Abstract
The diagnosis of neurosarcoidosis is often difficult; the imaging signs of spinal cord sarcoidosis sometimes mimic those of cervical spondylotic myelopathy, which is common in elderly persons. We examined the characteristics of spinal cord sarcoidosis in Japanese patients with neurosarcoidosis. This case series identified patients with neurosarcoidosis at four general hospitals and one university hospital from April 1998 to September 2010. All diagnoses were based on the diagnostic criteria proposed by Zajicek et al. Seventeen patients (nine men and eight women) were involved: six patients with spinal cord lesions accompanied by cervical spondylosis, five with cerebral lesions, three with cranial nerve lesions, two with meningitis, and one with nerve root lesions. Patients with spinal cord sarcoidosis had a higher onset age, longer duration from onset to diagnosis, reduced leukocytosis in the cerebrospinal fluid (CSF), and lower angiotensin-converting enzyme (ACE) levels in the CSF. The results of this study indicate that diagnosis of spinal cord sarcoidosis requires careful evaluation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neurosarcoidosis is a rare manifestation that occurs in 5% of systemic sarcoidosis patients; it is characterized by multisystem non-caseous granulomatous disease of an unknown etiology [1]. Neurosarcoidosis lesions mainly involve the optic and cranial nerves and the spinal cord [2]. The diagnosis of neurosarcoidosis is often difficult in clinical practice and requires magnetic resonance imaging (MRI) to detect the abnormalities and the evidence of systemic sarcoidosis [2, 3]. Spinal cord sarcoidosis exhibits intramedullary high-intensity signals on T2-weighted images (T2WI) and enhancements on gadolinium (Gd) DTPA-enhanced T1-weighted images (Gd-T1WI) [4, 5]; however, these signs also resemble cervical myelopathy with spondylosis [6]. Although cervical spondylotic myelopathy, which is common in elderly persons, sometimes mimics spinal cord sarcoidosis, a similar operative treatment is not effective for spinal cord sarcoidosis with cervical spondylosis [7]. Therefore, the diagnosis of spinal sarcoidosis is important for effective treatment. Systemic sarcoidosis shows racial differences in its incidence and clinical manifestations [8]. Case reports and case series on spinal cord sarcoidosis have been reported in western countries and Japan [5, 9]; however, the characteristics of spinal cord sarcoidosis have not been sufficiently investigated compared to other neurosarcoidosis lesions.
The purpose of this study was to identify the characteristics of spinal cord sarcoidosis that differentiate it from other neurosarcoidosis lesions in the Japanese population by reviewing consecutive patients in our hospital.
Methods
This study enrolled patients diagnosed with neurosarcoidosis at the neurology departments of four general hospitals (Asahikawa Red Cross Hospital, Hakodate Municipal Hospital, Sapporo Municipal Hospital, and Obihiro Kosei General Hospital) and one university hospital (Hokkaido University Hospital), from April 1998 to September 2010. The diagnosis of neurosarcoidosis was based on the diagnostic criteria proposed by Zajicek et al. [2] and the response to steroid treatment. We retrospectively reviewed medical records, and collected data on the course of neurosarcoidosis, diagnostic imaging, laboratory findings, and treatment regimens as well as their results. We compared patients with spinal cord sarcoidosis with patients with other forms of neurosarcoidosis. Age at onset, duration from the onset of neurological symptoms to the diagnosis of neurosarcoidosis, serum angiotensin-converting enzyme (ACE) levels, and cerebrospinal fluid (CSF) findings were compared using Mann–Whitney U test. We also compared laboratory findings before and after treatment to evaluate the usefulness of each item for disease activity. We excluded patients who did not have sufficient evidence of neurosarcoidosis, such as hemifacial palsy without abnormal findings in diagnostic imaging. The Institutional Review Board of Hokkaido University Hospital approved this study.
Results
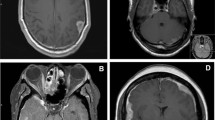
The demographics of the 17 patients are summarized in Table 1. Cases 3, 8, and 17 were previously described as case reports by one of the authors of the present study [10–12]. There were six patients with spinal cord lesions, five with cerebral lesions, three with cranial nerve lesions, two with meningitis, and one with nerve root lesions. All spinal cord sarcoidoses occurred in the cervical cord, and they were accompanied by cervical spondylosis. Three of the spinal cord sarcoidosis patients underwent 2-[18F]-fluoro-2-deoxy-d-glucose positron emission tomography (FDG-PET) examinations [13], and all of them displayed abnormal uptake in the spinal cord lesion. Methotrexate was additionally administered during the initial corticosteroid treatment for cases 1, 2, and 7.
A comparison between patients with spinal cord sarcoidosis and those with other forms of neurosarcoidosis revealed significant differences in onset age, duration from onset to diagnosis, leukocytes in CSF, and ACE levels in CSF. The onset age in spinal cord sarcoidosis (mean ± SD 61.0 ± 10.5 years) was higher than in other forms of neurosarcoidosis (mean ± SD 38.1 ± 18.5 years). Duration from onset to diagnosis in spinal cord sarcoidosis (mean ± SD 31.8 ± 36.4 months) was longer than other neurosarcoidoses (mean ± SD 7.3 ± 15.0 months). Patients with spinal cord sarcoidosis had lower leukocyte and ACE levels in CSF than patients with other forms of neurosarcoidosis (Fig. 1).
Alterations in the ACE levels after treatment for neurosarcoidosis are shown in Fig. 2. Serum ACE levels decreased in spinal cord sarcoidosis and other forms of neurosarcoidosis after treatment with corticosteroids. The reduction in ACE levels in CSF was less obvious than that in serum.
Discussion
We identified some characteristics of spinal cord sarcoidosis from our case series. First, spinal cord sarcoidosis tended to occur in elderly patients and required a longer duration to develop from onset to diagnosis. Second, leukocytes and ACE levels were not elevated in CSF of spinal cord sarcoidosis patients. Third, serum ACE levels reflected the disease activity after treatment.
A national survey on sarcoidosis in Japan revealed the incidence rate to be 1.01 per 100,000 individuals, with 7.2% of these cases displaying neurological complications [14]. The incidence rate exhibited a bimodal distribution that consisted of young men and middle-aged to elderly women. In our cases, spinal cord sarcoidosis was mainly associated with the elderly. Conversely, cerebral lesions in neurosarcoidosis were mainly associated with younger men. A longer duration between onset and diagnosis in spinal cord sarcoidosis may be associated with the elderly patients and cervical spondylosis complications, because cervical myelopathy mimicked the clinical symptoms of spinal cord sarcoidosis. Laboratory findings are essential for the diagnosis of neurosarcoidosis; however, spinal cord sarcoidosis resulted in less frequent abnormal findings in CSF than other forms of neurosarcoidosis in our study. Varron et al. [5] reported that four of seven cases of spinal cord sarcoidosis had normal or near-normal cell counts, and six of them had normal ACE levels in CSF. Cohen-Aubart et al. [15] also reported that eight of 28 cases of spinal cord sarcoidosis had normal cell counts and more than 50% patients had normal ACE levels in CSF. These characteristics indicate that careful evaluation for spinal cord sarcoidosis is required for patients with systemic sarcoidosis and cervical spondylosis.
2-[18F]-fluoro-2-deoxy-d-glucose positron emission tomography is becoming an additional diagnostic tool for different forms of neurosarcoidosis, including spinal cord sarcoidosis [9, 16]. We recently reported the usefulness of FDG-PET for the differentiation of spinal cord sarcoidosis from cervical spondylotic myelopathy [13].
Spinal cord sarcoidosis is one of the steroid-refractory lesions among neurosarcoidoses and often requires additional immunosuppressant therapy [17]. Methotrexate may be useful to maintain optimal disease suppression [3]. Therefore, indicators that represent the disease activity of spinal cord sarcoidosis are necessary for reasonable treatment. Oksanen et al. [18] reported the usefulness of ACE levels in CSF measured by an inhibitor binding assay to evaluate the disease activity of neurosarcoidosis; however, colorimetry was used in the present case, while investigation by Varron et al. [5] demonstrated that spinal cord sarcoidosis patients did not exhibit sufficient changes in the CSF-ACE levels to serve as an indicator. Although the methods used to measure ACE levels were different in each study, the symptoms caused by spinal cord lesions are still reliable indicators of spinal cord sarcoidosis. At the very least, on the basis of our findings, we propose that serum ACE levels may reflect the disease activity of neurosarcoidosis as a part of systemic sarcoidosis.
In conclusion, a review of Japanese patients with neurosarcoidosis found that spinal cord sarcoidosis is frequent in elderly patients with neurosarcoidosis and evinces fewer CSF abnormalities than other forms of neurosarcoidosis.
References
Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H Jr, Bresnitz EA, DePalo L, Hunninghake G, Iannuzzi MC, Johns CJ, McLennan G, Moller DR, Newman LS, Rabin DL, Rose C, Rybicki B, Weinberger SE, Terrin ML, Knatterud GL, Cherniak R (2001) Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med 164:1885–1889
Zajicek JP, Scolding NJ, Foster O, Rovaris M, Evanson J, Moseley IF, Scadding JW, Thompson EJ, Chamoun V, Miller DH, McDonald WI, Mitchell D (1999) Central nervous system sarcoidosis—diagnosis and management. QJM 92:103–117
Joseph FG, Scolding NJ (2007) Sarcoidosis of the nervous system. Pract Neurol 7:234–244
Saleh S, Saw C, Marzouk K, Sharma O (2006) Sarcoidosis of the spinal cord: literature review and report of eight cases. J Natl Med Assoc 98:965–976
Varron L, Broussolle C, Candessanche JP, Marignier R, Rousset H, Ninet J, Seve P (2009) Spinal cord sarcoidosis: report of seven cases. Eur J Neurol 16:289–296
Ozawa H, Sato T, Hyodo H, Ishii Y, Morozumi N, Koizumi Y, Matsumoto F, Kasama F, Aizawa T, Itoi E, Kokubun S (2009) Clinical significance of intramedullary Gd-DTPA enhancement in cervical myelopathy. Spinal Cord 48:415–422
Oe K, Doita M, Miyamoto H, Kanda F, Kurosaka M, Sumi M (2009) Is extensive cervical laminoplasty an effective treatment for spinal cord sarcoidosis combined with cervical spondylosis? Eur Spine J 18:570–576
Rybicki BA, Major M, Popovich J Jr, Maliarik MJ, Iannuzzi MC (1997) Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. Am J Epidemiol 145:234–241
Ota K, Tsunemi T, Saito K, Yamanami F, Watanabe M, Irioka T, Mizusawa H (2009) (18)F-FDG PET successfully detects spinal cord sarcoidosis. J Neurol 256(11):1943–1946
Takahashi I, Soma H, Sakushima K, Tsuji-Akimoto S, Niino M, Yabe I, Sasaki H (2010) Cervical intramedullary sarcoidosis diagnosed after laminoplasty for spondylosis. Shinkei Chiryogaku (Neurological Therapeutics) 27:209–213
Matsushima M, Miyazaki Y, Kano T, Tsuji S, Sasaki H (2006) Central nervous system sarcoidosis with extensive cerebral edema. ShinkeiNaika (Neurological Medicine) 64:314–316
Sakushima K, Niino M, Yabe I, Akimoto-Tsuji S, Sasaki H (2009) Weakness and sensory disturbance of the left extremities. J Clin Neurosci 16:1608–1711
Sakushima K, Yabe I, Shiga T, Yashima-Yamada M, Tsuji-Akimoto S, Terae S, Sasaki H (2011) FDG-PET SUV can distinguish between spinal sarcoidosis and myelopathy with canal stenosis. J Neurol 258:227–230
Morimoto T, Azuma A, Abe S, Usuki J, Kudoh S, Sugisaki K, Oritsu M, Nukiwa T (2008) Epidemiology of sarcoidosis in Japan. Eur Respir J 31:372–379
Cohen-Aubart F, Galanaud D, Grabli D, Haroche J, Amoura Z, Chapelon-Abric C, Lyon-Caen O, Valeyre D, Piette JC (2010) Spinal cord sarcoidosis: clinical and laboratory profile and outcome of 31 patients in a case-control study. Medicine (Baltimore) 89:133–140
Braun JJ, Kessler R, Constantinesco A, Imperiale A (2008) 18F-FDG PET/CT in sarcoidosis management: review and report of 20 cases. Eur J Nucl Med Mol Imaging 35:1537–1543
Bradley DA, Lower EE, Baughman RP (2006) Diagnosis and management of spinal cord sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 23:58–65
Oksanen V, Fyhrquist F, Somer H, Gronhagen-Riska C (1985) Angiotensin converting enzyme in cerebrospinal fluid: a new assay. Neurology 35:1220–1223
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sakushima, K., Yabe, I., Nakano, F. et al. Clinical features of spinal cord sarcoidosis: analysis of 17 neurosarcoidosis patients. J Neurol 258, 2163–2167 (2011). https://doi.org/10.1007/s00415-011-6080-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6080-3