Abstract
In this prospective study, the patients with head and neck cancer admitted to the Department of Otolaryngology and Head and Neck Surgery, Haukeland University Hospital, underwent examination with ultrasound of the abdomen (112 patients) and total bone scintigraphy (118 patients) in the primary staging of the disease and before the start of treatment. In only one patient did we find metastases of head and neck cancer in the liver by these additional investigations, and one patient was found to have bone metastases. No second primary cancers were found by these extra examinations. One patient was found to have an asymptomatic aorta aneurysm and was in need of urgent surgical treatment. Based on these findings, we nowadays only use ultrasound of the abdomen and total bone scintigraphy as part of the general examination of new head and neck patients in selected cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the preliminary evaluation of patients presenting with cancer of the head and neck region, there are several cancer-related factors to consider. Firstly, the tendency to metastasize. Cancers of the head and neck tend to metastasize first to the regional lymph nodes in the neck. Distant metastases are most frequently found in the lungs, and thereafter in order of frequency in the skeleton and liver [1, 2]. Most studies of distant metastases are based on follow-up studies or autopsy material. The incidence reported in the literature varies from 5.3–23% [3, 4] in clinical studies, and 17–46.7% in autopsy reports [5, 6].
Secondly, cancers of the head and neck are associated with a high frequency of second primary cancers (3–16%) [2]. The synchronous second primary carcinomas found in this group of patients in our department after evaluation with clinical examination, CT scanning of the primary cancer and neck, chest X-rays, esophagoscopy, bronchoscopy and examination under general anesthesia, are approximately 4% (unpublished data). Second primary cancers in organs not examined with the above-mentioned examinations, and not known at the time of diagnosis of the cancer of the head and neck, have not been well documented numerically, since most centers have no routine examinations of other organs in their pretreatment evaluation. Thirdly, other diseases not directly related to the head and neck might require treatment or may have an impact when deciding the type and timing of the treatment of the head and neck cancer.
All patients with a cancer of the head and neck are examined with physical examination and radiological examination of the primary cancer location and of the neck and lungs. Most centers do an additional endoscopic examination with esophagoscopy and broncoscopy at least in all patients with squamous carcinomas. In the study period we included investigations with ultrasound of the abdomen and total bone scintigraphy to find out the potential benefits of these additional examinations.
Materials and methods
This study was planned as a prospective clinical study. Over a period of 16 months, all patients admitted to our department with a cancer in the head and neck region were routinely examined with ultrasound of the abdomen and total body skeleton scintigraphy. Approximately 80% of the patients had squamous cell carcinomas.
All examinations were carried out on a routine basis, where the ultrasound of the abdomen and the bone scintigraphy were ordered in a normal clinical setting. No special staff other than what normally would have been assigned to the examinations was set to carry out the ultrasound and the bone scintigraphy. By ordering these examinations in a normal clinical setting, we wanted to avoid the heightened attention that could result if the examiners knew that the result would be used in a study. The results therefore should be close to what we could expect as a normal clinical routine. Bone scintigraphy was done as a whole body scan with 99m Tc-555 M Bq. All patients were followed at our clinic after treatment.
Results
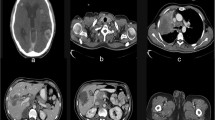
Bone scintigraphy was performed in 118 patients in whom 33 pathological results were found: 16 in the columna, 9 in the costae, 5 at the primary site, 2 in the kidney, 1 in the humerus and 1 with a metastasis. All patients with pathological uptake in the costae, humerus or columna were further evaluated with computerized tomography (CT). Only one patient of a total of 33 patients with pathological uptake was diagnosed as having metastases.
The metastases were found in a patient with a well-differentiated squamous cell cancer of the tonsillar pillar. Unfortunately, this patient died before further investigations of the metastases had been carried out. The death was due to a heart attack. The extensive skeleton metastases in the pelvic region could also have been from an undiagnosed prostate cancer. Postmortem examination of this patient was not permitted by the family. No other metastases were found in this patient at the time of primary evaluation.
Ultrasound of the abdomen was performed in 112 patients. In 43 patients, pathological results were recorded: cysts in the kidney (9), cysts in the liver (9), cholelithiasis (8), aneurysms of the aorta (6), hemangimoas in the liver (4), hydronephrosis (3), cysts in the pancreas (2), adrenal gland pathology (1), ascites (1) and metastasis (1).
Simple cysts of the kidney and the liver, as well as cholelithiasis, are in most cases adequately diagnosed by ultrasound alone and are accidental findings, which seldom require further diagnostic workup or treatment. The cysts in the pancreas were surgically treated after the treatment of the head and neck carcinoma. Of the six aneurysms of the aorta, only one was previously known. One of the aneurysms was urgently operated on, and in that respect took priority over the cancer treatment.
Hemangiomas of the liver can to some extent mimic metastases, and in our four patients, further workup was done with CT and/or ultrasound-guided fine-needle aspiration cytology (US-FNAC). The three patients with hydronephrosis were all found to have normal blood creatinin levels and were referred to a nephrologist for evaluation after having finished the treatment of the head and neck cancer.
The patient with adrenal gland pathology was examined with CT and US-FNAC and has been followed with repeated CT after ending treatment for his head and neck cancer. An exact pathological diagnosis has never been established, but metastases were excluded as a differential diagnosis. The ascites found in one patient were due to heart failure and did not have any consequence for the choice of treatment.
The only metastases found by the ultrasound of the abdomen in our study were in a patient with a low differentiated cancer of the ethmoidal region. The liver metastases found in this patient were not known at the time of the ultrasound. Blood samples taken a week after the ultrasound did, however, show elevated liver enzyme levels. No other metastases were found in this patient at the time of primary evaluation.
One of the patients with negative ultrasound of the abdomen died 3 months after the primary examinations. At the time of death, we found multiple liver metastases of considerable size. No second primary cancers were found with the ultrasound of the abdomen in our study.
Discussion
The primary intention of the more extensive pretreatment evaluation of our head and neck carcinoma patients was to detect possible distant metastases and second primary carcinomas. The distant metastases found with these additional investigations were only one patient with liver metastases and one patient with bone metastases. The liver metastases in our patient could have been detected by following up on pathological blood samples in this patient. Troell et al. [7] found two patients with liver metastases, but elevated liver function tests in only one of the two patients. Seventeen patients in their study had elevated liver function tests. Sensitivity of only 50% is too low for a clinical setting. We feel that doing ultrasound of the liver only in patients with elevated liver function tests is not sensitive enough for a screening test. Pooling our study with that of Troell et al. [7] and that of Dost et al. [8] gives six cases of liver metastasis in 576 patients, an incidence of about 1%.
One patient in our study with a normal ultrasound of the liver and normal liver enzymes in the primary cancer investigations turned up with extensive liver metastases in the liver 3 months after these preliminary investigations. The micrometastases in the liver that most likely were present at the time of the preliminary investigations were too small to be detected. The short time window between the negative primary investigation and the later detection of large and symptomatic liver metastases in this patient indicate further shortcomings with this investigation.
The bone metastases found in one patient in our study, could originate from a second primary cancer (most likely prostate cancer). Prostate cancer with metastases can be expected to give increased levels of prostate-specific antigen (PSA). We use PSA routinely on all male cancer patients admitted to our department, but unfortunately, this patient died of a heart attack before this test had been carried out.
Bone metastases could in some cases give elevated levels of alkaline phosphatase, but Troell et al. [7] found a sensitivity of only 20% when testing for bone metastases by alkaline phosphatase, making the clinical use of alkaline phosphatase a screening test of limited value. Bone scintigraphy is to date the best clinical screening test of bone metastases. We found one case of bone metastases in our study of 118 patients. Dost et al. found one patient with bone metastases in their study of 360 patients, while Troell et al. found as many as 5 patients in their study of 97 patients. Brown and Leakos reported a change in treatment in 3 out of 172 patients undergoing bone scan in a metastatic survey of patients with head and neck cancer [7, 8, 9]. If we pool these investigations together, we find at the time of primary diagnosis an incidence of bone metastases in head and neck cancer patients of 1.3% based on a total of 575 patients.
The consequence of detecting liver and bone metastases in our head and neck patients is not to increase survival, since these distant metastases, as a rule, are indications of noncurable disease. The advantage in finding these distant metastases is mainly to avoid extensive loco-regional treatment and to have to shift attention to palliative treatment.
The finding and treatment of a nearly rupturing aortic aneurysm in one patient had direct influence on the survival of this patient as she did not have any clinical symptoms. For a number of other patients, these additional findings only led to a number of further investigations and a prolonged stay in the hospital.
The exact cost of an ultrasound of the abdomen and bone scintigraphy is difficult to define in our public health system. In addition to the direct cost of the ultrasound and the bone scinitrgraphy, we have to add the cost of all further investigations we had to carry out to assess the true pathological significance of these findings and the prolonged stay in the hospital for some of these patients.
In summation, by adding ultrasound of the abdomen and bone scintigraphy in the general pretreatment evaluation of our head and neck carcinoma patients, we have found only two patients with distant metastases that would not have been detected without the two additional investigations. In addition, we found one case of disease not related to cancer that needed urgent treatment.
We have stopped the routine use of ultrasound of the abdomen and bone scintigraphy in our head and neck carcinoma patients, even if the results greatly changed the treatment in three patients (almost 3% of the patients). These investigations will only be carried out on those patients where we find a specific indication for such investigations. Such specific indications are not well defined. There are no other routine screening examinations that can fully replace ultrasound of the abdomen and bone scintigraphy in the clinical setting. The value of PET-scanning for routine metastatic survey is still being evaluated due to the limited access or absence of this examination in most centers [10]. The cost-efficacy of this examination has also to be been taken into account. Moreover, we have no clear indication from our study or from the literature concerning which subgroup of head and neck carcinoma patients would be at a higher risk of developing liver and bone metastases. A suggestion is that ultrasound of the abdomen and bone scintigraphy should be used in patients with clinical findings or symptoms indicating distant metastases, in patients with metastases in the lungs, in patients with extensive neck metastases, in patients with pathological liver function tests and in patients with poorly differentiated tumors or who are borderline cases for major surgery.
References
Merino OR, Lindberg RD, Fletcher GH (1977) An analysis of distant metastases from squamous cell carcinoma of the upper respiratory and digestive tracts. Cancer 40:145–151
Abramson AL, Parisier SC, Zamansky MJ, Sulka M (1971) Distant metastases from carcinoma of the larynx. Laryngoscope 81:1503–1511
Berger DS, Fletcher GH (1971) Distant metastasis following local control of squamous cell carcinoma of the nasopharynx, tonsillar fossa and base of tongue. Radiology 100:141–143
Castigliano SG, Rominger CJ (1954) Distant metastasis from carcinoma of the oral cavity. Am J Roentgenol 71:997–1006
O’Brian PH, Carlson R, Steubner EA, Staley CT (1971) Distant metastases in epidermoid cell carcinoma of the head and neck. Cancer 27:304–307
Peltier LF, Thomas LB, Crawford TH, Barclay MB, Kremer AJ (1951) The incidence of distant metastases among patients dying with head and neck cancers. Surgery 30:827–833
Troell RJ, Terris DJ (1995) Detection of metastasis from head and neck cancer. Laryngoscope 105:247–250
Dost P, Schrader M, Talanow D (1994) Nutzen der Abdomensonographie und der Skelettzintigraphie bei der TNM-Eintellung von Tumoren im Knopf-Hals-Bereich. HNO 42:418–421
Brown D, Leakos M (1998) The value of a routine bone scan in a metastatic survey. J Otolaryngol 27:187–189
Keyes JW, Chen MYM, Watson NE, Greven KM, McGuirt WF, Williams DW (2000) FDG PET evaluation of head and neck cancer: value of imaging the thorax. Head Neck 22:105–110
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lybak, S., Olofsson, J. Ultrasound of the abdomen and total bone scintigraphy in patients with cancer of the head and neck. Eur Arch Otorhinolaryngol 262, 887–889 (2005). https://doi.org/10.1007/s00405-004-0815-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-004-0815-z