Abstract
Purpose
Considerable number of patients with obstructive sleep apnea (OSA) failed to respond to positive airway pressure therapy and so turned to surgical procedures. A wide variety of surgical procedures have been developed and advanced, according to obstruction and target site through nasal cavity to trachea. We introduced our overlapping lateral pharyngoplasty (OLP) technique as a surgical option for OSA and evaluated its surgical outcomes both with and without endoscope-guided coblator tongue base resection (CobTBR).
Methods
Sixty-five patients underwent either OLP alone or OLP combined with CobTBR to treat OSA at academic tertiary center. Twenty-nine patients underwent postoperative polysomnography and were divided into two groups, as an OLP group and an OLP combined CobTBR group. Various parameters from physical examinations and polysomnographic results were compared and analyzed.
Results
Most enrolled patients improved on various polysomnographic parameters, including AHI and oxygen levels. In the OLP group, 91.7% of patients showed a surgical response and the overall success rate was 66.7%. Mean AHI improved significantly from 36.3 to 14.8. In the OLP + CobTBR group, all patients showed improvement in AHI and the surgical response rate was 100%. The overall success rate was 70.6% and mean AHI improved from 38.8 to 13.1. In both groups, various parameters such as RDI, lowest O2 saturation, mean O2 saturation, oxygen desaturation index, supine AHI, and ESS significantly improved after surgery.
Conclusion
Our OLP technique appears to be safe and effective among OSA patients. Multi-level OLP surgery combined with CobTBR can be a good surgical strategy for patients experiencing retroglossal obstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obstructive sleep apnea (OSA) is reported to be 3–9% in the general population, and OSA is associated with resistant hypertension, cardiovascular disease, neurological disease, and various types of mortality [21]. Moreover, OSA has deleterious effects on economic productivity, and is known to be a significant contributor to motor vehicle accidents [13]. The American Academy of Sleep Medicine (AASM) has recommended the use of a positive airway pressure (PAP) device for the first-line treatment of OSA [6]. However, studies of CPAP adherence rates have shown varying results [11, 18, 19]. Most studies reported a high non-adherence rate to CPAP; according to Weaver et al., the non-adherence rate to CPAP was 83%, using the defined value of adherence of the AASM minimum acceptable usage standards [18]. Given these findings, the role of surgery should not be overlooked, and optimal surgical techniques are necessary for OSA patients. However, the overall success rate using the traditional UPPP technique, first described by Fujita [9], was low, approximately 40% [17].
Therefore, the development and application of more effective sleep surgery techniques is necessary. Recently, the collapse of the lateral pharyngeal wall (LPW) has been suggested as an important factor in the pathogenesis of OSA, and persistent LPW collapse after conventional UPPP was one of the major contributors to the low success rate [14,15,16].
A new surgical procedure for preventing LPW collapse, lateral pharyngoplasty (LP), was first introduced by Cahali [2]. By involving the myotomy of the superior pharyngeal constrictor (SPC) muscle and suturing this with palatoglossus, this technique presented a better surgical outcome (approximately a 60% success rate) compared with conventional UPPP [2, 3]. In our clinical practice, we adopted this technique. However, we have encountered several problems with this technique. Therefore, we modified the original technique to improve LP.
In addition to LPW collapse, OSA patients often have multiple obstruction sites, and as such, multi-level surgery has become common. A recent meta-analysis reports a 66.4% success rate using multi-level surgery [12].
Among various multi-level surgeries, the surgical technique for OSA patients with retroglossal obstruction is often tongue base resection with Coblation® or transoral robotic technique, due to their good efficacy with low morbidity [1, 7].
To our knowledge, there have been no reports regarding the surgical outcomes of LP among patients requiring multi-level surgery or regarding the surgical outcomes of LP in multi-level surgery. Therefore, we aimed to introduce our overlapping LP (OLP) technique and analyze the surgical outcomes of OLP alone and OLP combined with coblator tongue base resection (CobTBR).
Materials and methods
Patients
We retrospectively reviewed the medical records of patients who attended our sleep clinic from 2013 to 2015. Among the patients with OSA, our OLP technique was applied to 65 patients who declined or failed to adhere to CPAP treatment. And twelve-nine patients agreed to postoperative PSG. Study patients received OLP alone or OLP combined with CobTBR. The patients were classified into two groups. The patients who underwent OLP without tongue base resection were classified as the OLP group and patients who underwent OLP with coblator tongue base resection were classified as the OLP + CobTBR group.
The subjects were assessed via physical examination, including nasopharyngoscopy with the Muller maneuver and/or drug-induced sleep endoscopy and findings were scored according to the scoring system reported by Kezirian [10]. We used OLP when the score was above 1 with a pattern of concentric or lateral wall obstruction of the velum (V) or lateral wall obstruction of the oropharynx (O). We considered the patient to have retroglossal obstruction if the tongue base (T) score was above 1 in antero-posterior and/or lateral dimension or if the tongue moved backward during full expiration with a closed mouth, according to Woodson’s hypotonic test [20], or with an open mouth. The CobTBR was considered if the patients were suspected of having a retroglossal obstruction (Table 1).
We analyzed and compared various features from physical examinations, polysomnographic parameters, surgical outcomes, and postoperative complications. We used two criteria to measure success, as reported by Carrasco-Llatas et al. [4]. The first criterion, a traditional definition suggested by Sher et al. [17], was a postoperative AHI below 20, with at least a 50% reduction in AHI. The second, stricter, criterion was a postoperative AHI below 10. Postoperative complications were evaluated using all the patients data with or without postoperative PSG (65 subjects) and other variables were evaluated using 29 subjects data with postoperative PSG. The study protocol was reviewed and approved by the Institutional Review Board.
Polysomnography
The PSG recording channels comprised two electroencephalographic (EEG) channels, electro-oculograms (EOG), electromyograms (EMG), pulse oximetry, nasal cannulas, thoracic and abdominal respiratory effort bands, and body position sensors. All 11 channels were applied to patients to measure the following parameters: EEG, EOG, EMG, electrocardiography, oxymetry, airflow, respiratory effort, and body position. All PSG data were scored manually, according to the AASM 2012 criteria.
Surgical techniques
All sleep surgeries were performed by a single surgeon under general anesthesia. If a tongue base procedure was planned, nasotracheal intubation was utilized.
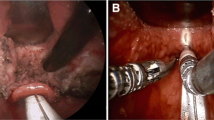
A McIvor mouth gag was applied to the open mouth and lateral pharyngoplasty was performed after bilateral tonsillectomy. In some cases, a surgical microscope was utilized to perform meticulous dissection in the initial attempt of lateral pharyngoplasty; now, a surgical loupe is used routinely for all lateral pharyngoplasty procedures. The upper portion of the anterior pillar, including part of the palatoglossus, was resected in a wedge shape to expose the entire tonsillar fossa (Figs. 1a, 2a). Then, we divided and undermined the superior and part of the middle pharyngeal constrictor muscle with tonsil forceps and a needle tip Bovie dissector (Figs. 1a, 2b). This creates two muscle flaps in the lateral pharyngeal wall (Figs. 1a, 2c). One flap is medially based and the other laterally based, as reported by Cahali et al. [2]. The dissection range is from the most upper pole of the tonsillar fossa superiorly to the lowest region of the tonsillar fossa where is near the inferior lingual root. During the dissection of the lateral pharyngeal wall (LPW), tonsillar arterial branches are often found and easily electrocauterized by bipolar bovie. Fat tissue in the parapharyngeal space was often observed, but not removed. Next, the two medial- and lateral-based muscle flaps were re-approximated in an overlapping technique to enhance the reinforcement of LPW (Fig. 1b). The two overlapping muscle flaps are sutured together with Vicryl 3-0 using a vertical mattress method (Fig. 2d–f). This is the surgical step that was modified from Cahali’s method [2] and the rationale for this modification is described below. Then, the palatopharyngeus is retracted supero-laterally and anteriorly with a suspension technique using Vicryl 3-0 sutures. The needle passes first through the superolateral point of the soft palate just near the second molar and comes out of the upper pole of the tonsillar fossa (Fig. 2g). Then, the palatopharyngeus muscle is tied up by the suture and the needle comes back through the upper pole to the initial starting point, very near the second molar and they are tied together (Fig. 1b, c). This enhances the expansion of the retropalatal area in both the anterior–posterior and lateral dimensions without the removal of soft palate. Finally, the upper portion of the posterior pillar is partially incised to release tension and the released posterior pillar was sutured to the anterior face of the soft palate to cover the denuded portion (Figs. 1d, 2h, i).
Illustration of the surgical steps of overlapping lateral pharyngoplasty. a The anterior pillar is partially resected in a wedge shape to expose the upper pole of the tonsillar fossa and the superior pharyngeal constrictor muscle is dissected and divided into medial- and lateral-based flaps. b The divided muscle flaps overlap and are closed with a modified vertical mattress suture from the upper to lower pole. c The palatopharyngeus is retracted supero-laterally and anteriorly with a suspension technique using Vicryl 3-0 suture. The redundant mucosa of the uvula is trimmed. d The upper portion of the posterior pillar is partially incised and the released posterior pillar is sutured to the anterior face of the soft palate to cover the denuded soft palate
Serial steps of the overlapping lateral pharyngoplasty surgical technique. a Bilateral markings for wedge resection of the anterior pillar. b, c Dissection and division of the superior constrictor muscle into medial- and lateral-based flaps. d–f Approximation and suture of the divided medial and lateral muscle flaps. g Lateral suspension suture of the palatopharyngeus. h Partial incision of the posterior pillar and trimmed soft palate. i Postoperative view after suturing the pillar and soft palate
Tongue base resection was performed with the Coblator II Surgery System (ArthroCare ENT, Sunnyvale, CA, USA). We have used this surgical technique when retroglossal obstruction was noted based on drug-induced sleep endoscopy and/or Muller’s maneuver. For coblator tongue base resection, an EVac 70 coblation wand (ArthroCare ENT) was used and a setting of coblation 9/coagulation 5 was applied in our procedure. A McIvor mouth gag was used to open a patient’s mouth and the 70′ rigid endoscope was positioned in the oral cavity facing upward to visualize the tongue base. Tongue base tissue was excised by moving the coblator wand in an anterior-to-posterior direction. We resected the bilateral lingual tonsils if they were observed and performed a midline partial glossectomy (Fig. 3). Postoperative tracheostomy was not required in all cases of tongue base resection.
Results
Profiles and comparison of the two surgical groups
Demographic data, including mean age, male to female ratio, preoperative BMI, neck circumference, waist–hip ratio, tonsil size, Mallampati stage, Friedman stage and preoperative AHI in all subjects are shown in Table 2. The mean age in the OLP and OLP + CobTBR groups was 36.1 ± 16.4 and 40.2 ± 10.7 years, respectively. Individuals in the OLP group had greater tonsil size compared with those in the OLP + CobTBR group, but this difference was not significantly different (t test, p = 0.387). Both the Mallampati stage and the Friedman stage were higher in the OLP + CobTBR group than in the OLP group, though not all levels reached statistical significance (t tests, p = 0.233, p = 0.055, respectively). The findings of the Muller maneuver were also calculated, and we used a modified VOTE classification, as suggested by Kezirian et al. [10], to score the degree and site of obstruction (Table 2). The scores of the velum, oropharynx, and epiglottis did not vary between the two groups, but the tongue base score was higher in the OLP + CobTBR group compared with the OLP group (p = 0.016). When performing the Muller maneuver with a nasopharyngoscope, we also checked for tongue base collapse while asking patients to relax with full expiration and an open mouth. Tongue base collapse was noted more frequently in the OLP + CobTBR group than in the OLP group (p = 0.032). Postoperative polysomnography was performed in both groups and their results are shown in Table 1.
Surgical outcomes in OLP and OLP with CobTBR groups
In the OLP group, 11 of 12 patients (91.7%) showed a surgical response. Mean AHI improved significantly from 36.3 ± 28.6 to 14.8 ± 17.9, a reduction of approximately 60%. Other parameters such as RDI, lowest O2 saturation, mean O2 saturation, oxygen desaturation index (ODI), supine AHI, and ESS also significantly improved after surgery (Table 3). According to Sher’s success criteria, 8 out of 12 patients achieved success (66.7%). The success rate among Friedman stages was as follows: stage 1 (n = 3); 100%, stage 2 (n = 7); 57.1%, stage 3 (n = 2); 50.0%. The success rate among the three different severity groups was as follows: mild group (n = 2), 100%; moderate group (n = 4), 50%; severe group (n = 6), 66.7%. According to the strict success criteria of an AHI below 10, the overall success rate was 41.7%.
In the OLP + CobTBR group, all patients showed improvement in AHI, and the surgical response rate was 100%. Mean AHI improved significantly from 38.8 ± 22.0 to 13.1 ± 14.1, a reduction of approximately 67%. Other parameters such as RDI, lowest O2 saturation, mean O2 saturation, ODI, supine AHI, and PSQI also significantly improved after surgery (Table 3). According to our surgical success criteria, 12 out of 17 patients achieved success and the overall success rate was 70.6%. The success rate among Friedman stages is as follows: stage 1 (n = 1), 100%; stage 2 (n = 8), 75.0%; stage 3 (n = 8), 62.5%. The success rate among the three different severity groups was as follows: mild group (n = 1), 100%; moderate group (n = 7), 57.1%; severe group (n = 9), 44.4%. According to the strict success criteria of AHI below 10, the overall success rate was 52.9%.
Surgical complications
To determine postoperative complications, we assessed bleeding, foreign body sensation (FBS), taste decrease (TD), and velopharyngeal insufficiency (VPI) in all patients who underwent OLP (n = 65). The symptoms of foreign body sensation, taste decrease, and velopharyngeal insufficiency were evaluated approximately 3 months after surgery. In the OLP group (n = 41), postoperative bleeding occurred in four cases (9.8%) and this bleeding stopped spontaneously in all cases without emergent surgery. FBS (n = 7; 17.1%), TD (n = 2; 4.9%), and VPI (n = 1; 2.4%) were observed. In the OLP + CobTBR group (n = 24), postoperative bleeding occurred in five cases (20.8%) and one case required emergent bleeder ligation surgery. FBS (n = 9; 37.5%) and TD (n = 5; 20.8%) were noted, but there were no complaints of VPI. Although FBS and TD in the OLP + CobTBR group were higher than in the OLP group, those symptoms were minor and gradually improved over time. Most patients also described these symptoms as minor complications and did not complain.
Discussion
Synopsis of new findings
Lateral pharyngoplasty is a remarkable technique first developed by Cahali MB [2, 3]. The surgical procedure consists of microdissection and sectioning of the superior pharyngeal constrictor muscle vertically within the tonsillar fossa and suturing the laterally based muscle flap to the same-side palatoglossus muscle with three separate stitches. In Cahali’s first report, after surgery, the median AHI decreased from 41.2 to 9.5 [2]. Lateral pharyngoplasty appears very promising, as it can increase the tension in the collapsible “pharyngeal tube,” including the tongue base. However, we encountered some cases that developed dehiscence of stitch in the laterally based muscle flap and same-side palatoglossus. Cahali MB also reported some wound dehiscence in the region of the caudal stitch after surgery [2]. There are two reasons for an easily dehiscent wound. First, SPC muscles lie obliquely and their muscle fibers are intermingled with each other. Therefore, suturing this muscle with the palatoglossus may make it vulnerable to tears by traction. Second, the palatoglossus may be an insufficient strut to support SPC, as the palatoglossus is a very thin muscle (its mean width was 3.2 ± 1.2 mm in Korean cadaveric study [5]) and it moves with the movement of the tongue and soft palate while swallowing food. Therefore, the weak palatoglossus may easily tear.
This is the primary reason why we reconsidered the procedure in detail and revised lateral pharyngoplasty. The main purpose of lateral pharyngoplasty is to increase the tension of the LPW by manipulating the pharyngeal muscles. We approximated the lateral- and medial-based muscle flaps by at least five stitches of vertical mattress suture, overlapping the two muscle flaps, instead of suturing the laterally based muscle flap and palatoglossus (Figs. 1b, 2d–f). With this modification, we aimed to augment the tension of the LPW more efficiently. We also focused on the palatopharyngeus muscle, because it is often very bulky among OSA patients. The palatopharyngeus is a flat muscle which emerges from the lateral pharyngeal wall and spreads into the soft palate [5]. We have noted that the remaining palatopharyngeus is still bulky, even after lateral pharyngoplasty, which may contribute to persistent pharyngeal collapse. We pulled it supero-laterally and performed anchoring sutures as described in the methods section. The anchoring suture technique results in expanding both the antero-posterior and lateral dimensions of pharyngeal lumen.
Strengths and limitations of the study
The surgical method of OLP combined with CobTBR appeared satisfactory among OSA patients with retroglossal obstruction. In our study, the combined procedure showed a 100% response rate and its overall success rate was 70.6% using Sher’s criteria, a rate that was higher than in the OLP group. Even in Friedman stages 2 or 3 and with severe OSA, the success rate in the OLP + CobTBR group was higher than compared with the OLP group. The LPW might be strengthened by OLP and the reduced volume of the tongue base may provide a reasonable surgical strategy for OSA. As previously reported [8], we also found that higher Friedman stages had lower success rates when Sher’s criteria were applied. However, strict success criteria (AHI below 10) showed a higher success rate in Friedman stage 3 than in stage 2.
This study has several limitations. First, the number of subjects enrolled in the study is lacking, and including more patients can elucidate different aspects of surgical outcomes. Second, we have not provided evidence that our OLP technique is better than the original LP technique. In this study, we hoped to introduce our concept of lateral pharyngoplasty and present its surgical outcomes with low postoperative complications. In addition, we were the first to report the surgical outcomes of lateral pharyngoplasty combined with coblator tongue base resection.
Conclusion
We modified the original LP technique by superimposing the anterior and posterior muscle flaps and anchoring sutures to the region of the upper second molar gingiva. Our overlapping LP technique appears to be safe and effective among OSA patients. The multi-level surgery of OLP combined with CobTBR can be a good surgical strategy for OSA patients with retroglossal obstruction. Moreover, these surgical methods can be considered for obese or elderly OSA patients with favorable prediction of surgical outcomes.
References
Babademez MA, Ciftci B, Acar B, Yurekli MF, Karabulut H, Yilmaz A, Karasen RM (2010) Low-temperature bipolar radiofrequency ablation (coblation) of the tongue base for supine-position-associated obstructive sleep apnea. ORL J Otorhinolaryngol Relat Spec 72(1):51–55
Cahali MB (2003) Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope 113(11):1961–1968
Cahali MB, Formigoni GG, Gebrim EM, Miziara ID (2004) Lateral pharyngoplasty versus uvulopalatopharyngoplasty: a clinical, polysomnographic and computed tomography measurement comparison. Sleep 27(5):942–950
Carrasco-Llatas M, Marcano-Acuna M, Zerpa-Zerpa V, Dalmau-Galofre J (2015) Surgical results of different palate techniques to treat oropharyngeal collapse. Eur Arch Otorhinolaryngol. https://doi.org/10.1007/s00405-015-3565-1
Cho JH, Kim JK, Lee HY, Yoon JH (2013) Surgical anatomy of human soft palate. Laryngoscope 123(11):2900–2904
Epstein LJ, Kristo D, Strollo PJ, Friedman N, Malhotra A, Patil SP, Ramar K, Rogers R, Schwab RJ, Weaver EM, Weinstein MD (2009) Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med 5(3):263–276
Friedman M, Hamilton C, Samuelson CG, Kelley K, Taylor D, Pearson-Chauhan K, Maley A, Taylor R, Venkatesan TK (2012) Transoral robotic glossectomy for the treatment of obstructive sleep apnea-hypopnea syndrome. Otolaryngol Head Neck Surg 146(5):854–862
Friedman M, Ibrahim H, Bass L (2002) Clinical staging for sleep-disordered breathing. Otolaryngol Head Neck Surg 127(1):13–21
Fujita S, Conway W, Zorick F, Roth T (1981) Surgical correction of anatomic azbnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 89(6):923–934
Kezirian EJ, Hohenhorst W, de Vries N (2011) Drug-induced sleep endoscopy: the VOTE classification. Eur Arch Otorhinolaryngol 268(8):1233–1236
Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, Boehlecke B, Brown TM, Coleman J Jr, Friedman L, Kapen S, Kapur VK, Kramer M, Lee-Chiong T, Owens J, Pancer JP, Swick TJ, Wise MS (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29(3):375–380
Lin HC, Friedman M, Chang HW, Gurpinar B (2008) The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope 118(5):902–908
Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR (2008) Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 31(8):1079–1085
Schellenberg JB, Maislin G, Schwab RJ (2000) Physical findings and the risk for obstructive sleep apnea. The importance of oropharyngeal structures. Am J Respir Crit Care Med 162(2 Pt 1):740–748
Schwab RJ, Gupta KB, Gefter WB, Metzger LJ, Hoffman EA, Pack AI (1995) Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. Am J Respir Crit Care Med 152(5 Pt 1):1673–1689
Schwab RJ, Pack AI, Gupta KB, Metzger LJ, Oh E, Getsy JE, Hoffman EA, Gefter WB (1996) Upper airway and soft tissue structural changes induced by CPAP in normal subjects. Am J Respir Crit Care Med 154(4 Pt 1):1106–1116
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19(2):156–177
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 5(2):173–178
Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, Greenberg H, Kader G, Mahowald M, Younger J, Pack AI (2007) Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep 30(6):711–719
Woodson BT, Feroah T, Connolly LA, Toohill RJ (1997) A method to evaluate upper airway mechanics following intervention in snorers. Am J Otolaryngol 18(5):306–314
Young T, Peppard PE, Gottlieb DJ (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165(9):1217–1239
Funding
This research was also supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2015R1D1A1A02062156).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no financial or personal conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 8 (WMV 39386 KB)
Rights and permissions
About this article
Cite this article
Park, DY., Chung, H.J., Park, S.C. et al. Surgical outcomes of overlapping lateral pharyngoplasty with or without coblator tongue base resection for obstructive sleep apnea. Eur Arch Otorhinolaryngol 275, 1189–1196 (2018). https://doi.org/10.1007/s00405-018-4940-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-4940-5