Abstract
Purpose
The purpose of this study was to compare the clinical outcomes and survival rate of autologous chondrocyte implantation (ACI) with or without concomitant meniscus allograft transplantation (MAT).
Methods
Patients who underwent ACI of the medial or lateral femoral condyle with or without concomitant MAT were retrospectively reviewed. There were 14 patients (mean age, 31.2 ± 9.9 years) who underwent isolated ACI and 19 patients who underwent ACI with concomitant MAT (mean age, 34.8 ± 8.4 years). The International Knee Documentation Committee (IKDC) subjective score, Lysholm score, Tegner activity score, and 10- to 15-year survival rate were compared between groups.
Results
All clinical scores showed significant improvement postoperatively in both groups. At final follow-up, the IKDC subjective score was superior in isolated ACI (75.8 ± 18.4) compared to ACI with MAT (61.0 ± 16.6, p = 0.024). The Lysholm score was also higher in isolated ACI (77.5 ± 19.1) than ACI with MAT (62.5 ± 18.1, p = 0.029). The Tegner activity score did not differ between treatments (isolated ACI, 5.3 ± 1.1; ACI with MAT, 4.5 ± 1.3; p = 0.072). The 15-year survival rate for isolated ACI was higher than that of ACI with concomitant MAT (69.6% vs 50.2%), but this difference was not statistically significant (p = 0.19).
Conclusions
ACI with concomitant MAT did not restore clinical outcomes as much as isolated ACI. There was a trend for the long-term survival rate to be greater in isolated ACI than ACI with MAT. These results should be considered in planning for the treatment of focal chondral defect with meniscus deficiency.
Level of study
Retrospective comparative trial; level of evidence, 3.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Focal chondral defects of the meniscus-deficient knee are a challenging problem for relatively young patients. Various treatments, from medication to surgery, have been recommended for knee joint preservation. High tibial osteotomy or distal femoral osteotomy can be performed alone or in combination, especially in patients with malalignment [3, 12]. Articular cartilage restoration operations, such as microfracture, autologous chondrocyte implantation (ACI), and osteochondral allograft transplantation with or without meniscus allograft transplantation (MAT), are other treatment options for these patients [4, 5, 7, 17].
Cartilage restoration surgery with concomitant MAT has been shown to have good clinical results. Furthermore, several studies have reported that combined MAT has no adverse effect on the cartilage restoration procedure. Recently, Frank et al. [5] demonstrated that there was no significant difference in reoperation or failure rate and clinical scores between osteochondral allograft transplantation with and without concomitant MAT. Rue et al. [17] demonstrated that the results of combined cartilage restoration and MAT were comparable to those of published reports on these procedures performed in isolation at a minimum 2-year follow-up.
However, the effect of concomitant MAT on clinical outcomes and survivorship after ACI has not been investigated. Although several studies have reported the clinical results of ACI with concomitant MAT [1, 4, 6, 15, 18], there has been no comparative clinical study of ACI with or without concomitant MAT. In addition, no studies have evaluated the long-term survival rate of combined ACI and MAT. The purpose of this study was to compare the clinical outcomes and survival rate of ACI with or without concomitant MAT. We hypothesized that ACI with concomitant MAT would not restore clinical outcomes as much as isolated ACI.
Materials and methods
Patient selection and study design
After approval from our institutional review board, 55 patients who underwent ACI with or without concomitant MAT from July 2002 to August 2007 were retrospectively reviewed. We retrospectively reviewed the patients’ existing medical records and radiologic data of patients and no patients were re-enrolled for this study. Inclusion criteria were primary ACI for chondral defects in the medial or lateral femoral condyle, with or without concomitant MAT in the ipsilateral compartment, and normal alignment (less than varus or valgus 3°). Exclusion criteria were revision ACI, fracture of the ipsilateral limb, ACI for patellofemoral lesion, bilateral knee injury, concomitant high tibial osteotomy or distal femoral osteotomy, ACI and MAT performed in different compartments, and follow-up of less than 10 years. Finally, 33 patients were enrolled (Fig. 1). There were 14 patients who underwent isolated ACI (isolated ACI group) and 19 patients who underwent ACI with concomitant MAT (ACI with MAT group).
Indications for ACI included patients younger than 50 years with normal alignment (less than varus or valgus 3°), persistent knee pain, and full-thickness (ICRS grade IV) chondral lesions ≥ 1 cm (diameter).
Treatment of a meniscal lesion was determined by its size, location and reparability. Meniscus repair was tried for acute, unstable longitudinal tears with good tissue quality in either the red–red or red–white zones and for radial tears that had extended to the red–red zone. Partial meniscectomy was performed when peripheral rim and hoop tension could be preserved after meniscectomy. Otherwise, subtotal or total meniscectomy was performed. Patients who underwent meniscus repair or partial meniscectomy were included in the isolated ACI group. On the other hand, concomitant MAT was performed in patients who had underwent subtotal or total meniscectomy. These patients were included in ACI with MAT group.
Clinical scores and failure rate at final follow-up were compared between the two groups. Survivorship analysis was performed with the projected-limit method considering follow-up loss data.
Surgical technique and rehabilitation
All operations were performed by a single senior surgeon. First-generation ACI was performed after chondrocyte culture and cryopreservation for 6 weeks. The chondral defect was radically debrided with a knife and curetted back to intact cartilage. Periosteum of a suitable size was harvested from the proximal tibia and distal femur and placed on the cartilage defect (inner periosteum from the distal femur, outer periosteum from the proximal tibia). It was secured to the articular surface with multiple interrupted 6-0 Vicryl sutures. The suture line was then waterproofed with autologous fibrin glue. Finally, cultured chondrocytes were injected underneath the periosteum, and the opening injection site was also sealed with fibrin glue.
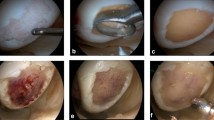
The MAT procedure was combined for medial or lateral meniscus deficiency. Fresh-frozen meniscus allografts were used in all cases. An ordinary bone plug technique was used for medial MAT, and a keyhole technique was used for lateral MAT [20]. The intraoperative findings of isolated ACI and ACI with MAT are shown in Figs. 2 and 3.
There were no differences in rehabilitation regardless of whether or not concomitant MAT was performed. A continuous passive motion machine was used for range of motion (ROM) exercises from 1 day after surgery. ROM exercises were performed within a tolerable range without restriction. Only non-weight-bearing ambulation was allowed in a full extension brace for the first 6 weeks. After the sixth week, partial weight-bearing crutch ambulation was permitted, and patients were encouraged to begin reducing brace wearing. After 3 months, full weight-bearing ambulation without crutches was possible.
Outcome measurements
Clinical outcomes were assessed with the International Knee Documentation Committee (IKDC) subjective score, Lysholm score, and Tegner activity score preoperatively and at the final follow-up by a senior resident who was blinded to the group allocations.
Definition of failure
Failure of ACI was defined as the need for revision surgery due to unrelieved symptoms, an ICRS grade IV chondral defect on MRI, and poor results on the Lysholm score (< 65) [11]. Failure rate was defined as the number of patients with failed ACIs until the final follow-up for all patients.
Statistical analysis
All statistical analyses were performed with SPSS version 21.0 (SPSS Inc., Chicago, IL, USA). Chi square tests were used to compare qualitative variables (sex, injured side, location of chondral defects, combined injury), and independent t tests were used to compare quantitative variables (age, BMI, size of chondral defect, follow-up period, clinical scores). For pre- and postoperative comparisons of clinical scores, the paired-samples t test was used. Survival analysis was performed with the Kaplan–Meier method. The log-rank test (Mantel–Cox, 95% CI) was used to determine if there was a significant difference between the two curves. A p value < 0.05 was considered statistically significant.
A power analysis was performed to determine the sample size for the current study. We defined a clinically relevant difference between the isolated ACI group and ACI with MAT groups as ten points in the postoperative IKDC score. Consequently, we determined that enrollment of 33 patients could achieve statistical significance with > 80% power.
Results
Demographics and clinical outcomes
The preoperative demographic data did not differ significantly between groups, except for the incidence of concomitant meniscus injury (Table 1). All clinical scores showed significant improvement postoperatively in both groups. At final follow-up, the IKDC subjective score was superior in isolated ACI (75.8 ± 18.4) than ACI with MAT (61.0 ± 16.6, p = 0.024). The Lysholm score was also higher in isolated ACI (77.5 ± 19.1) than ACI with MAT (62.5 ± 18.1, p = 0.029). However, the Tegner activity score did not differ significantly between groups (5.3 ± 1.1vs 4.5 ± 1.3, p = 0.072, Table 2).
Failure
There were four failures in isolated ACI (28.6%) and ten in ACI with MAT (52.6%). There was a trend for failure rate to be higher in ACI with MAT than isolated ACI, although this was not statistically significant (p = 0.167). In each group, the most common cause of failure was a poor Lysholm score (Table 3).
Survivorship
Kaplan–Meier survival curves were calculated with failure as the end point. The survival rate was 92.9% for isolated ACI and 89.5% for ACI with MAT at 8 years; these values were 69.6% and 50.2%, respectively, at 15 years. The log-rank test revealed no significant difference between the two Kaplan–Meier survival curves (p = 0.19). However, there was a trend for the long-term survival rate to be greater in isolated ACI than ACI with MAT. The mean and standard deviation for survival time was 12.3 ± 2.6 years (95% CI, 10.8 to 13.8 years) in isolated ACI and 11.2 ± 3.7 years (95% CI, 9.4 to 12.9 years) in ACI with MAT (Fig. 4).
Kaplan–Meier survival estimates, with failure of autologous chondrocyte implantation as the end point, demonstrating a projected 92.9% and 89.5% overall survival at 8 years and a 15-year survival of 69.6% and 50.2% in patients with isolated ACI and ACI with MAT, respectively. The log-rank test (Mantel–Cox, 95% CI) revealed no significant difference in survival rate between groups (p = 0.19)
Discussion
This study confirmed our hypothesis that ACI with concomitant MAT did not restore clinical outcomes as much as isolated ACI over long-term follow-up. Clinical scores for isolated ACI were significantly better than those of ACI with concomitant MAT. There was a trend for the long-term survival rate to be greater in isolated ACI than ACI with MAT. In fact, the two groups compared in this study were basically different patient groups (focal cartilage defects with and without meniscus deficiency). However, several studies reported that the cartilage restoration procedure with concomitant MAT showed no clinical differences compared to isolated cartilage restoration procedure despite the demographic difference [5, 17] Therefore, the clinical outcomes of the two groups were compared in this study.
Historically, combined cartilage restoration surgery and MAT, termed biological knee reconstruction, have been performed for relatively young patients with osteoarthritis [1, 8,9,10, 15] Bhosale et al. [1] performed biological knee reconstruction for osteoarthritis in young patients and reported that all patients were able to lead an active lifestyle after treatment. Harris et al. [8] reviewed several studies and reported good clinical outcomes after combined cartilage restoration and MAT.
Several studies have also reported clinical outcomes for ACI with concomitant MAT [1, 4, 6, 15, 17]. However, the clinical outcomes for combined ACI and MAT remain controversial. Farr et al. [4] reported that MAT in combination with ACI leads to improvement in symptoms and knee function at a minimum 2-year follow-up, but they concluded that the improvements were lower than the literature-reported outcomes of either procedure performed in isolation. Ogura et al. [15] noted that 58% of patients with concomitant ACI and MAT required subsequent surgical procedures over mid- to long-term follow-up. On the other hand, Gersoff et al. [6] reported that ACI with concomitant MAT improved knee function with minimal complications at a mean of 24.7 months follow-up.
The long-term survival rate was higher in isolated ACI than ACI with MAT, although this difference was not statistically significant. We found that the 15-year survival rate was projected at 69.6% for patients treated with isolated ACI, which is consistent with previous studies that have shown favorable long-term survival after ACI. Minas et al. [13] reported that ACI provided durable outcomes with a survivorship of 71% at 10 years and improved function in 75% of patients with symptomatic cartilage defects of the knee at a minimum of 10 years after surgery. A recent study with a 20-year follow-up after first-generation ACI showed a 63% survival rate [16].
Our findings showed that the survival rate of ACI with MAT was 89.5% at 8 years but decreased to 50.2% at 15 years. These results indicate that combined ACI and MAT had a comparable survival rate to isolated ACI up to the mid-term follow-up, but the long-term survival rate was poor. Although many studies have demonstrated that cartilage restoration procedures combined with concomitant MAT show favorable clinical improvements, most of these studies have had short-term follow-ups [1, 5, 6, 17]. Thus, studies with long-term clinical follow-ups are required.
Noyes et al. [14] reported the survival rate of MAT was 85% at 2 years, 77% at 5 years, 69% at 7 years, 45% at 10 years, and 19% at 15 years. These results are consistent with the inferior long-term clinical outcomes of ACI with concomitant MAT in the current study. Meniscal tissue has many important functions, including load transmission, lubrication, improvement of congruity, and shock absorption [2]. These functions of the meniscus protect the cartilage. Spahn et al. demonstrated a high frequency of degenerative cartilage lesions in symptomatic meniscus tears [19]. A recent systematic review suggested that MAT reduces the progression of osteoarthritis, although it is unlikely to be as effective as the native meniscus [18]. Therefore, the clinical outcomes of ACI with concomitant MAT appear to worsen as the survival rate of MAT declines over time.
This study had several limitations. First, the study had a retrospective, nonrandomized design, so selection bias may have influenced the results. Second, two groups of patients compared in this study had different knee states. Unlike the ACI with MAT group, the meniscus of the isolated ACI group was intact and required cartilage reconstruction only. Therefore, the results of this study suggest that the clinical outcome of ACI with transplanted meniscus is inferior to that of ACI with naive meniscus and does not imply that ACI with MAT is a worthless treatment. Third, this study evaluated clinical outcomes of first-generation ACI, so the results may be limited in application to current ACI practice. Fourth, this study lacks radiologic comparison between the two groups. Finally, the sample size in each group was relatively small.
Despite these limitations, this study had several strengths. It compared clinical outcomes of ACI with and without concomitant MAT in a single cohort and documented the long-term survival rate of combined ACI and MAT. In addition, the current study reported a more realistic survival rate, because failure of ACI was defined as either the need for revision surgery or poor results radiologically or clinically.
Conclusions
Both isolated ACI and ACI with concomitant MAT resulted in clinical improvement. However, ACI with concomitant MAT did not restore clinical outcomes as much as isolated ACI over a 10- to 15-year follow-up. There was a trend for the long-term survival rate to be greater in isolated ACI than ACI with MAT. These results should be considered while planning for the treatment of focal chondral defects with meniscus deficiency.
References
Bhosale AM, Myint P, Roberts S et al (2007) Combined autologous chondrocyte implantation and allogenic meniscus transplantation: a biological knee replacement. Knee 14(5):361–368
Biçer EK, Aydoğdu S, Sur H (2016) The structure, function, and healing of the meniscus musculoskeletal research and basic science. Springer, Berlin, pp 405–427
Bode G, von Heyden J, Pestka J et al (2015) Prospective 5-year survival rate data following open-wedge valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 23(7):1949–1955
Farr J, Rawal A, Marberry KM (2007) Concomitant meniscal allograft transplantation and autologous chondrocyte implantation: minimum 2-year follow-up. Am J Sports Med 35(9):1459–1466
Frank RM, Lee S, Cotter EJ, Hannon CP, Leroux T, Cole BJ (2018) Outcomes of osteochondral allograft transplantation with and without concomitant meniscus allograft transplantation a comparative matched group analysis. Am J Sports Med 46(3):573–580
Gersoff WK (2002) Combined meniscal allografttransplantation and autologous chiondrocyte implantation. Oper Tech Sports Med 10(3):165–167
Getgood A, Gelber J, Gortz S, De Young A, Bugbee W (2015) Combined osteochondral allograft and meniscal allograft transplantation: a survivorship analysis. Knee Surg Sports Traumatol Arthrosc 23(4):946–953
Harris JD, Cavo M, Brophy R, Siston R, Flanigan D (2011) Biological knee reconstruction: a systematic review of combined meniscal allograft transplantation and cartilage repair or restoration. Arthroscopy 27(3):409–418
Harris JD, Hussey K, Wilson H et al (2015) Biological knee reconstruction for combined malalignment, meniscal deficiency, and articular cartilage disease. Arthroscopy 31(2):275–282
Harris JD, McNeilan R, Siston RA, Flanigan DC (2013) Survival and clinical outcome of isolated high tibial osteotomy and combined biological knee reconstruction. Knee 20(3):154–161
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10(3):150–154
Mina C, Garrett WE Jr, Pietrobon R, Glisson R, Higgins L (2008) High tibial osteotomy for unloading osteochondral defects in the medial compartment of the knee. Am J Sports Med 36(5):949–955
Minas T, Von Keudell A, Bryant T, Gomoll AH (2014) The John Insall Award: a minimum 10-year outcome study of autologous chondrocyte implantation. Clin Orthop Relat Res 472(1):41–51
Noyes FR, Barber-Westin SD (2016) Long-term survivorship and function of meniscus transplantation. Am J Sports Med 44(9):2330–2338
Ogura T, Bryant T, Minas T (2016) Biological knee reconstruction with concomitant autologous chondrocyte implantation and meniscal allograft transplantation: mid- to long-term outcomes. Orthop J Sports Med 4(10):2325967116668490
Ogura T, Mosier BA, Bryant T, Minas T (2017) A 20-year follow-up after first-generation autologous chondrocyte implantation. Am J Sports Med 45(12):2751–2761
Rue JP, Yanke AB, Busam ML, McNickle AG, Cole BJ (2008) Prospective evaluation of concurrent meniscus transplantation and articular cartilage repair: minimum 2-year follow-up. Am J Sports Med 36(9):1770–1778
Smith NA, Parkinson B, Hutchinson CE, Costa ML, Spalding T (2016) Is meniscal allograft transplantation chondroprotective? A systematic review of radiological outcomes. Knee Surg Sports Traumatol Arthrosc 24(9):2923–2935
Spahn G, Plettenberg H, Hoffmann M, Klemm HT, Brochhausen-Delius C, Hofmann GO (2017) The frequency of cartilage lesions in non-injured knees with symptomatic meniscus tears: results from an arthroscopic and NIR- (near-infrared) spectroscopic investigation. Arch Ortho Trauma Surg 137(6):837–844
Yoon KH, Lee SH, Park SY, Kim HJ, Chung KY (2014) Meniscus allograft transplantation: a comparison of medial and lateral procedures. Am J Sports Med 42(1):200–207
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Institutional review board approval was obtained by the ethics committee of Kyung Hee University Hospital (IRB Number: KHUH 2018-04-042).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yoon, K.H., Kang, S.G., Kwon, Y.B. et al. Clinical outcomes and survival rate of autologous chondrocyte implantation with and without concomitant meniscus allograft transplantation: 10- to 15-year follow-up study. Arch Orthop Trauma Surg 139, 1117–1123 (2019). https://doi.org/10.1007/s00402-019-03148-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03148-0