Abstract
Purpose
Although left atrial (LA) enlargement is a recognized component of athlete’s heart, dynamic cavity changes occurring during the training period remain to be elucidated. We aimed to investigate the adaptive changes of LA reservoir, conduit, and active volumes in elite athletes vs. controls and their response to different training loads.
Methods
LA maximum, pre-P, and minimum volumes were assessed in 26 top-level athletes and 23 controls. In athletes, LA volumes were measured at pre-, mid-, end-training, and post-detraining time points using conventional 2D echocardiography.
Results
Athletes had larger maximum (27.5 ± 3.2 vs. 20.3 ± 5.8 mL/m2, p = 0.001), pre-P (11.5 ± 0.9 vs. 9.8 ± 2.2 mL/m2, p = 0.001), and minimum (6.6 ± 0.9 vs. 5.0 ± 1.2 mL/m2, p < 0.001) LA indexed volumes, compared with controls. Total and passive emptying volume indices were also larger in athletes compared with controls (18.7 ± 3.1 vs. 15.3 ± 4.9 mL/m2, p < 0.05 and 13.8 ± 2.9 vs. 10.5 ± 4.6 mL/m2, p < 0.05, respectively), while active emptying volume was similar (p = 0.74). During training, LA maximum (p < 0.0001), pre-P (p < 0.0001), minimum (p < 0.0001), total (p < 0.005), and passive (p < 0.05) emptying volume indices progressively increased, while active emptying volume (p = 0.10) and E/e′ ratio (p = 0.32) remained unchanged. After detraining, LA volume measurements were not different from pre-training ones. End-training left ventricular mass index was the only independent predictor of the respective maximum LA volume (β = 0.74, p < 0.005).
Conclusions
Top-level athletes exhibit a dynamic morphological and functional LA remodeling, induced by training, with an increase in reservoir and conduit volumes, but stable active volume. LA remodeling is closely associated with left ventricular adaptation to exercise and both completely regress after detraining.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morphological left atrial (LA) remodeling in athletes has been recognized as a component of the physiological cardiac adaptation to sustained exercise conditioning (D’Andrea et al. 2010; D’Ascenzi et al. 2011; D’Ascenzi et al. 2013; D’Ascenzi et al. 2015; Pelliccia et al. 2005). In highly trained athletes, the extent of LA dilatation may be so important that absolute LA size overlaps with that seen in patients with cardiac disease (Pelliccia et al. 2005; D’Andrea et al. 2010). Moreover, in competitive soccer players, morphological changes of the LA tend to increase during training (D’Ascenzi et al. 2012), suggesting that the extent of LA adaptation varies in response to incremental exercise load. The clinical implications of the latter on LA morphological and function changes have recently raised awareness as to their potential relationship with cardiac arrhythmia commonly seen in athletes, particularly atrial fibrillation (Calvo et al. 2012; Mascia et al. 2013; Ofman et al. 2013; Inama et al. 2010). Most available studies evaluating the athlete’s heart, however, are cross sectional in design (Pluim et al. 2000; Utomi et al. 2013; Fagard 2003) and very little data exist on functional adaptive changes of the LA in highly trained athletes.
The LA contributes to left ventricular (LV) filling by three mechanisms (Braunwald and Frahm 1961; Spencer et al. 2001; Nikitin et al. 2003; Jarvinen et al. 1994): during ventricular systole when LA acts as a “reservoir” receiving blood from the pulmonary veins; during early diastole when LA operates as a “conduit” transferring blood from the pulmonary veins into the LV; and during late diastole when LA actively contracts to pump blood into the LV cavity (Nikitin et al. 2003; Jarvinen et al. 1994; Abhayaratna et al. 2006; Thomas et al. 2002; Prioli et al. 1998; Tükek et al. 2001; Eshoo et al. 2009, 2010). A clear understanding of such dynamic variations in athletes may help differentiating physiological exercise related to LA remodeling from pathological changes occurring in cardiac diseases.
The present study aims at three objectives which assess (1) the adaptive variation of LA function parameters, including maximum and minimum, and phasic volumes in top-level athletes compared to controls; (2) the nature and extent of changes in LA volumes during the training period, and (3) LA and LV remodeling induced by regular exercise training. These objectives are based on the hypothesis that LA function differs in athletes compared to controls and that a further adaptation can occur in response to training with a preserved or even improved atrial function.
Methods
Study population and training protocol
Twenty-nine male elite professional soccer players were recruited for the purpose of this study. All were engaged in similar training program, under the supervision of a dedicated coach, with minimal variability based on player’s ability and role. Goal-keepers were excluded from the study because they were engaged in a different training program. All athletes were evaluated at the same time point of the training program, at the same time of the day, and at least 48 h after the last strenuous training session. Three athletes were eventually excluded because they withdrew from the training program due to musculoskeletal injuries; thus, the final study population consisted of 26 athletes.
In the athletes, cardiac measurements were made at the beginning of the study, after 5 months, and again after 10 months of training, corresponding, respectively, to (a) the pre-competition training period, (b) the mid-training period, and (c) the end of competition. A final measurement was obtained after 2 months of detraining. All recruited athletes were engaged in the intensive and closely supervised training program according to the following protocol:
-
(a)
During the pre-competition training period, lasting 4 weeks, athletes exercised for at least 20 h/week divided in 10 sessions/week. Training sessions consisted of high volume/low intensity running (achieving 60–80 % of maximal predicted heart rate) and sprinting conditioning (3–4 sessions/week). They also performed 2–3 resistance-training weekly sessions at moderate–high workload. Each session lasted 45 min.
-
(b)
During the mid-training period, athletes exercised for at least 12 h/week, divided in 6 sessions/week, and they played one/two matches weekly. They exercised at workloads achieving 70–95 % of maximal predicted heart rate, as indicated by individual heart rate monitoring. Training sessions consisted of technical–tactical drills, low volume/high intensity running, and sprinting. Athletes also performed 1–2 resistance-training moderate workload sessions weekly, lasting 45 min.
-
(c)
During the last 3 months of training, volume and intensity of training were reduced. Athletes trained 8 h/week, divided in 5 sessions/week, with only 1 session of resistance training, lasting 45 min. In the last month, training sessions were 4–5/week, lasting 75–90 min. The training program included only technical and tactical drills without resistance conditioning.
-
(d)
Detraining was defined as the suspension of usual training regimen (Mujika and Padilla 2000). During this period, none of the athletes performed any exercise for more than 3 h per week.
For comparison, 23 untrained age- and gender-matched healthy controls were enrolled. They were either completely sedentary or engaged in less than 2 h of exercise per week, and none was engaged in sports competitions.
Before enrolment in the study, all participants underwent complete physical examination, ECG, echocardiography, and treadmill ECG-test with no evidence of pathological findings. None had evidence for coronary artery disease, valvular and congenital heart disease, cardiomyopathy, arterial hypertension, or diabetes mellitus. All subjects were asymptomatic and did not have family history for sudden cardiac death.
After the rationale and the study protocol were explained, all participants gave informed consent to take part in the study, the protocol of which complied according to the ethical standards of the 1964 Declaration of Helsinki and its later amendments and which was also approved by the Local Ethics Committee.
Echocardiographic analysis
Echocardiographic examination was performed by a single cardiologist using a high-quality echocardiograph (Vivid 7, GE, USA), equipped with a 2.5-MHz probe. For all measurements, three cycles were stored and analyzed off-line using a dedicated software (EchoPac, GE, USA). Off-line data analysis was performed by an experienced reader, blinded to the study time point. Resting heart rate was measured from the electrocardiographic tracing taken during the echocardiographic examination.
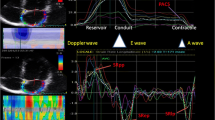
LA volumes
LA area and volume were calculated using the biplane method of disks (modified Simpson rule) in the apical 4- and 2-chamber views, and an average value was obtained and indexed to body surface area (BSA). Care was taken to exclude the pulmonary veins and LA appendage from the LA tracing. The plane of the mitral annulus was used as inferior border (Lang et al. 2006). For the aim of this study, LA volumes were measured at 3 time points: (1) maximum LA volume, at the end of LV systole, when LA chamber is at its greatest size; (2) pre-P-wave LA volume, just before the onset of the p wave on the superimposed ECG; and (3) minimum LA volume, at the end of LA systole, immediately after mitral valve closure (Eshoo et al.2010). The following LA phasic parameters were also derived (Eshoo et al. 2009, 2010; Thomas et al. 2002; Boyd et al. 2010):
-
(a)
LA total emptying volume = max vol–min vol and LA total emptying fraction = LA total reservoir vol/max vol. These two measurements were markers of LA reservoir function and are called hereafter LA reservoir volume and LA reservoir fraction, respectively.
-
(b)
LA passive emptying volume = max vol–pre-P vol and LA passive emptying fraction = LA passive emptying volume/max vol. LA passive emptying volume and fraction were considered as markers of LA passive conduit function and are called hereafter LA conduit volume and LA conduit fraction, respectively. “True” conduit volume was also estimated as LV stroke volume (SV) − (LA passive emptying volume + LA active emptying volume) (Abhayaratna et al. 2006, Leung et al. 2008).
-
(c)
LA active emptying volume = pre-P vol–min vol and LA active emptying fraction = LA active emptying volume/pre-P vol. These two measurements were taken as markers of LA active function.
In addition, LV end-diastolic and end-systolic wall thickness and volumes, LV mass (LVM), LV SV, and inferior vena cava diameter were obtained as recommended (Lang et al. 2006; Rudski et al. 2010) and were indexed to BSA (Du Bois and Du Bois 1916).
Standard and tissue Doppler imaging
LV spectral pulsed-wave Doppler was used in the apical 4-chamber view to obtain filling velocities, as recommended (Nagueh et al. 2009). Early diastolic (E-wave) velocity and late diastolic (A wave) velocity were obtained, and the E/A ratio was calculated.
Tissue Doppler imaging was performed by placing the sample volume at the level of septal and lateral insertion sites of the mitral leaflets from the apical four-chamber view (Nagueh et al. 2009; Yu et al. 2007), from which recordings of peak systolic (s′), early diastolic (e′), and late diastolic (a′) annular velocities were obtained. The average value of septal and lateral velocities was also calculated, as recommended (Nagueh et al. 2009). The e′ velocity and the derived e′/a′ ratio were used as markers of segmental ventricular relaxation (Kasner et al. 2007). The E/e′ ratio was calculated and used as an index of LV filling pressures (Ommen et al. 2000).
Statistical analysis
Normal distribution of all continuous variables was confirmed using the Shapiro–Wilk test, and data are presented as mean ± SD. Differences in baseline characteristics between athletes and controls were assessed using unpaired Student’s t test. Comparison of data collected at different time points was made using repeated-measures ANOVA with Bonferroni post hoc correction for multiple comparisons. Pre-training and detraining data were compared using the paired Student’s t test. A p value <0.05 was considered significant.
The relationship between two variables was assessed by Pearson’s correlation. The following variables were selected for potential impact on LA volumes: demographic data (age, BSA), LV end-diastolic volume (EDV), LVM, LV SV, and the difference between end-training and pre-training values of each variable. Multivariate stepwise linear regression analysis was used to examine independent predictors of LA total and phasic volumes. Statistics were performed using SPSS version 22.0 (Statistical Package for the Social Sciences, Chicago, Illinois).
Results
Comparison between athletes and controls
Athletes had similar age to controls (27.1 ± 3.7 vs. 26.7 ± 3.8 years, p = 0.70) but slightly higher BSA (2.0 ± 0.1 vs. 1.9 ± 0.1 m2, p < 0.05) and lower heart rate (61.3 ± 8.0 vs. 72.8 ± 9.3 bpm, p < 0.001). LA and LV volume indices and LV Doppler parameters are reported in Table 1. Athletes had higher maximum (p = 0.001), pre-P (p = 0.001), and minimum (p < 0.001) LA volumes compared with controls (Fig. 1) and also larger LV end-diastolic (p < 0.0001), LV end-systolic (p = 0.005), LV SV (p = 0.001), and LVM index (p < 0.0001). E/A ratio (p < 0.05) and e′/a′ ratio (p < 0.05) were both higher but E/e′ ratio lower in athletes compared to controls (p < 0.05) (all were within the normal range in both groups) (Table 1).
Dynamic changes in left atrial volume. Changes in maximum, minimum, and pre-P left atrial volumes observed in professional soccer players. *p = 0.001 vs. pre-season data; † p < 0.0001 vs. pre-season data. Data have been obtained in 26 athletes during the regular season (pre-, mid-, and end-season bars) and in 13 athletes after detraining (white bar with dotted lines)
Differences between athletes and controls in LA phasic volumes are shown in Fig. 2 and LA phasic volume indices in Table 2. Athletes had higher indexed LA reservoir volume (p < 0.05) and indexed LA conduit volume (p < 0.05) but similar indexed LA active volume (p = 0.74) to controls. LA reservoir and conduit fractions were not significantly different between the two groups; however, LA active fraction was lower in athletes than controls (p = 0.007).
Dynamic changes in left atrial phasic volumes. Changes in left atrial phasic volumes observed in professional soccer players during the season and after the detraining period. See text for details. ‡ p < 0.05 vs. pre-season data; § p ≤ 0.005 vs. pre-season data. Data have been obtained in 26 athletes during the regular season (pre-, mid-, and end-season bars) and in 13 athletes after detraining (white bar with dotted lines)
Changes in LA total volumes and in LV parameters during training period (Table 3)
No change in body surface area was observed during the training period (overall p = 0.47). Resting heart rate fell and reached the lowest value at mid-training (60.6 ± 5.6 vs. 54.9 ± 7.6 bpm; p < 0.05 pre- vs. mid-training). The maximum, pre-P, and minimum LA volumes significantly increased during the mid- and end-training compared with pre-training (p < 0.0001 for both), with max absolute changes between end- and pre-training of 12.6, 5.6, and 7.1 mL, respectively, corresponding to a respective increase in LA volumes of 25, 43, and 31 %. There were no significant differences in LV end-diastolic volume, LV end-systolic volume, or LV SV during the training period. However, LVM increased, reaching the highest value at end-training (p < 0.005 vs. pre-training), this was contributed to by the increase in LVEDD and septal thickness. E/A ratio and E/e′ ratio did not change. An increase in inferior vena cava diameter was noticed, with the highest value at mid-season (22.7 ± 4.6 vs. 20.3 ± 3.5 mm at pre-training; p < 0.05).
Changes in LA phasic volumes and LA phasic fractions (Table 4)
LA reservoir volume and LA conduit volume increased over the training period, reaching the highest value at end-training (p = 0.005 and p < 0.05, respectively). LA true conduit volume index did not significantly change over the training period (23.8 ± 6.5 at pre-training, 27.9 ± 8.8 at mid-training, and 22.1 ± 5.0 at end-training; p = 0.18 pre-training vs. mid-training; p = 0.39 pre-training vs. end-training; and p = 0.05 mid-training vs. end-training, respectively). LA active volume remained unchanged. LA reservoir and conduit fractions decreased at mid-training (p = 0.006 and p = 0.007, respectively), but LA active fraction did not change (p = 0.34).
Effect of detraining on LA function
After 2 months of detraining, LA size fell and there was no difference between pre- and detraining measurements of maximum (p = 0.31), pre-P (p = 0.16), or minimum (p = 0.52) volumes. Similar effect was seen in LA phasic volumes with no differences between pre- and detraining values in reservoir (p = 0.38), conduit (p = 0.84), and active (p = 0.15) volumes as well as in LA reservoir (p = 0.69), conduit (p = 0.71), and active (p = 0.44) fractions.
Univariate correlation of LA structural and function parameters over-time
On univariate analysis, maximum LA volume correlated with LV mass index at mid- and end-training (r = 0.55, p < 0.05 and r = 0.74, p < 0.005, respectively). LA reservoir volumes modestly correlated with LV mass indices (at mid- and end-training, r = 0.49, p < 0.05, and r = 0.64, p < 005, respectively). The changes in LA conduit volume (end- vs. pre-training) correlated with the change in LV EDV and SV between the two time points (r = 0.68, p < 0.05 and r = 0.86, p < 0.0001, respectively). The changes in LA minimum volume between the two time points correlated with the respective change in LV EDV and SV (r = 0.55, p < 0.05 and r = 0.64, p < 0.05, respectively).
In the controls, LVM index correlated modestly with LA maximum volume (r = 0.55, p < 0.005) and poorly with LA reservoir volume (r = 0.37, p < 0.05), on univariate analysis.
Determinants of LA total and phasic volumes
The only independent predictor of maximum LA volume was LVM index, at mid- and end-training (β = 0.55, p < 0.05 and β = 0.74, p < 0.005, respectively), accounting for 30 and 55 %, respectively, of the variability explained by the model. The only independent predictor of LA reservoir volume was LVM index, at the same two time points (β = 0.54, p < 0.05 and β = 0.87, p < 0.005, respectively), accounting for 30 and 76 %, respectively, of the variability. Respective predictor of the difference in LA minimum volume change was LV SV (β = 0.65, p < 0.05), accounting for 42 % of the total variability. LVM index was identified as the only independent predictor of both LA maximum volume (β = 0.49, p < 0.005) and LA reservoir volume (β = 0.36, p < 0.05) also in the control group.
Discussion
Findings: The present study confirms and extends previous observations showing the changes in LA size and function through the three phases of the cardiac cycle, i.e., maximal filling (reservoir), passive empting (conduit), and active empting (atrial pump) and demonstrating that the morpho-functional LA remodeling occurs in athletes in response to increasing training load over the competitive season.
Top-level athletes had larger indexed LA volumes at the time of maximum atrial filling and passive empting, but similar volumes during atrial systole compared with controls. LA volume increased further with changes in training intensity and volume, again during the reservoir and conduit phases, but remained unchanged during the active LA pumping phase. However, 2 months after detraining, the LA volumes fell and became not different from pre-training values. Finally, the only independent predictor of maximum LA volume at-end training was LVM index, which was determined by the increase in LV end-diastolic diameter and septal thickness.
Data interpretation: The increased LA pre-training volume is likely to reflect chronic cavity remodeling in a group of soccer players. The exact relationship between such changes in LA volumes and LV structure and function, being its counterpart during the cardiac cycle, has never been fully understood. It has, however, become clearer when we studied volume changes during training. LA volumes during the reservoir and conduit phases increased further, along with LV end-diastolic volume, and achieved their largest values at peak training time. This atrio-ventricular coupled behavior may, in part, be explained on the basis of LV adaptive mechanism and increased venous return in order to cope with the progressive increase in stroke volume demand with exercise. This theory is supported by the sole predicting ability of LVM index of maximum LA volume, confirming that the main driving force for LA volumetric change is the LV structure and function. Interestingly, LA volume during the active pumping phase (late diastole) was not different from controls and did not change with training. This confirms two facts: (1) in those athletes despite LA remodeling, its pump function remains preserved and (2) In the presence of maintained LV filling in early diastole, there was no need for a change in LA systolic function during its pumping phase. This is further confirmed when the volumes regressed to their original size after detraining and still its systolic function remained stable.
Furthermore, the results of this study demonstrate that a decrease in resting heart rate and an increase in LV preload are able to facilitate the observed increase in LA “true” conduit phase, identifying this phase as a relevant determinant of LV filling. Noteworthy, the interaction between the LA and the LV is complex: indeed, while previous cross-sectional investigations demonstrated a relationship between LA and LV volumes (D’Andrea et al. 2010; Pelliccia et al. 2005), in this longitudinal study, we found that, while LA seems to be early affected by the hemodynamic changes induced by exercise, its morphological remodeling is maintained in the long-term, contrary to the rapid response observed for the LV, after the decrease in training volume and intensity. Although we can only speculate about the possible mechanisms beyond this phenomenon, the different content in contractile proteins observed between the LA and the LV and the need to maintain an “economized” heart at rest with a different atrio-ventricular protein concentration (Pelouch et al. 1995) could at least in part explain our findings.
It is noteworthy that in our study, the index of intra-cardiac filling pressure (i.e., the E/e′ ratio) was normal and remained within normal limits over the different season periods, despite the substantial atrial and LV morphological remodeling. This finding suggests that atrial cavity responds to the increased hemodynamic pre-load (induced by chronic exercise) by enhancing the reservoir and conduit function in order to accommodate the increasing venous return and maintain normal contractile function, efficient emptying function, and stroke volume, in a manner similar to that seen in volume overloaded LV. It must be noted that the pattern of LA remodeling in the athlete substantially differs from that observed in pathological LV increased mass index such as systemic hypertension or hypertrophic cardiomyopathy. In those conditions, the LA enlargement is associated with the increase of LV filling pressure and the ensuing reduction of LA passive and emptying volumes, thus leads to the compensatory increase in the atrial active emptying time and emptying fraction (Eshoo et al. 2009; Erol et al. 2002). Similarly, LA enlargement in hypertrophic cardiomyopathy is associated with reduced LV compliance and relaxation, decreased atrial conduit volume, and increased active emptying fraction (Eshoo et al. 2010). Thus, in those pathological conditions, LA remodeling conveys impairment of reservoir and conduit function as a consequence of increased hemodynamic afterload and an abnormal LV stiffness. Conversely, in athlete’s heart, the dynamic remodeling of the LA is associated with an enhanced reservoir and conduit phase, while LA contractile function remains stable, suggesting also a benign adaptation of the LV. Indeed, contrary to data observed in this study, a maladaptive remodeling of the LV would be associated with a worsening in LA reservoir and conduit function and an increased LA active contribution to LV filling, in order to compensate the increased LV stiffness. Thus, taking together, the analysis of dynamic changes in LA phasic volumes demonstrates that exercise conditioning is able to generate in the athlete a further atrial functional reserve, representing a relevant benign contribution to training-induced cardiovascular remodeling.
Limitations: This study has obvious limitations. The sample size is small, and this limitation could have influenced the correlation analysis: indeed, a correlation between resting bradycardia and atrial function has been previously reported (D’Ascenzi et al. 2011). This correlation was not confirmed in this study, but we cannot exclude that this results is related to the small sample size of the study. However, the small sample size is justified by the need to enroll a well-selected group of athletes who shared the same sport and similar training protocol. We anticipate large number of variabilities with bigger sample volume including coaching pattern of practice and individual athlete’s skills.
We are unable to confirm or refute the absolute or partial recovery of LA structure and function after detraining, since many factors could play parts, including age and type of sports. Furthermore, although we observed an inverse remodeling of exercise-induced LA adaptation after detraining, we cannot exclude that the existence of a cumulative effect of repeated years of training could lead to some irreversible LA morphological or functional changes.
Conclusions
LA remodeling in top-level athletes includes functional changes such as increased LA reservoir and conduit volume and the relative reduction of LA active emptying. LA remodeling is dynamic in nature, varies during competitive training in response to incremental training loads and after detraining. The strong correlation between exercise-induced LA and LV remodeling supports the concept that morpho-functional LA remodeling also represents a physiological and benign response to athletic training.
Abbreviations
- LA:
-
Left atrial
- LV:
-
Left ventricular
- BSA:
-
Body surface area
- SV:
-
Stroke volume
- LVM:
-
Left ventricular mass
- EDV:
-
End-diastolic volume
References
Abhayaratna WP, Seward JB, Appleton CP, Douglas PS, Oh JK, Tajik AJ, Tsang TS (2006) Left atrial size: physiological determinants and clinical implications. J Am Coll Cardiol 47:2357–2363
Boyd AC, Ng AC, da Tran T, Chia EM, French JK, Leung DY, Thomas L (2010) Left atrial enlargement and phasic function in patients following non-ST elevation myocardial infarction. J Am Soc Echocardiogr 23:1251–1258
Braunwald E, Frahm C (1961) Studies on Starling’s law of the heart, IV: observations on the hemodynamic functions of the left atrium in man. Circulation 24:633–642
Calvo N, Brugada J, Sitges M, Mont L (2012) Atrial fibrillation and atrial flutter in athletes. Br J Sports Med 46(Suppl 1):i37–i43
D’Andrea A, Riegler L, Cocchia R, Scarafile R, Salerno G, Gravino R, Golia E, Vriz O, Citro R, Limongelli G, Calabrò P, Di Salvo G, Caso P, Russo MG, Bossone E, Calabrò R (2010) Left atrial volume index in highly trained athletes. Am Heart J 159:1155–1161
D’Ascenzi F, Cameli M, Zacà V, Lisi M, Santoro A, Causarano A, Mondillo S (2011) Supernormal diastolic function and role of left atrial myocardial deformation analysis by 2D speckle tracking echocardiography in elite soccer players. Echocardiography 28:320–326
D’Ascenzi F, Cameli M, Lisi M, Zacà V, Natali B, Malandrino A, Benincasa S, Catanese S, Causarano A, Mondillo S (2012) Left atrial remodelling in competitive adolescent soccer players. Int J Sports Med 33:795–801
D’Ascenzi F, Pelliccia A, Natali BM, Cameli M, Andrei V, Incampo E, Alvino F, Lisi M, Padeletti M, Focardi M, Bonifazi M, Mondillo S (2015) Increased left atrial size is associated with reduced atrial stiffness and preserved reservoir function in athlete’s heart. Int J Cardiovasc Imaging (Epub ahead of print)
D’Ascenzi F, Cameli M, Padeletti M, Lisi M, Zacà V, Natali B, Malandrino A, Alvino F, Morelli M, Vassallo GM, Meniconi C, Bonifazi M, Causarano A, Mondillo S (2013) Characterization of right atrial function and dimension in top-level athletes: a speckle tracking study. Int J Cardiovasc Imaging 29:87–94
Du Bois D, Du Bois EF (1916) A formula to estimate the approximate body surface area if height and weight be known. Arch Intern Med 17:863–871
Erol MK, Yilmaz M, Acikel M, Karakelleoglu S (2002) Left atrial mechanical function in patients with essential hypertension. Acta Cardiol 57:323–327
Eshoo S, Ross DL, Thomas L (2009) Impact of mild hypertension on left atrial size and function. Circ Cardiovasc Imaging 2:93–99
Eshoo S, Semsarian C, Ross DL, Thomas L (2010) Left atrial phasic volumes are modulated by the type rather than the extent of left ventricular hypertrophy. J Am Soc Echocardiogr 23:538–544
Fagard R (2003) Athlete’s heart. Heart 89:1455–1461
Inama G, Pedrinazzi C, Durin O, Inama L, Furlanello F (2010) Atrial fibrillation and flutter in athletes. G Ital Cardiol (Rome) 11:102S–106S
Jarvinen V, Kupari M, Hekali P, Poutanen VP (1994) Assessment of left atrial volumes and phasic function using cine magnetic resonance imaging in normal subjects. Am J Cardiol 73:1135–1138
Kasner M, Westermann D, Steendijk P, Gaub R, Wilkenshoff U, Weitmann K, Hoffmann W, Poller W, Schultheiss HP, Pauschinger M, Tschöpe C (2007) Utility of Doppler echocardiography and tissue Doppler imaging in the estimation of diastolic function in heart failure with normal ejection fraction: a comparative Doppler-conductance catheterization study. Circulation 116:637–647
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise J, Solomon S, Spencer KT, St John Sutton M, Stewart W (2006) Recommendations for chamber quantification. Eur J Echocardiogr 7:79–108
Leung DY, Boyd A, Ng AA, Chi C, Thomas L (2008) Echocaridographic evaluation of left atrial size and function: current understanding, pathophysiologic correlates, and prognostic implications. Am Heart J 158:836–844
Mascia G, Perrotta L, Galanti G, Padeletti L (2013) Atrial fibrillation in athletes. Int J Sports Med 34:379–384
Mujika I, Padilla S (2000) Detraining: loss of training-induced physiological and performance adaptations. Part I: short term insufficient training stimulus. Sports Med 30:79–87
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelisa A (2009) Recommendations of evalutation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr 10:165–193
Nikitin NP, Witte KKA, Thackray SDR, Goodge LJ, Clark AL, Cleland JGF (2003) Effect of age and sex on left atrial morphology and function. Eur J Echocardiogr 4:36–42
Ofman P, Khawaja O, Rahilly-Tierney CR, Peralta A, Hoffmeister P, Reynolds MR, Gaziano JM, Djousse L (2013) Regular physical activity and risk of atrial fibrillation: a systematic review and meta-analysis. Circ Arrhythm Electrophysiol 6:252–256
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfiled MM, Tajik AJ (2000) Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation 102:1788–1794
Pelliccia A, Maron BJ, Di Paolo FM, Biffi A, Quattrini FM, Pisicchio C, Roselli A, Caselli S, Culasso F (2005) Prevalence and clinical significance of left atrial remodeling in competitive athletes. J Am Coll Cardiol 46:690–696
Pelouch V, Milerová M, Ostádal B, Hucín B, Samánek M (1995) Differences between atrial and ventricular protein profiling in children with congenital heart disease. Mol Cell Biochem 147:43–49
Pluim BM, Zwinderman AH, van der Laarse A, van der Wall EE (2000) The athlete’s heart: a meta-analysis of cardiac structure and function. Circulation 101:336–344
Prioli A, Marino P, Lanzoni L, Zardini P (1998) Increasing degrees of left ventricular filling impairment modulate left atrial function in humans. Am J Cardiol 82:756–761
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines of the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713
Spencer KT, Mor-Avi V, Gorcsan J 3rd, DeMaria AN, Kimball TR, Monaghan MJ, Perez JE, Weinert L, Bednarz J, Edelman K, Kwan OL, Glascock B, Hancock J, Baumann C, Lang RM (2001) Effects of aging on left atrial reservoir, conduit, and booster pump function: a multi-institution acoustic quantification study. Heart 85:272–277
Thomas L, Levett K, Boyd A, Leung DY, Schiller NB, Ross DL (2002) Compensatory changes in atrial volumes with normal aging: is atrial enlargement inevitable? J Am Coll Cardiol 40:1630–1635
Tükek T, Akkaya V, Atilgan D, Demirel E, Ozcan M, Güven O, Korkut F (2001) Effect of left atrial size and function on P-wave dispersion: a study in patients with paroxysmal atrial fibrillation. Clin Cardiol 24:676–680
Utomi V, Oxborough D, Whyte GP, Somauroo J, Sharma S, Shave R, Atkinson G, George K (2013) Systematic review and meta-analysis of training mode, imaging modality and body size influences on the morphology and function of the male athlete’s heart. Heart 99:1727–1733
Yu CM, Sanderson JE, Marwick OhJK (2007) Tissue Doppler imaging a new prognosticator for cardiovascular disease. J Am Coll Cardiol 49:1903–1914
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Keith Phillip George.
Rights and permissions
About this article
Cite this article
D’Ascenzi, F., Pelliccia, A., Natali, B.M. et al. Training-induced dynamic changes in left atrial reservoir, conduit, and active volumes in professional soccer players. Eur J Appl Physiol 115, 1715–1723 (2015). https://doi.org/10.1007/s00421-015-3151-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-015-3151-7