Abstract
Dental implant material has an impact on adhesion and spreading of oral mucosal cells on its surface. Platelet-rich fibrin (PRF), a second-generation platelet concentrate, can enhance cell proliferation and adhesion. The aim was to examine the regulatory effects of PRF and titanium surfaces on cellular adhesion, spread, and cytokine expressions of gingival keratinocytes. Human gingival keratinocytes were cultured on titanium grade 4, titanium grade 5 (Ti5), and HA discs at 37 °C in a CO2 incubator for 6 h and 24 h, using either elutes of titanium-PRF (T-PRF) or leukocyte and platelet-rich fibrin (L-PRF), or mammalian cell culture medium as growth media. Cell numbers were determined using a Cell Titer 96 assay. Interleukin (IL)-1β, IL-1Ra, IL-8, monocyte chemoattractant protein (MCP)-1, and vascular endothelial growth factor (VEGF) expression levels were measured using the Luminex® xMAP™ technique, and cell adhesion and spread by scanning electron microscopy. Epithelial cell adhesion and spread was most prominent to Ti5 surfaces. L-PRF stimulated cell adhesion to HA surface. Both T-PRF and L-PRF activated the expressions of IL-1 β, IL-8, IL-1Ra, MCP-1, and VEGF, T-PRF being the strongest activator. Titanium surface type has a regulatory role in epithelial cell adhesion and spread, while PRF type determines the cytokine response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Integrity of the soft-tissue seal around the abutment of dental implants is crucial for the clinical success (Atsuta et al. 2012; Ivanovski and Lee 2018). Titanium, either in pure (Ti1–4) or in an alloy form, is the most common material used to fabricate implants in dentistry (Cordeiro and Barão 2017). Surface characteristics like chemical composition, charge, topography, and roughness have a significant effect on the adhesion and protein expression of human oral cells to titanium (Lauer et al. 2001; Schwartz-Filho et al. 2012). Formation of a thin-oxide layer on the outer surface of the titanium and titanium alloys also affects the adhesion of cells to implant surfaces (Lausmaa et al. 1990). The interaction of the titanium oxide layer, rutile surface, with the organic molecules provides further intercourse between the cell and implant (YazdanYar et al. 2018). Moreover, the contamination of the titanium surfaces with saliva and bacteria is a potential risk factor to maintain the integrity of the titanium oxide layer (Delgado-Ruiz and Romanos 2018). Therefore, numerous surface modification methods have been described to alter and create an antibacterial effect on titanium surfaces (Chouirfa et al. 2019). Recent evidence suggests that, in addition to its regulatory effects on cell adhesion, titanium may induce a strong immune response in macrophages (Li et al. 2018). There is evidence that titanium particles can be found in epithelial cells, connective tissue, macrophages, and bone tissue, and presence of these particles is associated with the initiation of the inflammatory response and expression of cytokines (Suárez-López del Amo et al. 2018). However, information on oral mucosal keratinocyte response is missing in this context.
Platelets have a stimulatory effect on wound healing and tissue hemostasis (Mosesson et al. 2001). Platelet-rich fibrin (PRF) is a natural biomaterial, and it is prepared by centrifuging the blood sample directly after drawing it. The main principle to obtain PRF membrane is the centrifugation of the freshly drawn blood in a glass/glass coated tubes at 2700–3000 rpm for 12–15 min, approximately 400G forces (Dohan Ehrenfest et al. 2006). PRF is an autogenous source of growth factors, in which platelets are the main cells responsible for its biologic activity. The flexible and dense fibrin structure of the PRF membrane provides slow- and long-term secretion of the growth factors such as platelet-derived growth factor, transforming growth factor ß, vascular endothelial growth factor, insulin-like growth factor-1 which are responsible for the enhanced healing (Pierce et al. 1991). Moreover, the trapped cytokines in the gel form of the PRF membrane induce the regulation of the epithelial cell migration to wound surfaces and accelerate angiogenesis (Ratajczak et al. 2018). PRF may stimulate the proliferation and differentiation of cells of oral origin, as well (Ehrenfest et al. 2009). The clinical benefits of both platelet products have been discussed recently (Schliephake et al. 2018) and their effect on enhancing the early phase of osseointegration has been pointed out (Strauss et al. 2018).
All protocols to produce PRF use an immediate centrifugation; however, variations in techniques, such as using titanium tubes [for titanium platelet-rich fibrin (T-PRF)] or glass tubes [for leukocyte and platelet-rich fibrin (L-PRF)], can significantly affect biological properties and clinical implications of the outcome product (Tunali et al. 2014). The histological structures of the L-PRF and T-PRF show similarities to each other, yet the fibrin network of the T-PRF was much denser than L-PRF (Tunali et al. 2014). Even though there are slight differences in the centrifugation protocol of both fibrin products [2800 rpm, 12 min for T-PRF (Tunali et al. 2014); 3000 rpm, 10 min for L-PRF (Dohan et al. 2009)], titanium tubes that are used in the production of T-PRF are found to be the underlying reason of potent platelet activation (Tunali et al. 2014). Dense fibrin structure of T-PRF membranes gives additional beneficial effects on the treatment of soft-tissue treatment around the teeth and dental implants due to its elongated resorption time (Ustaoglu et al. 2016).
In the present study, we hypothesized that adhesion, spread, and cytokine expression of gingival keratinocytes are affected by the grade of titanium, and this effect can be modified by PRF. Therefore, we aimed to examine the cellular adhesion of gingival keratinocytes to Ti4 and Ti5 titanium surfaces and the expression of interleukin (IL)-1β, IL-1Ra, IL-8, monocyte chemoattractant protein (MCP)-1, and vascular endothelial growth factor (VEGF) in the presence or absence of T-PRF and L-PRF.
Materials and methods
Preparation of L-PRF and T-PRF
A systemically healthy non-smoking study volunteer donated the whole blood samples. The L-PRF and T-PRF membranes were produced as described by Tunali et al. (2014), with slight modifications. A 36 ml of blood sample was collected with four non-additive test tubes (9 ml, Vacuette 455,092; Grenier Bio-One GmbH, Frickenhausen, Germany). A half of the blood sample (18 ml) was quickly transferred into two separate titanium grade 4 tubes. Two non-additive and two titanium grade 4 tubes were centrifuged (#SL8R, Thermo Fisher Scientific, Waltham, MA, USA) at 2700 rpm for 15 min at room temperature. After centrifugation, L-PRF (from non-additive tubes) and T-PRF (from two titanium grade 4 tubes) clots were taken out from the tubes using sterile tweezers and each one was placed on discrete sterile gauze pads. To obtain the L-PRF and T-PRF membranes, the bases of all fibrin clots including the red corpus part were removed with sterile scissors, and serum components of the fibrin clot were removed by squeezing the clot gently between sterile gauze pads.
PRF-elute extraction
Elute extractions were performed according to Gassling et al. (2013). Briefly, L-PRF and T-PRF membranes were broken into rectangular fragments with one side length 7 mm and three pieces obtained from each membrane were placed in a 24-well cell culture plate (Costar 3524, Corning Incorporated, Corning, NY, USA). Membrane fragments were incubated with a serum-free DMEM media for 1 h at 37 °C and 5% CO2. The elutes, which were obtained from the pieces of the PRF membranes, were pooled and stored separately at 4 °C.
Isolation of human oral keratinocyte cells
Human oral keratinocyte (HMK) cells, which are a spontaneously transformed cell line, were isolated from a healthy human gingival biopsy sample and were received from Dr. M. Mäkelä, University of Helsinki, Finland (Mäkelä et al. 1999). The chromosome number of the cells was found to be around hypertriploid range (70–76, with a cell-to-cell variation). HMK cells were sustained in a 75 cm2 cell culture flask (Corning Incorporated, Corning, NY, USA) with a keratinocyte serum-free media (SFM-X, Gibco, Thermo Fisher Sci. Co, Waltham, Massachusetts, USA), containing human recombinant epidermal growth factor, bovine pituitary extract, and antibiotics (penicillin–streptomycin, 10,000 U/mL, Gibco, Thermo Fisher Sci. Co, Waltham, Massachusetts, USA) at 37 °C and 5% CO2. Keratinocyte growth media were replaced with fresh SFM-X three times per week, and the HMK cells were passaged when reaching 80–90% confluence. HMK cells used for the experiments were chosen from passage number 22.
Test discs
In all experiments, machine surfaced titanium grade 4 (Ti4, Servo-Dental, Hagen, Germany), machine surfaced titanium grade 5 (Ti5, Implance, Trabzon, Turkey), and as a control surface hydroxyapatite (HA, Clarkson Chromatography Inc., South Williamsport, PA, USA) discs were used. All discs had a diameter of 5 mm and a thickness of 2 mm.
Cell culture
Equal numbers of HMK cells (1 × 104) were seeded on Ti4, Ti5, and HA discs, using either elutes of T-PRF or L-PRF, or SFM-X as growth media. Cells were incubated at 37 °C in a CO2 incubator for 6 h and 24 h. All experiments were performed in quintuplicate. At the end of the incubation periods, elute and media were transferred into Eppendorf tubes and stored in − 70 °C for cytokine analysis. The cells on titanium and HA surfaces were used for the cell number and SEM analyses.
Cell number analysis on test discs
Cell numbers on each test disc were determined using the Cell Titer 96 assay (Promega Corporation, Wisconsin, USA) with a plate reader at 490 nm. To convert the absorbance values to the number of living cells, HMK cells at five different densities were incubated with the cell titer assay at 37 °C in a CO2 incubator for 1 h. After incubation, the absorbance was measured at 490 nm; a standard curve was created by plotting the absorbance against the number of incubated cells. Elute and media alone were used in determination of the background absorbance.
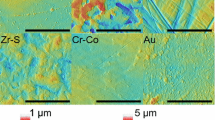
SEM imaging
After the incubation periods, the cells covering the surface were immediately fixed by a conventional chemical fixation with 5% glutaraldehyde in 0.16 mol 1–1 s-collidine–HCl buffer at pH 7.4 for 20 min, followed by a chemical dehydration in graded ethanol series (50%, 70%, and 98%) with 5 min embedding intervals. The discs were removed from the bottom of the Eppendorf tubes and kept at room temperature to allow air drying for overnight. Then, the discs were mounted on SEM specimen metal stubs (covered with electrically conductive material) and each one of them sputters carbon-coated for one second. The surface microtopography of the specimen was visualized by the LEO 1530Gemini scanning electron microscope (Carl Zeiss, Oberkochen, Germany). The magnification of the images taken corresponds to a Polaroid 545 print and an image size of 8.9 × 11.4 cm.
Cytokine concentrations
After incubating the cells for 6 and 24 h, IL-1β, IL-1Ra, IL-8, MCP-1, and VEGF concentrations in T-PRF and L-PRF elutes, and SFM-X media were measured with the Luminex® xMAP™ technique (Luminex Corporation, Austin, TX) using the pro-human cytokine group I assays (Bio-Rad, Santa Rosa, CA). The detection limit of the assay was 0.6 pg/mL for IL-1β, 5.5 pg/mL for IL-1Ra, 1.0 pg/mL for IL-8, 1.1 pg/mL for MCP-1, and 3.1 pg/mL for VEGF. Elute and media alone were used in the determination of the background absorbance.
Statistical analysis
The IBM SPSS V24.0 software (IBM, Armonk, North Castle, New York, USA) was used for statistical analysis. One-way analysis of variance (ANOVA) with Tukey’s HSD was used for the analysis of the differences in cell proliferation and cytokine expression levels. The p value of p < 0.05 was accepted as statistically significant.
Results
Elevated numbers of HMK cells on Ti4, Ti5, and HA discs were found after 6 and 24 h incubations in the T-PRF and L-PRF groups, in comparison to the SFM-X group. In addition, the numbers of HMK cells on HA discs after 24 h incubation were higher than those on Ti4 and Ti5 discs in the L-PRF and T-PRF groups (Fig. 1).
The SEM analysis revealed that, after 6 h incubation, more cell adhesion and spread had occurred in the Ti4 and Ti5 groups, in comparison to the HA group. Keratinocytes in the HA group were either round or started to be elongated with a few filopodia. In the Ti4 and Ti5 groups, both filopodia and lamellipodia were visible in majority of the cells. Of the three surfaces examined, cell spread was most prominent on Ti5 surface. In the HA group, cell spread improved when the cells were incubated with the L-PRF extract, while cells tend to form aggregates when they were incubated with T-PRF. A small number of platelet cells adhered to epithelial cells was observed in the PRF and T-PRF groups (Figs. 2, 3).
SEM analysis of human oral keratinocyte (HMK) cell adhesion and spread on grade 4 and 5 titanium (Ti4 and Ti5) and hydroxyapatite (HA) discs after 6 h of incubation. Two ended arrow: gap between HMK cells. Black arrow: A spreading HMK cell with lamellipodia. Black dashed arrow: A round HMK cell with filopodia. White arrows: Platelets. White dashed arrow: HMK cell clumps. Scale bars indicate 1 µm
After 24 h incubation, the PRF extract-treated cells on Ti4 and Ti5 discs formed uneven multilayers; however, the number of cell layers was not even in all the parts of the disc (Figs. 4, 5). Cell-to-cell junctions and cell spread were most prominent in Ti5 group. Cells in the HA group lost their initial roundness and become more elongated.
After 6 h incubation, cells on the T-PRF discs produced the highest concentrations of IL-1β, IL-1RA, and IL-8, while those on the SMF-X discs were the lowest. No difference was observed in the MCP-1 concentrations between the tested groups (Fig. 6). After 24 h incubation, the highest concentrations of IL-1β, IL-1RA, and IL-8 were produced by cells in the T-PRF group, and the lowest concentrations were in the SFM-X group. VEGF and MCP concentrations did not significantly differ between the T-PRF and L-PRF groups, yet their concentrations were higher than in the SFM-X group (Fig. 7).
Concentrations of interleukin (IL)-1β, IL-1ra, IL-8, monocyte chemoattractant protein (MCP)-1, and vascular endothelial growth factor (VEGF) in T-PRF and L-PRF elutes and SFM-X media after incubating gingival keratinocytes on grade 4 and 5 titanium (Ti4 and Ti5) and hydroxyapatite (HA) discs for 6 h
Concentrations of interleukin (IL)-1β, IL-1ra, IL-8, monocyte chemoattractant protein (MCP)-1, and vascular endothelial growth factor (VEGF) in T-PRF and L-PRF elutes and SFM-X media after incubating gingival keratinocytes on grade 4 and 5 titanium (Ti4 and Ti5) and hydroxyapatite (HA) discs for 24 h
There was no detectable concentration of IL-1β, IL-8, VEGF, or MCP-1 in elutes of L-PRF or T-PRF, or in SFM-X growth media, whereas low concentrations of IL-1RA were measured in each growth medium.
Discussion
To our knowledge, this is the first study to examine adhesion characteristics and cytokine production of gingival epithelial cells on two different titanium grade discs and to analyze the modifying effects of PRF on these parameters. According to our results, Ti5 has superiority in epithelial cell adhesion and spread against Ti4 and HA, besides the cytokine expression by epithelial cells is strongly induced in the presence of T-PRF.
Although machined surfaces of Ti4 and Ti5 show similar characteristics in their morphology, corrosion resistance, and biocompability, they differ in their chemical composition (Özcan and Hämmerle 2012). The amorphous oxide layer formation and existence of small amounts of alloying elements on Ti5 (Shah et al. 2016) may explain its superiority in epithelial cell spread and adhesion over Ti4 and HA surfaces.
One interesting finding in the present study was that the application of PRF increased the cell spread only on HA discs. Growth factors in the PRF play a significant role in stimulating the proliferation of human oral cells (Dohan Ehrenfest et al. 2009a, b). It has been shown that bone morphogenetic proteins have affinity to bind HA (Rohanizadeh and Chung 2011). As PRF carries high amounts of bone morphogenetic proteins, it is possible that these proteins accumulated on HA surface stimulate the proliferation and spread of gingival keratinocytes.
Based on our results, titanium surfaces have no regulatory effect on cytokine expression of gingival keratinocytes. It was recently demonstrated that titanium ions (9 ppm) activate cytokine expression of gingival epithelial cells (Wachi et al. 2015). In the present study, we used 6 and 24 h steady incubation models, which may not necessarily induce an abrasion on titanium surfaces, and eventually titanium release and elevated cytokine expression. Both T-PRF and L-PRF stimulated cytokine expression significantly. The previous studies have shown that platelet-released growth factors stimulate the induction of IL-6 and antimicrobial peptides in primary human keratinocytes (Bayer et al. 2016, 2018). Conversely, in a clinical study where the use of PRF membrane was compared to connective tissue graft in the treatment of localized gingival recessions, the application of PRF membrane had no effect on the gingival crevicular fluid IL-1β levels after 10 days (Eren et al. 2016). L-PRF contains leukocytes, monocytes, and platelets, thus being a significant source of IL-1β, IL-6, and VEGF as well, and the concentration, release dynamics, and kinetics of these growth factors have been demonstrated in vitro (Schär et al. 2015). Yet, in the present study, cytokine levels in PRF elute were nearly undetectable. Instead of PRF, we used PRF elute as a test material. This model has been applied successfully on osteoblast cultures for bone tissue engineering (Gassling et al. 2013). The purpose of the PRF-elute preparation was to get a well-homogenized PRF structure to be used in a disc-culture model. It was previously shown that leukocytes and platelets are not homogenously distributed in L-PRF and the heterogeneous distribution of growth factors and some other proteins in the fibrin network might be an explanation to the unequal release of these molecules after PRF’s application (Dohan Ehrenfest 2010). One limitation of the use of elute is that elute does not contain the fibrin component of PRF; thus, the cellular composition differs between PRF and PRF elute. The second limitation is that the origin of the blood and the epithelial cells used in the present study come from two different individuals. Even though the blood donor was a systemically healthy and non-smoking volunteer, it is unclear if age or gender has any effect on PRF composition. Finally, the present study used monolayer culture model to evaluate the cell spread and cytokine secretion. Non-differentiating cell monolayers do not simulate gingiva, because they lack of stratification, vertical cell contacts, and differentiation (Gursoy et al. 2016). Thus, it might be beneficial to test the present study hypothesis on an organotypic-titanium cell culture model.
In conclusion, the composition of titanium has a regulatory effect on the adhesion and spread of human gingival epithelial cells. PRF was proved to be a strong inducer of cytokine expression of gingival epithelial cells, but also contributed to the cell spread characteristics. Increased understanding of these mechanisms involved in the cellular process may help in an attempt to improve the wound healing in peri-implant tissues. Besides, it might be possible to improve pocket reduction and clinical attachment gain in peri-implantitis treatment with the aid of PRF treatments.
References
Atsuta I, Ayukawa Y, Ogino Y, Moriyama Y, Jinno Y, Koyano K (2012) Evaluations of epithelial sealing and peri-implant epithelial down-growth around “step-type” implants. Clin Oral Implants Res 23(4):459–466. https://doi.org/10.1111/j.1600-0501.2011.02163.x
Bayer A, Lammel J, Rademacher F, Groß J, Siggelkow M, Lippross S, Klüter T, Varoga D, Tohidenzhad M, Pufe T, Cremer J, Gläser R, Harder J (2016) Platelet-released growth factors induce the antimicrobial peptide human beta-defensin-2 in primary keratinocytes. Exp Dermatol 25(6):460–465. https://doi.org/10.1111/exd.12966
Bayer A, Tohidenzhad M, Berndt R, Lippross S, Behrendt P, Klüter T, Pufe T, Jahr H, Cremer J, Rademacher F, Simanski M, Gläser R, Harder J (2018) Platelet-released growth factors inhibit proliferation of primary keratinocytes in vitro. Ann Anat 2015:1–7. https://doi.org/10.1016/j.aanat.2017.09.002
Chouirfa H, Bouloussa H, Migonney V, Falentin-Daudré C (2019) Review of titanium surface modification techniques and coatings for antibacterial applications. Acta Biomater 83:37–54. https://doi.org/10.1016/j.actbio.2018.10.036
Cordeiro JM, Barão VAR (2017) Is there scientific evidence favoring the substitution of commercially pure titanium with titanium alloys for the manufacture of dental implants? Mater Sci Eng C Mater Biol Appl 71:1201–1215. https://doi.org/10.1016/j.msec.2016.10.025
Delgado-Ruiz R, Romanos G (2018) Potential causes of titanium particle and ion release in implant dentistry: a systematic review. Int J Mol Sci 19(11):,3585. https://doi.org/10.3390/ijms19113585
Dohan Ehrenfest DM (2010) How to optimize the preparation of leukocyte- and platelet-rich fibrin (L-PRF, Choukroun’s technique) clots and membranes: introducing the PRF Box. Oral Surg Oral Med Oral Pathol Oral Radiol Oral Endod 110(3):275–278. https://doi.org/10.1016/j.tripleo.2010.05.048
Dohan Ehrenfest DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evoluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101(3):e37–44. https://doi.org/10.1016/j.tripleo.2005.07.008
Dohan Ehrenfest DM, Rasmusson L, Albrektsson T (2009a) Classification of platelet concentrates from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol 27(3):158–167. https://doi.org/10.1016/j.tibtech.2008.11.009
Dohan Ehrenfest DM, Diss A, Odin G, Doglioli P, Hippolyte MP, Charrier JB (2009b) In vitro effects of Choukroun’s PRF (platelet-rich fibrin) on human gingival fibroblasts, dermal prekeratinocytes, preadipocytes, and maxillofacial osteoblasts in primary cultures. Oral Surg Oral Med Oral Pathol Oral Radiol Oral Endod 108:341–352. https://doi.org/10.1016/j.tripleo.2009.04.020
Eren G, Tervahartiala T, Sorsa T, Atilla G (2016) Cytokine (interleukin-1beta) and MMP levels in gingival crevicular fluid after use of platelet-rich fibrin or connective tissue graft in the treatment of localized gingival recessions. J Periodontal Res 51(4):481–488. https://doi.org/10.1111/jre.12325
Gassling V, Hedderich J, Açil Y, Purcz N, Wiltfang J, Douglas T (2013) Comparison of platelet rich fibrin and collagen as osteoblast-seeded scaffolds for bone tissue engineering applications. Clin Oral Implants Res 24(3):320–328. https://doi.org/10.1111/j.1600-0501.2011.02333.x
Gursoy UK, Gursoy M, Könönen E, Sintim HO, Uitto VJ, Syrjänen S (2016) Construction and characterization of a multilatered gingival keratinocyte culture model: the TURK-U model. Cytotechnology 68(6):2345–2354. https://doi.org/10.1007/s10616-016-0029-4
Ivanovski S, Lee R (2018) Comparison of peri-implant and periodontal marginal soft tissues in health and disease. Periodontol 76(1):116–130. https://doi.org/10.1111/prd.12150
Lauer G, Wiedmann-Al-Ahmad M, Otten JE, Hübner U, Schmelzeisen R, Schilli W (2001) The titanium surface texture effects adherence and growth of human gingival keratinocytes and human maxillar osteoblast-like cells in vitro. Biomaterials 22(20):2799–2809. https://doi.org/10.1016/S0142-9612(01)00024-2
Lausmaa J, Kasemo B, Mattsson H (1990) Surface spectroscopic characterization of titanium implant materials. Apple Surface Sci 44(2):133–146. https://doi.org/10.1016/0169-4332(90)90100-E
Li XZ, Huang Q, Elkhooly TA, Liu Y, Wu H, Feng Q, Liu L, Fang Y, Zhu W, Hu T (2018) Effects of titanium surface roughness on the mediation of osteogenesis via modulating the immune response of macrophages. Biomed Mater 13(4)::045013. https://doi.org/10.1088/1748-605X/aabe33
Mäkelä M, Larjava H, Pirilä E, Maisi P, Salo T, Sorsa T, Uitto VJ (1999) Matrix metalloproteinase 2 (gelatinase A) is related to migration of keratinocytes. Exp Cell Res 251(1):67–78. https://doi.org/10.1006/excr.1999.4564
Mosesson MW, Siebenlist KR, Meh DA (2001) The structure and biological features of fibrinogen and fibrin. Ann NY Acad Sci 936:11–30. https://doi.org/10.1111/j.1749-6632.2001.tb03491.x
Özcan M, Hämmerle C (2012) Titanium as a reconstruction and implant material in dentistry: advantages and pitfalls. Materials (Basel) 5(9):1528–1545. https://doi.org/10.3390/ma5091528
Pierce GF, Mustoe TA, Altrock BW, Deuel TF, Thomason A (1991) Role of platelet-derived growth factor in wound healing. J Cell Biochem 45(4):319–326. https://doi.org/10.1002/jcb.240450403
Ratajczak J, Vangansewinkel T, Gervois P, Merckx G, Hilkens P, Quirynen M, Lambrichts I, Bronckaers A (2018) Angiogenic properties of ‘Leukocyte- and Platelet-Rich Fibrin’. Sci Rep 8(1):14632. https://doi.org/10.1038/s41598-018-32936-8
Rohanizadeh R, Chung K (2011) Hydroxyapatite as a carrier for bone morphogenetic protein. J Oral Implantol 37(6):659–672. https://doi.org/10.1563/AAID-JOI-D-10-00005
Schär MO, Diaz-Romero J, Kohl S, Zumstein MA, Nesic D (2015) Platelet-rich concentrates differentially release growth factors and induce cell migration in vitro. Clin Orthop Relat Res 473(5):1635–1643. https://doi.org/10.1007/s11999-015-4192-2
Schliephake H, Sicilia A, Nawas BA, Donos N, Gruber R, Jepsen S, Milinkovic I, Mombelli A, Navarro JM, Quirynen M, Rocchietta I, Schiødt M, Schou S, Stähli A, Stavropoulos A (2018) Drugs and diseases: summary and consensus statements of group 1. In: The 5th EAO consensus conference 2018. Clin Oral Implants Res, pp 18:93–99. https://doi.org/10.1111/clr.13270
Schwartz-Filho HO, Morandini AC, Ramos-Junior ES, Jimbo R, Santos CF, Marcantonio E Jr, Wennerberg A, Marcantonio RA (2012) Titanium surfaces with nanotopography modulate cytokine production in cultured human gingival fibroblasts. J Biomed Mater Res A 100(10):2629–2636. https://doi.org/10.1002/jbm.a.34200
Shah FA, Stenlund P, Martinelli A, Thomsen P, Plamquist A (2016) Direct communication between osteocytes and acid-etched titanium implants with a sub-micron topography. J Mater Sci Mater Med 27(11):167. https://doi.org/10.1007/s10856-016-5779-1
Strauss FJ, Stähli A, Gruber R (2018) The use of platelet-rich fibrin to enhance the outcomes of implant therapy: a systematic review. Clin Oral Implants Res 29(18):6–19. https://doi.org/10.1111/clr.13275
Suárez-López del Amo, F, Garaicoa-Pazmiño C, Fretwurst T, Castilho RM, Squarize CH (2018) Dental implants-associated releasef titanium particles: a systematic review. Clin Oral Implants Res 29(11):1085–1100. https://doi.org/10.1111/clr.13372
Tunali M, Özedemir H, Küçükodacı Z, Akman S, Yaprak E, Toker H et al (2014) A novel platelet concentrate: titanium-prepared platelet-rich fibrin. BioMed Res Int 2014:209548. https://doi.org/10.1155/2014/209548
Ustaoglu G, Ercan E, Tunali M (2016) The role of titanium-prepared patelet rich fibrin in palatal mucosal wound healing nd histoconduction. Acta Odontol Scand 74(7):558–564. https://doi.org/10.1080/00016357.2016.1219045
Wachi T, Shuto T, Shinohara Y, Matono Y, Makihira S (2015) Release of titanium ions from an implant surface and their effect on cytokine production related to alveolar bone resorption. Toxicology 327:1–9. https://doi.org/10.1016/j.tox.2014.10.016
YazdanYar A, Aschauer U, Bowen P (2018) Interaction of biologically relevant ions and organic molecules with titanium oxide (rutile) surfaces: a review on molecular dynamics studies. Colloids Surf B Biointerfaces 161:563–577. https://doi.org/10.1016/j.colsurfb.2017.11.004
Acknowledgements
The authors are grateful for the skillful technical assistances of Katja Sampalahti from University of Turku and Linus Silvander from Åbo Akademi.
Funding
This study was supported by the Turku University Foundation (Grant no: 12198, UKG) and by the Scientific and Technological Research Council of Turkey (Grant no: BIDEB 2219-1059B191600656, GK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kasnak, G., Fteita, D., Jaatinen, O. et al. Regulatory effects of PRF and titanium surfaces on cellular adhesion, spread, and cytokine expressions of gingival keratinocytes. Histochem Cell Biol 152, 63–73 (2019). https://doi.org/10.1007/s00418-019-01774-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-019-01774-8