Abstract
Purpose
Excessive femoral internal torsion is an important risk factor for patellar dislocation. The aim of the present study was to estimate the effect of derotational osteotomy of the femur on the tibial tubercle trochlear groove (TTTG) distance or patellar tilt angle (PTA) and to report our clinical outcomes of recurrent patellar dislocation after femoral derotation osteotomy.
Methods
A retrospective analysis of 16 patients (17 knees) with recurrent patellar dislocation treated by femoral derotation osteotomy in our department from January 2016 to February 2019 was carried out. The procedure was performed with supracondylar femoral derotation. A few procedures were combined with soft tissue procedures. Knee function was evaluated by using the International Knee Documentation Committee (IKDC) score, Kujala score, Lysholm score, visual analog scale (VAS) score and patient satisfaction. Additionally, CT was used to assess the influence of femoral derotational osteotomy on TTTG distance and PTA.
Results
The average femoral antetorsion angle before surgery was 33° (SD ± 5°), and the intraoperative correction angle was 23° (SD ± 4°). A total of 17 femoral derotation osteotomies in 16 patients with patellar instability [11 females, 5 males, aged 20.8 (range 15–41) years] were included in the study. No dislocation occurred within 26.5 months after follow-up (range 12–49 months). The IKDC score, Kujala score, Lysholm score and VAS score significantly improved. The preoperative TTTG distance was 15.63 mm (SD ± 2.07 mm), and it was 14.69 mm (SD ± 1.78 mm) at the follow-up. The PTA decreased from 26.35° (SD ± 6.86°) to 11.65° (SD ± 2.85°). The powers of TTTG and PTA measurements are 0.78 and 1.00, respectively and all of these differences were statistically significant.
Conclusions
Derotational osteotomy of the femur for the treatment of recurrent patellar dislocation can achieve good clinical results, including improved TTTG distance and PTA and improved knee function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the clinical work of orthopedic surgeons, patellofemoral problems are considered to be one of the most common diseases, with the highest incidence observed in adolescents and active young adults. Increased femoral internal torsion is a known risk factor for patellofemoral dislocation. Some studies [8, 10, 13] have found that patients with anterior knee pain or patellofemoral joint instability often have greater femoral internal torsion than healthy controls, and femoral derotation osteotomy is recommended as a treatment in cases of increased femoral antetorsion [13]. However, increased femoral internal torsion are often not detected in time; therefore, dislocation of the patella cannot be effectively treated [1, 14]. Derotation osteotomy for the treatment of patellar dislocation requires a combination of clinical symptoms and detailed physical examination as well as a comprehensive multijoint radiological assessment.
In the normal adult population, the range of femoral internal torsion is generally between 5° and 15°. Nelitz et al. reported the angle of femoral internal torsion is greater than 25° is considered a risk factor for patellar instability and recommended that the goal of the operation was to correct the excessive femoral internal torsion to 15° [16]. However, increased femoral internal torsion is common in children, but most cases can correct themselves as the skeletal system grows and develops, and surgery correction may be needed if excessive femoral internal torsion continues into adolescence > 25° to 30° [17]. Furthermore, this femoral deformity can cause many clinical manifestations, including anterior knee pain, patellar dislocation or subluxations, and abnormal gait [17, 19, 24, 25]. Previous studies have reported that derotational osteotomy of the femur has a good patient subjective effect for the treatment of patellar instability, and neglecting the treatment of patellar dislocation with torsional deformity of the femur will greatly affect the outcomes of other treatments [7, 11, 17]. However, few studies have objectively assessed patellofemoral alignment via imaging.
Our research objectives were as follows: (1) to estimate the effect of femoral derotational osteotomy on the TTTG distance and patellar tilt angle (PTA); (2) to report on the improvement of knee function and the degree of pain after derotational osteotomy in the distal femur; and (3) to assess the effect of the TTTG distance on clinical outcomes and after surgery by grouping.
Materials and methods
Patients
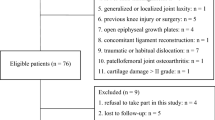
In our study, 17 femoral derotation osteotomies in 16 patients with patellar instability [11 females, 5 males, aged 20.8 (range 15–41) years], performed from January 2016 to February 2019 were included (Table 1). One of the patients underwent bilateral knee surgery within 2 years. For patients with patellofemoral instability, we performed a detailed clinical examination and continuous CT scans of the hip, knee, and ankle and measured the PTA and the TTTG distance on axial CT.
The following inclusion criteria were defined for this study:
-
1.
Excessive femoral internal torsion (≥ 25°) and
-
2.
Physiologic trochlea and Dejour type A or B trochlear dysplasia [6] and
-
3.
Patellar dislocations (≥ 2 times).
No patient had previously undergone orthopedic surgery. We also performed a comprehensive assessment of all other causes of anterior knee pain in all patients, including but not limited to lower extremity torsion deformities, neuropsychiatric systems, and hip, knee, and ankle joint arthropathy. The minimum follow-up time was 12 months.
The exclusion criteria were open epiphysis, lower extremity deformities after trauma, joint replacement of the lower limbs, severe knee valgus or varus (> 5°) deformities and severe trochlear dysplasia including Dejour type C and D dysplasia. Moreover, tibial torsional deformity was also excluded.
Clinical imaging investigation
In all patients, the degree of damage to soft tissue around the patella was assessed by magnetic resonance imaging (MRI) prior to surgery. Preoperative knee X-ray examinations included a full-length anteroposterior view of the lower extremity with weight-bearing and a lateral view of the knee with 45° of flexion to evaluate lower extremity malalignment and the patella alta. CT images were taken of the hips, knees, and ankles preoperatively, and femoral internal torsion was determined by the techniques described by Waidelich et al. [29] femoral internal torsion was defined as the angle between two lines, one of which was the line connecting the center of an ellipse around the greater trochanter on one slice and the center of the femoral head on another slice. The other line was a line tangent to the posterior condyles on an axial image. The TTTG distance and PTA were also measured on axial CT scans in all patients. The TTTG distance was measured between two parallel lines perpendicular to the posterior condylar tangents: one line passed the foremost point of the tibial tubercle, and the other line passed the deepest point of the trochlear groove [6]. The PTA was defined as the angle between the line tangent to the posterior femoral condyles and the longest axis of the patella on a transverse image [13]. CT scans of the knee and hip joints and radiographic examinations of the knee joint including anteroposterior and lateral views were performed postoperatively.
For subjective scores, the Kujala Score [5], the IKDC score, the Lysholm score and VAS score were determined at the most recent postoperative follow-up and compared with preoperative records. Changes in the above scores reflect improvement or worsening of knee function and pain. Patient satisfaction after the surgery was carefully evaluated by asking the patients if they were satisfied, and the results were divided into very satisfied, satisfied, partially satisfied, or dissatisfied. All the postoperative clinical assessments compared with preoperative assessments were collected at last follow-up. Furthermore, Studies reported that TTTG > 20 mm was often considered as a cause of patellar dislocation, we set up two groups of all patients (TTTG > 20 mm in group A, TTTG ≤ 20 mm in group B) to assess the influence of TTTG on PTA and knee function.
The review and measurement of the above data information were done independently by two of us. In order to solve the disagreements or inconsistencies of the data collection, there would be a third author involved in the discussion and resolution.
Surgery
Patients typically suffered from patellar dislocation in both limbs. Considering the safety of the operation and the time of postoperative recovery, we chose to have surgery on a more painful leg. All patients underwent arthroscopy to evaluate the cartilage and patellar tracking before the torsional osteotomy and to remove abnormal synovial tissue from the knee joint if necessary.
For torsional correction, the osteotomy level was determined by drilling two Kirschner wires (a) perpendicular to the mechanical axis of the lower extremity on the femur. The intraoperative torsion angle was controlled by using two other Kirschner wires that were parallel (b) to each other and placed at the ends of the osteotomy level, and the femur was fixed with a Tomofix distal femoral plate (DePuy Synthes, Umkirch, Germany) with 10 screws after osteotomy. According to the patellar tracking and patellar glide test after temporary fixation of the joint capsule, intraarticular pathologies were treated with medial retinaculum reefing or MPFL reconstruction after the osteotomy. We chose MPFL reconstruction in the case where the medial patellofemoral ligament had been ruptured on the MRI image, otherwise we chose strengthening sutures of the medial retinaculum (Fig. 1).
An intraoperative photograph of femoral derotational osteotomy (A); the osteotomy level was determined by two K wires (a). The derotational angle was controlled by another two K wires (b). Double bundle MPFL reconstruction (B): the MPFL insertion position on the femoral side is located behind the midpoint of the adductor tubercle and epicondylus medialis femoris. The insertion site of the patellar side is located at the midpoint of the inner edge of the patella and at a distance of about 7 mm from the upper pole of patella, respectively. Medial retinaculum reefing (C). Tighten the two sides of the incision on the medial retinaculum
On the second day after surgery, the patients could walk on the ground under partial load bearing (30 kg) with knee orthoses and double crutches and were recommended to perform quadriceps exercises, and knee flexion angle to reach 90° in the first week and reach normal angle 3 months after surgery. Patients can give up crutches and orthoses 3 months after surgery.
Statistical analysis
At least 17 cases per group were needed to reach an effect size of 0.5, a power of 0.8, and an alpha of 0.05 using G*power v.3.1 (G*power, Dusseldorf, Germany). Statistical analysis was performed with SPSS 23.0 (SPSS Inc. Chicago, IL, USA). All the parametric data were analyzed by paired Student’s t test. Numeric data are shown as the mean ± standard deviation. A P value less than 0.05 was considered statistically significant. And G*power was used to do a power analysis for the TTTG and PTA measurements.
Results
The average follow-up time of this study was 26.5 (range 12–49) months. The follow-up examinations involved the imaging studies and functional scores mentioned above.
Angle of femoral internal torsion
The preoperative femoral internal torsion angle was 33° (SD ± 5°, range 25° to 43°). The angle of correction during surgery is 23° (SD ± 4°) and the femoral internal torsion angle was corrected to 10° (SD ± 3°) postoperatively. We illustrate a CT image with a calculation of the femur rotational axis before and after surgery (Fig. 2).
Dislocation of the patella
Sixteen patients (17 knees) had experienced recurrent patellar dislocation, and one of them had suffered recurrent dislocation almost weekly before surgery. No patellar dislocation occurred after surgery.
TTTG distance and the PTA
The mean TTTG distance before surgery was 15.6 ± 2.1 mm, while it was 14.7 ± 1.8 mm after surgery. The mean PTA before and after surgery was 26.4° ± 6.9° and 11.7° ± 2.9°, respectively. The powers of TTTG and PTA measurements are 0.78 and 1.00, respectively. The above differences were statistically significant. (p < 0.05) (Table 2) However, no significant differences were found in the change in the PTA between the two groups after the operation (Table 3). It can be seen that the patellofemoral joint alignment was well improved after the operation according to CT of the knee joint (Fig. 3). Since medial patellar ligament reconstruction or medial retinaculum reefing can also improve PTA, we analyzed the changes of PTA in patients who underwent isolated derotational femoral osteotomy. The mean PTA before and after surgery was 22.50° ± 4.89° and 10.5° ± 2.32°, respectively. The difference was statistically significant (p < 0.05).
Subjective scores (Lysholm/IKDC/Kujala/VAS/patient satisfaction)
Compared with the preoperative Kujala score (59.9 ± 7.9), the postoperative Kujala score significantly increased to 80.7 ± 7.2, while the IKDC score significantly increased from 48.0 ± 11.2 to 72.6 ± 9.3. The average Lysholm score was 56.7 ± 10.5 before osteotomy and 77.9 ± 7.7 upon re-evaluation after the procedure. The postoperative VAS score was only 1.9, and the preoperative pain score was 4.6 (Table 2). These results suggested a marked improvement in the stability of the patients' patella after surgery. In addition, there were no significant differences in the change in the subjective scores postoperatively between the two groups (Table 3). The results of patient satisfaction with the procedure were as follows: 8 (47%) patients were very satisfied results, 6 (35%) were satisfied, 2 (12%) were partially satisfied, and 1 (6%) was dissatisfied at the follow-up.
Complications
In terms of the postoperative complications in our study, 2 patients had knee joint stiffness 2 months after surgery, and the stiffness improved after half a month of passive exercise enhancement. Furthermore, 2 patients reported pain around the knee joint 2 months after surgery, and the pain was gradually relieved during the follow-up. A previous study reported that supracondylar osteotomies of the distal femur can result in increased valgus angulation due to the decreased mLDFA [18]. Fortunately, the patients in our study were not found to have these complications.
Discussion
The main finding of our study was that supracondylar derotation osteotomy of the femur could be an effective treatment for recurrent patellar dislocation induced by increased femoral internal torsion, and good clinical results and improved patellofemoral congruence were obtained. In addition, femoral supracondylar osteotomy is a safe method of surgery, and it can be combined with soft tissue surgery around the knee joint for the treatment of patellar dislocation.
Based on the aforementioned studies, increased femoral internal torsion is one of the major risk factors for malalignment between patella and trochlea, and malalignment seen in all three planes has a great influence on patellar tracking and loading [7, 17, 26]. Excessive femoral internal torsion alters the normal relationship between the femoral neck and femoral condyles, leading to patellofemoral instabilities. Surgical treatment for recurrent patellofemoral instability aims to decrease excessive femoral internal torsion to improve the relationship of the shaft of the femoral neck and the coronal plane of the femoral condyles. In addition, recent studies from Stambough et al. [23] and Nelitz et al. [16] showed that derotational osteotomy of the distal femur could be an excellent treatment for patellofemoral instabilities.
Previous studies have confirmed that the TTTG and the PTA are higher in the instability group than in the normal group without a history of patellofemoral instability [12]. The angle of the femoral internal torsion should be considered in patients with patellar dislocation with an increased TTTG distance. Single correction of the TTTG distance through tibial tubercle transfer surgery may not achieve satisfactory results for patellar dislocation patients with severe femoral internal torsion. After derotational osteotomy, the excessive anteversion angle of the femur was corrected. Furthermore, the TTTG distance and PTA decreased accordingly, results that are similar to those of a previous study which suggested that changes in the tension of the lateral femoral soft tissues after surgery may led to a decrease in the TTTG distance, but more evidence is needed to prove this conclusion [13].
At present, MPFL reconstruction is the main method for the treatment of recurrent patellar dislocation [9, 30]. The medial patellofemoral ligament is considered to be the main soft tissue force that restricts outward movement of the patella by approximately 50–60%, especially knee flexion in the range of 0°–30°. Therefore, MPFL reconstruction is the basic surgical method for the treatment of recurrent patellofemoral instability [9, 22]. However, it has been confirmed that neglecting the treatment of patellofemoral dislocation with torsional deformity of the femur will greatly affect the outcomes of treatment. Franciozi et al. [11] reported 48 cases of tibial tubercle transfer and MPFL reconstruction for recurrent patellar dislocation and confirmed the surgical outcomes. Furthermore, the researchers divided the patients into two groups, one with excessive femoral internal torsion and the other with normal femoral internal torsion, and found that the knee functional score of the patients with increased femoral internal torsion was significantly lower than that of the patients in the normal group, indicating that increased femoral internal torsion can affect the postoperative prognosis. Based on the follow-up study of this experiment, it was confirmed that femoral derotational osteotomy combined with soft tissue surgery was an effective method for the treatment of patellofemoral instability complicated by torsional deformity of the femur.
We conducted 17 derotational osteotomies of the distal femur in patients. The medial patellofemoral retinaculum or MPFL were slack and/or ruptured due to previous dislocation or subluxation of the patella and the medial restrictive structure of patellofemoral joint is weak or damaged when the patella moves outward over 3/4 of the width of the patella [15]. We temporarily fixed the joint capsule after the derotational osteotomy was completed to evaluate the tracking of the patella. If the patellar still had a tendency toward dislocation during the course of passive flexion and extension of the knee joint or the distance of the patellar glide test exceeded the patellar width by 3/4, MPFL reconstruction or strengthening sutures of the medial retinaculum was performed based on the quality of the MPFL on MRI image. We chose MPFL reconstruction in the case where the medial patellofemoral ligament had been ruptured, otherwise we chose medial retinaculum reefing. In our study, all patients underwent femoral derotation osteotomy, four of whom underwent medial ligament reconstruction and five with medial retinaculum reefing. During the follow-up, no redislocation occurred; knee function scores (Kujala, Lysholm, and IKDC scores) were significantly improved, and the VAS score was significantly reduced. The results of patient satisfaction with the procedure were as follows: 8 (47%) patients were very satisfied, 6 (35%) were satisfied, 2 (12%) were partially satisfied, and 1 (6%) was dissatisfied at the follow-up.
Because femoral derotational osteotomy can be performed at different levels, the fixation method and postoperative weight-bearing time are also different. The surgical procedure we are accustomed to is femoral supracondylar osteotomy and fixation with a locking plate. On the second day after surgery, the affected limbs could undergo mild weight-bearing exercises with the aid of knee orthoses and double crutches. We recommended that patients take the initiative to perform quadriceps exercises and knee flexion and to give up crutches and orthoses 3 months after surgery. Looking back upon previous studies, although no studies have confirmed which type of osteotomy is recommended, we believe that femoral supracondylar osteotomy is safer than other osteotomy methods and that it can be combined with soft tissue surgery around the knee joint for the treatment of patellar dislocation.
In the past few decades, the research on the etiology and surgical treatment of patellar dislocation have made substantial progress, such as patellofemoral ligament reconstruction for ligament injuries, tibial tubercle transfer osteotomy (TTO) for increased quadricep angle (Q angle) and the tibial tubercle trochlear groove (TTTG) distance, trochleoplasty for the treatment of trochlear dysplasia or severe patellofemoral arthritis, and combined surgery for patellar dislocation [3, 4, 20, 21, 27, 28]. Sometimes, multiple causes of patellar dislocation exist simultaneously. For example, in patellar dislocation patients with medial patellar ligament injury and excessive femoral internal torsion reconstruction of the patellofemoral ligament is not enough, and femoral derotational osteotomy is required to correct excessive femoral internal torsion. It is important to clarify the cause of patellar dislocation and choose the tailored approach. To achieve more precise treatment, we should carry out individualized treatments. Patients should be systematically evaluated before surgery, including physical examinations, imaging data, patient symptoms, etc., to determine the indications for osteotomy. Only after surgical indications are determined will we achieve the desired postoperative effect.
Limitations
This study has several limitations. First, articular cartilage was not shown on the CT images, so cartilage thickness was not considered when measuring the parameters [2]. Second, our study design was retrospective, and the number of patients included was insufficient. Third, additional soft tissue surgery was performed in some cases, which may have affected the results of femoral derotational osteotomy.
Conclusion
Femoral derotational osteotomy is a suitable treatment for recurrent patellar dislocation and achieves good clinical results, and improved patellofemoral congruence is achieved.
References
Bruce WD, Stevens PM (2004) Surgical correction of miserable malalignment syndrome. J Pediatr Orthop 24(4):392–396
Charles MD, Haloman S, Chen L, Ward SR, Fithian D, Afra R (2013) Magnetic resonance imaging-based topographical differences between control and recurrent patellofemoral instability patients. Am J Sports Med 41(2):374–384
Christensen TC, Sanders TL, Pareek A, Mohan R, Dahm DL, Krych AJ (2017) Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med 45(9):2105–2110
Clark D, Walmsley K, Schranz P, Mandalia V (2017) Tibial tuberosity transfer in combination with medial patellofemoral ligament reconstruction: surgical technique. Arthrosc Tech 6(3):e591–e597
Dammerer D, Liebensteiner MC, Kujala UM et al (2018) Validation of the German version of the Kujala score in patients with patellofemoral instability: a prospective multi-centre study. Arch Orthop Trauma Surg 138(4):527–535
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2(1):19–26
Dickschas J, Harrer J, Pfefferkorn R, Strecker W (2012) Operative treatment of patellofemoral maltracking with torsional osteotomy. Arch Orthop Trauma Surg 132(3):289–298
Diederichs G, Kohlitz T, Kornaropoulos E, Heller MO, Vollnberg B, Scheffler S (2013) Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med 41(1):51–57
Du H, Tian XX, Guo FQ et al (2017) Evaluation of different surgical methods in treating recurrent patella dislocation after three-dimensional reconstruction. Int Orthop 41(12):2517–2524
Eckhoff DG, Brown AW, Kilcoyne RF, Stamm ER (1997) Knee version associated with anterior knee pain. Clin Orthop Relat Res 339:152–155
Franciozi CE, Ambra LF, Albertoni LJ et al (2017) Increased femoral anteversion influence over surgically treated recurrent patellar instability patients. Arthroscopy 33(3):633–640
Hernigou J, Chahidi E, Bouaboula M et al (2018) Knee size chart nomogram for evaluation of tibial tuberosity-trochlear groove distance in knees with or without history of patellofemoral instability. Int Orthop 42(12):2797–2806
Kaiser P, Konschake M, Loth F et al (2019) Derotational femoral osteotomy changes patella tilt, patella engagement and tibial tuberosity trochlear groove distance. Knee Surg Sports Traumatol Arthrosc 28:928
Kling TF Jr, Hensinger RN (1983) Angular and torsional deformities of the lower limbs in children. Clin Orthop Relat Res 176:136–147
Kolowich PA, Paulos LE, Rosenberg TD, Farnsworth S (1990) Lateral release of the patella: indications and contraindications. Am J Sports Med 18(4):359–365
Nelitz M (2018) Femoral derotational osteotomies. Curr Rev Musculoskelet Med 11(2):272–279
Nelitz M, Dreyhaupt J, Williams SR, Dornacher D (2015) Combined supracondylar femoral derotation osteotomy and patellofemoral ligament reconstruction for recurrent patellar dislocation and severe femoral anteversion syndrome: surgical technique and clinical outcome. Int Orthop 39(12):2355–2362
Nelitz M, Wehner T, Steiner M, Durselen L, Lippacher S (2014) The effects of femoral external derotational osteotomy on frontal plane alignment. Knee Surg Sports Traumatol Arthrosc 22(11):2740–2746
Price CT (1985) Lower-extremity rotational problems in children. Normal values to guide management. J Bone Joint Surg Am 67(5):823–824
Schottle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J (2005) Trochleaplasty for patellar instability due to trochlear dysplasia: a minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop 76(5):693–698
Schottle PB, Romero J, Schmeling A, Weiler A (2008) Technical note: anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg 128(5):479–484
Smith TO, Walker J, Russell N (2007) Outcomes of medial patellofemoral ligament reconstruction for patellar instability: a systematic review. Knee Surg Sports Traumatol Arthrosc 15(11):1301–1314
Stambough JB, Davis L, Szymanski DA, Smith JC, Schoenecker PL, Gordon JE (2018) Knee pain and activity outcomes after femoral derotation osteotomy for excessive femoral anteversion. J Pediatr Orthop 38(10):503–509
Steensen RN, Bentley JC, Trinh TQ, Backes JR, Wiltfong RE (2015) The prevalence and combined prevalences of anatomic factors associated with recurrent patellar dislocation: a magnetic resonance imaging study. Am J Sports Med 43(4):921–927
Teitge RA (2018) The power of transverse plane limb mal-alignment in the genesis of anterior knee pain—clinical relevance. Ann Joint 3:70–70
Teitge RA, Torga-Spak R (2011) Rotational femoral osteotomy. Springer, London, pp 441–442
Thompson P, Metcalfe AJ (2019) Current concepts in the surgical management of patellar instability. Knee 26(6):1171–1181
Vacariu A, Studer K, Rutz E, Camathias C (2019) High failure rate 108 years after vastus medialis transfer and lateral release (Green's quadricepsplasty) for recurrent dislocation of the patella. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-019-03322-4
Waidelich HA, Strecker W, Schneider E (1992) Computed tomographic torsion-angle and length measurement of the lower extremity. The methods, normal values and radiation load. Rofo 157(3):245–251
Zheng X, Hu Y, Xie P et al (2019) Surgical medial patellofemoral ligament reconstruction versus non-surgical treatment of acute primary patellar dislocation: a prospective controlled trial. Int Orthop 43(6):1495–1501
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
All authors stated on the manuscript were fully involved in evaluating the study and writing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there are no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tian, G., Yang, G., Zuo, L. et al. Femoral derotation osteotomy for recurrent patellar dislocation. Arch Orthop Trauma Surg 140, 2077–2084 (2020). https://doi.org/10.1007/s00402-020-03598-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03598-x