Abstract
In patients with a neck metastasis from an unknown primary with non-squamous cell cancer (non-SCC) histology, the primary is often located outside the head and neck area. We retrospectively evaluated 326 patient records and found 14 patients with non-SCC neck lymph node metastasis from an unknown primary undergoing whole body F-18-fluorodeoxyglucose (FDG) positron emission tomography (PET) with or without coregistered computed tomography (PET/CT). The PET or PET/CT findings were verified by pathological work-up, additional imaging tests, and clinical follow-up. PET detected pathological FDG uptake suspicious for the primary in eight patients. PET or PET/CT findings were true positive in seven patients, true negative in 4, false positive in 1, and false negative in two patients. In one patient PET/CT revealed a synchronous ovarian carcinoma. The results suggest that whole body imaging with FDG PET and PET/CT can be useful to identify unknown primaries of non-SCC origin. However, the work-up of patients undergoing PET or PET/CT in our study was very heterogeneous and the primary was more likely found in patients without extensive imaging before PET scanning. Further studies should evaluate if the histology of a neck nodal metastasis should influence the choice of the imaging method and the role of PET and PET/CT imaging for the work up of patients with a non-SCC neck lymph node metastasis of an unknown primary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recent reports suggest that positron emission tomography (PET) with F-18-fluorodeoxyglucose (FDG) can successfully be used for the identification of the primary site in patients with a neck lymph node metastasis from an unknown primary tumour [1–8]. The primary tumour is usually found in the upper aero-digestive tract. In patients with squamous cell cancer histology the primary is often located in the tonsils or in areas difficult to inspect clinically, such as the pyriform sinus or the nasopharynx [9, 10].
The primary can also be in the thorax and in the gastro-intestinal or urogenital tracts, if the histology of the cervical metastasis shows an adenocarcinoma [11]. The pathologic diagnosis of adenocarcinoma is usually based on the identification of glandular structures that are formed by the neoplastic cells. Poorly differentiated adenocarcinoma and poorly differentiated carcinoma can be seen as descriptions of the same spectrum of histologic appearance with carcinoma cells showing a lesser degree of glandular differentiation. However, a subset of patients with poorly differentiated adenocarcinoma may be distinctive in their tumour biology and responsiveness to systemic chemotherapy (Hainsworth and Greco, http://www.uptodate.com).
The biopsy material should be carefully evaluated and instead of material obtained by fine needle aspiration an adequate biopsy specimen is preferred. Histological work-up comprises immunohistochemical techniques to better describe the potential origin of the primary and can be complemented by electron microscopy, chromosome analysis, and gene micro array analysis.
Additionally, it has been suggested that involvement of supraclavicular and low cervical lymph nodes are suspicious for a primary in the chest or abdomen, and are associated with a poorer prognosis than lymph node metastases of the upper neck levels [12, 13]. As the search for the primary in patients with a neck metastasis of non-squamous cell cancer (non-SCC) histology should not be limited to the head and neck area, only, the use of whole body imaging for further work-up, such as FDG PET, seems beneficial. A previous study suggested a low clinical impact of FDG PET in patients undergoing extensive work-up with panendoscopy for a neck metastasis of squamous cell cancer histology before PET or PET/CT scanning [14]. This recent work stressed the importance of defining the work-up before PET scanning, since it is more likely to detect an unknown primary the less is done as routine clinical work-up.
In our hospital routine work-up of patients with a lymph node metastasis from a squamous cell carcinoma consists of a thorough physical examination including transnasal fibre-endoscopy of the nasal cavity, the nasopharynx, oropharynx, hypopharynx and larynx, contrast-enhanced high-resolution computed tomography (CT) or contrast-enhanced magnetic resonance imaging (MRI) of the neck, and chest X-ray in the postero-anterior and lateral views. Furthermore, patients undergo tonsillectomy of the ipsilateral side if no other primary tumour is detected during panendoscopy under general anaesthesia. Panendoscopy consist of rigid esophagoscopy, tracheobronchoscopy, hypopharyngoscopy, laryngoscopy and inspection and palpation of the oropharynx and oral cavity. The nasal cavity and the nasopharynx are assessed through transnasal rigid endoscopy with 0 and 30° endoscopes. Biopsies are only taken from suspicious mucosal areas and no random biopsies neither in the nasopharynx nor in the base of tongue are taken. Usually, PET or PET/CT is acquired after this extensive work-up when all other methods failed to find the primary.
In patients with a non-SCC histology the work-up is less standardized, but a similar work-up is done in most patients to evaluate the upper aero-digestive tract. CT of the chest and abdomen as well as clinical evaluation with pelvic examination in women and prostate evaluation in men is often performed, additionally. Procedures such as endoscopic gastrointestinal evaluation may complement the work-up. However, the role of PET and PET/CT is less defined in these patients.
Although recommendations exist how to evaluate patients with an unknown primary site of a metastasis from an adenocarcinoma or poorly differentiated neoplasm, no guideline exists on how to use the various imaging methods in a defined algorithm. Furthermore, the influence of the histology and the level of the lymph node metastasis in the neck on the choice of the imaging method is not well defined.
The purpose of this retrospective study was to evaluate the use of whole body PET and PET/CT to identify primaries outside the head and neck area in patients with a neck lymph node metastasis of non-SCC origin.
Patients and methods
The records of all patients undergoing FDG PET or PET/CT at the Division of Nuclear Medicine of the University Hospital Zurich between January 1999 and April 2006 were retrospectively reviewed. This review was done in accordance with the guidelines of the local ethics committee and for this retrospective analysis no informed signed consent of the patients was necessary. Only data of patients with cytologically/histologically proven cervical lymph node metastases of a non-SCC unknown primary was selected for this evaluation. The findings of the clinical evaluation and imaging including at least a chest X-ray was available in all patients. PET or PET/CT scanning was done in these patients as part of the work-up before or after imaging with morphological methods (ultrasound, CT, MRI) of the head and neck area, thorax, and abdomen. In all patients with additional CT and MRI studies these structural imaging tests were acquired using standard protocols with contrast enhancement.
Prior to PET or PET/CT scanning the patients fasted for at least 4 h. A standard activity of 370 MBq was injected intravenously approximately 60 min prior to the examination. All whole body PET and PET/CT scans were acquired in supine position in a 2D mode using an acquisition time of 4 min for the emission scan on a Advance PET scanner or a Discovery LS PET/CT device (both GE Medical Systems, Waukesha, WI, USA). For attenuation correction either the built-in transmission source was used on the PET only device or the CT data on the combined scanner. The CT scan was acquired with the built-in multislice detector CT scanner (140 kV, 40 mAs, pitch 6) and without intravenous contrast injection. The CT acquisition as well as PET images covered the whole body from the head to the pelvic floor. Images were reconstructed using a standard iterative algorithm (ordered subset expectation maximization algorithm, OSEM; 28 subsets, two iterative steps). The acquired images were viewed with software providing multiplanar reformatted images of PET alone or of PET, CT and fused data with linked cursors (eNtegra 3.0215; GE Medical Systems, Waukesha, USA).
In patients undergoing PET/CT scanning areas with increased FDG uptake guided the further search for pathologies visible on the CT scan. The non-contrast enhanced CT data of PET/CT scans were not separately evaluated. All PET and PET/CT images were re-evaluated by two experienced readers in consensus. They knew that the patients had neck lymph node metastasis of an unknown primary and were blinded for the results of other imaging tests.
In all patients with imaging findings suggesting a primary lesion, histological confirmation or cytological work-up was available. In patients without suspicious PET findings the clinical follow-up and the results of additional imaging tests served as the standard of reference.
Results
We evaluated the records of 326 consecutive patients examined for neck lymph node metastases of an unknown primary. Most patients underwent PET or PET/CT for a neck metastasis of an unknown primary cancer with squamous cell carcinoma histology. Only 14 patients (4.3%; 5 women and 9 men) with a mean age of 63.2 years (range 29–85 years) underwent PET or PET/CT for an unknown primary with non-SCC histology.
In all patients at least information on physical examination, chest X-ray, and results of fine needle biopsy/histology of the neck lymph node was available before scanning. The result of cytology or histology of the neck metastases was adenocarcinoma and undifferentiated adenocarcinoma (n = 9), undifferentiated carcinoma (n = 3), undifferentiated neuroendocrine tumour (n = 1) and low-grade sarcoma (n = 1) (Table 1).
There were six in-patients and eight out-patients undergoing PET or PET/CT scanning (Table 1). The six in-patients (patient 3, 4, 7, 12, 13, 14; Table 1) were send for scanning either from the Department of Otorhinolaryngology, Head and Neck Surgery (patient 3, 4, 12, 13), the Department of Dermatology (patient 7) or the Department of Internal Medicine (patient 14). CT/MRI of the head and neck area was available in 5 and CT of the thorax and/or abdomen or ultrasound of the abdomen in four patients before PET or PET/CT scanning. Histology was always available in our in-patients. However, the clinical and imaging work-up before sending the patient to PET or PET/CT differed largely between the referring physicians. In contrast, the diagnosis of a lymph node metastasis of non-SCC origin was based on fine needle aspiration in six out of eight out-patients (patient 1, 2, 6, 8, 9, 10; Table 1). In four of the eight out-patients a CT or MRI of the head and neck area was available and in three out-patients a CT of the thorax and/or abdomen or an ultrasound of the abdomen was done before PET or PET/CT scanning.
In patients 3, 6, 8, 9, and 11 lymph node involvement was described in areas below the level of the cricoid cartilage (Level IV and lower part of Level V including the supraclavicular area). In all other patients lymph nodes were identified in levels I through III and upper region of Level V.
PET suggested a primary tumour in eight patients (patient 1, 3, 4, 5, 6, 8, 10, 12; Table 1). An example of a patient with a lung tumour with positive PET/CT findings but first missed on conventional chest X-ray is shown in Fig. 1. In seven of eight examinations the PET findings were true positive and in one patient false positive (patient 6). All positive PET findings were confirmed by histology of the primary lesion, except in patient 3 where the final diagnosis of an adenocarcinoma in the left lung was based on the evaluation of pleural effusion. In patient 6 PET suggested an esophageal carcinoma, but endoscopy with biopsy revealed inflammatory changes with hyperkeratosis and no evidence of cancer. During a follow-up of 11 months the primary was not found in this patient, but additional metastases were identified.
Coronal maximum intensity projection (MIP) image and transverse PET, CT and coregistered PET/CT images of a 72-year-old male patient (patient 12) with a neck lymph node metastasis at the left Level II (short arrow). PET revealed intense FDG uptake in a primary (black and white arrowheads) in the right lung. Lymph node metastases are found in the mediastinum and an additional intrapulmonary metastasis in the right lower lobe (long arrow). The lung lesions were not identified on conventional chest X-ray acquired in posterior–anterior projection. The final diagnosis was adenocarcinoma of the lung. The black line indicates the level of the transverse sections
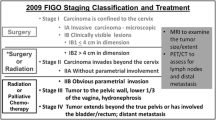
In four patients PET was true negative (patient 7, 9, 11, 13) and in two patients false negative (patient 2 and 14). In 6 patients (patient 2, 7, 9, 11, 13, 14) PET did not suspect a primary, although in-patient 13 a second primary was suggested. Both, the neck lymph node metastasis and the ovarian cancer were surgically resected. In this patient a secondary adenocarcinoma of the right ovary (FIGO IIIb) was found at PET/CT with a different histological appearance than the neck lymph node metastasis (Fig. 2). The primary was not identified during a 2 years clinical follow-up using additional imaging with CT of the neck, thorax and abdomen, as well as mammography and regular gynaecological controls, and PET/CT scanning (8 months after the first PET/CT scan). In patient 7, 9, and 11 the primary was not found during the follow-up of at least one year (as reported by the referring physician).
Coronal maximum intensity projection (MIP) image and transverse PET, CT and coregistered PET/CT images of a 48-year-old female patient (patient 13) with a neck lymph node metastasis (2.5 cm) at Level II under the strenocleidomastoid muscle. PET revealed low to moderate FDG uptake in the lymph node, which was enlarged on CT images (black and white arrowheads). A second lesion with low to moderate FDG uptake is visible adjacent to the bladder corresponding to an enlarged ovary on CT images (black and white arrows). The final diagnosis was an adenocarcinoma of the ovary (FIGO IIIb) as an incidental synchronous tumour, but the primary responsible for the lymph node metastasis was not found during 2 years of clinical follow-up and additional PET/CT scanning (after 8 months). The transverse sections are done at the level of the arrow/arrowhead
Based on these numbers the sensitivity, specificity, and accuracy of PET was 77.8, 80.0, and 78.6%. The positive and negative predictive values were 87.5 and 66.7%, respectively.
Discussion
The results of this study confirm previous observations that PET with FDG is able to identify the primary tumour in patients with a neck lymph node metastasis [1–8]. In this study FDG PET and PET/CT had a moderate sensitivity and specificity of 77.8 and 80.0%. The whole body imaging approach used in our patients allowed for the identification of five malignancies located in the chest and one incidentally found secondary gynaecological tumour. These results support the view that patients with non-SCC histology and neck lymph node involvement have a relatively high probability of a primary in the chest or abdomen. Therefore, we suggest to acquire PET and PET/CT scans using a whole body imaging protocol.
The histology of the primary may influence FDG uptake and the visibility of a lesion on PET images. FDG uptake was very variable as shown for example in-patient 12 with an adenocarcinoma of the lung and a very intense uptake (Fig. 1) and in patient 13 with only low to moderate uptake in an ovarian adenocarcinoma (Fig. 2). In all patients with adenocarcinoma of the lung (patient 3, 4, 8, 12) the primary was seen with PET. Furthermore, PET detected a small cell lung cancer (patient 5; histology of a low differentiated neuroendocrine carcinoma). Schumacher et al. [15] suggested FDG PET to be of potential use as a simplified staging tool for small cell lung cancer. In another patient with metastasis from an adenocarcinoma (patient 6), PET did not detect the primary but was false positive due to oesophageal inflammatory changes with hyperkeratosis. It is well known that inflammatory cells in acute and chronic inflammation take up FDG.
In four patients the primary was identified in the head and neck area (patient 1, 2, 10, 14). In two of these patients the primary was located in the salivary glands. In a recent work it has been shown that FDG PET can have a positive impact on the management of patients with salivary gland malignancy at staging and in the restaging situation [16]. In one patient a primary sarcoma originating from the nerve sheath (patient 10) was easily identified. It has previously been shown that sarcomas of the head and neck usually have a high FDG uptake [17, 18]. However, in patient 2 a superficially spreading melanoma of the skin of the scalp was not detected, although melanoma regularly shows high FDG uptake. This is because a small and superficial lesion can easily be missed due to the limited resolution of the scanner. In this patient the fine needle aspiration biopsy of the lymph node revealed an undifferentiated carcinoma and only the histological work-up after surgical excision of the whole lymph node with immuno-histochemical staining of the cells indicated the presence of melanoma. This case underlines the importance of obtaining high quality specimens for analysis since the interpretation of cells obtained by fine needle aspiration may be more difficult.
All patients with primaries within the head and neck area had their lymph node metastasis above the level of the cricoid. In contrast, only two of the five lung cancers metastasised to a neck lymph node below this level. In Europe it is widely spread praxis that especially in patients with lymph node involvement below the cricoid level a CT scan of the lung and mediastinum should be obtained. This was done for example in patient 3 before PET imaging, but interestingly, the in-patients number 4, 12, and 13 had neck lymph nodes involved above this level an did not undergo CT of the thorax. In two of them this would clearly have allowed the identification of the primary lung tumour, thus avoiding the need of additional PET imaging. Chest X-ray alone is not as sensitive as CT scanning to identify small lung lesions and peribronchial tumours at the hilar level. Therefore, the praxis to only admit patients to CT scanning when lymph node metastases are found below the cricoid level has to be reconsidered, especially when non-SCC histology has been found.
The small patient group and the inconsistent imaging work-up before PET or PET/CT scanning are major drawbacks of our retrospective analysis. It clearly shows that an algorithm is needed to define the use of imaging tests during the clinical work-up of patients with cervical non-SCC metastasis of an unknown primary. The pre-PET evaluation of our patients varied widely between in- and out-patients and in the in-patients referred from different departments.
On the other hand FDG PET or PET/CT could serve as a screening test to assess the whole body in patients with a suggested FDG avid histological type of the neck lymph node metastasis. A positive PET result could guide further diagnostic evaluation of the patient. However, to date the role of PET or PET/CT early in the work-up of patients with a neck lymph node metastasis of an unknown non-SCC primary is not clear. As an alternative approach contrast enhanced computed tomography of the head and neck area, thorax and abdomen is done in many centres for whole body staging of patients with suspected malignant disease. The role of MRI is less well defined than CT and MRI is mainly used for the work-up of the head and neck area. In patient 14 a small adenocarcinoma of the parotid gland was not detected with CT and PET/CT imaging, but intra-operatively found when removing further lymph nodes adjacent to the parotid gland. This underlines to use MRI with its well-known high soft tissue contrast to evaluate the head and neck area. Furthermore, it is well possible that this lesion would have been identified with ultrasound. However, structural imaging of the head and neck area is not only used for staging purposes but also is needed for correct treatment planning.
Our results question the use of chest X-rays in these patients for staging purposes and detection of an unknown primary. Additionally, it has previously been suggested that screening imaging tests such as ultrasound of the abdomen or whole body skeletal scintigraphy have only a minor impact on identifying distant metastases in patients with a cancer in the head and neck area [19]. In contrast, whole body FDG PET or PET/CT can add relevant information in patients undergoing staging with squamous cell carcinoma of the head and neck. Additional suspicious lesions such as distant metastases and secondary synchronous carcinomas can be detected with PET/CT underlining the impact of whole body imaging in patients with a pathology in the head and neck area, although false positive findings may decrease the performance of this imaging test [20].
In patients with a lymph node metastasis from a non-SCC unknown primary, FDG PET and PET/CT is preferably acquired as a whole body imaging method. Most of the primaries in our patients were located in the thorax and head and neck area. Therefore, a scrutinized work-up of the head and neck area and thorax using morphological imaging methods is to be recommended in all patients with non-SCC histology of the lymph node metastasis even when the involved lymph node is located in a neck level above the cricoid. The information on histology could influence the choice of the imaging methods used for patient work-up. However, it remains to be clarified if PET could serve as a cost-effective first line method for whole body imaging of patients with a non-SCC neck lymph node metastasis of an unknown primary. Prospective studies in large patient groups are needed to define the role of PET and PET/CT imaging as part of the work up such patients.
References
Fogarty GB, Peters LJ, Stewart J, Scott C, Rischin D, Hicks RJ (2003) The usefulness of fluorine 18-labelled deoxyglucose positron emission tomography in the investigation of patients with cervical lymphadenopathy from an unknown primary tumor. Head Neck 25(2):138–145
Regelink G, Brouwer J, de Bree R et al (2002) Detection of unknown primary tumours and distant metastases in patients with cervical metastases: value of FDG–PET versus conventional modalities. Eur J Nucl Med Mol Imaging 29(8):1024–1030
Jungehulsing M, Scheidhauer K, Pietrzyk U, Eckel H, Schicha H (1999) Detection of unknown primary cancer with fluor-deoxy-glucose positron emission tomography. Ann Otol Rhinol Laryngol 108(6):623–626
Safa AA, Tran LM, Rege S et al (1999) The role of positron emission tomography in occult primary head and neck cancers. Cancer J Sci Am 5(4):214–218
Bohuslavizki KH, Klutmann S, Kroger S et al (2000) FDG PET detection of unknown primary tumors. J Nucl Med 41(5):816–822
Lassen U, Daugaard G, Eigtved A, Damgaard K, Friberg L (1999) 18F-FDG whole body positron emission tomography (PET) in patients with unknown primary tumours (UPT). Eur J Cancer 35(7):1076–1082
Braams JW, Pruim J, Kole AC et al (1997) Detection of unknown primary head and neck tumors by positron emission tomography. Int J Oral Maxillofac Surg 26(2):112–115
Mendenhall WM, Mancuso AA, Amdur RJ, Stringer SP, Villaret DB, Cassisi NJ (2001) Squamous cell carcinoma metastatic to the neck from an unknown head and neck primary site. Am J Otolaryngol 22(4):261–267
Mendenhall WM, Mancuso AA, Parsons JT, Stringer SP, Cassisi NJ (1998) Diagnostic evaluation of squamous cell carcinoma metastatic to cervical lymph nodes from an unknown head and neck primary site. Head Neck 20(8):739–744
Jones AS, Phillips DE, Helliwell TR, Roland NJ (1993) Occult node metastases in head and neck squamous carcinoma. Eur Arch Otorhinolaryngol 250(8):446–449
Wang RC, Goepfert H, Barber AE, Wolf P (1990) Unknown primary squamous cell carcinoma metastatic to the neck. Arch Otolaryngol Head Neck Surg 116(12):1388–1393
Hainsworth JD, Greco FA (1993) Treatment of patients with cancer of an unknown primary site. N Engl J Med 329(4):257–263
Kirschner MJ, Fietkau R, Waldfahrer F, Iro H, Sauer R (1997) Therapy pf cervical lymph node metastases of unknown primary tumor. Strahlenther Onkol 173(7):362–368
Stoeckli SJ, Mosna-Firlejczyk K, Goerres GW (2003) Lymph node metastasis of squamous cell carcinoma from an unknown primary: impact of positron emission tomography. Eur J Nucl Med Mol Imaging 30(3):411–416
Schumacher T, Brink I, Mix M et al (2001) FDG–PET imaging for the staging and follow-up of small cell lung cancer. Eur J Nucl Med 28(4):483–488
Otsuka H, Graham MM, Kogame M, Nishitani H (2005) The impact of FDG–PET in the management of patients with salivary gland malignancy. Ann Nucl Med 19(8):691–694
Hujala K, Martikainen P, Minn H, Grenman R (1993) Malignant nerve sheath tumors of the head and neck: four case studies and review of the literature. Eur Arch Otorhinolaryngol 250(7):379–382
Ferner RE, Lucas JD, O’Doherty MJ et al (2000) Evaluation of (18)fluorodeoxyglucose positron emission tomography ((18)FDG PET) in the detection of malignant peripheral nerve sheath tumours arising from within plexiform neurofibromas in neurofibromatosis 1. J Neurol Neurosurg Psychiatr 68(3):353–357
Lybak S, Olofsson J (2005) Ultrasound of the abdomen and total bone scintigraphy in patients with cancer of the head and neck. Eur Arch Otorhinolaryngol 262(11):887–889
Goerres GW, Schmid DT, Gratz KW, von Schulthess GK, Eyrich GK (2003) Impact of whole body positron emission tomography on initial staging and therapy in patients with squamous cell carcinoma of the oral cavity. Oral Oncol 39(6):547–551
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Paul, S.A.M., Stoeckli, S.J., von Schulthess, G.K. et al. FDG PET and PET/CT for the detection of the primary tumour in patients with cervical non-squamous cell carcinoma metastasis of an unknown primary. Eur Arch Otorhinolaryngol 264, 189–195 (2007). https://doi.org/10.1007/s00405-006-0177-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-006-0177-9