steady-state cerebral blood flow regulation at altitude: interaction between oxygen and carbon dioxide. Eur J Appl Physiol 119(11–12):2529–2544. https://doi.org/10.1007/s00421-019-04206-6
Lucas SJ, Burgess KR, Thomas KN, Donnelly J, Peebles KC, Lucas RA, Fan JL, Cotter JD, Basnyat R, Ainslie PN (2011) Alterations in cerebral blood flow and cerebrovascular reactivity during 14 days at 5050 m. J Physiol 589(Pt 3):741–753. https://doi.org/10.1113/jphysiol.2010.192534
Millet GP, Debevec T (2020) CrossTalk proposal: barometric pressure, independent of P O 2, is the forgotten parameter in altitude physiology and mountain medicine. J Physiol 598(5):893–896. https://doi.org/10.1113/JP278673
Millet GP, Faiss R, Pialoux V (2012) Point: hypobaric hypoxia induces different physiological responses from normobaric hypoxia. J Appl Physiol 112(10):1783–1784. https://doi.org/10.1152/japplphysiol.00067.2012
Naeije R (2010) Physiological adaptation of the cardiovascular system to high altitude. Prog Cardiovasc Dis 52(6):456–466. https://doi.org/10.1016/j.pcad.2010.03.004
Naeije R, Melot C, Mols P, Hallemans R (1982) Effects of vasodilators on hypoxic pulmonary vasoconstriction in normal man. Chest 82(4):404–410. https://doi.org/10.1378/chest.82.4.404
Pollard V, Prough DS, DeMelo AE, Deyo DJ, Uchida T, Stoddart HF (1996) Validation in volunteers of a near-infrared spectroscope for monitoring brain oxygenation in vivo. Anesth Analg 82(2):269–277. https://doi.org/10.1097/00000539-199602000-00010
Rasmussen P, Siebenmann C, Diaz V, Lundby C (2013) Red cell volume expansion at altitude: a meta-analysis and Monte Carlo simulation. Med Sci Sports Exerc 45(9):1767–1772. https://doi.org/10.1249/MSS.0b013e31829047e5
Richardson DW, Kontos HA, Raper AJ, Patterson JL Jr (1967) Modification by beta-adrenergic blockade of the circulatory respones to acute hypoxia in man. J Clin Invest 46(1):77–85. https://doi.org/10.1172/JCI105513
Rickards CA (2015) Cerebral blood-flow regulation during hemorrhage. Compr Physiol 5(4):1585–1621. https://doi.org/10.1002/cphy.c140058
Rickards CA, Johnson BD, Harvey RE, Convertino VA, Joyner MJ (2015) Barnes JN (2015) Cerebral blood velocity regulation during progressive blood loss compared with lower body negative pressure in humans. J Appl Physiol (1985) 119(6):677–685. https://doi.org/10.1152/japplphysiol.00127.2015
Rowell LB, Blackmon JR (1986) Lack of sympathetic vasoconstriction in hypoxemic humans at rest. Am J Physiol 251(3 Pt 2):H562-570. https://doi.org/10.1152/ajpheart.1986.251.3.H562
Rowell LB, Seals DR (1990) Sympathetic activity during graded central hypovolemia in hypoxemic humans. Am J Physiol 259(4 Pt 2):H1197-1206. https://doi.org/10.1152/ajpheart.1990.259.4.H1197
Rupp T, Esteve F, Bouzat P, Lundby C, Perrey S, Levy P, Robach P, Verges S (2014) Cerebral hemodynamic and ventilatory responses to hypoxia, hypercapnia, and hypocapnia during 5 days at 4350 m. J Cereb Blood Flow Metab 34(1):52–60. https://doi.org/10.1038/jcbfm.2013.167
Schlittler M, Gatterer H, Turner R, Regli IB, Woyke S, Strapazzon G, Rasmussen P, Kob M, Mueller T, Goetze JP, Maillard M, van Hall G, Feraille E, Siebenmann C (2021) Regulation of plasma volume in male lowlanders during 4 days of exposure to hypobaric hypoxia equivalent to 3500 m altitude. J Physiol 599(4):1083–1096. https://doi.org/10.1113/JP280601
Severinghaus JW, Chiodi H, Eger EI 2nd, Brandstater B, Hornbein TF (1966) Cerebral blood flow in man at high altitude. Role of cerebrospinal fluid pH in normalization of flow in chronic hypocapnia. Circ Res 19(2):274–282. https://doi.org/10.1161/01.res.19.2.274
Sheets A, Wang D, Logan S, Atkins D (2018) Causes of death among avalanche fatalities in colorado: a 21-year review. Wilderness Environ Med 29(3):325–329. https://doi.org/10.1016/j.wem.2018.04.002
Siebenmann C, Cathomen A, Hug M, Keiser S, Lundby AK, Hilty MP, Goetze JP, Rasmussen P, Lundby C (2015) Hemoglobin mass and intravascular volume kinetics during and after exposure to 3,454-m altitude. J Appl Physiol (1985) 119(10):1194–1201. https://doi.org/10.1152/japplphysiol.01121.2014
Siebenmann C, Robach P, Lundby C (2017) Regulation of blood volume in lowlanders exposed to high altitude. J Appl Physiol 123(4):957–966. https://doi.org/10.1152/japplphysiol.00118.2017
Subudhi AW, Olin JT, Dimmen AC, Polaner DM, Kayser B, Roach RC (2011) Does cerebral oxygen delivery limit incremental exercise performance? J Appl Physiol 111(6):1727–1734. https://doi.org/10.1152/japplphysiol.00569.2011
Thomas KN, Lewis NC, Hill BG, Ainslie PN (2015) Technical recommendations for the use of carotid duplex ultrasound for the assessment of extracranial blood flow. Am J Physiol Regul Integr Comp Physiol:ajpregu 00211:02015. https://doi.org/10.1152/ajpregu.00211.2015
van Helmond N, Johnson BD, Holbein WW, Petersen-Jones HG, Harvey RE, Ranadive SM, Barnes JN, Curry TB, Convertino VA, Joyner MJ (2018) Effect of acute hypoxemia on cerebral blood flow velocity control during lower body negative pressure. Physiol Rep. https://doi.org/10.14814/phy2.13594
Weisbrod CJ, Minson CT, Joyner MJ, Halliwill JR (2001) Effects of regional phentolamine on hypoxic vasodilatation in healthy humans. J Physiol 537(Pt 2):613–621. https://doi.org/10.1111/j.1469-7793.2001.00613.x
Wilkins BW, Schrage WG, Liu Z, Hancock KC, Joyner MJ (2006) Systemic hypoxia and vasoconstrictor responsiveness in exercising human muscle. J Appl Physiol 101(5):1343–1350. https://doi.org/10.1152/japplphysiol.00487.2006
Wilkins BW, Pike TL, Martin EA, Curry TB, Ceridon ML, Joyner MJ (2008) Exercise intensity-dependent contribution of beta-adrenergic receptor-mediated vasodilatation in hypoxic humans. J Physiol 586(4):1195–1205. https://doi.org/10.1113/jphysiol.2007.144113
Willie CK, Macleod DB, Shaw AD, Smith KJ, Tzeng YC, Eves ND, Ikeda K, Graham J, Lewis NC, Day TA, Ainslie PN (2012) Regional brain blood flow in man during acute changes in arterial blood gases. J Physiol 590(Pt 14):3261–3275. https://doi.org/10.1113/jphysiol.2012.228551
Willie CK, Smith KJ, Day TA, Ray LA, Lewis NC, Bakker A, Macleod DB, Ainslie PN (2014) Regional cerebral blood flow in humans at high altitude: gradual ascent and 2 wk at 5,050 m. J Appl Physiol 116(7):905–910. https://doi.org/10.1152/japplphysiol.00594.2013
Woodman RJ, Playford DA, Watts GF, Cheetham C, Reed C, Taylor RR, Puddey IB, Beilin LJ, Burke V, Mori TA, Green D (2001) Improved analysis of brachial artery ultrasound using a novel edge-detection software system. J Appl Physiol 91(2):929–937. https://doi.org/10.1152/jappl.2001.91.2.929
Zhao J, You G, Yin Y, Zhang Y, Wang Y, Chen G, Zhao L, Zhou H (2018) Acute high-altitude exposure shortens survival after uncontrolled hemorrhagic shock in rats. J Surg Res 226:150–156. https://doi.org/10.1016/j.jss.2018.01.028
Acknowledgements
The authors thank our participants for their time and cheerful participation in this study. We also thank all other members of the White Mountain 2019 expedition team, and the staff at the Barcroft Research Laboratory for their generous support and service throughout the expedition.
Funding
Funding for this study was provided, in part, by an American Heart Association Grant-in-Aid (CAR; 17GRNT33671110), a Natural Sciences and Engineering Research Council of Canada Discovery Grant (TAD; RGPIN-2016-04915), a University of Calgary Research Grant Committee (RJAW), a NSERC Discovery grant (RJAW), and training fellowships awarded to GKA through a National Institutes of Health-supported Neurobiology of Aging Training Grant (T32 AG020494, Principal Investigator: N. Sumien) and an American Heart Association Predoctoral Fellowship (20PRE35210249), and to AJR through a Ruth L. Kirchstein NRSA F32 Postdoctoral Fellowship (1F32 HL144082-01A1). NGJ was a Parker B Francis Fellowship Recipient.
Author information
Authors and Affiliations
Contributions
AJR was responsible for conducting experiments, data analysis, drafting the work and revising it critically for important intellectual content, and final approval of the version to be published. GKA was responsible for conducting experiments, data analysis, revising the work for important intellectual content, and final approval of the version to be published. HJB was responsible for data analysis, revising the work for important intellectual content, and final approval of the version to be published. JB, BP, and BRMB were responsible for conducting experiments, revising the work for important intellectual content, and final approval of the version to be published. NJ, RJW, and TAD were responsible for coordinating and supervising the expedition, revising the work for important intellectual content, and final approval of the version to be published. CAR was responsible for conception of the work, obtaining funding for the study, conducting experiments, supervising data analysis, drafting the work and revising it critically for important intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest.
Additional information
Communicated by Guido Ferretti.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rosenberg, A.J., Anderson, G.K., McKeefer, H.J. et al. Hemorrhage at high altitude: impact of sustained hypobaric hypoxia on cerebral blood flow, tissue oxygenation, and tolerance to simulated hemorrhage in humans. Eur J Appl Physiol 124, 2365–2378 (2024). https://doi.org/10.1007/s00421-024-05450-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-024-05450-1