Abstract
Introduction
Unicompartmental knee arthroplasty (UKA) is a well-accepted treatment for isolated unicompartmental osteoarthritis (OA) of the knee. In previous literature, it has been suggested that bi-unicompartmental knee arthroplasty (bi-UKA) which uses two UKA implants in both the medial and lateral compartments of the same knee is a feasible and viable option for the treatment of knee OA. Given the advantages of UKA treatment, it is warranted to review the literature of bi-UKA and discuss the evidence in terms of implant selection, indications, surgical techniques, and outcomes, respectively.
Materials and methods
Following the PRISMA guidelines, PubMed, Medline, Embase, CINAHL, Web of Science, and Cochrane Library were searched for studies presenting outcome of bi-UKA. Studies were included if they reported clinical outcomes using two unicompartmental prostheses for both medial and lateral femorotibial arthritis. Studies with the addition of patellofemoral arthroplasty or concomitant soft-tissue reconstruction and those not published in English were excluded.
Results
In the early literature, the procedure of bi-UKA were performed for very severe OA and rheumatoid arthritis, but indications have evolved to reflect a more contemporary case-mix of knee OA patients. Both mobile and fixed bearing implants have been used, with the latter being the most frequent choice. A medial parapatellar approach for incision and arthrotomy has been the most frequently used technique. The present review found a promising clinical outcome of both simultaneous and staged bi-UKA although the number of long-term follow-up studies was limited.
Conclusions
Both simultaneous and staged bi-UKA has demonstrated good functional outcomes. However, the volume and level of evidence in general is low for studies captured in this review, and the data on long-term outcomes remain limited. The present review indicates that bi-UKA is a feasible and viable surgical option for bicompartmental femorotibial OA in carefully selected patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) is a well-accepted treatment for isolated compartment osteoarthritis (OA) of the knee [1, 2]. It has been estimated that medial UKA may be performed in up to 50% of all primary knee arthroplasties [3]. Refinement of indications, instrumentation, and implant designs has resulted in implant survivorship for medial UKA that is similar to those reported for total knee arthroplasty (TKA) when medial UKA is used appropriately [4, 5]. Reliable outcomes after lateral UKA have also been reported [6,7,8]. In comparison with TKA, UKA allows for smaller implants, shorter operative times, less blood loss, preservation of both cruciate ligaments, and minimal bone resection [9, 10]. The kinematics and proprioceptive activities of the native knee have been reported to be better preserved by UKA than by TKA [11,12,13]. Perhaps most important are the reports of a significantly higher probability of excellent patient-reported outcome measures (PROMs) and lower rates of complications, readmissions, and mortality after medial UKA compared with TKA [14, 15].
In early reports concerning UKA designs, unicompartmental femorotibial joint implants were used in both the medial and lateral compartments of the same knee to treat severe arthritis [16, 17]. This is referred to as “simultaneous” bi-unicompartmental knee arthroplasty (bi-UKA). Opposed to this is “staged” bi-UKA in which a lateral or medial UKA is added, due to the progression of contralateral femorotibial OA, to a knee with an existing, well-functioning UKA [5, 18,19,20,21] (Fig. 1). In more recent literature, it has been suggested that bi-UKA is a feasible and viable option for the treatment of knee OA in the ACL intact patient [22,23,24], but reports are scattered and an overview is in demand. Given the advantages of UKA treatment, it is warranted to establish if there is proof of a bi-UKA concept in the existing literature. Therefore, the present paper reviews the literature on bi-UKA and discusses the evidence for bi-UKA in terms of implant selection, indications, surgical techniques, and outcomes.
Materials and methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed [25]. An electronic database search of PubMed, Medline, Embase, CINAHL, Web of Science, and Cochrane Library was performed to identify studies reporting outcome of bi-UKA for both medial and lateral femorotibial arthrosis. The following search strategy was used: “(Knee) AND (arthroplasty OR replacement) AND (bi-unicompartmental OR bi-compartmental OR bicompartmental OR bi-condylar OR bicondylar OR bi-unicondylar).” This search returned relevant studies published between the time of inception of the databases to July 2019.
The inclusion criteria were agreed upon by authors KW and AT prior to the identification phase. Studies were included if they were reported clinical outcomes using two unicompartmental prostheses for both medial and lateral femorotibial arthritis. Studies with addition of patellofemoral arthroplasty or concomitant soft tissue reconstruction and those not published in English were excluded. Studies that did not individually state clinical outcomes of bi-UKA or that did not specify a follow-up period were considered inappropriate to review. Studies that appeared to report on the same or similar cohorts as other studies were also excluded. The articles of review or meta-analysis were also excluded.
Screening was performed in three phases to identify relevant titles, abstracts, and full texts. Two reviewers (KW, AT) extracted the data through a standardized data collection form and checked the data for accuracy and any inconsistent results were handled by discussion. The following data were extracted: number of knees, number of patients and patient’s demographic data, type of prosthesis, inclusion criteria, contraindications, surgical approach, clinical outcome measurements, and follow-up period.
The risk of bias of each study has been assessed with a methodological index for evaluation of non-randomized studies (MINORS) score [26]. MINORS is a validated instrument for assessing the methodologic quality of studies and is scored on a scale from 0 to 16 for noncomparative studies (8-item checklist scored from 0–2) and a scale from 0 to 24 for comparative studies (12-item checklist scored from 0–2), in which higher scores represent lower levels of bias.
Results
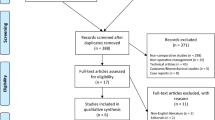
The PRISMA flowchart for study selection is shown in Fig. 2. The initial search identified 903 studies which were screened for eligibility. After removing duplicates and reviewing the titles and abstracts, 15 studies were reviewed in full-text version. Additional five articles were identified through cross-referencing. After reviewing the full text articles, 12 studies were considered eligible for inclusion in the systematic review (Tables 1, 2, 3).
Implant selection
The results are summarized in Table 1. In 1971, Gunston described the performance of bi-UKA with the use of polycentric, fixed-bearing components [16]. In the literature review, the choice of fixed bearing components has been predominant [22,23,24, 27,28,29,30]. In contrast, Goodfellow and O'Connor published on the use of mobile bearing components for bi-UKA [17]. They focused on the theoretical advantages of including analogs of the natural menisci of the knee in the design of their prosthesis, which was the origin of the Oxford UKA [31]. In the report on staged bi-UKA by Pandit et al., a mobile bearing lateral UKA was inserted with the existing mobile bearing medial UKA [19], whereas Lustig et al. used fixed bearing UKA in both compartments [20].
Indication
The results are summarized in Table 2. Gunston performed bi-UKA mainly in patients with longstanding rheumatoid arthritis (RA) [16]. Walker et al. had a similar concept and used the prosthesis for both RA and OA, reporting a total loss of articular surface of less than 12 mm and a body weight of under 73 kg as their inclusion criteria [27]. Goodfellow and O'Connor considered these joints suitable for the procedure if the patient had an adequate range of motion (ROM) (at least 75º of flexion under anesthesia), flexion deformity of not more than 40º, and varus or valgus deformity of not more than 30º [17]. Absence of the posterior cruciate ligament was deemed a contraindication, but not absence of the anterior cruciate ligament (ACL). However, in their series, there were no failures in knees when the ACL was intact, and the revision rate was low. These authors suggested that the presence or absence of the ACL was a significant determinant of the outcome of bi-UKA [17].
After the initial reports, the criteria for bi-UKA evolved to reflect more contemporary constitutions of patients undergoing knee arthroplasty. In 2005, Confalonieri et al. described the typical selection criteria for simultaneous bi-UKA as bi-unicompartmental OA, an asymptomatic patellofemoral joint, ROM greater than 90º, axis deviation less than 10º, and no important anterior or posterior laxity, systemic articular disease, or severe postural defect [30, 32]. Obesity, varus deformity associated with osteoporosis, RA, significant symptomatic patellofemoral OA, extreme laxity, and flexion contracture of more than 10º were considered absolute contraindications. Parratte et al. reported similar indications, except that the acceptable ROM was greater than 100º [24]. They also added the following contraindications: planned high tibial osteotomy, planned or previous ACL reconstruction, and revision arthroplasty.
Staged bi-UKA was mainly developed for patients with progressive OA in the retained compartment after UKA. Pandit et al. considered that patients with clear evidence of progression of OA in the lateral compartment were suitable candidates for the addition of lateral UKA without any evidence of loosening of medial UKA [19]. During surgery, the authors considered TKA if there was severe patellofemoral OA or ACL insufficiency. Lustig et al. additionally stated that staged bi-UKA is particularly attractive for patients with high demands or suffering from comorbidity [20].
Surgical technique
The results are summarized in Table 2. Simultaneous bi-UKA has mainly been performed through a medial parapatellar approach with lateral dislocation of the patella [16, 17, 23, 24, 28,29,30]. Walker et al. inserted the prosthesis through two parapatellar incisions using stereotactic jigs to ensure the accuracy of alignment [27]. In the report on staged bi-UKA by Pandit et al., the medial UKA incision was opened and extended proximally and distally and the lateral compartment was approached using a lateral parapatellar arthrotomy [19]. Lustig et al. suggested to use standard lateral and medial approach for staged bi-UKA if there are at least 8 cm security distance to the previous scar [20].
Goodfellow and O'Connor preserved the joint line at the same level as the natural articular surface [17]. Using an extramedullary guide, the tibial cut was made with a posterior slope of 7º. After the trial components were inserted, gap gauges with a range of thickness to match the implantable bearings were used to determine by trial and error the thickest size that each component could accept comfortably. They also stated that no effort was made to align the bone of the limb and that their focus was on prevention of soft tissue release to preserve the native soft tissue balance. In contrast, Confalonieri et al. reported making the tibial cut using an extramedullary guide [30], which allowed for correct re-alignment of the limb by replacing the most severely affected compartment first. They calculated the amount of bone to be resected to correct the limb alignment based on the preoperative radiographs and the thickness of the implanted components. They also tried to restore the original tibial slope of the different compartments. Dettmer and Kreuzer presented usefulness of robotic arm-assisted, 3D-navigation system for accurate bi-UKA [23].
Outcome
The results are summarized in Table 3. The first report on simultaneous bi-UKA by Gunston stated that polycentric arthroplasty provided a painless knee and eliminated preoperative lateral instability in almost all patients. One (4.5%) knee was later arthrodesed because of the lack of functional improvement [16]. Walker et al. performed bi-UKA using the prosthesis in the manner described by Gunston and reported that 77.3% of patients were enthusiastic about or satisfied with their results. In their report, eight (7.6%) knees required revision or were arthrodesed because of infection or loosening [27]. Stockley et al. also reported the outcomes of using a bicondylar sledge prosthesis, stating that pain relief was substantial (75%) and that functional ability improved in a commensurate manner [28]. In their series, 3 (5.7%) of the arthroplasties failed and required revision.
In the report on mobile bearing bi-UKA by Goodfellow and O'Connor, pain was relieved in 90% of cases, the mean flexion limit was 99º, and the mean flexion deformity was 7º [17]. Failure occurred in six knees (four loosening, one recurrent dislocation of the bearings, and one infection), which were arthrodesed or converted to another prosthesis. Eight (6.4%) knees required revision surgery because of dislocation of the bearings (five cases) or loosening of components (two tibial, one femoral). They also reported that there were no failures and that the revision rate was low in knees with an intact ACL. Barret et al. reported similar result of mobile bearing bi-UKA, and stated that 57 (85%) of the knees had significant relief of pain [31].
More recently, Parratte et al. performed a retrospective analysis of their cases with a fixed bearing bi-UKA and reported that implant survival was 78% at 17 years [24]. The authors stated that bi-UKA alleviated pain effectively, with an increase in mean Knee Society knee and function scores. In their report, 17 knees underwent revision surgery after a mean 6.5 (range 0.8–12) years (16 for aseptic loosening and one for symptomatic progression of OA in the patellofemoral compartment).
The literature on staged bi-UKA is limited. Pandit et al. reported a significant improvement in the mean Oxford Knee Score (OKS). In their report, there were no significant surgery-related complications and there was no need for any further surgical procedures or revisions at the final follow-up [19]. Lustig et al. described that the mean International Knee Society Score for knee and function were improved at the latest follow-up [20].
There have been some studies comparing bi-UKA with other prostheses. Fuchs et al. compared a simultaneous fixed bearing bi-UKA group to a UKA group and stated that implantation of bi-UKA retaining both cruciate ligaments achieved functional results as good as for UKA [29]. Confalonieri et al. reported a matched-pair study of simultaneous fixed bearing bi-UKA and TKA for the treatment of isolated bicompartmental tibiofemoral arthritis with an asymptomatic patellofemoral joint [30]. The Western Ontario and McMaster Universities Arthritis Index (WOMAC) function and stiffness scores were significantly better in the bi-UKA group and the implants were significantly better aligned in the TKA group. The researchers concluded that bi-UKA is a viable option for bicompartmental tibiofemoral OA, with results that are at least as good as those for TKA but with preservation of a higher level of function. Dettmer and Kreuzer (n = 17 patients) also matched patients who received simultaneous bi-UKA with a similar age group of patients who received TKA and compared the subscales of postoperative knee injury and osteoarthritis outcome scores (KOOS) of both the groups [23]. The authors concluded that bi-UKA group had significantly better score in symptoms and activities of daily living. Biazzo et al. matched and compared the long-term outcomes of bi-UKA with those of computer assisted TKA, and described that there were no statistically significant differences were seen for KSS, Function scores and WOMAC Arthritis Index (pain score) at the latest follow-up.
Discussion
The most important finding of this literature review is the favorable clinical outcomes of bi-UKA. However, knowledge of the long-term outcome remains limited, and MINORS scores of the studies were relatively low.
Implant selection
The choice of fixed bearing components for bi-UKA has been predominant in the present review. This is likely to reflect the preferred implant by the authors for medial and lateral UKA in isolation. The optimal design for medial UKA continues to be debated [33, 34], and probably the surgeon should choose the implant design that he/she is familiar with for bi-UKA. Especially, the reports of outcome after mobile-bearing lateral UKA have been diverse [35,36,37]. Pandit et al. used the Oxford Domed Lateral for staged bi-UKA and reported that there were no significant surgery-related complications and that there was no need for any further surgical procedures or revisions [19]. Based on the literature review, it seems the authors chose the implant that they were familiar with in UKA for bi-UKA.
Indication
In early studies, bi-UKA was used for both medial and lateral arthrosis mainly in patients with RA. In recent reports, only knees with OA were candidates for bi-UKA. The indications and exclusion criteria described by Confalonieri et al. were used in recent studies. Although some previous reports suggested that the presence or absence of the ACL was a significant determinant of the outcome of bi-UKA, Romagnoli et al. have introduced a surgical technique that includes bi-UKA with concomitant reconstruction of the ACL [38]. However, use of this technique should be considered carefully, given that no long-term results are available at present for patients who have undergone this procedure. Based on the contemporary reports, it seems appropriate to recommend the following inclusion criteria for bi-UKA: bicompartmental tibio-femoral OA, asymptomatic patella-femoral joint, intact ACL, correctable deformity, and preserved ROM.
Surgical technique
The medial parapatellar approach was mainly used for exposure of bi-unilateral compartments in simultaneous bi-UKA. In some reports, two parapatellar incisions were used, and Romagnoli et al. mentioned that an advantage of this approach is its ability to reduce damage to the extensor mechanism [38]. They also pointed out that the superomedial geniculate artery ensures a blood supply to the patella because the superomedial area of the knee is preserved. Nevertheless, some previous reports have warned that anatomic considerations are needed to prevent necrosis when performing multiple skin incisions on the knee [39, 40]. Further discussions are required regarding the prevention of complications after bi-UKA. From the viewpoint of vascularity, it would be suggested to use the approach which was described by Pandit et al. [19]. They opened the medial UKA incision and extended proximally and distally, and the lateral compartment was approached using a lateral parapatellar arthrotomy. The benefit of this approach is performing the surgery with all ligaments in situ.
In terms of alignment and implant positioning for bi-UKA, there were too few studies to discuss about what was appropriate. In addition, discussing these parameters seems to require evaluation with implant selection [41, 42]. Furthermore, to perform bi-UKA procedure accurately, it seems to be useful to use a navigation system or a robotic arm which recently reported favorable outcome after UKA [43].
Outcome
In the present review, the favorable outcomes of bi-UKA were found. Especially in recent literature, good results of PROMs after bi-UKA were reported. However, varied scoring systems were used for outcome evaluation. In addition, there were limited data about revision surgery procedure after bi-UKA. Further long-term follow-up studies using contemporary PROMs should be conducted to assess functional benefits and durability including procedure of revision surgery after bi-UKA.
Considering the good outcomes of bi-UKA, Fuchs et al. presented that bi-UKA that retains all intraarticular ligaments achieves proprioceptive results comparable with healthy subjects of the same age [44]. The author’s group also described that the clinical scores were significantly better in the bi-UKA group than in the constrained TKA group [45], and stated that the knees after bi-UKA which preserves the native ligaments could be expected to show better joint kinematics than those after TKA. However, previous reports have indicated that the kinematics of the native knee is not restored after bi-UKA. Banks et al. reported that knees that had undergone bi-UKA showed kinematics that were closer to those after TKA than those after medial UKA [46]. Watanabe et al. compared the kinematics of the knee in patients after medial UKA, medial UKA, and patellofemoral arthroplasty, or bi-UKA and found that knees with bi-UKA showed the least femoral external rotation and posterior translation during knee flexion [47]. Nevertheless, there have been few kinematic studies of bi-UKA and no kinematic studies that have included bi-UKA with mobile bearing-type implants. Therefore, further research is needed to evaluate the kinematics after bi-UKA.
The evidence to determine the outcome of staged bi-UKA is limited. A report by Lewold et al. did not recommend the addition of lateral UKA for progression of OA in a retained compartment after medial UKA [48]. However, there has been a report of favorable outcomes after staged bi-UKA: Pandit et al. reported significant increases in PROMs and no cases of revision surgery [19]. Using similar indications, Lustig et al. performed medial UKA for progression of medial compartment disease after lateral UKA with no need of revision surgery for the progression of patellofemoral OA or implant loosening [20, 21]. Although these reports are promising, further studies are necessary to determine the efficacy of staged bi-UKA.
Limitation of review and the published literature
This systematic review is limited by the small number of studies reporting the outcomes of bi-UKA, and in general, the number of patients in all the studies was low. Furthermore, MINORS scores of the studies included in this review were relatively low. In the future, there is a need for more prospective, randomized controlled or comparative studies to bring forward higher level evidence in the comparison of bi-UKA with TKA for the treatment of both medial and lateral arthritis. In addition, evidence considering the long-term outcomes should be further investigated.
Conclusion
Both simultaneous and staged bi-UKA have demonstrated good functional outcomes. However, the volume and level of evidence in general are low for studies captured in this review, and the data on long-term outcomes remain limited. The general experience with the procedure amongst knee surgeons must be considered low, perhaps highlighting the perceived technical difficulty of the procedure. The present review indicates that bi-UKA is a feasible and viable surgical option for bicompartmental femorotibial OA in carefully selected patients.
Abbreviations
- UKA:
-
Unicompartmental knee arthroplasty
- OA:
-
Osteoarthritis
- TKA:
-
Total knee arthroplasty
- PROMs:
-
Patient-reported outcome measures
- bi-UKA:
-
Bi-unicompartmental knee arthroplasty
- RA:
-
Rheumatoid arthritis
- ROM:
-
Range of motion
- ACL:
-
Anterior cruciate ligament
- OKS:
-
Oxford Knee Score
- IKSS/KSS:
-
International knee society score
- WOMAC:
-
Western Ontario and McMaster Universities Arthritis Index
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Scores
- HTO:
-
High tibial osteotomy
- GIUM:
-
A dedicated UKR outcome score developed by the Italian Orthopaedic UKR’s Users Group
- HSS:
-
Hospital for Special Surgery score
- VAS:
-
Visual analog scale
- AKSS:
-
American Knee Society Score
References
Argenson JN, Blanc G, Aubaniac JM, Parratte S (2013) Modern unicompartmental knee arthroplasty with cement: a concise follow-up, at a mean of twenty years, of a previous report. J Bone Jt Surg Am 95(10):905–909. https://doi.org/10.2106/JBJS.L.00963
Winnock de Grave P, Barbier J, Luyckx T, Ryckaert A, Gunst P, Van den Daelen L (2018) Outcomes of a fixed-bearing, medial, cemented unicondylar knee arthroplasty design: survival analysis and functional score of 460 cases. J Arthroplasty 33(9):2792–2799. https://doi.org/10.1016/j.arth.2018.04.031
Willis-Owen CA, Brust K, Alsop H, Miraldo M, Cobb JP (2009) Unicondylar knee arthroplasty in the UK National Health Service: an analysis of candidacy, outcome and cost efficacy. Knee 16(6):473–478. https://doi.org/10.1016/j.knee.2009.04.006
Lisowski LA, Meijer LI, van den Bekerom MP, Pilot P, Lisowski AE (2016) Ten- to 15-year results of the Oxford Phase III mobile unicompartmental knee arthroplasty: a prospective study from a non-designer group. Bone Jt J 98:41–47. https://doi.org/10.1302/0301-620X.98B10.BJJ-2016-0474.R1
Mohammad HR, Strickland L, Hamilton TW, Murray DW (2018) Long-term outcomes of over 8,000 medial Oxford Phase 3 Unicompartmental Knees-a systematic review. Acta Orthop 89(1):101–107. https://doi.org/10.1080/17453674.2017.1367577
Argenson JN, Parratte S, Bertani A, Flecher X, Aubaniac JM (2008) Long-term results with a lateral unicondylar replacement. Clin Orthop Relat Res 466(11):2686–2693. https://doi.org/10.1007/s11999-008-0351-z
Pennington DW, Swienckowski JJ, Lutes WB, Drake GN (2006) Lateral unicompartmental knee arthroplasty. J Arthroplasty 21(1):13–17. https://doi.org/10.1016/j.arth.2004.11.021
Seo SS, Kim CW, Lee CR, Kwon YU, Oh M, Kim OG, Kim CK (2019) Long-term outcomes of unicompartmental knee arthroplasty in patients requiring high flexion: an average 10-year follow-up study. Arch Orthop Trauma Surg 139(11):1633–1639. https://doi.org/10.1007/s00402-019-03268-7
Mullaji AB, Sharma A, Marawar S (2007) Unicompartmental knee arthroplasty: functional recovery and radiographic results with a minimally invasive technique. J Arthroplasty 22(4 Suppl 1):7–11. https://doi.org/10.1016/j.arth.2006.12.109
Hauer G, Sadoghi P, Bernhardt GA, Wolf M, Ruckenstuhl P, Fink A, Leithner A, Gruber G (2020) Greater activity, better range of motion and higher quality of life following unicompartmental knee arthroplasty: a comparative case-control study. Arch Orthop Trauma Surg 140(2):231–237. https://doi.org/10.1007/s00402-019-03296-3
Argenson JN, Komistek RD, Aubaniac JM, Dennis DA, Northcut EJ, Anderson DT, Agostini S (2002) In vivo determination of knee kinematics for subjects implanted with a unicompartmental arthroplasty. J Arthroplasty 17(8):1049–1054. https://doi.org/10.1054/arth.2002.34527
Heyse TJ, El-Zayat BF, De Corte R, Chevalier Y, Scheys L, Innocenti B, Fuchs-Winkelmann S, Labey L (2014) UKA closely preserves natural knee kinematics in vitro. Knee Surg Sports Traumatol Arthrosc 22(8):1902–1910. https://doi.org/10.1007/s00167-013-2752-0
Isaac SM, Barker KL, Danial IN, Beard DJ, Dodd CA, Murray DW (2007) Does arthroplasty type influence knee joint proprioception? A longitudinal prospective study comparing total and unicompartmental arthroplasty. Knee 14(3):212–217. https://doi.org/10.1016/j.knee.2007.01.001
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101 330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384(9952):1437–1445. https://doi.org/10.1016/s0140-6736(14)60419-0
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Jt J 97(6):793–801. https://doi.org/10.1302/0301-620X.97B6.35155
Gunston FH (1971) Polycentric knee arthroplasty. Prosthetic simulation of normal knee movement. J Bone Jt Surg Br 53(2):272–277
Goodfellow JW, O'Connor J (1986) Clinical results of the Oxford knee. Surface arthroplasty of the tibiofemoral joint with a meniscal bearing prosthesis. Clin Orthop Relat Res 205:21–42
Walton MJ, Weale AE, Newman JH (2006) The progression of arthritis following lateral unicompartmental knee replacement. Knee 13(5):374–377. https://doi.org/10.1016/j.knee.2006.05.005
Pandit H, Mancuso F, Jenkins C, Jackson WFM, Price AJ, Dodd CAF, Murray DW (2017) Lateral unicompartmental knee replacement for the treatment of arthritis progression after medial unicompartmental replacement. Knee Surg Sports Traumatol Arthrosc 25(3):669–674. https://doi.org/10.1007/s00167-016-4075-4
Lustig S, Servien E, Neyret P, Pereira H (2008) An original indication for biunicondylar knee antroplasty: subsequent contralateral unicondylar knee arthroplasty after degenerative changes of the opposite compartment. Tech Knee Surg 7(4):240–250
Lustig S, Lording T, Frank F, Debette C, Servien E, Neyret P (2014) Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee 21:S26–S32. https://doi.org/10.1016/s0968-0160(14)50006-3
Biazzo A, Manzotti A, Confalonieri N (2018) Bi-unicompartmental versus total knee arthroplasty: long term results. Acta Orthop Belg 84(3):237–244
Dettmer M, Kreuzer SW (2015) Bi-unicompartmental, robot-assisted knee arthroplasty. Oper Techn Orthop 25(2):155–162. https://doi.org/10.1053/j.oto.2015.03.004
Parratte S, Pauly V, Aubaniac JM, Argenson JN (2010) Survival of bicompartmental knee arthroplasty at 5 to 23 years. Clin Orthop Relat Res 468(1):64–72. https://doi.org/10.1007/s11999-009-1018-0
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Walker SJ, Sharma P, Parr N, Cavendish ME (1986) The long-term results of the Liverpool Mark II knee prosthesis. J Bone Jt Surg Br 68(1):111–116
Stockley I, Douglas DL, Elson RA (1990) Bicondylar St. Georg sledge knee arthroplasty. Clin Orthop Relat Res 255:228–234
Fuchs S, Tibesku CO, Frisse D, Genkinger M, Laass H, Rosenbaum D (2005) Clinical and functional comparison of uni- and bicondylar sledge prostheses. Knee Surg Sports Traumatol Arthrosc 13(3):197–202. https://doi.org/10.1007/s00167-004-0580-y
Confalonieri N, Manzotti A, Cerveri P, De Momi E (2009) Bi-unicompartmental versus total knee arthroplasty: a matched paired study with early clinical results. Arch Orthop Trauma Surg 129(9):1157–1163. https://doi.org/10.1007/s00402-008-0713-8
Barrett DS, Biswas SP, MacKenney RP (1990) The Oxford knee replacement. A review from an independent centre. J Bone Jt Surg Br 72(5):775–778
Confalonieri N, Manzotti A (2005) Mini-invasive computer assisted bi-unicompartimental knee replacement. Int J Med Robot 1(4):45–50. https://doi.org/10.1002/rcs.56
Parratte S, Pauly V, Aubaniac J-M, Argenson J-NA (2011) No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin Orthop Relat Res 470(1):61–68. https://doi.org/10.1007/s11999-011-1961-4
Confalonieri N, Manzotti A, Pullen C (2004) Comparison of a mobile with a fixed tibial bearing unicompartmental knee prosthesis: a prospective randomized trial using a dedicated outcome score. Knee 11(5):357–362. https://doi.org/10.1016/j.knee.2004.01.003
Ernstbrunner L, Imam MA, Andronic O, Perz T, Wieser K, Fucentese SF (2018) Lateral unicompartmental knee replacement: a systematic review of reasons for failure. Int Orthop 42(8):1827–1833. https://doi.org/10.1007/s00264-017-3662-4
Parratte S, Ollivier M, Lunebourg A, Abdel MP, Argenson JN (2015) Long-term results of compartmental arthroplasties of the knee: long term results of partial knee arthroplasty. Bone Jt J 97:9–15. https://doi.org/10.1302/0301-620X.97B10.36426
Newman SDS, Altuntas A, Alsop H, Cobb JP (2017) Up to 10 year follow-up of the Oxford Domed Lateral Partial Knee Replacement from an independent centre. Knee 24(6):1414–1421. https://doi.org/10.1016/j.knee.2017.05.001
Romagnoli S, Marullo M, Massaro M, Rustemi E, D'Amario F, Corbella M (2015) Bi-unicompartmental and combined uni plus patellofemoral replacement: indications and surgical technique. Joints 3(1):42–48
Younger AS, Duncan CP, Masri BA (1998) Surgical exposures in revision total knee arthroplasty. J Am Acad Orthop Surg 6(1):55–64
Vince K, Chivas D, Droll KP (2007) Wound complications after total knee arthroplasty. J Arthroplasty 22(4 Suppl 1):39–44. https://doi.org/10.1016/j.arth.2007.03.014
Zhang Q, Zhang Q, Guo W, Gao M, Ding R, Wang W (2019) Risk factors of postoperative valgus malalignment in mobile-bearing medial unicompartmental knee arthroplasty. Arch Orthop Trauma Surg 139(2):241–248. https://doi.org/10.1007/s00402-018-3070-2
Ozcan C, Simsek ME, Tahta M, Akkaya M, Gursoy S, Bozkurt M (2018) Fixed-bearing unicompartmental knee arthroplasty tolerates higher variance in tibial implant rotation than mobile-bearing designs. Arch Orthop Trauma Surg 138(10):1463–1469. https://doi.org/10.1007/s00402-018-3005-y
Canetti R, Batailler C, Bankhead C, Neyret P, Servien E, Lustig S (2018) Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg 138(12):1765–1771. https://doi.org/10.1007/s00402-018-3042-6
Fuchs S, Tibesku CO, Genkinger M, Laass H, Rosenbaum D (2003) Proprioception with bicondylar sledge prostheses retaining cruciate ligaments. Clin Orthop Relat Res 406:148–154. https://doi.org/10.1097/01.blo.0000038053.29678.a5
Fuchs S, Tibesku CO, Genkinger M, Volmer M, Laass H, Rosenbaum D (2004) Clinical and functional comparison of bicondylar sledge prostheses retaining all ligaments and constrained total knee replacement. Clin Biomech (Bristol, Avon) 19(3):263–269. https://doi.org/10.1016/j.clinbiomech.2003.11.004
Banks SA, Fregly BJ, Boniforti F, Reinschmidt C, Romagnoli S (2005) Comparing in vivo kinematics of unicondylar and bi-unicondylar knee replacements. Knee Surg Sports Traumatol Arthrosc 13(7):551–556. https://doi.org/10.1007/s00167-004-0565-x
Watanabe T, Abbasi AZ, Conditt MA, Christopher J, Kreuzer S, Otto JK, Banks SA (2014) In vivo kinematics of a robot-assisted uni- and multi-compartmental knee arthroplasty. J Orthop Sci 19(4):552–557. https://doi.org/10.1007/s00776-014-0578-3
Lewold S, Robertsson O, Knutson K, Lidgren L (1998) Revision of unicompartmental knee arthroplasty: outcome in 1,135 cases from the Swedish Knee Arthroplasty study. Acta Orthop Scand 69(5):469–474
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AP is a consultant of Zimmer-Biomet Company. All other authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wada, K., Price, A., Gromov, K. et al. Clinical outcome of bi-unicompartmental knee arthroplasty for both medial and lateral femorotibial arthritis: a systematic review—is there proof of concept?. Arch Orthop Trauma Surg 140, 1503–1513 (2020). https://doi.org/10.1007/s00402-020-03492-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03492-6