Abstract
Direct calorimetry is the gold standard means of measuring human metabolic rate and its use has been fundamental for understanding metabolism in health and disease. While metabolic rate is now more commonly estimated indirectly from measures of the oxygen consumed during respiration, direct calorimetry provides the user with the unique capacity to quantify the heat produced from aerobic and anaerobic metabolism by measuring heat exchange between the body and the environment. This review provides a brief historical overview of the fundamental concepts which underlie direct calorimetry, of pioneer scientists which developed these concepts into functional pieces of equipment and the subsequent use of direct calorimetry to advance our understanding of energy balance, nutrition, and the pathogenesis of metabolic diseases. Attention is directed to seminal studies that successfully employed direct calorimetry to verify that the law of energy conservation also applies to human beings and to establish the validity of indirect calorimetry. Finally, we discuss the more recent use of direct calorimetry for the measurement of whole-body heat exchange and body heat storage in the study of human thermoregulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
All of the metabolic processes that occur within an organism produce heat and every living organism is an open system that constantly exchanges heat with its surroundings. Heat production occurs via cellular metabolism (bioenergetics) and cell work. Much of our understanding of metabolism and the classical control systems active within living organisms is based on measurements of heat production using the technique of direct calorimetry. In the study of living organisms, direct calorimeters have been developed to precisely measure heat production from metabolism. Direct calorimetry of the living system had its origins in the 18th century with the ice calorimeter of Lavoisier and Laplace who were the first to use this method to measure animal heat. Their work led to the observation that the source of animal heat was due to the combustion of carbon fuel. In the late 19th century, the first human calorimeter was constructed—the Atwater–Rosa calorimeter (also referred to as a respiration calorimeter), which marked the start of more than 200 years of human metabolic research using direct calorimetry. The calorimeter enabled the measurement of gaseous exchange between a living organism and the surrounding atmosphere (indirect calorimetry), as well as the simultaneous measurement of the heat produced by that organism (direct calorimetry). Numerous experiments relating energy input to energy expenditure successfully verified the law of conservation of energy in human beings. Moreover, it established the validity of the relationship between direct and indirect calorimetry by demonstrating that an equivalency exists between the fuel consumed and the heat generated in humans. These early findings revealed that energy expenditure can be directly measured in humans (direct calorimetry) or estimated by measuring the consumption of oxygen and translating these quantities into a heat equivalent (indirect calorimetry). For practical reasons, indirect calorimetry has now become the method of choice for the routine measurement of whole-body metabolism and energy expenditure. Direct calorimeters continue to be used today for the measurement of whole-body heat exchange in the study of human thermoregulation. The present review will discuss how this technique was employed to advance our understanding of metabolism (energy balance and nutrition) in human beings both in health and in disease, as well as the classical control systems (e.g., temperature regulation) active within the human system.
Heat energy and exchange
In the study of chemical reactions, the heat of a reaction is the heat exchanged between a substance and its environment. During spontaneous decomposition of a substance, there is usually a release of heat to the surroundings and this heat can be measured by allowing the reaction to occur in an enclosed, isolated system of known heat capacity. The reaction heat may be measured by the change in temperature of the system. Heat energy can only be conceived as coupled with an exchange of energy and is always associated with a heat flux or exchange. The idea of energy flux between two systems underlines the quantitative nature of energy and of heat energy in particular. As such, heat is the quantity of energy exchanged per unit time between two systems in the form of a heat exchange. By the strictest definition, calorimetry is the measurement of heat energy and a calorimeter is used to measure this heat.
Calorimetry and energy expenditure
Every living organism is in constant heat exchange with its environment and measuring the heat released from metabolism requires a very sophisticated system—the calorimeter. As such, calorimetry plays a pivotal role in our ability to understand the function of the human system within its environment. The maintenance of all body functions including the active transport of chemical and electrical gradients across cellular membranes, the synthesis of macronutrients, muscle contraction, and other physiological processes requires the constant expenditure of the energy-rich adenosine triphosphate (ATP) molecule which is harvested from the consumption of food and oxygen. Through this process of cellular metabolism (bioenergetics), some amount of energy is lost in a form that is unusable and liberated as heat. Physical activity provides the greatest demand for energy. During physical activity, energy output from active muscles increases well above resting levels in proportion to the volume of muscle mass involved and the intensity at which the activity is performed.
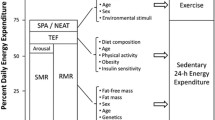
Calorimetry, which derives from the Latin word ‘calor’ (heat) and the Greek word ‘metrion’ (measure), is used to quantify energy expenditure during rest or physical activity. The rate of heat production in an individual is directly proportional to energy expenditure and, therefore, metabolic rate. As such, energy expenditure, and, therefore, heat energy produced by the body, can be accurately quantified by measuring heat release with direct calorimetry. Energy expenditure may also be estimated from the quantitative measurement of the chemical by-products of metabolism, a process termed indirect calorimetry, whereby the measurement of heat production is assessed by gas exchange (Fig. 1). Since all energy-releasing reactions in the body ultimately depend on oxygen and because a direct relationship exists between oxygen consumed and the amount of heat produced in the body, the measurement of oxygen consumption, therefore, provides an indirect, yet highly accurate, estimate of energy expenditure.
Indirect versus direct calorimetry. Instead of measuring the heat produced as a result of biological reactions (direct calorimetry), the rate of oxygen (O2) consumption and carbon dioxide (CO2) production during biological oxidations at rest or during physical work is used to estimate heat production (indirect calorimetry)
Origins of calorimetry
In the late 18th century, French chemist Antoine Lavoisier (1743–1794) with the aid of Pierre Simone Laplace (1749–1827), a prominent French mathematical physicist and astronomer, were credited with the development of the first animal calorimeter (Lavoisier and Laplace 1780). They conducted their first series of experiments (performed over a 1-day period) on the generation of heat of a living animal in the winter of 1783 (Lodwig 1974). However, some believed that Scottish chemist and physicist Adair Crawford, a pioneer in the development of calorimetric methods for measuring the specific heat capacity of substances and the heat of chemical reactions, was the first to measure animal heat albeit his work appeared later (Crawford 1788). Lavoisier, who has been called the “Father of Modern Chemistry” for his fundamental contributions to this science, disproved the phlogiston theory (which postulated that a fire-like element called phlogiston is contained within combustible bodies and released during combustion) by demonstrating the existence of oxygen as the agent of combustion. In their work on the study of combustion and animal heat, Lavoisier and Laplace placed guinea pigs within a calorimeter (an adiabatic device) which contained an outer shell packed with snow and an inner layer filled with ice. As the metabolic heat from the animal melted the ice, the water was collected and weighed to allow the calculation of the heat absorbed using the latent heat of ice. Lavoisier and Laplace also estimated the amount of carbon dioxide production from the same animals. By measuring the heat and carbon dioxide generation of burning charcoal, they could estimate the amount of heat loss per unit carbon dioxide production. In light of their observation that heat production estimated by indirect calorimetry nearly matched the heat measured by direct calorimetry, they concluded that the heat produced by the animal was the product of slow combustion of carbon, a process comparable to combustion of charcoal (Holmes 1985). While their observations provided important new insights into animal energetics, they were unable to identify, where within the body, this heat was produced. As with many direct calorimeters, their calorimeter had a number of limitations (e.g., experiments had to be conducted in the winter when air temperature was near freezing), and following their initial experiments, the calorimeter saw little use (Lodwig 1974).
Origins of indirect calorimetry
Many years later, Césav-Mansuète Despretz (1824) and Pierre Louis Dulong (1841) found a significant discrepancy between heat production and respiration of guinea pigs albeit the reasons for this disparity remained unresolved. They concluded, however, that the combustion of carbon and hydrogen alone could not be responsible for animal heat production (Kleiber 1961). They directly measured heat production of the animals using a water bath calorimeter that measured the temperature of a known mass of water. Despretz won a prize in 1824 for his thesis on animal heat production. The calorimeter was subsequently improved by Lefèvre (1911) who also originated the first convection or air calorimeter. In 1849, Henrik Scharling and later, in 1877, Claude Bernard examined heat production in large animals and humans using a water-cooled calorimeter. These early measures of heat production did not, however, elucidate to any degree the metabolic processes involved. In 1849, famous French chemist and physicist Henri V. Regnault (1810–1878) and the physiologist Jules Reiset (1818–1896) devised a closed-circuit system for the measurement of oxygen consumption using a sealed space and carbon dioxide absorbers (Regnault and Reiset 1849). In 1850, Regnault and Reiset published an account of respiration experiments, wherein small animals were placed under a bell-jar containing a known quantity of oxygen. Oxygen was provided to replace the amount consumed by the animal, while carbon dioxide was removed from the system by pumping the expired air through potassium hydrate. The oxygen consumed by the animal and its environment could be readily quantified by determining the volume of oxygen required to maintain constant pressure in the system (Poncet and Dahlberg 2011). However, since the carbon dioxide in expired air was ‘scrubbed’ during this process, their system did not permit the measurement of carbon dioxide production from the animal. In Munich, Germany, Carl von Voit (Physiologist, 1831–1908), who has been referred to as the founding father of metabolic research and is best known for his pioneering use of indirect calorimetry, modified the system with the help of his colleague Max Joseph von Pettenkofer to allow both oxygen consumption and carbon dioxide production to be measured. Their open-circuit method and that of Regnault and Rieset were essential tools for understanding human metabolism. Voit’s subsequent work on metabolism in mammals, including humans, helped establish the study of the physiology of metabolism and the foundation of modern nutritional science. In particular, his discovery that the urinary excretion of nitrogen (i.e., urea) was related to the rate of protein metabolism (Cathcart 1921; Voit 1866), combined with the respiratory exchange ratio, made it possible to quantitatively determine the relative contributions of different fuel sources (i.e., carbohydrates, fats, and proteins) to whole-body metabolism.
Indirect calorimetry
While direct calorimetry is considered the gold standard method for quantifying heat production, indirect calorimetry is the most widely employed method to measure rates of energy production and, therefore, substrate oxidation. It is a technique that has been used for over two centuries and has led to major advancements in our understanding of nutrition and energetics, thermogenesis, the energetics of muscular exercise, the pathogenesis of metabolic diseases, and others areas. Because heat production is not measured directly, the term ‘indirect’ calorimetry is used.
Open-circuit spirometry is the most common technique used to indirectly quantify energy expenditure. Systems today typically combine automated and continuous metabolic gas analysis as well as electronic flow sensors to measure ventilation, and computer technology for instantaneous calculations. Portable systems have even been developed, allowing scientists to measure energy expenditure during a wide range of activities performed in different environments (i.e., mountain climbing, swimming, outdoor cycling, deep-mechanized mining work, etc.). The basic premise of indirect calorimetry is to measure the difference in oxygen and carbon dioxide contents between expired and inspired air which, along with minute ventilation, allows the quantification of oxygen consumption and carbon dioxide production. Oxygen consumption and carbon dioxide production are subsequently used to calculate the respiratory exchange ratio, an estimate of substrate utilization. This allows for the calculation of energy expenditure using the caloric equivalents for macronutrients. While the basic principles of indirect calorimetry are well established, it is important to recognize that there are some potential limitations. The reader is referred to specific reviews published by the European Journal of Applied Physiology for a more in depth discussion of techniques associated with indirect calorimetry. Relevant to this article, it is important to remember that indirect calorimetry measures energy expenditure, not metabolic heat production. Metabolic heat production represents the amount of energy liberated as heat during metabolic processes which is not directed to performing external work. At rest, energy expenditure is equal to metabolic heat production as no external work is performed. During exercise, however, a certain amount of energy produced by metabolism goes towards performing external work. Humans are at most 20% efficient during exercise, meaning that a minimum of ~80% of energy expenditure is liberated as heat (Whipp and Wasserman 1969).
Direct calorimetry
As applied to whole organisms, direct calorimetry involves placing an individual within a small chamber which is insulated from the environment. It is not the most convenient method for quantifying energy expenditure, albeit it relies on quite easily measured physical principles. Unlike indirect calorimetry, direct calorimetry measures the total heat dissipated by the body as a result of both anaerobic and aerobic metabolisms. Anaerobic contribution to overall metabolism can be quite substantial in a wide range of activities and is a key contributor in the early stages of exercise (Pahud et al. 1980). Of fundamental importance to our understanding of direct calorimetry is the law of conservation of energy which states that the total energy of an isolated system cannot be created or destroyed, but can be converted to a different form of energy. Within the human system, energy is converted to different forms all the time. For example, the food we ingest and store starts as chemical energy, with the latter stored in the bonds of macromolecules (e.g., muscle and liver glycogen) and ATP. When physical activity is performed (e.g., gardening, walking, running, cycling, etc.), this chemical energy is converted to mechanical energy and heat. During exposure to a cold environment, metabolic heat is released from the initiation of shivering to prevent potentially dangerous reductions in body core temperature. These and all other metabolic processes that occur within the body ultimately result in heat production which can be measured by direct calorimetry.
Indirect and direct calorimetry: the relationship
While direct and indirect calorimetries have inherent limitations, they are both valuable techniques for assessing energy expenditure. However, it is important to remember that direct and indirect calorimetry do not measure the same energy. As outlined above, indirect calorimetry estimates energy expenditure from measurements of oxygen consumption and carbon dioxide production. In contrast, direct calorimetry estimates energy expenditure from the measure of heat dissipation from the body. In a resting state of thermoneutrality, heat loss from the body is equal to metabolic heat production from oxidative processes in the body. Under these conditions, all the energy transformed within the body is dissipated as heat, including internal work such as the mechanical work of the heart and lungs which is ultimately converted into heat (McLean and Tobin 1987; Webb 1985). However, there are important limitations to consider when employing direct calorimetry. Metabolism increases in direct proportion to exercise intensity and a steady-state rate of oxygen consumption is reached within 1–2 min (see Fig. 1 in Kenny et al. 2008). Thus, while an increase in heat released by oxidative processes can be rapidly assessed by indirect calorimetry, this is not paralleled by a similarly rapid increase in heat loss. In these situations, indirect calorimetry has the advantage of a faster response time, whereas direct calorimetry is associated with a more delayed response (Kenny and Jay 2013). This disparity is best evidenced under conditions where rapid changes in metabolism and, therefore, heat production occur such as during dynamic exercise (see Fig. 1 in Kenny et al. 2008). The human body constitutes a large heat capacity that undergoes changes in heat storage. Thus, under conditions wherein acute and rapid changes in metabolic heat production occur, such as during the early stages of exercise, a large part of the heat produced is stored in the body resulting in a change in body temperature (see Fig. 3 in Kenny et al. 2008). At the onset of exercise, the increase in total heat loss lags behind the more rapid increase in heat production. As a consequence, there is a delay in achieving a steady-state rate of total heat loss. As long as a mismatch between heat production and total heat loss is maintained, heat will be stored in the body resulting in elevations in body temperatures (muscle and core). However, as exercise continues, no further increase in body temperature is observed. This is due to heat balance being achieved, which occurs when heat production equals heat loss. Thus, following an initial delay, rate of heat generation (indirect calorimetry) will become equal to the rate of heat dissipation (direct calorimetry).
Direct calorimeters
To be effective, a calorimeter must be a closed system to ensure that all of the heat produced from metabolism is measured, and no transfer of energy occurs between the calorimeter and its surroundings (Webb 1985). Meeting these specifications requires a highly sophisticated system which can be both costly and technically challenging to achieve. In their most simple form, calorimeters measured only the nonevaporative components of total heat loss (i.e., sensible or dry heat loss) consisting of radiant, convective and conductive heat transfers. For many calorimeters, modifications were required to allow for the separate evaluation of evaporative (i.e., insensible) heat loss from the skin, respiratory tract, and production of sweat (McLean and Tobin 1987; Webb 1985). However, with advancements in technology, more sophisticated calorimeters were constructed to permit the continuous measurement of both evaporative heat loss and dry heat exchange (McLean and Tobin 1987; Webb 1985). These ingeniously designed calorimeters proved especially valuable in the study of human thermoregulation. One obvious limitation of direct calorimetry is the fact that it cannot be used during most daily activities as calorimeters require the individual to be isolated within a confined space. To circumvent this problem, large size calorimeters were developed which allowed scientists to perform measurements of heat exchange during a wide range of activities associated with normal daily living (e.g., sleep, eating, clerical work, exercise, etc.). As discussed below, studies stemming from these calorimeters served to advance our understanding of human metabolism which included germinal studies of energy balance, nutrition, pathogenesis of metabolic diseases (e.g., obesity), thermoregulation, and other key areas. In the following sections, we review the development of calorimetry and highlight some of the classical studies conducted with these unique systems.
The first direct calorimeters for use on animals
Around the turn of the 20th century, there was considerable interest in the development and use of adiabatic calorimeters with an emphasis placed on proving the agreement between direct and indirect calorimetry. Much of this effort stemmed from the development of animal calorimetry by Voit, as the Pettenkofer-Voit apparatus for quantitative evaluation of respired gases of humans and animals provided a mathematical definition of nutrients (Lusk 1932). Voit had himself constructed a direct calorimeter, but no studies were ever published (Lusk 1932). Voit’s students, Max Rubner (1854–1932), and Wilbur Olin Atwater (1844–1907) also went on to make significant advancements in the field of calorimetry. In fact, it was Atwater who later led the development of the first human calorimeter in 1892 at Wesleyan University in the United States with the Atwater–Rosa calorimeter. Around the same time in Germany, Rubner (1894) performed calorimetric measurements on dogs using both indirect and direct methods and demonstrated that a correlation existed between the two methods. Rubner’s calorimeter employed the thermal gradient between an isothermal animal chamber and an air space surrounding the chamber (McLean and Tobin 1987). The volume change produced by the small rise in air temperature was used to calculate heat loss. Evaporative heat loss was also measured. Using an open-circuit Voit-Pettenkofer respirometer, Rubner was able to perform the simultaneous measurement of energy expenditure and demonstrate a strong agreement between direct and indirect calorimetry. From measurements performed on a dog living in the calorimeter for 45 consecutive days, 17,439 calories were measured by the calorimeter compared to 17,406 calories computed from nitrogen loss in urine and feces and the carbon dioxide in respiration, a difference of only 0.2% (Lusk 1932; Rubner 1894). His work showed that Hess’ law (an expression of the principle of conservation of energy) was applicable not only in chemistry, but also in biology. As discussed below, Atwater and colleagues also verified the same principle on human subjects (DuBois and Riddle 1958). Noteworthy, in addition to his work on animal metabolism, Rubner made a significant advancement to our understanding of temperature regulation by classifying physical heat loss and chemical heat production (Rubner 1883).
In 1901, Henry P. Armsby of the Pennsylvania State College, with the assistance of Professor Jons A. Fries and I. Thornton Osmond, started the construction of the first respiration calorimeter in the world large enough to study cattle (Fig. 2). Operational in 1902, the calorimeter consisted of an airtight, thermally insulated chamber. The heat produced and radiated by the animal within the calorimeter was removed by a constant flow of cold water circulating in copper conduits (heat absorbers) located below the chamber’s ceiling. The heat produced by the animal was determined by measuring the difference between the temperature of the water entering and leaving the chamber. By measuring the heat released during feeding, they could determine the nutritive value of different feed by assessing how much energy an animal was able to derive from different food sources (Armsby 1913; Armsby and Fries 1913, 1919). This calorimeter was subsequently used for human studies wherein energy expenditure was assessed for different diets (Swift et al. 1958). However, it required two men to produce enough heat to be accurately measured. Over the subsequent years, a number of comparable large calorimeters were built to study food energy requirements of farm animals (Kleiber 1935; Mitchell and Hamilton 1932; Mollgard and Anderson 1917; Ritzman and Benedict 1929). This included the chamber developed at Cambridge University in England by Archibald V. Hill (1886–1977) for work on sheep and dogs (Hill and Hill 1914) and others for work on pigs and young cattle (Capstick 1921; Deighton 1926). Differential calorimetry was also used for the study of energy expenditure in small animals (Benedict and Lee 1937; Deighton 1939). Unlike other calorimeters, this type of calorimeter provided a high speed of response to rapid changes in heat output. The calorimeter generally consisted of two identical cylindrical chambers—one containing the animal and the other an electric heating element. Both chambers were made of very thin metal mounted side by side in a large duct though which preconditioned air was passed by a fairly elaborate ventilation system. The air flow in the heating element was continuously adjusted, so that the rise in temperature of both chambers was the same. The rate of heat delivery to the element in one chamber was then taken to be equal to the nonevaporative heat output of the animal in the other (McLean and Tobin 1987).
The first direct calorimeter for use on humans
As noted above, in 1892, Atwater commenced the construction of the first direct calorimeter for use in the study of human metabolism at Wesleyan University with the indispensable help of expert physicist Edward B. Rosa (1861–1921) and chemists Charles F. Langworthy (1864–1932) and Francis G. Benedict (1870–1957). Langworthy and Benedict joined the team in 1893 and 1895, respectively. The construction of the calorimeter was completed in 1897 and in 1901 Rosa formally ended his collaboration with the group due to his new responsibilities as chief physicist of the Bureau of Standards at Washington. The Atwater–Rosa calorimeter, an adiabatic or heat-sink direct calorimeter (also often called a respiration calorimeter), was the first human calorimeter used to simultaneously measure oxygen consumption and whole-body heat loss (Atwater 1905; Atwater and Rosa 1899a, b, c). It was rebuilt several times and successive improvements were made. The original Atwater–Rosa calorimeter employed the open-circuit Pettenkofer system for the indirect estimation of energy expenditure. However, this technique yielded measurement errors as a high as 24% depending on whether carbohydrate or fat was being oxidized. Around 1902, Atwater subsequently integrated within their calorimeter the closed-circuit system for the measurement of oxygen consumption developed by Regnault and Reiset in 1849 (Regnault and Reiset 1849). This revised approach made it possible to measure not only the non-protein carbon in respiration, but also to calculate how much of the oxygen absorbed was used for the metabolism of fat and carbohydrate. In this way, energy expenditure could be calculated by the respiratory quotient method instead of the carbon–nitrogen balance. The Atwater–Rosa calorimeter also permitted the measurement of heat loss. A liquid cooled copper coil inside the chamber, which was attached to heat exchangers conveying water, was regulated, such that the heat absorbed exactly balanced the heat produced by the subject. The increase in temperature of a known volume of water served as the basis for calculating nonevaporative heat loss. Evaporative heat loss (respiratory and sweating) was quantified by recirculating air through a system of freezers to absorb water (McLean and Tobin 1987). In addition to measuring whole-body heat exchange, their studies included the measurement of internal body temperature which demonstrated, for the first time, an interest in the study of heat exchange and human thermoregulation.
Atwater and Benedict conducted numerous studies on rest, exercise, and diet using the Atwater–Rosa calorimeter until Atwater’s death in 1907. Their studies played a key role in the empirical justification for the standard tables and formulas giving calorific equivalents of oxygen and carbon dioxide based on respiratory gas exchanges. Their numerous experiments relating energy input to energy expenditure successfully verified the law of the conservation of energy in human beings and established the validity of the relationship between direct and indirect calorimetry. Benedict noted himself that “the development of the closed-circuit respiration apparatus and calorimeter at Wesleyan University is, in my judgment, the most important mechanical contribution I have been privileged to make. This was developed from the ground up, based upon the idea that if the actual amount of oxygen absorbed by the human body in life processes could be directly measured, such a measure would have great significance in the comparison with the simultaneous heat production” (DuBois and Riddle 1958).
Benedict relocated the Atwater–Rosa calorimeter to Boston at the Nutrition Laboratory of the Carnegie Institution of Washington (he was appointed its director from 1907 to 1937), where he continued to carry out many experiments in his new nutrition laboratory. Built alongside Harvard’s Medical School, it became famous as one of the leading research laboratories in the United States (DuBois and Riddle 1958). Benedict developed two smaller calorimeters based on the Atwater–Rosa concept and devised several much smaller and relatively inexpensive instruments for measuring oxygen consumption as a means of estimating energy expenditure. This included the “Benedict apparatus” which was widely employed in hospitals to assess metabolism in patients (1916–1918). He also modified various devices to measure heat production of both humans and animals and his work added much to our understanding of heat production and heat regulation. With respect to his studies in humans, his work included the study of metabolism in newborn infants (Benedict and Talbot 1915), growing children and adolescents (Benedict 1919), men and women (Benedict et al. 1914), starving people (Benedict and Roth 1918), athletes (Benedict and Smith 1915) and vegetarians (Benedict and Roth 1915) as well as the investigation of the effects of diet, temperature regulation, and exercise on metabolism. During this same period, Lusk’s technical assistant, H. B. Williams at Cornell University Medical College, New York, developed a small respiration calorimeter (constant-temperature water-cooled calorimeter) also designed from the Atwater–Rosa calorimeter (Williams 1912) to assess energy metabolism in infants and small animals. An animal or child rested in an air-filled copper box through which water was circulated through a system of pipes to carry away the heat produced by the subject at the same rate that it was produced. The heat produced was then calculated based on the flow rate of the water and the temperature increase between the inflow and outflow. Evaporative heat loss was determined from the amount of water vapor contained in the air absorbed by sulphuric acid. Closed-circuit gas flow was used to measure oxygen consumption and carbon dioxide production (Williams 1912).
As the science of human calorimetry developed, an increasing number of calorimeters were constructed albeit smaller in size to the original room size machine of Atwater and Rosa. While the studies conducted in the Atwater–Rosa calorimeter provided valuable new insights into our understanding of whole-body metabolism in humans, many of the experimental studies carried out in this relatively large calorimeter lasted several hours from which only one or two good hours of measurements were typically acquired. The prolonged nature of the trials was designed to get the patient or subject and the calorimeter into a steady state. Transients in temperature, heat production, and metabolism caused significant errors in the estimate of energy expenditure. The transition to a smaller size calorimeter was an effective way of reducing the time required to achieve stability, thereby allowing for faster response times owing to the smaller thermal mass of the chamber. As such, valid data over a much shorter time period (e.g., 1 h) could be collected rather than the ≥6-h data periods of the typical studies conducted in the original Atwater–Rosa calorimeter.
Direct calorimeters used for the study of human metabolism
In 1909, Graham Lusk (1866–1932), who had recently been appointed Professor of Physiology at the Cornell University Medical College in New York City, had also developed a small respiration calorimeter. His small calorimeter was used to study both dogs and children, including sleep studies in children. Of note, John Howland (Physicist) was the first to use this calorimeter to perform the simultaneous measurement of heat loss and heat production in infants. He found a difference of less than 3% between both measures (Howland 1912). Inspired by his work with Carl von Voit (Lusk studied with him in 1887), particularly in nutrition and metabolism, and his appreciation of Rubner’s work in calorimetry (Editorial 1965), Lusk subsequently constructed a human calorimeter in 1912 (see below). Dr. H. B. Williams, a member of the Cornell physiology department, and J. A. Riche who were both well versed in the use of the Atwater–Rosa calorimeter contributed to its development. Lusk devoted his career to the understanding of metabolic processes through the use of the calorimeter in the analysis of intake and output, in both normal and pathological states (e.g., diabetes). Lusk published extensively on these subjects and his best known publication was his book titled The Elements of the Science of Nutrition which was first published in 1906 and was highly cited even after his death in 1932 (Lusk 1906).
The sage calorimeter
In 1912, Lusk became scientific director of Cornell’s Russell Sage Institute of Pathology. He invited Eugene F. Dubois (1882–1959) to join as medical director of the Institute. Prior to this period, DuBois had worked at the Charité Hospital in Berlin for a 2-year period starting in 1909 to work under Theodor Brugsch (1878–1963). Interestingly, it was on the advice of John Howland that Dubois went to study the newly emerging field of human metabolism in Berlin. Prior to this chance meeting, DuBois had planned to study bacteriology in France. While in Berlin, he met Borden Veeder (a graduate of Pennsylvania Medical School, later a professor of pediatrics at Washington University in St-Louis), and with his help, they resurrected the Pettenkofer-Voit metabolic machine, where he served as the control subject for many of their experiments (Aub 1962). In 1910, they published their first collaborative study examining energy requirements in diabetes (Dubois and Veeder 1910). While in Berlin, Graham Lusk visited their facilities. As noted above, Lusk had recently commenced his study of energy requirements in dogs and recognized the exciting possibilities of studying this in humans during his visit to Berlin. Upon returning to the United States, Dubois returned to the department of pathology at Presbyterian Hospital in New York, where he was interning prior to his departure to Europe. However, having developed a strong interest for the emerging field of calorimetry and metabolism, and his desire to extend his work on metabolism in disease, he accepted Lusk’s invitation to join the Russell Sage Institute of Pathology of Cornell Medical School. It was there that he remained for the duration of his career carrying out extensive studies of human metabolic rate and temperature regulation during health and disease. A large calorimeter suitable for patients was constructed and installed in a metabolism ward in Bellevue Hospital—the Sage calorimeter. The calorimeter was designed based on the ‘small’ calorimeter developed by Benedict, and provided the ability to measure energy expenditure and heat loss of man over prolonged periods. The accuracy of the system was remarkable with an average error of 0.9, 0.6 and 1.6% for heat loss, carbon dioxide production, and oxygen consumption, respectively, over a 3–4 h period. A technical description was prepared by Riché and Soderstrom (1915) which appeared in a special issue of the Archives of Internal Medicine. The leading-edge work conducted by Lusk’s team in the large calorimeter dealt with a wide range of topics, such as basal metabolism, typhoid fever, diabetes, metabolic acidosis, intermediary metabolism, heat production, and others. Lusk noted: “The Sage calorimeter reports of the disturbances that nature works and of her cures without having, as concerns the sick human being, at any time, in the slightest degree, affected any patient to his disadvantage, but rather having yielded information regarding his condition which has been beneficial in this subsequent treatment” (Editorial 1915). The publication of a first series of papers on clinical calorimetry appeared in a special supplement to the May 1915 issue of the Archives of Internal Medicine with the first paper summarizing the development of the calorimeter by Lusk (1915b). Others included work on the determination of basal metabolism of normal men and the effect of food (Gephart and Dubois 1915), the measurement of surface area of man (DuBois and Dubois 1915), the absorption of fat and protein in typhoid fever (Coleman and Gephart 1915), the metabolism of typhoid patients (DuBois and Coleman 1915), and the diabetic respiratory quotient (Lusk 1915a). For his part, DuBois was particularly interested in the study of metabolism of disease (e.g., diabetes), including febrile illnesses (e.g., typhoid fever); a field of interest he pursued for much of his career. Interestingly, his work revealed that patients with typhoid fever need food (DuBois 1912; DuBois and Coleman 1915), in contrast to one of the medical dicta of the time that one should not feed these patients (DuBois 1919).
As with many calorimeters, the Sage calorimeter required the continuous attention of a mechanic and it required the subject or patient to be inside the box which was uncomfortable for people who were sick. It was noted by Dubois at the time that if the measurement of energy expenditure could be done indirectly by assessing the amount of oxygen used over time and calculating the amount of energy expended, one would then have a much simpler approach to testing patients in a clinical setting (DuBois 1950). Others had thought of this, but had never standardized the procedure by evaluating a sufficient number of healthy adults so as to determine what was normal and what was not. Furthermore, such an approach would only be valid if it could be shown that direct and indirect measurements were highly correlated not only in healthy individuals but also in clinical population groups. Dubois and his colleagues accomplished both of these tasks (DuBois 1950). Noteworthy, they went even further to standardize the indirect method, by normalizing heat production to body surface area which decreased the variance of the method. By the mid-1910s, Dubois and his team had created reference standards for oxygen consumption at rest—the basal metabolic rate (Gephart and Dubois 1915). As a result of their work, a simpler method of indirect calorimetry to convert basal metabolic rate from an investigative tool to a clinically useful test could now be performed in a relatively short time period. A sharp contrast to the many hours it took to obtain stable measurements by direct calorimetry (DuBois 1950).
In the ensuing years, DuBois and his colleagues produced many integral studies of the pathology of human heat production (Dubois 1916) and on the generation of heat during exercise (Dubois 1937). Many of these studies included women as subjects. In 1932, on the behest of DuBois, Graham Lusk, who was then director of the Russell Sage Institute of Pathology, offered physicist James D. Hardy (1904–1985) a position. He accepted and joined the laboratory in 1932, where he worked closely with DuBois. Dubois noted in his autobiography published by the National Academy of Sciences that “Perhaps my important service was to bring James D. Hardy, a physicist, into the field of physiology where he could apply his basic training in radiation”. Hardy’s research on the measurement and effect of thermal radiation on humans became the cornerstone for his interest in temperature regulation. He published a series of papers from 1934 to 1936 on this subject which included the development of an instrument for measuring the radiation and surface temperature of skin (Hardy 1934). He used a portable radiometer to measure radiant energy flux, which he expressed in calories per second per square centimeter of body surface. Hardy and DuBois continued their work on human thermal physiology until World War II, which took both of them into the Navy. After the work of DuBois, the interest in the clinical applications of calorimetry became of great interest to the medical community. The use of calorimeters to examine and diagnose medical problems took on an important role in the study of various infections such as typhoid and pneumonia. Hardy’s research on the measurement and effect of thermal radiation on humans became the cornerstone for his interest in temperature regulation.
Room-sized calorimeters to measure daily energy expenditure
With an increasing focus on the causes of metabolic disorders such as obesity and diabetes in the mid-to-late 20th century, the clinical evaluation of energy balance and the nutritional requirements associated with these and other metabolic disorders became paramount (Dauncey 1980; Dauncey and Bingham 1983; Durnin et al. 1973; Garrow 1973, 1974; Irsigler et al. 1979; Jequier 1981; Jequier et al. 1974; Seale 1995; Tschegg et al. 1979; Veitl and Irsigler 1983). This, in part, led to the return of larger size calorimeters capable of the dual high precision measurement of whole-body energy expenditure and heat loss over long continuous measurement periods (e.g., 24 h).
In 1977, John S. Garrow (Head of the Nutrition Research Group at the Clinical Research Centre, London, England) constructed a room size calorimeter similar to that of Atwater–Rosa that could be occupied for 24 h (Garrow et al. 1977). In a personal communication to Paul Webb, Garrow noted that “intermittent measurements, such as those made with conventional metabolism devices employing masks, would not help to find differences in energy expenditure in the order of 2%; therefore, a chamber was needed for 24-h measurements”. Measurements of heat output using this chamber had an estimated error of 1% over the 24-h period. Around the same period, Dauncey and colleagues (Dunn Nutrition unit at Cambridge) also developed a heat-sink calorimeter (Dauncey et al. 1978) to investigate the regulation of energy balance and obesity. The calorimeter, designed with the assistance of engineer Peter R. Murgatroyd, who had been instrumental in the construction of Garrow’s calorimeter, was partly based on the heat-sink calorimeter developed by L. E. Mount and co-workers for work with pigs (Mount 1967). It was a relatively large room (2.08 m long and 1.22 m wide; room volume 5 m3) which permitted the evaluation of a broader range of human activities and included furnishings and entertainment facilities. While there were other calorimeters in use around this time period capable of performing similar measurements, they were small in size (i.e., approximately <2 m3) which dramatically restricted the type of activities that could be performed and assessed (Carlson et al. 1964; Spinnler et al. 1973b; Tiemann 1969). A number of larger size calorimeters were subsequently developed that retained the high level of precision typical of smaller units. For example, this included the heat-sink calorimeters by S. Jacobsen (5.8 m3) (Jacobsen et al. 1982) and Joan D. Webster (6.8 m3) (Webster et al. 1986), as well as the gradient-free, isothermic Vienna whole-body calorimeter developed by Tschegg et al. (1979). However, the introduction of even larger size calorimeters enabled measurements of energy expenditure during more dynamic activities such as weight lifting (Jacobsen et al. 1985; Seale et al. 1991). Jacobsen of Odense University in Denmark introduced a 24-m3 heat-skin calorimeter (2.4 m wide and 5.1 m long) (Jacobsen et al. 1985). The system enabled the measurement of energy expenditure (as determined by the measurement of heat output) for periods of up to 72 h with a response of time of 15 min for evaporative and dry heat exchange. James L. Seale at the US Department of Agriculture in Beltsville, Maryland, developed a large water-cooled gradient-layer chamber (20.4 m3) (Seale et al. 1991) suitable for measuring human heat production (Beltsville calorimeter). The chamber was combined with uniquely designed open-circuit indirect calorimetry that provided a continuous measurement of changes in gas composition of the air entering and existing the chamber thus allowing for a high precision partitioning of energy expenditure associated with different activities (e.g., sleep, exercise, rest, and general activities) performed over a 24-h period (Seale 1995; Seale and Rumpler 1997).
While dual indirect and direct room-sized calorimeters served as valuable tools in the concomitant measurements of energy expenditure and heat exchange, there are important limitations that can restrict their usefulness, namely, differences in response time. As noted earlier, the relationship between heat production and heat loss is variable. It is, therefore, necessary that the measured rates of whole-body energy expenditure and heat loss are synchronized as a function of time. In recognition of this important limitation, Seale and Rumpler introduced a set of corrective equations to compensate for the response times of different calorimetry systems (Seale and Rumpler 1997). This made it possible to measure simultaneous heat emission and energy expenditure in a room-sized calorimeter.
A changing focus in the use of direct calorimetry: human thermoregulation
Early research employing direct calorimetry was aimed at studying whole-body metabolism. Prior to World War II, few researchers had employed direct calorimeters for the specific purpose of studying human thermoregulation. However, around this period and over the subsequent years, an increasing number of direct calorimeters were designed with this purpose in mind. While calorimeters continued to be used for clinical purposes (Dauncey 1980; Dauncey and Bingham 1983; Garrow et al. 1977; Jequier 1975; McManus et al. 1984; Meis et al. 1994; Ravussin and Bogardus 1982; Ravussin et al. 1982; Webster et al. 1986), interest in temperature control and thermal physiology was a driving force behind the development of a number of calorimeters built specifically for measuring heat exchange in humans (Chappuis et al. 1976; Close et al. 1980; Glushko et al. 1976; Jacobsen et al. 1985; Reardon et al. 2006; Snellen 1969; Snellen et al. 1983; Spinnler et al. 1973b; Tiemann 1969). As a result, a large number of studies on human thermoregulation employing direct calorimetry have been conducted over the last 50 years. These include studies examining heat exchange at rest (Mitchell et al. 1969; Kenny et al. 2015) and during exercise (Gagnon and Kenny 2011; Kenny et al. 2008, 2009) which included the evaluation of factors such as fluid intake (Snellen 1969; Snellen and Mitchell 1972; Snellen et al. 1972), exercise training (Stapleton et al. 2010), heat acclimation (Poirier et al. 2015), work exposure limits for work in hot conditions (Meade et al. 2016), and others on whole-body heat exchange. Numerous studies were also conducted to evaluate how sex (Gagnon and Kenny 2012; Gagnon et al. 2008), aging (Larose et al. 2013a, b, c; 2014); Stapleton et al. 2015a, b), chronic health disorders such as diabetes (Kenny et al. 2013; Stapleton et al. 2013), and severe burns (Ganio et al. 2012; Jelenko et al. 1979) affect the body’s ability to lose heat.
The first airflow calorimeter
French scientists A. Auguete and J. LeFèvre developed the first convection or air flow calorimeter (Fig. 3). With their calorimeter, they conducted a series of studies aimed at understanding the thermal responses of man exposed to different ambient conditions (Auguet and Lefèvre 1929). With the subjects confined in a ventilated tunnel, the heat output during experimental sessions was estimated from the flow rate and temperature increase of the airstream. An isothermal current of cold air was evenly distributed throughout the chamber by a series of orifices. The air was recirculated, cooled, heated, and purified. Air mass was measured, as was the change in temperature. Condensation in the chamber was prevented by regulating the hygrometric state of the chamber. An ergometer also allowed the participant to perform exercise (Webb 1985).
Schematic diagram depicting an air flow calorimeter. The temperature change of air flowing through an insulated space, multiplied by its mass flow rate and specific heat gives the rate of nonevaporative heat exchange from the subject. The change in water vapor content of the air stream is also measured to determine evaporative heat loss. Image is reproduced with permission from the Paul Webb Collection, Wright University Special Collections, and Archives
The Burton calorimeter
In 1935, John R. Murlin (1874–1960) and Alan C. Burton (1904–1979) developed a new respiration calorimeter at the University of Rochester Medical School (Murlin and Burton 1935). Murlin, who had previously worked with Lusk and the Sage calorimeter in its early days, engaged Burton, a physicist, to develop the chamber. Regarded as the immediate forerunner to the modern gradient-layer calorimeter, the calorimeter embodied both heat-sink and gradient principles and also operated as a closed-circuit respiration chamber (McLean and Tobin 1987; Murlin and Burton 1935). The chamber was a glass cylinder 1.93 m long by 0.58 m in diameter. The cylinder and the piping of the calorimeter were constructed with glass given that they wanted to investigate mechanisms of heat regulation, and artificial states, induced by diathermy (a technique involving the production of heat in a part of the body by high-frequency electric currents). The high-frequency electromagnetic energy from the diathermy machine would have been blocked by metal walls. As with many previous labs, they showed agreement between measurements of direct and indirect calorimetry. Much of their early work was directed at studying processes involved in simple oxidation, such as the conversion of carbohydrate to fat, production of lactic acid, and conversion of glucose to glycogen.
With the addition of body temperature measurements, Burton began the first experiments using direct calorimetry to study human thermoregulation. Burton’s estimate of the average temperature of the body calculated from the temperatures of the skin and core represents a landmark study in human thermoregulation (Burton 1935). He proposed a two-compartment thermometry model that splits the body into a “core” compartment measured using the change in rectal temperature and a “shell” compartment measured using the change in mean skin temperature. The contribution of each compartment is determined by a sum-to-one ratio of weighting coefficients (a, alpha) for core (T co) and skin (T sk) as follows:
The general form of the equation was based on the logic that core tissues are relatively homogeneous whereas tissue temperature in the periphery decreases parabolically from core temperature to skin temperature. The value of a (alpha), the coefficient describing the contribution of core temperature to mean body temperature, was then estimated by simultaneously measuring the change in body heat content (in a calorimeter), core temperature, and mean skin temperature. The resulting value of the coefficient alpha was 0.64, thus giving the formula:
To this day, the formula is widely used albeit different weighting coefficients that are dependent on ambient temperature conditions were introduced (Kenny and Jay 2013). Using a similar approach to that employed by Burton, Hardy and DuBois (1938) proposed a coefficient of 0.7 for a neutral environment; Stolwijk and Hardy (1966a) proposed a coefficient of 0.7 for a hot environment; and Snellen (Snellen 1966) found that the coefficient to be ≈0.8 during exercise performed in a hot environment. Subsequently, Colin et al. (1971b) reported that Burton’s coefficient was correct for a neutral environment; however, they showed that the coefficient increased to 0.79 in an extremely warm environment. Burton later worked with another calorimeter, this one an insulated bath tub that employed a compensating heater (Burton and Bazett 1936). His purpose was to study temperature regulation further, with special emphasis on the variability of the blood circulation in the skin. In 1942, Day and Hardy (1942) designed a scaled-down version of Burton’s calorimeter to study heat loss in neonates. A key challenge faced in conducting calorimetry-based studies on neonates was the ability to quantify the rather low heat loss of the preterm and term neonate.
The first partitional calorimeter
During the same period that Murlin and Burton developed their calorimeter, the first partitional calorimeter was developed by Charles-Edward A. Winslow (1877–1957) and colleagues at the John B. Pierce Laboratory of Hygiene (now the John B. Pierce Laboratory), New Haven, Connecticut (Winslow et al. 1936a, b) which enabled them to perform elaborate studies of human thermoregulation. As they noted, their calorimeter offered two advantages over traditional calorimeters. First, “it makes it possible a record of thermal interchanges as they occur within a brief interval of time instead of summing up results extending over a period of several hours, in which the process of adaptation is masked by cumulative averages”. Second, “its data are given in terms of rates of thermal interchange partitioned by primary measurement in accordance with the physical avenues through which the interchanges occur”. It was not a typical calorimeter but rather an open, unsealed chamber that permitted the partitioning of heat loss into conductive, convective, radiative, and evaporative components as well as a separation of heat loss via the lungs and skin (Winslow et al. 1936a, b). It was a creative device for estimating each parameter of the heat balance equation without actually measuring them directly. The subject sat on a scale which recorded weight loss and was surrounded by reflecting walls whose radiant temperature could be altered. Respiratory measurements using a mask system allowed the calculation of energy expenditure, metabolic water, and metabolic weight losses. Temperature measurements of the deep body, skin, and surroundings allowed for the calculation of body heat storage, while measurements of skin and surrounding temperatures allowed for the calculation of heat exchange by radiation and convection. Evaporative heat loss was calculated from weight losses attributable to moisture evaporation. The design of the calorimeter permitted a high speed of response. However, a key shortcoming of their calorimeter was the fact that the heat-flow coefficients were applicable only to their special conditions—a semi-reclining subject confined in the slow-moving airstream of their calorimeter and with no drip-off of sweat from the body (McLean and Tobin 1987). Their leading-edge studies in human calorimetry defined the physical principles that are central to how humans exchange energy with their environment (Winslow et al. 1937) and laid the foundation for later studies in pulmonary and thermal physiology and air quality and pollution.
The gradient-layer calorimeter
An important advancement in direct calorimetry was made by Theodore H. Benzinger (1905–1999) and co-workers following the end of World War II. They introduced the thermoelectric measurement of the mean temperature gradient across a thin plastic layer (Benzinger and Kitzinger 1949a, b) and subsequently constructed the first gradient-layer calorimeter to study adult humans. The advantages of the gradient-layer calorimeter over earlier designs were its rapid response time, which enabled studies of dynamic thermal events, and its relative simplicity of operation compared with earlier calorimeters which required tedious calibrations to perform measurements (McLean and Tobin 1987). Benzinger, a former physiologist and Director of the German Air Forces Testing Center (1934–944), was the Director of the bioenergetics division of the US Naval Medical Research Institute in Bethesda, where the calorimeter was built. A primary focus of their work was to conduct the calorimetric evaluation of whole-body heat exchange for the purpose of studying the effector system of human temperature regulation. In their gradient-layer calorimeter (Benzinger et al. 1958), which was later adapted by Spinnler et al. (1973b), the temperature gradient was measured across a thin plexiglass sheet. The difference in temperature between the inner and outer surfaces of the sheet was measured at approximately 6000 sites of small, equal surface area using interlaced thermocouples all connected in series. Since the difference in resistance across the material is precisely dependent upon the temperature difference between the two sides of the gradient layer, the rate of dry heat exchange via radiation and convection from the participant could be estimated. Using a series of heat exchangers lined with similar gradient layers, which they called platemeters, they were also able to precisely measure evaporative heat loss from their participants (McLean and Tobin 1987). Temperature conditions within the calorimeter could be controlled from near freezing to temperatures well above human heat tolerance. With this design, a rapidly responding and continuous measurement of total heat loss was possible for the first time. Earlier calorimeters required at least 1 h for a full response which limited their use to steady-state conditions only. More importantly, their system permitted the precise partitioning of the rate of dry heat exchange and evaporative heat loss. With concurrent measurements of aural canal temperature [developed at this laboratory and which provided an estimate of central nervous system temperature (Benzinger 1963a)] and skin temperatures, they were able to conduct advanced studies aimed at examining the thermoregulatory system of man during rest and exercise in cold and hot environments. These studies led to modifications in the classical concepts of body temperature regulation (Benzinger 1959, 1961, 1963b; Benzinger et al. 1961). Their research also led to the development of screening and selection criteria of personnel for exposure to extreme temperatures, development of cold and heat acclimation protocols, exposure limits for work in extreme temperatures, evaluation of protective clothing, and others.
Webb’s portable suit calorimeter
The desire to estimate energy expenditure and study thermoregulatory responses outside the confinement of a calorimeter led some researchers to find alternative approaches to measure heat exchange. For example, Close and co-workers examined the use of heat-flow meters spaced equally in a belt fastened in contact with the skin around the subject’s waist (Close et al. 1980). However, their system was found to be less accurate under conditions of elevated sweating and was limited for use in sedentary individuals. A few investigators began to investigate the possibility of developing calorimeters in the form of suits for the measurement of heat exchange (Gorodinskii et al. 1976; Webb et al. 1972; Young et al. 1951). A suit capable of measuring segmental heat loss was introduced by Young et al. (1955); however, it had limited use due to the accumulation of sweat inside the garment. Subsequent to the development of cooling suits such as the ones used by NASA, Paul Webb (1923–2014) began to investigate the possibility of adapting these suits. On this basis, he introduced a suit calorimeter which was an interesting variation of the heat-sink technique (Webb et al. 1970, 1972). The insulated suit incorporated a network of thin plastic tubing worn against the skin through which water flowed (Fig. 4). Water was circulated through the suit and the temperature of the influent water was adjusted to match the rate of heat production from the subject. However, without the precise control of the individual’s thermal physiology, an accurate measurement of heat exchange was not possible. During their studies, the temperature of the cooling water was controlled so as to maintain the subject in comfortable thermal balance. It could be sufficiently regulated to accommodate quite heavy work rates by the subject without sweating being induced (Webb et al. 1988, 1991) (Fig. 4). As Webb noted, “with good control, thermal comfort can be achieved day and night at any level of physical activity. A vigorously exercising subject with a metabolic rate of 15 kcal/minute is as readily controlled as is a small sleeping person with a metabolic rate of 0.5 kcal/minute”. When worn, the suit calorimeter was connected to a computer by an “umbilical cord” containing the many cords and tubes involved. The subject was able to move about relatively unrestricted—the ultimate level of portable calorimetry. As water was pumped through the tubes, it carried the heat through a specially designed computer system that provided real-time measurements of heat production during rest and exercise under many varied working conditions (Webb 1985). Studies were conducted over extended periods and included studies in women (Webb 1986) and obese subjects (Webb 1981) under varied nutritional status. It was also possible for the subject to wear the suit calorimeter and at the same time calculate heat production from measures of energy expenditure (by indirect calorimetry), accounting for any external wok performed (Fig. 5). Combined use of the two systems made it possible to analyze heat balance parameters simultaneously over 24-h periods, while the subject remained free from the confined space of the calorimetric chamber (Brun et al. 1985).
Suit calorimeter worn by a participant exercising on a cycle ergometer. The insulating garments cover the water-cooled suit which connects to the hardware for controlling water temperature, located on the equipment cart to the right side of the participant. An automated metabolic unit is used to measure gas exchanges. Image is reproduced with permission from the Paul Webb Collection, Wright University Special Collections, and Archives
The Snellen calorimeter
Instrumental to the advancement of direct calorimetry in the study of human thermoregulation was the introduction of new technology that enabled a rapid response time. Like the Benzinger calorimeter (response time of 0.5 min) (Benzinger et al. 1958), many of the newly developed calorimeters had very rapid response times (Snellen et al. 1983; Spinnler et al. 1973a; Reardon et al. 2006). The interest in calorimetry had grown to the extent where a commercial version of the Spinnler calorimeter was made available (Thermometrics, La Jolla, Ca) (Poppendiek and Hody 1972). In addition, the air flow-temperature rise or convection principle for direct calorimetry was also resurrected for the study of man (Carlson et al. 1964; Reardon et al. 2006; Snellen et al. 1983; Visser and Hodgson 1960a), of which the Snellen calorimeter located at the Human and Environmental Physiology Research Unit of the University of Ottawa is the last known operational human calorimeter in existance (Reardon et al. 2006).
The air calorimeter located at the University of Ottawa was originally developed by Jan Snellen during the 1970s at the Memorial University of Newfoundland (Snellen et al. 1983) (Fig. 6). A world-recognized authority in the area of human thermo-dynamics, Snellen developed one of the very few specialized whole-body calorimeters in the world at that time. This was based on a calorimeter employed by Snellen in studies conducted during his tenure in South Africa (1967–1970) (Snellen and Mitchell 1972; Snellen et al. 1970, 1972), which was designed by Visser and Hodgson in the late 1950s (Visser and Hodgson 1960b). Prior to his work in South Africa, Snellen had also completed thermoregulatory studies using a direct calorimeter at the University of Nijmegen in the Netherlands (Snellen 1966, 1969). While at Memorial University in Canada, he performed a limited number of studies for clinical application (Chang et al. 1984; Fernandez et al. 1986) as well as for the investigation of human thermoregulation (Snellen 2000). It remained operational until his retirement in 1990, after which it was decommissioned. It was acquired by Glen P. Kenny in 1998 and re-engineered and upgraded (Reardon et al. 2006). Like the gradient-layer calorimeter developed by Benzinger et al. (1958), it has a very fast response time. The main advantages of the Snellen air flow calorimeter are the fast response time, particularly for evaporative heat loss measurements, low thermal inertia, and the level of precision, particularly at high metabolic rates. The re-engineered Snellen calorimeter yields an unparalleled accuracy in the measure of total heat loss of 2.3 W. With the simultaneous measurement of energy expenditure via indirect calorimetry, the Snellen calorimeter has been used to quantify the change in body heat content. When combined with the measurement of body temperature (core, skin and muscle), studies conducted with the Snellen calorimeter have provided valuable insights into the regulation of body temperature under a wide array of conditions. Since the commissioning of the new Snellen air calorimeter, over 100 studies examining human thermoregulation have been conducted. The reader is directed to a series of recent topical reviews, wherein these studies are discussed (Kenny and Jay 2013; Kenny and Journeay 2010; Kenny and McGinn 2016; Kenny et al. 2016). Nonetheless, while gradient layer and air flow calorimeters are both excellent for studying thermal regulation over periods of a few hours, they are expensive to maintain and operate and the small size of the chambers restricts the activities that can be performed.
Using direct calorimetry to measure body heat storage
With the simultaneous measurement of energy expenditure via indirect calorimetry, direct calorimetry can be used to measure changes in body heat content. However, due to the limited accessibility of direct calorimeters, changes in body heat content are most often estimated using a weighted average of core and skin temperatures. This is done using a thermometric approach, with the following equation:
where ∆T b is the change in the volume-weighted mean temperature of the tissues of the body (in °C); b m is body mass (in kg); and C p is the average specific heat of the tissues of the body (in kJ kg−1 °C−1).
As discussed earlier, extensive research has been conducted to determine the optimal core and shell weighting coefficients for this linear two-compartment model which dates back to the work of Burton in the 1930s (Burton 1935). However, several studies (Colin et al. 1971a; Hardy and Stolwijk 1966; Horstman and Horvath 1972; Jay et al. 2007a, b; Snellen 1972, 2000; Vallerand et al. 1992) have since suggested that this approach substantially underestimates how much heat is stored in the body. In a recent editorial, Sawka and Castellani wrote “How much body heat is gained or lost during exercise and/or environmental exposure? This seems like a simple question that should be easily quantified; however, this is an unresolved issue that likely has produced flawed deductions concerning thermoregulatory control and treatment affects on body heat content” (Sawka and Castellani 2007). Ethan R. Nadel (1941–1998), a pioneer and authority in the field of thermoregulation, recognized that a potential source of error in thermometry likely relates to the fact that the two-compartment model does not consider changes in muscle temperature (Nadel et al. 1972). Indeed, muscle has a large heat storage capacity for a given temperature rise and muscle temperature varies considerably between different muscle groups (Aikas et al. 1962; Aulick et al. 1981; Jay et al. 2007a; Kenny and Jay 2013; Kenny et al. 2008, 2009; Saltin et al. 1968, 1970). Nadel et al. (1972) went on to develop a three-compartment model for the calculation of absolute mean body temperature during exercise in the heat by estimating the mass of working muscles. The model was based on data previously collected from Stolwijk and Hardy (1966b). The resulting formula for estimating absolute mean body temperature was as follows:
where T es is esophageal temperature, T m is quadriceps temperature, and T sk is mean skin temperature.
Using the portable suit calorimeter, Webb (1998) introduced a similar equation, where he also reduced the contribution of skin temperature and added the contribution of the muscle compartment to the estimation of mean body temperature during level and uphill walking. The equation was as follows:
where T re is rectal temperature, T m is change in mean muscle temperature, and T sk is mean skin temperature.
Later work by Jay et al., using the Snellen calorimeter and the simultaneous measurements of active (quadriceps) and inactive (triceps brachii and upper trapezius) muscle temperatures showed that the two-compartment thermometry model underestimates body heat storage by 15–35% during exercise in temperate and warm conditions (Jay et al. 2007a). Their work revealed that a three-compartment model, which includes the thermal influences of “muscle” in addition to core and skin temperatures, consistently yielded a more precise estimate of body heat storage, albeit it only explained ~50% of the overall variability in the change in body heat content (Jay et al. 2007a). The use of an adjusted core/skin model incorporating a correction factor was found to remove the statistical bias of the traditional model during exercise (Jay et al. 2007b). The best solution was not simply the addition of a correction factor to the optimally fitting traditional model, but also an adjustment of the relative weightings of the “core” and “shell” compartments when employing a correction factor. In more recent work using the Snellen calorimeter, it was demonstrated that the traditional two-compartment model for estimating mean body temperature (using conventional core/shell weightings) can be significantly improved when accounting for individual characteristics (i.e., body surface area) and simple environmental parameters (i.e., Oxford Index) (Jay et al. 2010). However, this two-compartment model was only assessed for light-to-moderate exercise intensities performed under temperate and warm ambient conditions. To date, the traditional thermometric model for estimating changes in body storage continues to be used in large part due to the fact that no practical alternative currently exists. However, a growing number of recent direct calorimetry studies examining the heat stress response in various populations (i.e., young and older adults, workers, individuals with chronic disease, etc.) during rest and exercise under a wide range of ambient conditions demonstrate that the change in body heat storage as estimated by the two-compartment thermometry model is greatly underestimated [the reader is referred to a recent review for a comprehensive discussion on this topic (Kenny and Jay 2013)]. This work underlines the need to develop models that can provide an improved estimation of how much heat is stored in the body using standard temperature measurements which can only be achieved using direct calorimetry.
Considerations for the accuracy of direct calorimetry
As the previous sections highlight, direct calorimeters built for use on humans came in all shapes and forms. Regardless of the different designs and specifications, the ultimate and common goal of all these calorimeters was to measure whole-body heat loss from human participants. As such, there are fundamental considerations that are common to direct calorimeters and understanding them allows one to gain a better appreciation of the factors that must be considered to achieve precision and minimize measurement error. In this section, we briefly describe some of these considerations by using some of the described human calorimeters as examples.
Ensuring zero-gradient for heat exchange
To measure heat loss from the body, all direct calorimeters employed either air or water as a medium to “carry away” the heat lost from the body. This principle is based upon the specific heat capacity of the medium, that is the amount of heat required for a 1 °C change in temperature. By measuring the temperature change of the medium and knowing its specific heat capacity, heat exchange can subsequently be calculated. For this concept to be valid, it must be ensured that changes in temperature of the medium are solely due to the heat lost from the participant within the calorimeter. If heat were exchanged with the environment surrounding the calorimeter, heat would “escape” measurement and lead to an underestimation of heat loss. To ensure that no heat exchange occurs between the calorimeter and the surrounding environment, a number of approaches have been used. In the late 1800s, the Atwater–Rosa calorimeter was designed with an inner chamber that was separated from the surrounding environment by four layers of air space, each approximately 5–7 cm wide, that provided inner and outer layers of dead space and circulating currents (Atwater and Rosa 1899a). The objective was to keep air temperature of these spaces equal to air temperature of the inner chamber, thus creating a zero-gradient for heat exchange. To do so, an observer would manually heat or cool the circulating currents by controlling the flow of hot or cold water through a system of pipes. The decision to cool or warm was based on the output of a galvanometer connected to 304 pairs of thermoelectric elements placed throughout the inner walls to detect temperature differences across the insulating layers. Fast-forward to the 21st century, the re-engineered Snellen calorimeter consists of an insulated cylinder surrounded by an outer “box” that is slightly pressurized. Conditioned air is supplied to the outer box and circulated through the inner chamber of the calorimeter, where the participant is located, as well as through a surrounding annular space. This ensures that no thermal gradient occurs between the inner chamber and the surrounding environment. Importantly, conditioning of the air is fully automated and finely controlled using proportional integral derivative feedback control loops (Reardon et al. 2006). In addition, worth mentioning is the approach employed by Webb to insulate the suit calorimeter from the environment. To ensure that temperature changes of the water circulating through the water-cooled suit were only due to heat loss from the participant, an insulating garment was placed on top of the suit. The participant would wear, on top of the suit, a first layer consisting of an insulated jacket and pants such as those designed for cold weather. A second layer consisted of an arctic parka and pants, as well as heavy woolen socks, down-filled boots, a knitted woolen cap, woolen gloves, and down-filled mittens (Webb 1985). Despite these insulating layers, heat exchange with the surrounding environment was unavoidable. To correct for “heat leakage”, temperature was measured at six locations within the inner surface of the suit. The difference in temperature between the inner surface of the suit and the environment was subsequently used to estimate heat that was lost to the environment and taken into account for the calculation of heat loss from the participant.
Technology
The level of sophistication and precision of various calorimeters was necessarily a result of the available technology at the time. To ensure accurate measurements of heat loss, differences in temperature and humidity of the medium must be measured with the greatest level of precision. To determine dry heat exchange, the Atwater–Rosa calorimeter contained a series of pipes through which cold water was circulated. The outflow-inflow temperature difference was measured with mercury thermometers (Atwater and Rosa 1899a). For evaporative heat loss, air exiting the calorimeter was passed through a system of “freezers” which consisted of pipes through which liquid ammonia was circulated. As the moisture from the air exiting the calorimeter passed through these freezers, water would condense onto special copper cylinders that were subsequently weighed to determine the amount of moisture produced by evaporation (Atwater and Rosa 1899a). Using these same operating principles, Benedict built two smaller calorimeters, which formed the basic design of the larger, Sage calorimeter. While similar instrumentation was used to quantify evaporative heat loss in the Sage calorimeter, the mercury thermometers used in the Atwater–Rosa calorimeter were replaced with faster responding electrical resistance thermometers to more precisely determine dry heat exchange from outflow-inflow temperature differences of circulating water (Riche and Soderstrom 1915). In sharp contrast to these early systems, outflow-inflow differences in air temperature and humidity are measured using high precision thermistors and dew point mirrors, respectively, with the re-engineered Snellen calorimeter (Reardon et al. 2006). For the suit calorimeter, water was continuously circulated through a loop that included the suit, a water bath, and a pump. The temperature of the water entering the suit was manually controlled by an operator to ensure the participant was neither hot, cold, or sweating. Although automatic controllers of water temperature were developed, they were deemed more complex than required for most applications (Webb 1985). The main criterion for adjusting water temperature was thermal comfort of the participant. During exercise, a lack of sweating was crucial, as evaporation of sweat not accounted for in the measurement of heat loss would induce large errors. To calculate heat loss, the temperature of the water entering and exiting the suit was measured with thermistors.
Size and response time
Size is an important consideration for direct calorimeters, both for measurement precision and the activities that will be carried out by the participant. Naturally, larger-sized calorimeters were designed with subject comfort in mind to allow measurements over periods of 24 h or more, whereas smaller-sized calorimeters limited the activities that could be performed and were only comfortable for periods of a few hours. The main consequence of calorimeter size will be to ensure adequate flow of air or water to achieve the desired response time of the system. To allow for measurements to be performed over long periods of time, the inner chamber of the Atwater–Rosa was 2.15 m long, 1.92 m high, and 1.22 m wide (Atwater and Rosa 1899a). This allowed for furniture and a bed within the calorimeter, as well as an ergometer for exercise studies. To ensure that the room was equilibrated prior to performing measurements, participants would enter the inner chamber in the evening and measurements would not begin until the next morning. Furthermore, measurements were performed in 6 h periods. While several smaller calorimeters were later built to improve response time (Murlin and Burton 1935; Rubner 1894), measurement time for these systems remained slower than the rate of heat transfer from the subject. Consequently, many calorimeters, particularly in the pre-war era, required more than 1 h to respond to a change in the thermal status of the participant (McLean and Tobin 1987). To avoid underestimating whole-body heat loss during thermal transients, these systems were restricted to use in steady-state conditions.
The gradient-layer system developed by Benzinger et al. (1958) introduced a significant improvement in the response time of direct calorimetry that permitted the rapid measurement of whole-body heat loss. Their system utilized a series of temperature sensors interwoven in a thin plexiglass sheet within the calorimeter walls to rapidly measure radiative and convective heat losses, while a series of heat exchanges lined with similar gradient layers (platemeters) rapidly measured evaporative heat loss. However, the small size of this calorimeter (2.13 m × 0.81 m × 0.81 m) restricted its use to resting exposures (Webb 1985). Unlike these systems, the re-engineered Snellen calorimeter was specifically designed to measure rapid transients in heat loss from an exercising participant. To achieve a rapid response time, the inner cylinder of the calorimeter is relatively smaller with a height of 1.83 m and a diameter of 1.68 m. It encloses a volume of 4000 L that can be circulated at a rate of ~6–15 kg of air per min. Continuous measurements of temperature and humidity of the air entering and leaving the calorimeter are automatically collected every 8 s. A room-sized (8 m3), convection calorimeter was also developed to perform rapid, long-term measurements of heat exchange during daily living activities (Tschegg et al. 1979, 1981). However, the larger size of this calorimeter increased the response time to 15 min to obtain 90% of the heat loss response from the subject over a broad range of air temperatures (15–40 °C). For the Webb suit calorimeter, flow rate of the water circulating through the suit was set at a fixed level of ~1.5 kg/min and water temperature was kept within a range of 25–32 °C for studies of resting metabolism and within a range of 10–25 °C during exercise (Webb 1985).
Summary
Direct calorimetry has been used over the past two centuries to establish fundamental concepts which have shaped our understanding of human metabolism and human heat exchange with the environment. These concepts have been applied to a number of fields, including the study of nutrition, disease, thermometry, and temperature regulation. Seminal work employing direct calorimetry also established the relationship between the heat produced during metabolic processes and the indirect derivation of metabolic rate from measures of oxygen consumption. Direct calorimetry saw its heyday during the 1900s, with calorimeters built in many shapes and forms, from large rooms to portable suit designs. However, direct calorimeters never gained widespread use due to the technical challenges and high costs of their operation and maintenance, so much so that only one known operational direct calorimeter is still in use today. Nonetheless, the ongoing use of direct calorimetry continues to be of great importance for understanding whole-body heat exchange in healthy and diseased populations.
References
Aikas E, Karvonen MJ, Piironen P, Ruosteenoja R (1962) Intramuscular, rectal and oesophageal temperature during exercise. Acta Physiol Scand 54:366–370
Armsby HP (1913) A comparison of the observed and computed heat production of cattle. J Am Chem Soc 35(11):1794–1800
Armsby HP, Fries JA (1913) The influence of standing or lying upon the metabolism of cattle. Am J Physiol 31(4):245–253
Armsby HP, Fries JA (1919) Net energy values and starch values. J Agric Sci 9(2):182–187
Atwater WO (1905) A respiration calorimeter with appliances for the direct determination of oxygen, vol 42. Carnegie Institute of Washington, Washington, DC
Atwater WO, Rosa EB (1899a) Description of a new respiration calorimeter and experiments on the conservation of energy in the human body. Government Printing Office, Washington
Atwater WO, Rosa EB (1899b) A new respiration calorimeter and experiments on the conservation of energy in the human body, II. Phys Rev (Series 1) 9:214–251
Atwater WO, Rosa EB (1899c) A new respiration calorimeter and experiments on the conservation of energy in the human body. I. Phys Rev (Series I) 9:129–163
Aub JC (1962) Biographical memoir: Eugene Floyd DuBois. In: National academy of sciences, vol 36, pp 125–145
Auguet A, Lefèvre J (1929) Nouvelle chamber calorimetrique du laboratoire de bioenergetique. Comptes Renders des Seances de la Societe de Biologie et de ses Filiales 100:251–253
Aulick LH, Robinson S, Tzankoff SP (1981) Arm and leg intravascular temperatures of men during submaximal exercise. J Appl Physiol 51(5):1092–1097
Benedict FG (1919) Energy requirements of children from birth to puberty. Boston Med Surg J 181(5):107–139
Benedict FG, Lee RC (1937) Lipogenesis in the animal body, with special reference to the physiology of the goose. Carnegie Institute of Washington, pp 232
Benedict FG, Roth P (1915) The metabolism of vegetarians as compared with the metabolism of non-vegetarians of like weight and height. J Biol Chem 20(3):231–241
Benedict FG, Roth P (1918) Effects of a prolonged reduction in diet on 25 men I. Influence on basal metabolism and nitrogen excretion. Proc Natl Acad Sci USA 4(6):149–152
Benedict FG, Smith HM (1915) The metabolism of athletes as compared with normal individuals of similar height and weight. J Biol Chem 20(3):243–252
Benedict FG, Talbot FB (1915) The physiology of the new-born infant. Proc Natl Acad Sci USA 1(12):600–602
Benedict FG, Emmes LE, Roth P, Smith HM (1914) The basal, gaseous metabolism of normal men and women. J Biol Chem 18(2):139–155
Benzinger TH (1959) On physical heat regulation and the sense of temperature in man. Proc Natl Acad Sci USA 45:645–659
Benzinger TH (1961) The diminution of thermoregulatory sweating during cold-reception at the skin. Proc Natl Acad Sci USA 47:1683–1688
Benzinger TH (1963a) Gradient layer calorimetry and human calorimetry. In: Dahl AI, Herzfeld CM (eds) Temperature—its measurement and control in science and industry, vol 3. Reinhold, New York
Benzinger TH (1963b) Peripheral cold- and central warm-reception, main origins of human thermal discomfort. Proc Natl Acad Sci USA 49:832–839
Benzinger TH, Kitzinger C (1949a) Direct calorimetry by means of the gradient principle. Rev Sci Instr 20:849
Benzinger TH, Kitzinger C (1949b) Gradient layer calorimetry and human calorimetry. In: Hardy JD (ed) Temperature—its measurement and control in science and industry, vol 3. Reinhold, New York, pp 158–165
Benzinger TH, Huebscher RG, Minard D, Kitzinger C (1958) Human calorimetry by means of the gradient principle. J Appl Physiol (1985) 12(2):S1–S24
Benzinger TH, Pratt AW, Kitzinger C (1961) The thermostatic control of human metabolic heat production. Proc Natl Acad Sci USA 47(5):730–739
Brun T, Webb P, de Benoist B, Blackwell F (1985) Calorimetric evaluation of the diary-respirometer technique for the field measurement of the 24-hour energy expenditure. Hum Nutr Clin Nutr 39(5):321–334
Burton AC (1935) Human calorimetry: the average temperature of the tissues of the body. J Nutr 9:261–280
Burton AC, Bazett HC (1936) A study of the average temperature of the tissues, of the exchanges of heat and vasomotor responses in man by means of a bath calorimeter. Am J Physiol 117:36–54
Capstick G (1921) A calorimeter for use with large animals. J Agric Science (Cambridge) 11:408–431
Carlson LD, Honda N, Sasaki T, Judy WV (1964) A human calorimeter. Proc Soc Exp Biol Med 117:327–331
Cathcart EP (ed) (1921) The physiology of protein metabolism. Longmans, Green, London
Chang KS, Farrell RT, Snellen JW, King FG (1984) Calorimetrical comparison of insulative properties of metalized plastic, clear polyethylene, and polyester blanket. Can Anaesth Soc J 31(6):690–694
Chappuis P, Pittet P, Jequier E (1976) Heat storage regulation in exercise during thermal transients. J Appl Physiol (1985) 40(3):384–392
Close WH, Dauncey MJ, Ingram DL (1980) Heat loss from humans measured with a direct calorimeter and heat-flow meters. Br J Nutr 43(1):87–93
Coleman W, Gephart AB (1915) Sixth paper notes on the absorption of fat and protein in typhoid fever. Arch Intern Med XV:882–886
Colin J, Timbal J, Boutelier C (1971a) Experimental determination of the equation permitting the calculation of the mean body temperature in neutral and hot environment. J Physiol (Paris) 63(3):229–231
Colin J, Timbal J, Houdas Y, Boutelier C, Guieu JD (1971b) Computation of mean body temperature from rectal and skin temperatures. J Appl Physiol 31(3):484–489
Crawford A (1788) Experiments and observations on animal heat and inflammation of combustible bodies. Johnson, London
Dauncey MJ (1980) Metabolic effects of altering the 24 h energy intake in man, using direct and indirect calorimetry. Br J Nutr 43(2):257–269
Dauncey MJ, Bingham SA (1983) Dependence of 24 h energy expenditure in man on the composition of the nutrient intake. Br J Nutr 50(1):1–13
Dauncey MJ, Murgatroyd PR, Cole TJ (1978) A human calorimeter for the direct and indirect measurement of 24 h energy expenditure. Br J Nutr 39(3):557–566
Day R, Hardy JD (1942) Respiratory metabolism in infancy and in childhood. XXIV. A calorimeter for measuring the heat loss of premature infants. Am J Dis Children 63:1086–1095
Deighton T (1926) A new calorimeter for use with young farm animals. J Agric Sci (Cambridge) 16:376–382
Deighton T (1939) A study of the metabolism of fowls. I. A calorimeter for teh directed determination of the metabolism of fowls. J Agric Sci (Cambridge) 29:431–451
DuBois EF (1912) The absorption of food in typhoid fever. Arch Intern Med 10:177
Dubois EF (1916) Studies of the basal metabolism in disease and their importance in clinical medicine. Boston Med Surg J 174:864
DuBois EF (1919) The basal metabolism as a guide in the diagnosis and treatment of thyroid disease. Med Clin N Am 2:1201
DuBois E (1937) The mechanism of heat loss and temperature regulation. Stanford University Press, Stanford
DuBois EF (1950) 50 years of physiology in America; a letter to the editor. Annu Rev Physiol 12:1–6. doi:10.1146/annurev.ph.12.030150.000245
DuBois EF, Coleman W (1915) Clinical calorimetry VII. Calorimetric observations on the metabolism of typhoid patients with and without food. Arch Intern Med 15:887
DuBois D, Dubois EF (1915) Fifth paper: the measurement of the surface area of man. Arch Intern Med XV:868–881
DuBois E, Riddle O (1958) Francis gano benedict, 1870–1957—a biographical memoir. Biographical Memoirs. National Academy of Sciences, pp 65–99
Dubois EF, Veeder BS (1910) The total energy requirements in diabetes mellitus. Arch Intern Med 5:37
Durnin JV, Edholm OG, Miller DS, Waterlow JC (1973) How much food does man require? Nature 242(5397):418
Editorial (1915) Editorial: clinical calorimetry in the United States. JAMA LXIV 25:2069–2070
Editorial (1965) Editorial: Max Rubner—1854–1932. Energy physiologist. JAMA 194(1):86–87
Fernandez PG, Snedden W, Snellen JW, Galway AB, Nath C (1986) Increased metabolic heat production following chronic alpha-methyldopa therapy in hypertensives. Can J Physiol Pharm 64(2):138–144
Gagnon D, Kenny GP (2011) Exercise-rest cycles do not alter local and whole body heat loss responses. Am J Physiol Regul Integr Comp Physiol 300(4):R958–R968
Gagnon D, Kenny GP (2012) Sex differences in thermoeffector responses during exercise at fixed requirements for heat loss. J Appl Physiol 113(5):746–757
Gagnon D, Jay O, Lemire B, Kenny GP (2008) Sex-related differences in evaporative heat loss: the importance of metabolic heat production. Eur J Appl Physiol 104(5):821–829
Ganio MS, Gagnon D, Stapleton J, Crandall CG, Kenny GP (2012) Effect of human skin grafts on whole-body heat loss during exercise heat stress: a case report. J Burn Care Res 34(4):e263–e270
Garrow JS (1973) Diet and obesity. Proc R Soc Med 66(7):642–644
Garrow JS (1974) Energy balance and obesity in man. North Holland Publishing Company, Amsterdam
Garrow JS, Murgatroyd P, Toft R, Warwick P (1977) A direct calorimeter for clinical use (proceedings). J Physiol 267(1):15P–16P
Gephart AB, Dubois EF (1915) Fourth paper: the determination of the basal metabolism of normal men and the effect of food. Arch Intern Med XV:835–867
Glushko AA, Gorodinskii SM, Orekhov BV (1976) Human calorimetry in sealed hermetic enclosures. Kosm Biol Aviakosm Med 10(4):64–69
Gorodinskii SM, Glushko AA, Orekhov BV (1976) Human calorimetry in protective garments. Mashinostroyeniye, Moscow
Hardy JD (1934) The radiation of heat from the human body. I. An instrument for measuring the radiation and surface temperature of skin. J Clin Investig 13:593–604
Hardy JD, Dubois EF (1938) Basal metabolism, radiation, convection and evaporation at temperature from 22 to 35 C. J Nutr 15:477–492
Hardy JD, Stolwijk JA (1966) Partitional calorimetric studies of man during exposures to thermal transients. J Appl Physiol (1985) 21(6):1799–1806
Hill AV, Hill AM (1914) A self-recording calorimeter for large animals. J Physiol (Lond) xiii:xiv
Holmes FL (1985) Lavoisier and the chemistry of life: an exploration of scientific creativity. University of Wisconsin Press, Madison
Horstman DH, Horvath SM (1972) Cardiovascular and temperature regulatory changes during progressive dehydration and euhydration. J Appl Physiol (1985) 33(4):446–450
Howland J (1912) Direct calorimetry of infants with a comparison of the results obtained by this and other methods. Trans 15th Int Congr Hyg Dermatol 2:438–451
Irsigler K, Veitl V, Sigmund A, Tschegg E, Kunz K (1979) Calorimetric results in man: energy output in normal and overweight subjects. Metabolism 28(11):1127–1132
Jacobsen S, Johansen O, Garby L (1982) 5.8 m3 human heat-sink calorimeter with online data acquisition, processing and control. Med Biol Eng Comput 20(1):29–36
Jacobsen S, Johansen O, Garby L (1985) A 24-m3 direct heat-sink calorimeter with on-line data acquisition, processing, and control. Am J Physiol 249(4 Pt 1):E416–E432
Jay O, Gariepy LM, Reardon FD, Webb P, Ducharme MB, Ramsay T, Kenny GP (2007a) A three-compartment thermometry model for the improved estimation of changes in body heat content. Am J Physiol Regul Integr Comp Physiol 292(1):R167–R175
Jay O, Reardon FD, Webb P, Ducharme MB, Ramsay T, Nettlefold L, Kenny GP (2007b) Estimating changes in mean body temperature for humans during exercise using core and skin temperatures is inaccurate even with a correction factor. J Appl Physiol 103(2):443–451
Jay O, DuCharme MB, Webb P, Reardon FD, Kenny GP (2010) Estimating changes in volume-weighted mean body temperature using thermometry with an individualized correction factor. Am J Physiol Regul Integr Comp Physiol 299(2):R387–R394
Jelenko C 3rd, Wheeler ML, Callaway BD (1979) Studies in burns, XVI: the effect of surgical trauma on metabolic heat production. Am Surg 45(5):314–318
Jequier E (1975) Direct calorimetry: a new clinical approach for measuring thermoregulatory responses in man. Bibl Radiol 6:185–190
Jequier E (1981) Long term measurement of energy expenditure in man: Direct or indirect calorimetry? In: Bjornstorp P, Cairella M, Howard AN (eds) Recent advances in obesity research III. J. Libbey, London, pp 130–135
Jequier E, Gygax PH, Pittet P, Vannotti A (1974) Increased thermal body insulation: relationship to the development of obesity. J Appl Physiol 1985 36(6):674–678
Kenny GP, Jay O (2013) Thermometry, calorimetry, and mean body temperature during heat stress. Compr Physiol 3:1–31
Kenny GP, Journeay WS (2010) Human thermoregulation: separating thermal and nonthermal effects on heat loss. Front Biosci 15:259–290
Kenny GP, McGinn R (2016) Restoration of thermoregulation after exercise. J Appl Physiol (1985) 122(4):933–944
Kenny GP, Webb P, Ducharme MB, Reardon FD, Jay O (2008) Calorimetric measurement of postexercise net heat Loss and residual body heat storage. Med Sci Sports Exerc 40(9):1629–1636
Kenny GP, Dorman LE, Webb P, Ducharme MB, Gagnon D, Reardon FD, Hardcastle SG, Jay O (2009) Heat balance and cumulative heat storage during intermittent bouts of exercise. Med Sci Sports Exerc 41(3):588–596
Kenny GP, Stapleton JM, Yardley JE, Boulay P, Sigal RJ (2013) Older adults with type 2 diabetes store more heat during exercise. Med Sci Sports Exerc 45(10):1906–1914
Kenny GP, Flouris AD, Dervis S, Friesen BJ, Sigal RJ (2015) Older adults experience greater levels of thermal and cardiovascular strain during extreme heat exposures. Med Sci Sports Exerc 46(5):S396
Kenny GP, Sigal RJ, McGinn R (2016) Body temperature regulation in diabetes. Temperature (Austin) 3(1):119–145
Kleiber M (1935) The California apparatus for respiration trials with large animals. Hilgardia 9:1–70
Kleiber M (1961) The fire of life—an introduction to animal energetics. Wiley, New York
Larose J, Boulay P, Sigal RJ, Wright HE, Kenny GP (2013a) Age-related decrements in heat dissipation during physical activity occur as early as the age of 40. PLoS One 8(12):e83148
Larose J, Wright HE, Sigal RJ, Boulay P, Hardcastle S, Kenny GP (2013b) Do older females store more heat than younger females during exercise in the heat? Med Sci Sports Exerc 45(12):2265–2276
Larose J, Wright HE, Stapleton J, Sigal RJ, Boulay P, Hardcastle S, Kenny GP (2013c) Whole-body heat loss is reduced in older males during short bouts of intermittent exercise. Am J Physiol 305(6):R619–R629
Larose J, Boulay P, Wright-Beatty HE, Sigal RJ, Hardcastle S, Kenny GP (2014) Age-related differences in heat loss capacity occur under both dry and humid heat stress conditions. J Appl Physiol (1985) 117(1):69–79
Lavoisier AL, Laplace PS (1780) Histoire de l’Académie des Sciences. Année, p 355
Lefèvre J (1911) Chaleur animal et bioenergetique. Masson et Cie, Paris
Lodwig TH (1974) The ice calorimeter of Lavoisier and Laplace and some of its critics. Ann Sci 31:1–18
Lusk G (1906) The elements of the science of nutrition. Saunders, Philadelphia
Lusk G (1915a) First paper: a respiration calorimeter for the study of disease. Arch Intern Med XV:793–804
Lusk G (1915b) Eigth paper on the diabetic respiratory quotient. Arch Intern Med XV:939–944
Lusk G (1932) A tribute to the life and work of Max Rubner. Science 76(1963):129–135. doi:10.1126/science.76.1963.129
McLean JA, Tobin G (1987) Animal and human calorimetry. Cambridge University Press, Cambridge
McManus C, Newhouse H, Seitz S, Nixon D, Poppendiek H, Heymsfield S (1984) Human gradient-layer calorimeter: development of an accurate and practical instrument for clinical studies. JPEN J Parenter Enter Nutr 8(3):317–320
Meade RD, Poirier MP, Flouris AD, Hardcastle SG, Kenny GP (2016) Do the threshold limit values for work in hot conditions adequately protect workers? Med Sci Sports Exerc 48(6):1187–1196
Meis SJ, Dove EL, Bell EF, Thompson CM, Glatzl-Hawlik MA, Gants AL, Kim WK (1994) A gradient-layer calorimeter for measurement of energy expenditure of infants. Am J Physiol 266(3 Pt 2):R1052–R1060
Mitchell HH, Hamilton TS (1932) The effect of the amount of feed consumed by cattle on the utilisation of its energy content. J Agric Res 45:163–191
Mitchell D, Wyndham CH, Vermeulen AJ, Hodgson T, Atkins AR, Hofmeyr HS (1969) Radiant and convective heat transfer of nude men in dry air. J Appl Physiol (1985) 26(1):111–118
Mollgard H, Anderson AC (1917) Respiration apparatus: its significance and use in experiments with dairy cattle. Beretning fra Forsogslaboratoriet Kobenhaven 94:1–180
Mount LE (1967) The heat loss from new-born pigs to the floor. Res Vet Sci 8(2):175–186
Murlin JR, Burton AC (1935) Human calorimetry I. A semi-automatic respiration calorimeter. J Nutr 9:233–260
Nadel ER, Bergh U, Saltin B (1972) Body temperatures during negative work exercise. J Appl Physiol 33(5):553–558
Pahud P, Ravussin E, Jequier E (1980) Energy expended during oxygen deficit period of submaximal exercise in man. J Appl Physiol Respir Environ Exerc Physiol 48(5):770–775
Poirier MP, Gagnon D, Friesen BJ, Hardcastle SG, Kenny GP (2015) Whole-body heat exchange during heat acclimation and its decay. Med Sci Sports Exerc 47(2):390–400
Poncet E, Dahlberg L (2011) The legacy of Henri Victor Regnault in the arts and sciences. Int J Arts Sci 4(13):377–400
Poppendiek H, Hody GL (1972) Design considerations and applications of gradient layer calorimeters for use in biological heat production measurement. In: Plumb HH (ed) Temperature—its measurement and control in science and industry, vol 2079–2088. Int Soc Am, Pittsburgh
Ravussin E, Bogardus C (1982) Thermogenic response to insulin and glucose infusions in man: a model to evaluate the different components of the thermic effect of carbohydrate. Life Sci 31(18):2011–2018
Ravussin E, Burnand B, Schutz Y, Jequier E (1982) Twenty-four-hour energy expenditure and resting metabolic rate in obese, moderately obese, and control subjects. Am J Clin Nutr 35(3):566–573
Reardon FD, Leppik KE, Wegmann R, Webb P, Ducharme MB, Kenny GP (2006) The Snellen human calorimeter revisited, re-engineered and upgraded: design and performance characteristics. Med Biol Eng Comput 44(8):721–728
Regnault HV, Reiset J (1849) Recherches chimiques sur la respiration des animaux des diverses classes. Ann Chim Phys, série 3, tome 26, 299–519
Riche JA, Soderstrom GF (1915) The respiration calorimeter of the Russell Sage Institute of Pathology in Bellevue Hospital. Arch Intern Med 15:805–828
Ritzman EG, Benedict FG (1929) Simplified technique and apparatus for measuring energy requirements of cattle. N H Agric Exp Stn Bull 240, pp 30
Rubner M (1883) The effect of body size on food and energy metabolism. Z Biol 19:535–562
Rubner M (1894) Die quelle de thierschen warme. Zeitschrift fur biologie 30:73–142
Saltin B, Gagge AP, Stolwijk JA (1968) Muscle temperature during submaximal exercise in man. J Appl Physiol 25(6):679–688
Saltin B, Gagge AP, Stolwijk JA (1970) Body temperatures and sweating during thermal transients caused by exercise. J Appl Physiol 28(3):318–327
Sawka MN, Castellani JW (2007) How hot is the human body? J Appl Physiol 103(2):419–420
Seale JL (1995) Energy expenditure measurements in relation to energy requirements. Am J Clin Nutr 62(5 Suppl):1042S–1046S
Seale JL, Rumpler WV (1997) Synchronous direct gradient layer and indirect room calorimetry. J Appl Physiol (1985) 83(5):1775–1781
Seale JL, Rumpler WV, Moe PW (1991) Description of a direct-indirect room-sized calorimeter. Am J Physiol 260(2 Pt 1):E306–E320
Snellen JW (1966) Mean body temperature and the control of thermal sweating. Acta Physiol Pharmacol Neerl 14(2):99–174
Snellen JW (1969) The discrepancy between thermometry and calorimetry during exercise. Pflug Arch 310(1):35–44
Snellen JW (1972) Set point and exercise. In: Bligh J, Moore RE (eds) Essays on temperature regulation. North Holland, Amsterdam, pp 139–148
Snellen JW (2000) An improved estimation of mean body temperature using combined direct calorimetry and thermometry. Eur J Appl Physiol 82(3):188–196
Snellen JW, Mitchell D (1972) Calorimetric analysis of the effect of drinking saline solution on whole-body sweating. II. Response to different volumes, salinities and temperatures. Pflug Arch 331(2):134–144
Snellen JW, Mitchell D, Wyndham CH (1970) Heat of evaporation of sweat. J Appl Physiol (1985) 29(1):40–44
Snellen JW, Mitchell D, Busansky M (1972) Calorimetric analysis of the effect of drinking saline solution on whole-body sweating. I. An attempt to measure average body temperature. Pflug Arch 331(2):124–133
Snellen JW, Chang KS, Smith W (1983) Technical description and performance characteristics of a human whole-body calorimeter. Med Biol Eng Comput 21(1):9–20
Spinnler G, Jequier E, Favre R, Dolivo M, Vannotti A (1973a) Human calorimeter with a new type of gradient layer. J Appl Physiol (1985) 35(1):158–165
Spinnler G, Jequier E, Favre R, Dolivo M, Vannotti A (1973b) Human calorimeter with a new type of gradient layer. J Appl Physiol 35(1):158–165
Stapleton J, Gagnon D, Kenny GP (2010) Short-term exercise training does not improve whole-body heat loss when rate of metabolic heat production is considered. Eur J Appl Physiol 109(3):437–446
Stapleton JM, Yardley JE, Boulay P, Sigal RJ, Kenny GP (2013) Whole-body heat loss during exercise in the heat is not impaired in type 1 diabetes. Med Sci Sports Exerc 45(9):1656–1664
Stapleton JM, Poirier MP, Flouris AD, Boulay P, Sigal RJ, Malcolm J, Kenny GP (2015a) Aging impairs heat loss, but when does it matter? J Appl Physiol (1985) 118(3):299–309
Stapleton JM, Poirier MP, Flouris AD, Boulay P, Sigal RJ, Malcolm J, Kenny GP (2015b) At what level of heat load are age-related impairments in the ability to dissipate heat evident in females? PLoS One 10(3):e0119079
Stolwijk JA, Hardy JD (1966a) Partitional calorimetric studies of responses of man to thermal transients. J Appl Physiol (1985) 21(3):967–977
Stolwijk JA, Hardy JD (1966b) Temperature regulation in man—a theoretical study. Pflug Arch Gesamte Physiol Menschen Tiere 291(2):129–162
Swift RW, Barron GP, Fisher KH, French CE, Hartsook EW, Hershberger TV, Keck E, Long TA, Magruder ND (1958) The effect of high versus low protein equicaloric diets on the heat production of human subjects. J Nutr 65(1):89–102
Tiemann J (1969) A respiration calorimeter for the determination of combustion transformation degree in the human organism. Elektromed Biomed Tech 14(4):135–145
Tschegg E, Sigmund A, Veitl V, Schmid P, Irsigler K (1979) An isothermic, gradient-free, whole-body calorimeter for long-term investigations of energy balance in man. Metabolism 28(7):764–770
Tschegg E, Sigmund A, Veitl V, Irsigler K (1981) A whole-body calorimeter for long-term measurements in man. J Phys E 14(5):550–554
Vallerand AL, Savourey G, Hanniquet AM, Bittel JH (1992) How should body heat storage be determined in humans: by thermometry or calorimetry? Eur J Appl Physiol Occup Physiol 65(3):286–294
Veitl V, Irsigler K (1983) The clinical use of direct calorimetry for measuring energy expenditure. Infusionsther Klin Ernahr 10(5):255–258
Visser J, Hodgson T (1960a) The design of a human calorimeter for the determination of body heat storage. S Afr J Mech Eng 9:243–260
Visser J, Hodgson T (1960b) The design of a human calorimeter for the determination of body heat storage. S Afr Mech Eng 9:243–260
Voit C (1866) Zeitschrift fur biologie II:307
Webb P (1985) Human calorimeters. Praeger, New York
Webb P (1998) Heat storage during exercise, especially in muscle. In: Hodgdon JA (ed) 8th International conference on environmental ergonomics, San Diego, CA, USA, pp 121–124
Webb P, Troutman SJ Jr, Annis JF (1970) Automatic cooling in water cooled space suits. Aerosp Med 41(3):269–277
Webb P, Annis JF, Troutman SJ Jr (1972) Human calorimetry with a water-cooled garment. J Appl Physiol 32(3):412–418
Webb P (1981) Energy expenditure and fat-free mass in men and women. Am J Clin Nutr 34(9):1816–1826
Webb P (1986) Direct calorimetry and the energetics of exercise and weight loss. Med Sci Sports Exerc 18(1):3–5
Webb P, Saris WH, Schoffelen PF, Van Ingen Schenau GJ, Ten Hoor F (1988) The work of walking: a calorimetric study. Med Sci Sports Exerc 20(4):331–337
Webb P, Nagle FJ, Wanta DM (1991) Heat regulation during exercise with controlled cooling. Eur J Appl Physiol Occup Physiol 62(3):193–197
Webster JD, Welsh G, Pacy P, Garrow JS (1986) Description of a human direct calorimeter, with a note on the energy cost of clerical work. Br J Nutr 55(1):1–6
Whipp BJ, Wasserman K (1969) Efficiency of muscular work. J Appl Physiol 26(5):644–648
Williams HB (1912) Animal calorimetry first paper. a small respiration calorimeter. J Biol Chem 12(3):317–347
Winslow CEA, Herrington LP, Gagge AP (1936a) The determination of radiation and convection exchanges by partitional calorimetry. Am J Physiol 116:669–684
Winslow CEA, Herrington LP, Gagge AP (1936b) A new method of partitional calorimetry. Am J Physiol 116:641–655
Winslow CEA, Herrington LP, Gagge AP (1937) Physiological reactions of the human body to varying environmental temperatures. Am J Physiol 120(1):1–21
Young AC, Burns HL, Quinton WF, Carlson LD (1951) Temperature gradient calorimetry. Wright-Pattern AFB, Ohio
Young AC, Carlson LD, Burns HL (1955) Regional heat loss by temperature gradient calorimetry. Arctic Aeromedical Laboratory, Ladd Air Force Base, Alaska
Acknowledgements
Support for this work is provided in part by the Natural Sciences and Engineering Research Council of Canada (funds held by Dr. Glen P. Kenny). G. P. Kenny is supported by a University of Ottawa Research Chair Award. This work is presented in memory of Dr. Paul Webb (MD). Dr. Webb was born in Willoughby, Ohio, on Dec. 2, 1923. He received his M.D. from the University of Virginia in 1943 and an M.S. in physiology from the University of Washington in 1949. He served in the U.S. Army from 1948 to 1950, taught physiology at University of Oklahoma medical school from 1952 to 1954, and worked at the Air Force Biomedical Laboratory at Wright-Patterson Air Force Base from 1954 to 1958. In 1959, he founded Webb Associates, a research company, in Yellow Springs. Webb Associates performed several major research studies for the U.S. Department of Agriculture, the Office of Naval Research and the Air Force. Dr. Webb closed his Yellow Springs laboratory in 1982 and moved to France. There, he performed experiments at Hospital Bichat in Paris. From 1984 to 1988, he worked in various technical companies and universities in Norway, The Netherlands and Sweden. During his career, Dr. Webb received a great many awards for his work; two of these awards are the Fritz J. Russ Award in bioengineering and the Jeffries Aerospace Medicine and Life Sciences Research Award from the American Institute of Aeronautics and Astronautics, notification of which he received a short time before his death on May 18, at the age of 90 (Online edition of the Yellow Springs News, May 29, 2014).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Communicated by Michael Lindinger.
Rights and permissions
About this article
Cite this article
Kenny, G.P., Notley, S.R. & Gagnon, D. Direct calorimetry: a brief historical review of its use in the study of human metabolism and thermoregulation. Eur J Appl Physiol 117, 1765–1785 (2017). https://doi.org/10.1007/s00421-017-3670-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-017-3670-5