Abstract
Purpose
To assess predictors of success and failure of an updated lateral pharyngoplasty as an independent procedure in treating obstructive sleep apnea with CPAP failures.
Methods
Forty-six patients with known OSAS who were resistant to CPAP or failures were included. BMI, Stop-Bang score, and sleep study data were recorded before and after the updated Cahali pharyngoplasty procedure. Pre-operative DISE was done for all cases; however, postoperative DISE was done only for non-responders.
Results
Successful operation outcomes achieved in 69.6% (32 cases) and 30.4% (14 cases) were failure rates. Postoperative snoring index, Stop Bang score, and AHI were significantly decreased compared to pre-operative data (p value < 0.001). There is statistically a significant increase in minimal and baseline SpO2 postoperatively (p value < 0.001). Patients with no laryngeal collapse (L0) predict operation success. However, patients with high pre-operative snoring index, collapse at lateral wall hypopharynx, high tongue collapse, laryngeal collapse, tongue palate interaction, and low grades tonsils (1, 2) predict the failure of the surgery (p value = 0.006*,0.024*,0.047*, respectively).
Conclusion
Updated Cahali lateral pharyngoplasty could not be used as an independent procedure in all OSA patients. The lack of laryngeal collapse (L0) is a considerable success predictor for the procedure. However, the pre-operative low-grade tonsils (1, 2) and high snoring index predict operation failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a major subgroup of sleep apnea distinguished by repetitive episodes of upper airway partial or total collapse despite the effort to breathe during sleep and is accompanied by a reduction in blood oxygen [1].
Severe sleep apnea patients had an increased risk for many systemic diseases as coronary artery disease, diabetes mellitus, and stroke [2]. A sleep study (polysomnography) is considered now as the “gold-standard” of diagnosis of obstructive sleep apnea and its degree [3].
The prevalence of OSA varies depending on the definition of hypopneas. Utilizing the traditional definition, hypopnea necessitates a 4% reduction in oxygen saturation of the blood. A cohort sleep study by Wisconsin approximated that 17.4% of ladies versus 33.9% of men in the united states aged 30–70 suffered from mild OSA (AHI of 5–14.9) [4].
People suffered from OSA are associated with a narrow upper airway, usually caused by parapharyngeal fat pads and pharyngeal muscles fat deposition or craniofacial structure abnormalities [5].
Many treatment options for obstructive sleep apneas syndrome (OSA) are obtainable, ranging from non-invasive behavioral modification to continuous positive airway pressure (CPAP) devices to surgical procedures. Patient selection for these therapies is a complex process due to variability in anatomy and physiology in every patient, patient preference, the severity of the disease, and controversy about the adequacy of the treatments accessible for the patients [3].
Lateral pharyngoplasty (LP) was introduced in 2003 by Cahali [6], and since then, it was updated several times [7,8,9,10,11,12] till it came to the updated Cahali lateral pharyngoplasty technique [13].
Cahali suggested that his updated lateral pharyngoplasty approach would benefit all OSA patients regardless of the sleep endoscopy results. The soft palate, tongue, and the thickness of the posterior tonsillar pillar are not selection factors [13].
Up till now, he has discovered no motivation to accept that the area or pattern of obstruction shown in drug-induced sleep endoscopies would better indicate or contraindicates this technique [13].
This proposition is against the current management plan, which recommends that a surgical treatment plan is made according to the obstruction site(s) [14].
This study intends to assess predictors of success and failure of an updated lateral pharyngoplasty as an independent procedure in treating obstructive sleep apnea with CPAP failures.
Materials and methods
This research examined 46 patients who suffered from OSAS with CPAP failures; it included 25 males (54.3%) and 21 females (45.7%) with ages ranging between 25 and 54. This research was carried out in Kafrelsheikh and Mansoura university hospitals from December 2018 to March 2020 and approved by Kafrelsheikh University Hospital ethical committee; explanation and informed written consent for this research has been endorsed from all patients.
Inclusion criteria
Adult patients > 18 years, general anesthesia fitness, obstructive sleep apneas syndrome patients confirmed and graded by polysomnography, CPAP failures patients with no history of sleep surgery.
Exclusion criteria
Young patients < 18 years, general anesthesia unfitness, patients with a past history of palatal surgery, e.g., Uvulopalatopharyngoplasty, morbid obesity, the presence of uncontrolled hypothyroidism, and considerable craniofacial abnormalities, e.g., Down syndrome, micrognathia, and retrognathia.
Evaluation
Every patient has been assessed by history with concern to sleep history utilizing the Stop Bang score. A thorough general examination is carried, with concern to BMI, neck circumference. ENT examination is carried for a deviated septum, hypertrophied turbinates, or any nasal masses; evaluation of the oral cavity for tongue, uvula, tonsils sizes, and Friedman’s tongue position. Brodsky grading scale was utilized to grade the tonsils into five grades: grade 0 (tonsils inside the tonsillar fossa), grade 1 (tonsils only outside of the tonsillar fossa and involve ≤ 25% of the oropharyngeal width), grade 2 (tonsils involve 26–50% of the oropharyngeal width), grade 3 (tonsils involve 5–75% of the oropharyngeal width), and grade 4 (tonsils involve > 75% of the oropharyngeal width) [15].
Polysomnography
Patients had a pre-operative and 6 months postoperative polysomnography utilizing (SOMNOscreen™ plus, USA) device to diagnose and grade the severity of OSAS. Apnea was characterized by airflow cessation for at least 10 s at the nostril and mouth, while hypopnea was characterized by a 30% or more reduction in oro-nasal airflow for at least 10 s with > 4% decline in baseline oxyhemoglobin saturation. Apnea–hypopnea index (AHI) is calculated by summation of apneas and hypopneas that occur in 1 h of sleep [16]. According to AHI, the OSA was graded to; mild: AHI = 5–15/hour, moderate: AHI = 15–30/hour, and severe: AHI > 30/hour.
Drug-induced sleep endoscopy (DISE)
Drug-induced sleep endoscopy (DISE) was performed in anesthetized patients with obstructive sleep apneas as a procedure of choice for analyzing the anatomic and dynamic areas of collapsibility prior to surgery [17]. Observation of the lateral pharyngeal wall, soft palate, tongue base, and larynx for anatomical and dynamic collapsible regions [18, 19], then lateral pharyngeal wall, palate, tongue, and larynx (LwPTL) grading system was utilized to classify the level of obstruction in our patients [19].
Surgical technique
Updated lateral pharyngoplasty by Dr. Cahali was done to our study patients independent of the sleep endoscopy results. The procedure began with bilateral tonsillectomy under general anesthesia; however, if previously performed, the tonsillar fossa mucosa was eliminated to distinguish the palatoglossus and palatopharyngeus muscles. The Brodsky grading scale was utilized to assess tonsil size, and none of our cases had a grade of 0, so tonsillectomy was performed for all cases. An upside-down ‘V-shape’ incision of mucosa and muscle of the oral lateral free margin of the soft palate and anterior pillar was eliminated [13]. A monopolar cautery and sharp dissection undermined the palatopharyngeus muscle (cranial half) from the superior pharyngeal constrictor muscle (SPC) until we reached the buccopharyngeal fascia (Fig. 1).
Stitch (3–0 monofilament absorbable suture) was inserted at the palatopharyngeus muscle at its lower end, where SPC is still linked there. A long Hartman nasal dressing forceps was utilized to undermine and elevate the caudal part of the SPC from the buccopharyngeal fascia medially within the tonsillar fossa to enlarge the retropalatal segment, then cut and cauterize the SPC vertically till the posterior pillar arch (less than 1 cm), then stitch the palatopharyngeus flap to the anterior pillar utilizing three to four separated 3–0 absorbable monofilament, vertical mattress stitches, with attention to that the higher the stitching place for the flap, the more anteriorly soft palate will be pulled (Fig. 2a,b,c) [13, 20].
Suturing the palatopharyngeus flap to the anterior pillar a, b. However, we do not fix those stitches until the next step, which is the cross-cutting of the palatopharyngeus muscle, comprise its pharyngeal mucosa, at the caudal portion of the flap, which acts for the first relaxed incision c next; we tie those sutures just tightly enough to oppose the edges
Finally, the wound’s margins might be everted and stitched by simple interrupted stitches of absorbable 3–0 monofilament type close to the uvula. A vertical loosening incision in the posterior pharyngeal wall’s mucosa is done medial to the flap from the soft palate’s free edge until it meets the first relaxing incision, complete the separation of the flap from the pharynx.
All the procedure steps should be repeated on the opposite side. Extubation should be delayed till the patients are fully awake with good muscle tone. The patients should be checked for 1–2 h in the recovery room before setting off to the ward. The surgical procedure should be assessed for: duration of surgery, the incidence of bleeding, and other complications, duration of hospital stay, and postoperative complications [13, 20].
The most recent strategy’s primary changes were planned to avoid extending the pharyngeal mucosa, increase retropalatal space, and splint the upper lateral pharyngeal wall with mucosal palatopharyngeus flap [13]. It contrasts with ordinary Cahali lateral pharyngoplasty, which relies principally on the laterally based flap of superior constrictor muscle stitched anteriorly to the palatoglossus muscle by four or five separate stitches [21].
Follow-up
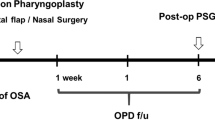
All patients were postoperatively checked at 1 week, 2 weeks, 1 month, and 6 months as outpatient visits to assess complications and manifestation relief. In addition, 6 months postoperatively, polysomnography was performed to report the AHI and other respiratory parameters to compare it to the pre-operative data. Sher’s success standards were utilized to define the surgical success; 50% reduction of the pre-operative AHI and AHI < 20 events/h. The surgical cure was reported if AHI became < 5 events/h postoperatively [22]. Six months after surgery, drug-induced sleep endoscopy (DISE) was repeated for failed cases to evaluate the pattern and level of obstruction and correlate as a predictor of failure for the procedure.
Statistical analysis
Data analysis was performed using the software SPSS (Statistical Package for the Social Sciences) version 20. Quantitative variables were described using their means and standard deviations. Categorical variables were described using their absolute frequencies and were compared using the Chi-squared test and the Fisher’s exact test when appropriate. Kolmogorov–Smirnov (distribution-type) and Levene (homogeneity of variances) tests were used to verify assumptions for use in parametric tests. An independent sample t test (used with normally distributed data) was used to compare two groups’ means. The Wilcoxon signed-rank test was used to compare the same group medians at two points of time (when data is not normally distributed). To compare the means of quantitative normally distributed variables for the same group at two points of time, a paired sample t test was used. Binary logistic regression was used to predict the odds of being a case based on the independent variables’ values (predictors). The level of statistical significance was set at 5% (p < 0.05). A highly significant difference was present if p ≤ 0.001.
Results
The research assessed 46 patients with obstructive sleep apneas syndrome with CPAP failure performed updated lateral pharynogoplasty; 25 males (54.3%) and 21 females (45.7%) and aged 25–54 with a mean 39.04 ± 6.802. All patients’ pre-operative clinical parameters as BMI, Stop Bang, AHI, snoring index, minimal SpO2, and baseline SpO2 were announced in the Table 1. Drug-induced sleep endoscopy (DISE score) for all study patients were announced in Table 2.
The results of the study based on Sher’s success criteria [22] (a decrease of the AHI by 50% and AHI < 20), that the success rate was 69.6% (32 cases) and 30.4% failure rate (14 cases) while 19.6% (nine patients) was a cure rate (AHI < 5 events/h).
There is statistically a significant increase in minimal and baseline SpO2 postoperatively (pre-operative minimal SpO2 increased from 78.8 to 87.72%, and pre-operative baseline SpO2 increased from 96.2 to 96.54%). There is a statistically significant decline in the snoring index from 157.74 to 82.65. Similarly, there is a statistically significant decrease in the apnea–hypopnea index from 34.05 to 16.6. There is a statistically significant decrease in the stop bang index (median decreased from 4 to 2) Table 1.
In this study, surveying the relationship between DISE results and their effect on operation results announced that patients with lateral wall hypopharynx collapse, high tongue, laryngeal collapse, and tongue palate interaction considerably predict failure of the surgery (p value = 0.022). In comparison, the absence of laryngeal collapse (L0) predicts a successful operation results Table 2.
There is a statistically significant relation between outcome and pre-operative snoring index, minimal SpO2, baseline SpO2, AHI, and Stop Bang score. Failure is associated with a higher pre-operative snoring index, AHI, and Stop Bang score. It is also associated with lower minimal and baseline SpO2. There is a statistically significant association between outcome and OSA grades. Severe degrees were associated with failure. There is a statistically non-significant relation between outcome and age, BMI, operation time, or complications Table 3.
Multivariate analysis of factors associated with operation failure among the studied patients by binary logistic regression showed that a higher snoring index and lower minimal SpO2 increases the risk of operation failure by 1.145- and 1.622-folds, respectively Table 4.
There were no patients with the previous tonsillectomy enrolled in this study. However, there was a statistically significant positive relationship between tonsil grade and operation success, where success rate increase with high grades (3, 4). Comparing results of low grades (1, 2) and high grades (3, 4), we found that tonsil grades 1 and 2 increased the risk of failure of operation by 4.77-folds, Table 5.
Bleeding in two patients (4.3%) and velopharyngeal insufficiency (VPI) in one patient (2.22%) were announced as complications Table 3.
Discussion
The updated lateral pharyngoplasty procedure was performed for all patients independent of their sleep endoscopy results. Patients were always counseled about the availability of non-surgical option before proceeding to surgery, and we recommend surgery in case of CPAP refusal or failure as CPAP orientation is mandatory.
The results of the study based on Sher’s success criteria [22] reported that the success rate was 69.6% (32 cases) and 30.4% failure rate (14 cases). The cure rate (19.6%) is low but taking in consideration that reaching AHI less than 5 as a cure rate is extremely difficult especially most of our cases were severe OSAS (more than 30 event/hour) which were 29 cases in our study, so we depend mainly on success criteria than cure rate [23, 26]. Park et al. [24] showed a surgical response in 11 of 12 patients (91.7%) in the lateral pharyngoplasty group, and eight out of 12 patients achieved success (66.7%). Mean AHI improved significantly from 36.3 ± 28.6 to 14.8 ± 17.9, reducing approximately 60%.
Even with higher grade tonsillar hypertrophy, we prefer to do lateral pharyngoplasty and not isolated tonsillectomy because the burden of isolated adult tonsillectomy remains a significant issue. Moreover, if velar collapse persisted after tonsillectomy dissection of the palatopharyngeus will be more difficult and less successful. Best chance is to operate upon a virgin lateral pharyngeal wall.
The procedure substantially decreases the Stop Bang score, AHI, and snoring index (p value < 0.001). Likewise, it substantially increases minimal SpO2 and baseline SpO2 dramatically (p value < 0.001), with significant postoperative AHI degree improvement. Cahali et al. [21] reported a substantial reduction of AHI with 60% of the patients over 50%, a reduction in AHI in contrast with pre-operative one where the median AHI decreased from 41.2 to 9.5. Likewise, Dizdar et al. [25] reported a significant reduction in the mean AHI from 23.4 to 11.3 postoperative to lateral pharyngoplasty (p < 0.05). Parameters such as RDI, lowest O2 saturation, oxygen desaturation index (ODI), mean O2 saturation, supine AHI, and ESS also significantly improved after surgery in Park et al.’s work [24].
Correlation of DISE results to the success of the operation, we found that lateral wall, tongue, and laryngeal collapses, significantly predict failure operation outcomes. However, the palatal collapse had no significant prediction in operation outcome. All patients with lateral wall-collapse at hypopharynx (LH) level, high tongue base (TH), laryngeal collapse (L1), and tongue palate interaction had failure outcomes. Although other levels had successful outcomes, they were not significant predictors.
Missale et al. [26] had a success rate of 89% with a cure rate of 20%. But, it depends on the criteria chosen, which influence the success rate, as they include patients with obstruction at the palatal or lateral pharyngeal wall, according to the NOHL classification. They excluded patients with complete base-tongue, hypopharyngeal, or laryngeal collapse.
A second DISE was repeated for failed cases; it showed that four patients still had persistent collapse at lateral wall hypopharynx; five patients still had high tongue base collapse; three patients still had a persistent laryngeal collapse; and two patients still had a palatal collapse. Postoperative DISE of cases showed the same findings except tongue palate interaction which showed a stiff palate with high tongue collapse, so the interaction seems to disappear, and they needed further procedure according to the level of collapse [19].
Green et al. [27] reported that any oropharyngeal lateral wall-collapse or obstruction was related to a 50% reduction in the surgery outcome’s odds. Poorer results may be explained by non-easily handled oropharyngeal lateral walls in surgery.
In the Chi et al. [28] study, patients with moderate OSAS can be benefited more from lateral pharyngoplasty than those with severe OSAS. As in patients suffering from severe OSAS, the lateral pharyngeal space and the retroglossal space should be evaluated.
We performed transoral DISE to understand the tongue's role more deeply. We evaluated the degree of tongue retraction, interaction with the palate, and position from the oral cavity and the nasopharynx, highlighting a secondary anteroposterior soft palate collapse, due to the tongue position [29].
In this research, there were three successful cases with isolated lateral pharyngoplasty that had low tongue base collapse (6.5%) with an improvement of AHI, the usage of (LwPTL) classification could explain why we had only three successful cases with low tongue base collapse as we did not consider the partial collapse of a given structure favorable. Genta PR et al. [30] announced that no significant data of physiological meaning could be given for partial visual collapses. Likewise, Katsantonis et al. [31] had 4 (20%) cases of tongue collapse using VOTE classification.
So, the updated Cahali lateral pharyngoplasty technique could not be used as an independent procedure in all OSA patients. It can be used in most OSA patients except in patients who had a collapse of the lateral wall at the hypopharynx level (LH), high tongue base collapse (TH), laryngeal collapse (L1), and tongue palate interaction.
This study utilized a multivariate analysis of operation failure factors among the studied patients by binary logistic regression. This showed that a higher snoring index and lower minimal SpO2 increase the risk of operation failure by 1.145- and 1.622-folds, respectively.
In this research, there were no patients with previous tonsillectomy enrolled in this study. However, there is a statistically significant positive relationship between tonsil grade and operation success (65.6% % success rate in grades 3, 4). Comparing results of low grades (1, 2) and high grades (3, 4), we found that tonsil grades 1 and 2 (low grades) increased the risk of failure of operation by 4.77-folds. These findings are only valid if tonsillectomy was a part of the procedure. Green et al. [27] did a univariate analysis and reported an increase in the odds of healing response (p = 0.008) with increasing tonsil size: 31% (32 of 102) with 0 tonsils, 41% (43 of 104) with 1 + tonsils, and 55% (38 of 69) with 2 + tonsils with no significant difference in surgical outcome in OSA severity subgroup (p = 0.78) or center (p = 0.50).
No significant intra-operative complications are documented. However, minimal postoperative complications were announced with no substantial long-term morbidity as; secondary hemorrhage in 2 (4.3%) patients and velopharyngeal insufficiency (VPI) in one (2.2%) patient. Park and his colleague’s [24] announced postoperative hemorrhage in 9.8% (four cases) of the patients, which stopped spontaneously without intervention, but there were no complaints of VPI. Operative time ranged from 35 to 60 min.
Conclusions
The updated Cahali lateral pharyngoplasty technique could not be used as an independent procedure in all OSA patients. It can be used in most OSA patients except in the collapse of a lateral wall at the hypopharynx level (LH), high tongue base collapse (TH), laryngeal collapse (L1), and tongue palate interaction patients. The absence of laryngeal collapse (L0) is a significantly predict success of the procedure. The pre-operative high snoring index and low grades tonsils (1, 2) predict the surgery’s failure.
Data availability
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gottlieb DJ, Punjabi NM (2020) Diagnosis and management of obstructive sleep apnea: a review. JAMA 323(14):1389–1400
Jean-Louis G, Zizi F, Clark LT, Brown CD, McFarlane SI (2008) Obstructive sleep apnea and cardiovascular disease: role of the metabolic syndrome and its components. J Clin Sleep Med 4(3):261–272
Flemons WW (2002) Clinical practice. Obstructive sleep apnea. N Engl J Med 347(7):498–504
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep disordered breathing in adults. Am J Epidemiol 177(9):1006–1014
Schwab RJ, Pasirstein M, Pierson R et al (2003) Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am J Respir Crit Care Med 168(5):522–530
Cahali MB, Formigoni GGS, Gebrim EMMS, Miziara ID (2004) Lateral pharyngoplasty versus uvulopalatopharyngoplasty: a clinical, polysomnographic, and computed tomography measurement comparison. Sleep 27(5):942–950
Pang KP, Woodson BT (2007) Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg 137(1):110–114
Li HY, Lee LA (2009) Relocation pharyngoplasty for obstructive sleep apnea. Laryngoscope 119(12):2472–2477
Dantas DA, Mauad T, Silva LF, Lorenzi-Filho G, Formigoni GG, Cahali MB (2012) The extracellular matrix of the lateral pharyngeal wall in obstructive sleep apnea. Sleep 35(4):483–490
Komada I, Miyazaki S, Okawa M, Nishikawa M, Shimizu T (2012) A new modification of uvulopalatopharyngoplasty for the treatment of obstructive sleep apnea syndrome. Auris Nasus Larynx 39(1):84–89
Sorrenti G, Piccin O (2013) Functional expansion pharyngoplasty in the treatment of obstructive sleep apnea. Laryngoscope 123(11):2905–2908
De Paula Soares CF, Cavichio L, Cahali MB (2014) Lateral pharyngoplasty reduces nocturnal blood pressure in patients with obstructive sleep apnea. Laryngoscope 124(1):311–316
Cahali MB (2019) Lateral pharyngoplasty. In: Friedman M, Jacobowitz O (eds) Sleep apnea and snoring: surgical and nonsurgical therapy, 2nd edn. Philadelphia, EUA, Elsevier, pp 229–234
Carvalho B, Hsia J, Capasso R (2012) Surgical therapy of obstructive sleep apnea: a review. Neurotherapeutics 9(4):710–716
Ng SK, Lee DL, Li AM, Wing YK, Tong MC (2010) Reproducibility of clinical grading of tonsillar size. Arch Otolaryngol Head Neck Surg 136(2):159–162
Hirshkowitz M (2016) Polysomnography challenges. Sleep Med Clin 11(4):403–411
Sharifian MR, Zarrinkamar M, Alimardani MS et al (2018) Drug induced sleep endoscopy in obstructive sleep apnea. Tanaffos 17(2):122–126
Park D, Kim JS, Heo SJ (2019) Obstruction patterns during drug-induced sleep endoscopy vs natural sleep endoscopy in patients with obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg 145(8):730–734 (Published online ahead of print, 2019 Jun 27)
Elsobki A, Cahali MB, Kahwagi M (2019) LwPTL: a novel classification for upper airway collapse in sleep endoscopies. Braz J Otorhinolaryngol 85(3):379–387
Elzayat S, El-Sobki A, El-Deeb ME, Moussa HH (2020) Managing obstructive sleep apnea patients with CPAP failure with a novel lateral pharyngoplasty as a stand-alone procedure. Am J Otolaryngol 41(4):102500
Cahali MB (2003) Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope 113(11):1961–1968
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19(2):156–177
Iannella G, Magliulo G, Di Luca M, De Vito A, Meccariello G, Cammaroto G et al (2020) Lateral pharyngoplasty techniques for obstructive sleep apnea syndrome: a comparative experimental stress test of two different techniques. Eur Arch Otorhinolaryngol 277(6):1793–1800
Park DY, Chung HJ, Park SC et al (2018) Surgical outcomes of overlapping lateral pharyngoplasty with or without coblator tongue base resection for obstructive sleep apnea. Eur Arch Otorhinolaryngol 275(5):1189–1196
Dizdar D, Civelek Ş, Çaliş ZA, Dizdar SK, Coşkun BU, Vural A (2015) Comparative analysis of lateral pharyngoplasty and uvulopalatopharyngoplasty techniques with polysomnography and Epworth Sleepiness Scales. J Craniofac Surg 26(7):e647–e651
Missale F, Fragale M, Incandela F et al (2020) Outcome predictors for non-resective pharyngoplasty alone or as a part of multilevel surgery, in obstructive sleep apnea-hypopnea syndrome. Sleep Breath 24(4):1397–1406
Green KK, Kent DT, D’Agostino MA et al (2019) Drug-induced sleep endoscopy and surgical outcomes: a multicenter cohort study. Laryngoscope 129(3):761–770
Chi JC, Chiang RP, Chou TY, Shu CH, Shiao AS, Lin CM (2015) The role of lateral pharyngoplasty in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 272(2):489–496
De Vito A, Carrasco Llatas M, Ravesloot MJ et al (2018) European position paper on drug-induced sleep endoscopy: 2017 update. Clin Otolaryngol 43(6):1541–1552
Genta PR, Sands SA, Butler JP et al (2017) Airflow shape is associated with the pharyngeal structure causing OSA. Chest 152(3):537–546
Katsantonis GP, Moss K, Miyazaki S, Walsh J (1993) Determining the site of airway collapse in obstructive sleep apnea with airway pressure monitoring. Laryngoscope 103(10):1126–1131
Funding
The authors have no funding or financial relationships to disclose.
Author information
Authors and Affiliations
Contributions
AE research conception and design, HH methodology statistical analysis, MD final revision and data collection, AF reference collection and data collection, SZ review writing and supervision.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research editorial boards and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for publication
Formal consent was signed by the patients to share and to publish their data in this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on sleep apnea syndrome. Guest editors: Manuele Casale, Rinaldi Vittorio.
Rights and permissions
About this article
Cite this article
Elsobki, A., Moussa, H.H., Eldeeb, M.E. et al. Efficacy, predictors of success and failure of an updated lateral pharyngoplasty approach as an independent procedure in treating obstructive sleep apnea with CPAP failures. Eur Arch Otorhinolaryngol 279, 945–953 (2022). https://doi.org/10.1007/s00405-021-06825-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06825-2