Abstract
Introduction
Unicompartmental knee arthroplasty (UKA) is frequently performed on active patients with symptomatic osteoarthritis who desire a quick return to sports. The aim of this study was to compare return to sport after lateral UKA performed by robotic-assisted and conventional techniques.
Materials and methods
This retrospective study has assessed 28 lateral UKA (25 patients), 11 performed with robotic-assisted technique and 17 with conventional technique, between 2012 and 2016. The mean age was 65.5 and 59.5 years, with a mean follow-up of 34.4 months (range 15–50) and 39.3 months (range 22–68). Both groups were comparable pre-operatively. Sport habits and the details of the return to sports were assessed using University of California, Los Angeles Scale (UCLA) and direct questioning.
Results
Robotic-assisted surgical technique provided significantly quicker return to sports than conventional technique (4.2 ±1.8 months; range 1–6 vs 10.5 ± 6.7 months; range 3–24; p < 0.01), with a comparable rate of return to sports (100% vs 94%). The practiced sports after lateral UKA were similar to those done preoperatively, with mainly low- and mid-impact sports (hiking, cycling, swimming, and skiing).
Conclusion
Robotic-assisted lateral UKA reduces the time to return to sports at pre-symptomatic levels when compared with conventional surgical technique. The return to sports rate after surgery is high in both groups. A long-term study would provide data on the prothesis wear in this active population.
Level of evidence
Comparative retrospective study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee osteoarthritis (OA) is a limiting factor in patient participation in physical and recreational activities. Arthroplasty represents a reliable solution after failure of conservative treatments [1] and leads to an improvement of health-related quality of life [2]. Unicompartmental knee arthroplasty (UKA) offers an efficient alternative to total knee arthroplasty (TKA) for isolated medial or lateral osteoarthritis [3, 4], showing good results in return to daily and physical activities, and good survival rates, above 90% at 10 years for lateral UKA [5] and above 95% at 8 years for medial UKA [6]. Those good results enable a surgeon to proceed with UKA in young, active patients with high functional demands [7], particularly for isolated lateral osteoarthritis [8, 9].
Current developments in robotic-assisted surgical technique give surgeons intra-operative tools to improve accuracy. In recent studies, the authors reported that robotic-assisted surgical technique for UKA resulted in an improvement of joint-line restitution compared to conventional technique [10] and a lower rate of postoperative limb alignment outliers, as well as a lower revision rate compared to conventional technique [11], using The BlueBelt Navio surgical system (Smith and Nephew®).
At the moment, very few studies assess return to sport (RTS) after UKA, but their results seem encouraging [12], especially for lateral UKA [13].
The aim of this study was to compare RTS in lateral UKA performed by robotic-assisted and conventional techniques. Our hypothesis was that patients undergoing lateral UKA using the robotic-assisted technique would have a faster RTS than those using a conventional technique.
Materials and methods
Patients
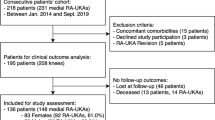
Forty-four lateral UKA in 41 patients were performed with either a robotic-assisted system or conventional technique, between April 2012 and December 2016, by a single senior surgeon. Valgus greater than 14°, anterior cruciate ligament rupture, collateral ligament insufficiency, inflammatory disease of the knee, and multiple compartment osteoarthritis were contraindications to UKA. For this retrospective study, the exclusions criteria were patients with knee-unrelated pathology jeopardizing RTS, patients with revision surgery and patients who did not practice sports before OA onset. Among 44 lateral UKA, 16 patients have been excluded: 9 in the robotic-assisted technique group and 7 in the conventional technique group (Fig. 1). Three of them for osteoarthritis in another joint (two contralateral knee OA and one hip OA), six for knee-unrelated pathology jeopardizing physical activity (two strokes, two cancers with chemotherapy, one with vertebrae fractures and one Parkinson’s disease), three who did not participate in sport before surgery (UCLA score < 5), and three in conventional technique group who underwent revision surgery (two TKA implantation for aseptic loosening, one UKA replacement for impingement).
Thus, 28 lateral UKA were reviewed in 25 patients who participated in sports before surgery and were physically able to return to physical activity. The mean follow-up was 37.2 ± 5.3 months (range 15–68 months). There was no significant demographic difference between both groups (Table 1). Both groups had comparable UCLA scores.
Surgical technique
The implant used was a cemented resurfacing unicompartmental prosthesis with an all-polyethylene tibial component (HLS Uni Evolution, Tornier®). Lateral parapatellar approach was used. All three articular compartments and the cruciate ligaments were examined to confirm suitability for UKA. The BlueBelt Navio robotic surgical system [14] was used in the robotic-assisted surgery group. Choice to carry out either robotic-assisted or conventional technique was dependent on robot availability (dedicated operation room vacant, qualified nurse present, consumable material in stock, availability of the ancillary). The proper surgical robotic-assisted or conventional techniques have already been described [10]. Figure 2 shows postoperative X-ray of robotic-assisted lateral UKA.
Assessment
Standard follow-up was performed at 2 months, 1 year and every year after surgery. At each consultation several outcome scores were assessed: the Objective International Knee Society Score (IKSS-O), the Functional International Knee Society Score (IKSS-F) [15], the Lysholm Knee Scale [16] and the Forgotten Joint Score (FJS) [17]. Level of sport and physical activity were assessed using the University of California, Los Angeles activity scale (UCLA) [18]. Number and types of practiced sports were assessed by direct questioning. Amount of time before returning to sports was asked (“how long did it take you to get back to sports?”). Satisfaction was evaluated by a scaling from 1 to 5 to the question “how well are you satisfied with your prosthesis?” (1 = disappointed; 2 = poorly satisfied; 3 = mildly satisfied; 4 = satisfied; 5 = very satisfied). IKSS-O and IKSS-F were recorded pre- and postoperatively. UCLA, Lysholm, FJS and direct questions were collected at the last survey.
Statistical analysis
Statistical analysis was performed with the online software EasyMedStat® (http://www.easymedstat.com; Neuilly-Sur-Seine; France). Distribution of continuous variables was averaged as range and standard deviation. Difference between unpaired groups was examined using Wilcoxon–Mann–Whitney non-parametric test. Categorical data analysis was performed using two-tailed Fisher’s exact test. Statistical significance was considered at p < 0.05 for all tests.
Results
Robotic-assisted surgical technique produced a significantly quicker RTS (4.2 ± 1.8 months, range 1–6) than conventional technique (10.5 ± 6.7 months, range 3–24) (p < 0.01), with a similar RTS rate of 100% in the robotic-assisted group vs 94% (16/17 patients) in the conventional technique group.
Regarding the type of sports practiced, there was no increase in the number of different sports (from 2.3 to 2.4 in robotic-assisted group; from 1.8 to 1.9 in conventional group). There was no significant difference in intensity level between the groups after surgery (Table 2). Patients did not change their type of sport. Few variations between pre- and postoperative sports practice were found (Table 3).
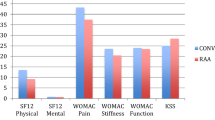
The robotic-assisted group also had a better postoperative IKSS-Objective (97.2 ± 5.9 vs 91.2 ± 6.5; p < 0.05) and a higher improvement in IKSS-Objective comparing pre- and postoperative scores (+ 30.9 ± 7.7 vs + 22.8 ± 12.2; p < 0.05). All results are reported in Table 2. IKSS values are demonstrated in Fig. 3.
Concerning the surgical complications, one patient in the conventional technique group presented with a common peroneal nerve paralysis after surgery and was not able to return to sports.
Discussion
This study is the first to compare RTS after lateral UKA with robotic-assisted surgical technique vs conventional technique. One of the main findings of this study is a faster RTS after robotic-assisted surgery, at an average of 4.2 months postoperatively compared to 10.5 months with a conventional technique. One explanation is a less invasive approach with the robotic-assisted technique. Skin incision is smaller, and with the robotic burr working in difficult-to-visualize areas with a constant monitoring of the cuts, less traction on soft tissues and extensor mechanism is needed to perform safe cuts. Thus, muscle recovery may be faster and soft tissue damage is limited. Another explanation could be better implant positioning with the robotic-assisted system. Loner et al. [14] showed robotic-assisted surgery to be a safe and reproducible technique for UKA implantation with precise positioning of the femoral and tibial components.
In addition, Thienpont et al. [19] showed that valgus deformity in OA mostly lies in distal femoral valgus anatomy, and that correction of valgus deformity needs to be performed on the femoral side principally. In this way, Herry et al. [10] showed in a case–control study comparing 40 medial and lateral UKA using BlueBelt Navio System™ that joint-line height can be improved in robotic-assisted resurfacing UKA by avoiding femoral component distalization and thus reducing tibial resection. Very few studies assessed the RTS after UKA, particularly after lateral UKA. A systematic review of the literature performed by Witjes et al. [7] reported an average RTS at 3 months after medial UKA, which is close to our robotic-assisted technique group. Walker et al. described a RTS after lateral UKA for 77.8% of patients within 6 months in a highly active population [13].
Currently, there is only one study reviewing RTS after lateral UKA, and the authors used conventional techniques with a mobile-bearing tibial plateau implant [13]. They studied 45 patients, with a mean age of 60 years and demonstrated an RTS rate of 98%, with 55.5% of them returning to their activities within 3 months after surgery and 77.8% within 6 months. Our study also demonstrated a high rate of RTS in patients who participated in sports before the onset of OA. However, the cohort of Walker et al. [13] showed a higher level of participation in sport. It can be partly explained by inherent population difference. Indeed, it seems that their patients were more active and motivated to return to sport. While our patients performed between 1.8 and 2.3 different sports, theirs participated in an average of 3. Moreover, 21% of our patients had a UCLA Score ≥ 7, compared to 66% in their cohort (representing highly active patients). Even if there are limited published data on the rate of return to sport after lateral UKA, our data are comparable to rates published for medial UKA [20,21,22,23]. Witjes et al. [7] showed an overall return varied from 75 to 100% after UKA, mostly to lower impact types of sport. The largest portion of their review was based on medial UKA, specifically a study done by Naal et al. [23] which showed a RTS rate of 88%, with 68.6% within 6 months.
Patients who underwent lateral UKA have continued to practice the same sports as pre-operatively in both our study and in the study by Walker et al. There was no statistically significant difference in the number of sports disciplines patients took part in before or after UKA. In the study by Walker et al. [13], only the high-impact activities such as tennis, soccer, jogging or skiing showed a significant decrease in regular postoperative patient participation. The main reason for this decrease in patients’ level of activity was precautionary, with the intention of preserving the prosthesis. Our patients practiced low- or mid-impact sports before surgery. These activities continue to be performed after surgery without difficulties, as reflected by the high satisfaction rate. Similar results were reported by Naal et al. [23] and Fisher et al. [21] for medial compartment UKA.
As reported in the literature [24,25,26], lateral UKA have good functional and objective outcomes, with a high satisfaction rate and a good Forgotten Joint score. For the same implants, our surgical team has shown a survival rate at 94.4% at 10 years and 91.4% at 15 years. For those patients, after 15 years, the mean IKSS-O was 95.1 points and mean IKSS-F was 82.2 points [5]. This study also reports high satisfaction rates at the last follow-up.
There are several limitations to this study. Most importantly, this is a small cohort. Among the 44 lateral UKA, only 28 were eligible for statistical review, mostly because of knee-unrelated pathologies. However, lateral UKA is not common and few studies assess this prothesis. Second, the retrospective questioning concerning their sporting habits has made patients answer to a health state they were in some years ago. Their accuracy could be compromised, introducing recall bias. Then, although it is not statistically significant, patients in the robotic-assisted group seemed to have a higher sports and activity level with a higher mean number of sports and a higher average UCLA score even though this group is older.
Conclusion
Robotic-assisted surgery for lateral UKA reduces the time to return to sports at a patient’s pre-symptomatic level. This robotic tool permits surgeons to be less invasive regarding soft tissues, including quadriceps muscle, extensor mechanism and bony resection, which may lead to a shorter recovery. The RTS rates are high in both groups. These results can help surgeons to inform patients planning for lateral UKA regarding their anticipated postoperative level of activity, especially in young, active patients with high expectations. Future study to include a long-term assessment of wear and revision rates in this highly active population undergoing lateral UKA is indicated.
Abbreviations
- BMI:
-
Body mass index
- FJS:
-
Forgotten Joint Score
- IKSS:
-
International Knee Society Score
- OA:
-
Osteoarthritis
- RTS:
-
Return to sport
- TKA:
-
Total knee arthroplasty
- UCLA:
-
University of California, Los Angeles
- UKA:
-
Unicompartmental knee arthroplasty
References
Lutzner J, Kasten P, Gunther KP, Kirschner S (2009) Surgical options for patients with osteoarthritis of the knee. Nat Rev Rheumatol 5(6):309–316. https://doi.org/10.1038/nrrheum.2009.88
Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY (2004) Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 86-A(5):963–974
Heyse TJ, Tibesku CO (2010) Lateral unicompartmental knee arthroplasty: a review. Arch Orthop Trauma Surg 130(12):1539–1548. https://doi.org/10.1007/s00402-010-1137-9
Dalury DF, Fisher DA, Adams MJ, Gonzales RA (2009) Unicompartmental knee arthroplasty compares favorably to total knee arthroplasty in the same patient. Orthopedics 32(4):253–257
Lustig S, Lording T, Frank F, Debette C, Servien E, Neyret P (2014) Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee 21(Suppl 1S):26–32. https://doi.org/10.1016/S0968-0160(14)50006-3
Hawi N, Plutat J, Kendoff D, Suero EM, Cross MB, Gehrke T et al (2016) Midterm results after unicompartmental knee replacement with all-polyethylene tibial component: a single surgeon experience. Arch Orthop Trauma Surg 136(9):1303–1307. https://doi.org/10.1007/s00402-016-2515-8
Witjes S, Gouttebarge V, Kuijer PP, van Geenen RC, Poolman RW, Kerkhoffs GM (2016) Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med 46(2):269–292. https://doi.org/10.1007/s40279-015-0421-9
van der List JP, Chawla H, Zuiderbaan HA, Pearle AD (2016) Patients with isolated lateral osteoarthritis: unicompartmental or total knee arthroplasty? Knee 23(6):968–974. https://doi.org/10.1016/j.knee.2016.06.007
Servien E, Ait Si Selmi T, Neyret P, Verdonk P (2008) How to select candidates for lateral unicompartmental prosthesis. Curr Orthop Pract 19(4):451–458
Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S (2017) Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop 41(11):2265–2271. https://doi.org/10.1007/s00264-017-3633-9
Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S (2018) Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5081-5
Waldstein W, Kolbitsch P, Koller U, Boettner F, Windhager R (2017) Sport and physical activity following unicompartmental knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 25(3):717–728. https://doi.org/10.1007/s00167-016-4167-1
Walker T, Gotterbarm T, Bruckner T, Merle C, Streit MR (2015) Return to sports, recreational activity and patient-reported outcomes after lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(11):3281–3287. https://doi.org/10.1007/s00167-014-3111-5
Lonner JH, Smith JR, Picard F, Hamlin B, Rowe PJ, Riches PE (2015) High degree of accuracy of a novel image-free handheld robot for unicondylar knee arthroplasty in a cadaveric study. Clin Orthop Relat Res 473(1):206–212. https://doi.org/10.1007/s11999-014-3764-x
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res (248):13–14
Swanenburg J, Koch PP, Meier N, Wirth B (2014) Function and activity in patients with knee arthroplasty: validity and reliability of a German version of the Lysholm Score and the Tegner Activity Scale. Swiss Med Wkly 144w13976. https://doi.org/10.4414/smw.2014.13976
Thienpont E, Opsomer G, Koninckx A, Houssiau F (2014) Joint awareness in different types of knee arthroplasty evaluated with the Forgotten Joint score. J Arthroplasty 29(1):48–51. https://doi.org/10.1016/j.arth.2013.04.024
Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC (1998) Assessing activity in joint replacement patients. J Arthroplasty 13(8):890–895
Thienpont E, Schwab PE, Cornu O, Bellemans J, Victor J (2017) Bone morphotypes of the varus and valgus knee. Arch Orthop Trauma Surg 137(3):393–400. https://doi.org/10.1007/s00402-017-2626-x
Pietschmann MF, Wohlleb L, Weber P, Schmidutz F, Ficklscherer A, Gulecyuz MF et al (2013) Sports activities after medial unicompartmental knee arthroplasty Oxford III-what can we expect? Int Orthop 37(1):31–37. https://doi.org/10.1007/s00264-012-1710-7
Fisher N, Agarwal M, Reuben SF, Johnson DS, Turner PG (2006) Sporting and physical activity following Oxford medial unicompartmental knee arthroplasty. Knee 13(4):296–300. https://doi.org/10.1016/j.knee.2006.03.004
Hopper GP, Leach WJ (2008) Participation in sporting activities following knee replacement: total versus unicompartmental. Knee Surg Sports Traumatol Arthrosc 16(10):973–979. https://doi.org/10.1007/s00167-008-0596-9
Naal FD, Fischer M, Preuss A, Goldhahn J, von Knoch F, Preiss S et al (2007) Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med 35(10):1688–1695. https://doi.org/10.1177/0363546507303562
Marmor L (1984) Lateral compartment arthroplasty of the knee. Clin Orthop Relat Res (186):115–121
Argenson JN, Blanc G, Aubaniac JM, Parratte S (2013) Modern unicompartmental knee arthroplasty with cement: a concise follow-up, at a mean of twenty years, of a previous report. J Bone Joint Surg Am 95(10):905–909. https://doi.org/10.2106/JBJS.L.00963
Lustig S, Parratte S, Magnussen RA, Argenson JN, Neyret P (2012) Lateral unicompartmental knee arthroplasty relieves pain and improves function in posttraumatic osteoarthritis. Clin Orthop Relat Res 470(1):69–76. https://doi.org/10.1007/s11999-011-1963-2
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
RC: study design, data collection, statistical analysis, literature review and manuscript writing. CB: study design, statistical analysis, literature review and manuscript editing. CB: study design, literature review and manuscript editing. PN and ES: study design and manuscript editing. SL: study design, supervision, literature review and manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
CB, RC and CB declare that they have no conflict of interest. PN: consultant for Smith and Nephew, royalties from Tornier-Wright, institutional research support to Tornier-Wright and Amplitude. ES: consultant for Corin. SL: consultant for Smith and Nephew, institutional research support to Corin and Amplitude. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical approval
All procedures were performed in accordance with the ethical standards of the institutional and/or national research committee, the 1964 Helsinki declaration and its later amendments, or comparable ethical standards. The Advisory Committee on Research Information Processing in the Field of Health (CCTIRS) approved this study in Paris on February 17, 2016 under number 16–140. As per institutional standards, formal patient consent is not required for this type of study.
Rights and permissions
About this article
Cite this article
Canetti, R., Batailler, C., Bankhead, C. et al. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg 138, 1765–1771 (2018). https://doi.org/10.1007/s00402-018-3042-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3042-6