Abstract
Purpose
Open-wedge high tibial osteotomy using internal plate fixation is a well-established and frequently performed treatment option for the management of medial compartment osteoarthritis (OA) in the young and active patients. The present study provides survival rate and functional outcome preoperatively and after 6, 12, 24, 36 and 60 months following open-wedge high tibial osteotomy. Hypothesis of the authors was high survival rates after 5 years with still remaining satisfying functional results.
Methods
Sixty-two patients suffering from tibial conditioned knee joint varus deformity and medial compartment OA that underwent high tibial osteotomy using an internal plate fixator (TomoFix™, Synthes) were included. Functional outcome was evaluated prior to surgery and in the further clinical course using standard instruments (IKDC score, Lysholm score). Treatment failure was defined as the need for total knee arthroplasty (TKA).
Results
Fifty-one patients (mean age 46.8 ± 10.2 years) were available at a mean of 60.5 (SD ± 2.5) months (follow-up rate 82.3 %) postoperatively. Sixty-month IKDC (69.4 % SD ± 18.6) and Lysholm (76.6 SD ± 20.5) improved significantly when comparing with preoperative values (IKDC 44.6 SD ± 17.8; Lysholm 52.1 SD ± 20.8). Two of 51 subjects underwent TKA, resulting in a survival rate of 96 % among those patients followed (51 of 60; 85 %). Overall complication rate was 8.6 %.
Conclusion
With a survival rate of over 96 % at 5 years, high tibial osteotomy seems to be a reliable treatment option with satisfying clinical outcome. Functional outcome was stable following 60 months. While a delay of the necessity for TKA seems likely with regard to the survival rate demonstrated in this article, possible avoidance needs to be demonstrated by longer follow-up studies.
Level of evidence
Therapeutic case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High tibial osteotomy (HTO) is an accepted treatment option for young and active patients with varus gonarthritis [25]. Lateral closed and medial open-wedge osteotomies represent the most common techniques for valgization osteotomies of the proximal tibia. Data describing midterm outcome and survival rates of HTO using an internal plate fixator are still rare [43].
Medial open-wedge HTO provides a number of theoretical benefits. Fibular osteotomy is not necessary, the surgical approach to the medial metaphyseal tibia seems less invasive, and additionally, the continuous opening of the medial aspects of the metaphysis provides the possibility of an alignment “fine-tuning” during the surgery. In addition, shortening of the leg is no longer relevant, and since the lateral aspects of the knee are not affected, consecutive lateral instabilities are not of clinical relevance [25]. Nevertheless, as a significant benefit, closed-wedge HTO is used to result in a more stable situation of the proximal tibia initially after surgery; therefore, additional bone graft was used in open-wedge HTO in order to achieve more stability and safe consolidation of the osteotomy gap. New concepts have been developed, which do not require the transplantation of autogenous or artificial bone in routine cases. First of all, implants have been introduced that provide more stable fixation (i.e. Puddu Plate™, Arthrex, Naples, USA; Position HTO™, Aesculap, Tuttlingen, Germany; and TomoFix™, Synthes, Solothurn, Switzerland). Both concepts seem to be associated with specific advantages and disadvantages, such as irritation at the implant side for the internal plate fixator [31] and secondary loss of correction or even failure of the implant in less stable implants [1, 37]. However, data describing midterm outcome and survival rates of both groups of implants are still rare; therefore, the purpose of the present study was to evaluate the efficiency and safety of HTO with regard to functional outcome and survival at 5 years. While 2- and 3-year results of these patients have been reported earlier [30, 31], focus of the present manuscript is to evaluate midterm outcome and survival rates at 5 years. Hypothesis of the authors was high survival rates after 5 years with still remaining satisfying functional results.
Materials and methods
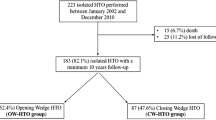
This prospective case series was designed to evaluate functional outcome and survival without knee arthroplasty of patients undergoing HTO with an internal plate fixator for medial compartment varus gonarthritis. From April 2004 to December 2006, 62 patients suffering from medial unicompartmental osteoarthritis of the knee with varus malalignment (minimum 3° of varus malalignment) and medial knee pain were treated with a medial open-wedge osteotomy. In all patients, a routine arthroscopy of the affected knee was performed prior to the osteotomy to exclude patients with full-thickness cartilage lesions of the lateral compartment and to assess the anterior compartment. Defects were classified according to the International Cartilage Research Society (ICRS). Patients of the present study represent a cohort of realistic patients and include all patients treated in our institution during the study period. Therefore, inclusion and exclusion criteria are identical to the general criteria concerning indication of HTO. In short patients with ICRS grade 3 or 4, cartilage lesions of the lateral compartment were excluded from surgical correction of varus malalignment and are not part of the present study. Asymptomatic cartilage defects of the anterior compartment were tolerated. Further contraindications included obesity (no patients with a BMI of 35 or more underwent HTO during the study period), absence or extensive loss of the lateral meniscus, extensive OA (Kellgren and Lawrence grade 3 or 4) of the patellofemoral joint, active knee flexion below 120° or an extension deficiency exceeding 20°, high-grade ligamentous instabilities, active local or systemic infections, and inflammatory arthropathy. Smoking has not been considered a contraindication of the present study.
Preoperative diagnostics
Concerning preoperative diagnostics, all patients obtained radiographs of the knee joint (anteroposterior view and true lateral view at 30° of knee flexion) and anteroposterior long-leg weight-bearing radiographs. Last mentioned were used to determine the degree of varus malalignment. Limb alignment of the affected leg was assessed by the recommendations given by Hsu et al. [18].
Surgical technique was identical in all patients, and HTO was performed according to the technique recommended by the AO International knee expert group [24, 39]. In all cases, an ascending biplanar step osteotomy was performed without the use of additional bone grafts, and an internal plate fixator was used for the stabilization of the osteotomy (TomoFix™ system, Synthes, Solothurn, Switzerland). A mild overcorrection inspired by Fujisawa and other authors [14] has been aspired in all patients. Five different, experienced orthopaedic surgeons carried out surgeries.
Post-operative rehabilitation
With regard to post-operative rehabilitation, all patients were mobilized at the first post-operative day. Continuous passive motion was recommended to all patients after HTO from day 1 postoperatively for 6 weeks for up to 4 h per day. Limited weight bearing was recommended for 2–3 weeks after HTO. Thereafter, weight bearing was stepwise increased to full-weight bearing by week 4 after surgery. Only in patients with additional cartilage repair procedures, a longer period of partial weight bearing for 6 weeks, followed by an increase to full-weight bearing within 10 days, was carried out. Once full-weight bearing was possible, full-leg radiographs were taken to analyse post-operative weight-bearing axis of the affected lower limb.
Patient evaluation
Main outcome parameter in the present study was event-free survival. The necessity of total knee arthroplasty (TKA) was defined as failure and analysed by Kaplan–Meier curve.
Functional outcome was evaluated by established standardized scoring system prior to surgery and at 6, 12, 24, 36 and 60 months following OW-HTO using the Lysholm score and the subjective score of the International Knee Documentation Committee (IKDC).
Statistical analysis
SPSS for Windows (version 17.0; SPSS, Chicago, IL) and GraphPad Prism 5 for Windows (version 5.01, GraphPad Software Inc., La Jolla, California, USA) were used for statistical analyses designed to examine the data ascertained in this study. Quantitative variables at baseline were expressed as mean ± SD. For statistical evaluation of clinical data including IKDC and Lysholm scores, a nonparametric Mann–Whitney test was used. Failure rates were compared using the Chi-square test. Survival curves were shown as a Kaplan–Meier curve. Accordingly, P < 0.05 was considered significant.
Results
At the time of data collection, 51 out of 62 patients were available for follow-up evaluation at 60 months (follow-up rate 82.3 %). Patient’s characteristics are presented in Table 1. Distribution of cartilage lesions is presented in Table 2. Mean preoperative femorotibial axis deviation was 9.5° ± 1.1° of varus. Mean post-operative femorotibial axis was 1.2° of valgus (±1.6), resulting in a slight overcorrection as intended. Baseline date of the nine missing patients is included above. All of them were lost to follow-up after 60 months.
Complications
Intra- and post-operative complication data have been presented earlier [31]. Summing up, one intra-articular fracture of the lateral tibia plateau, three cases of overcorrection (defined as post-operative weight-bearing line >70 % of transverse diameter of proximal tibia), and two cases of delayed union, which were defined as “major” complications, were observed. The percentage of major complications was 8.6 %. In addition, one case of disturbed post-operative wound healing was observed, and 28 patients (40.6 %) felt that the implant was uncomfortable.
Survival
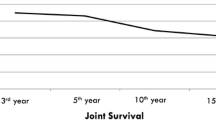
By the time of data collection, two out of 51 patients required total knee arthroplasty because of progressed osteoarthritis of the knee almost 4 years after osteotomy. Therefore, at a mean follow-up of 60 (SD ± 2.7) months, 5-year survival rate was 96 %.
Functional outcome assessed by IKDC and Lysholm scores
Both scores revealed significant improvement of knee function at all follow-up points compared to preoperative data (Fig. 1). IKDC increased continuously from a baseline value of 47.3 (SD ± 18.8) to 69.4 (SD ± 18.6) at 60 months (P < 0.01). Analogous significant improvement from a mean preoperative Lysholm score of 54.3 (SD ± 20.8) to a final score of 76.6 (SD ± 20.5) at 60 months was observed (P < 0.01). No further significant differences between 36 and 60 months after HTO were found, while the remaining time intervals each time were in display of significant improvement.
Discussion
The main findings of the present study were high survival rates even after 5 years following HTO and still good-to-very good functional outcome.
The technique of valgization HTO has much improved in recent years [26, 28, 42], and consideration of the biomechanical axis, proper patient selection, preoperative planning, standardized surgeries, angular stable implants and intra-operative computer navigation leads to improved results [5, 9, 24, 36]. Recently, HTO is even of growing importance as a concomitant surgery in patients with cartilage defects of the medial femoral condyle [20] associated with improved functional outcome [7, 22]. Aiming to delay or even avoid TKA implantation, mid- and long-term survival rates and functional outcome are needed but still elusive [27].
This is the first study presenting survival rates after HTO using an angular stable internal fixator (Tomofix, Synthes, Solothurn, Schweiz) without transplantation of autogenous or artificial bone.
Concerning safety of the procedure, complications of the present patient cohort have been reported earlier [30, 31]. In summary, we observed one case of a lateral intra-articular tibia plateau fracture as an intra-operative complication that required revision with screw osteosynthesis. Furthermore, in three patients overcorrection defined as valgization of more than 70 % of the tibial plateau width was performed. These patients received revision surgery at days 5–6 after the initial treatment. Nevertheless, these complications, especially the cases of overcorrection, very well represent difficulties of valgization osteotomy. Interestingly, all three patients in whom an overcorrection was performed suffered from additional ligamentous instability of the lateral collateral ligament in terms of a double-varus deformity [20]. This is difficult to quantify preoperatively and needs to be considered during planning of the amount of correction. As a consequence of this overcorrection, we introduced intra-operative computer navigation, which significantly helps to reduce outliers in HTO as demonstrated in a subsequent study [21, 34]. This seems to be additional importance since precise correction is an important prognostic parameter for functional outcome [10].
Although the optimal aiming point is still discussed controversially [3], correction of the femorotibial axis to the desired 50–70 % to the transverse diameter of the tibial plateau was considered an adequate post-operative alignment. Mean post-operative femorotibial axis was 1.2° of valgus (±1.6), resulting in a slight overcorrection as intended. No case of undercorrection was observed.
Concerning consolidation of the osteotomy gap, two cases of nonunion were noticed (3.2 %). Both patients were treated with autologous cancellous bone graft from the iliac crest 13 months after the primary surgery. During the further follow-up of the study, between 24 and 60 months, no further complications have been observed. Therefore, overall rate of complication was 8.6 %, which is still significant but relatively low when compared to other techniques. For lateral closed-wedge osteotomy, complication rates of 11, 21 or even 34 % [38, 42] have been reported. In matters of medial open-wedge osteotomy, Miller et al. [28] reported an overall complication rate of 36.9 %.
Spahn et al. [37] monitored overall complication rate of 43.6 % when performing HTO with the Puddu plate, while he found a significant lower complication rate of 16.7 % when using C-plates. These results underline the importance of the choice of the implant in OW-HTO as very low implant-associated complication rates were observed when an internal plate fixator is used for stabilization of OW-HTO [13, 33].
This clinical observation is supported by biomechanical data as published by Agneskirchner et al. [1].
Coming back to clinical outcome even after 5 years, the functional outcomes after HTO are still satisfying (Fig. 1). A stable plateau seemed to be achieved concerning knee function between 36 and 60 months when no further significant differences were found.
Although not being able to proof statistically, the further increase in function between 24 and 36 months might be associated with the removal of the implant. This goes along with the observation that a significant proportion of patients reported discomfort with the implant, which has also been reported earlier [31], and in the majority of cases, implant removal was performed during this period of time.
Direct comparison with studies reporting functional outcome following HTO is difficult as only a surprisingly low number of studies report functional outcome of HTO. Among those various different techniques, implants and scoring systems are described. Improvement of the Oxford Knee Society Score and KOOS after 1 year have been reported, as well as improvement of the HSS score, American Knee Society and Oxford Knee Score after 2–3 years [4, 8, 11, 44]. Details of those studies have been listed in Table 1.
In a recent multicenter study presenting functional outcome of 533 patients after medial open-wedge osteotomy with the internal plate fixator, Floerkenmaier et al. [13] presented good-to-excellent functional outcome with a mean Oxford Knee Score of 43 points.
While clinical results at 2 and 3 years generally focus on clinical outcome and initial complications, at 5 years holding times in terms of midterm results can be reported [15, 16, 23, 29, 35, 41].
Although HTO aims for the reduction in pain and for improvement of function, in a mid- and long-term view it ultimately aims at delay or avoidance of TKA. Therefore, survival time in terms of the need to convert HTO into total knee replacement is a well-accepted and objective criterion for the determination of treatment efficiency. Implantation of TKA was necessary in two of the 51 patients (3.2 %). In those two cases, no specific problems during TKA implantation and in the further clinical course have been observed. Both patients could be treated with Columbus© TKA (Fa. Braun, Melsungen, Germany).
Having defined implantation of TKA as failure, a 5-year survival rate of 96 % after a mean follow-up of over 60 months was observed. Comparing the conversion rate of patients with previously published studies, a percentage of 96 % at 60 months following HTO seems remarkably high. Comparison of results is difficult as different techniques, mostly lateral closed-wedge osteotomy, and implants [40] were used.
Several studies also presented their 5-year results with survival rates ranging from 97 % [23] to 80 % [6]. A 5-year survival rate of 96 % is in the upper range of the present literature [15, 23, 32, 35, 40, 41] (Table 3).
If avoiding unicondylar knee arthroplasty (UKA) or TKA is the aim of HTO, these results must be compared with those known for UKA and TKA. A recent retrospective population-based study performed by W-Dahl et al. [43] presented 10-year results with a survival rate of 70 %, including closed-wedge and open-wedge osteotomies. A revision rate of 30 % in their study was quiet high in comparison with 10-year revision rates of 16 % for UKA and only 6 % for TKA. On the other hand, both HTO and UKA are surgeries performed to delay TKA but always offering an alternative procedure if patients are not satisfied. Once TKA was implanted, the indication for revision is made much more cautious. Furthermore, HTO is mostly performed in patients younger than 65 years where the revision rate for TKA is higher. They concluded that young and active patients benefit from HTO aiming to delay TKA.
Yet, it is notable that many studies, especially those using closed-wedge osteotomy, reported high survival rates after 5–10 years with a later loss of the beneficial effect after 10–15 years [15, 32, 41].
Concerning limitations of the present study, it has to be considered that 5-year results are only midterm results. Nonetheless, a follow-up period of 5 years is a common period when presenting first survival rates. Thus, further studies monitoring still longer-term results using internal fixators for medial open-wedge osteotomy are needed.
As a further potential limitation, the patient cohort in the present study represents rather younger patients with a mean age of 47 years [23]. This might on the one hand influence the indication for consecutive TKA and is also represented by the fact that a significant proportion of patients suffered from early osteoarthritis and not from progressed stages of disease. This is supported by the high rate of accompanying cartilage-regenerating procedures. Furthermore, age under 50 has been proved to be related to higher survival rates after closed-wedge osteotomy [19].
Conclusion
Medial open-wedge osteotomy using the TomoFix® system leads to reliable 5-year results with survival rates of 96 %. Functional outcome improved significantly even after 5 years even though further improvements compared to 36 months could not be observed.
References
Agneskirchner JD, Freiling D, Hurschler C, Lobenhoffer P (2006) Primary stability of four different implants for opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 14(3):291–300
Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H (2008) The long-term outcome of high tibial osteotomy: a ten- to 20-year follow-up. J Bone Joint Surg Br 90(5):592–596
Amis AA (2013) Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):197–205
Asik M, Sen C, Kilic B, Goksan SB, Ciftci F, Taser OF (2006) High tibial osteotomy with Puddu plate for the treatment of varus gonarthrosis. Knee Surg Sports Traumatol Arthrosc 14(10):948–954
Babis GC, An KN, Chao EY, Larson DR, Rand JA, Sim FH (2008) Upper tibia osteotomy: long term results—realignment analysis using OASIS computer software. J Orthop Sci 13(4):328–334
Baumgarten KM, Fealy S, Lyman S, Wickiewicz TL (2007) The coronal plane high tibial osteotomy. Part 1: a clinical and radiographic analysis of intermediate term outcomes. HSS J 3(2):147–154
Bode G, Schmal H, Pestka JM, Ogon P, Sudkamp NP, Niemeyer P (2012) A non-randomized controlled clinical trial on autologous chondrocyte implantation (ACI) in cartilage defects of the medial femoral condyle with or without high tibial osteotomy in patients with varus deformity of less than 5 degrees. Arch Orthop Trauma Surg 133(1):43–49
Briem K, Ramsey DK, Newcomb W, Rudolph KS, Snyder-Mackler L (2007) Effects of the amount of valgus correction for medial compartment knee osteoarthritis on clinical outcome, knee kinetics and muscle co-contraction after opening wedge high tibial osteotomy. J Orthop Res 25(3):311–318
Brinkman JM, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ (2008) Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br 90(12):1548–1557
El-Azab HM, Morgenstern M, Ahrens P, Schuster T, Imhoff AB, Lorenz SG (2011) Limb alignment after open-wedge high tibial osteotomy and its effect on the clinical outcome. Orthopedics 34(10):e622–e628
Esenkaya I, Elmali N (2006) Proximal tibia medial open-wedge osteotomy using plates with wedges: early results in 58 cases. Knee Surg Sports Traumatol Arthrosc 14(10):955–961
Flecher X, Parratte S, Aubaniac JM, Argenson JN (2006) A 12–28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res 452:91–96
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P (2012) Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc 21(1):170–180
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 10(3):585–608
Gstottner M, Pedross F, Liebensteiner M, Bach C (2008) Long-term outcome after high tibial osteotomy. Arch Orthop Trauma Surg 128(1):111–115
Hernigou P, Ma W (2001) Open wedge tibial osteotomy with acrylic bone cement as bone substitute. Knee 8(2):103–110
Hernigou P, Roussignol X, Flouzat-Lachaniette CH, Filippini P, Guissou I, Poignard A (2010) Opening wedge tibial osteotomy for large varus deformity with Ceraver resorbable beta tricalcium phosphate wedges. Int Orthop 34(2):191–199
Hsu RW, Himeno S, Coventry MB, Chao EY (1990) Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res 255:215–227
Hui C, Salmon LJ, Kok A, Williams HA, Hockers N, van der Tempel WM, Chana R, Pinczewski LA (2011) Long-term survival of high tibial osteotomy for medial compartment osteoarthritis of the knee. Am J Sports Med 39(1):64–70
Imhoff AB, Linke RD, Agneskirchner J (2004) Corrective osteotomy in primary varus, double varus and triple varus knee instability with cruciate ligament replacement. Orthopade 33(2):201–207
Iorio R, Pagnottelli M, Vadala A, Giannetti S, Di Sette P, Papandrea P, Conteduca F, Ferretti A (2013) Open-wedge high tibial osteotomy: comparison between manual and computer-assisted techniques. Knee Surg Sports Traumatol Arthrosc 21(1):113–119
König UWH, Friederich NF (2004) Meaning of high tibial valgus osteotomy in cartilage repair. Arthroskopie 17:234–238
Koshino T, Yoshida T, Ara Y, Saito I, Saito T (2004) Fifteen to twenty-eight years’ follow-up results of high tibial valgus osteotomy for osteoarthritic knee. Knee 11(6):439–444
Lobenhoffer P, Agneskirchner J, Zoch W (2004) Open valgus alignment osteotomy of the proximal tibia with fixation by medial plate fixator. Orthopade 33(2):153–160
Lobenhoffer P, Agneskirchner JD (2003) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11(3):132–138
Lutzner J, Gross AF, Gunther KP, Kirschner S (2010) Precision of navigated and conventional open-wedge high tibial osteotomy in a cadaver study. Eur J Med Res 15(3):117–120
McNamara I, Birmingham TB, Fowler PJ, Giffin JR (2013) High tibial osteotomy: evolution of research and clinical applications—a Canadian experience. Knee Surg Sports Traumatol Arthrosc 21(1):23–31
Miller BS, Downie B, McDonough EB, Wojtys EM (2009) Complications after medial opening wedge high tibial osteotomy. Arthroscopy 25(6):639–646
Naudie D, Bourne RB, Rorabeck CH, Bourne TJ (1999) The Install Award. Survivorship of the high tibial valgus osteotomy. A 10- to -22-year followup study. Clin Orthop Relat Res 367:18–27
Niemeyer P, Koestler W, Kaehny C, Kreuz PC, Brooks CJ, Strohm PC, Helwig P, Suedkamp NP (2008) Two-year results of open-wedge high tibial osteotomy with fixation by medial plate fixator for medial compartment arthritis with varus malalignment of the knee. Arthroscopy 24(7):796–804
Niemeyer P, Schmal H, Hauschild O, von Heyden J, Sudkamp NP, Kostler W (2010) Open-wedge osteotomy using an internal plate fixator in patients with medial-compartment gonarthritis and varus malalignment: 3-year results with regard to preoperative arthroscopic and radiographic findings. Arthroscopy 26(12):1607–1616
Papachristou G, Plessas S, Sourlas J, Levidiotis C, Chronopoulos E, Papachristou C (2006) Deterioration of long-term results following high tibial osteotomy in patients under 60 years of age. Int Orthop 30(5):403–408
Pape D, Kohn D, van Giffen N, Hoffmann A, Seil R, Lorbach O (2013) Differences in fixation stability between spacer plate and plate fixator following high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):82–89
Reising K, Strohm PC, Hauschild O, Schmal H, Khattab M, Sudkamp NP, Niemeyer P (2012) Computer-assisted navigation for the intraoperative assessment of lower limb alignment in high tibial osteotomy can avoid outliers compared with the conventional technique. Knee Surg Sports Traumatol Arthrosc 21(1):181–188
Schallberger A, Jacobi M, Wahl P, Maestretti G, Jakob RP (2011) High tibial valgus osteotomy in unicompartmental medial osteoarthritis of the knee: a retrospective follow-up study over 13-21 years. Knee Surg Sports Traumatol Arthrosc 19(1):122–127
Smith JO, Wilson AJ, Thomas NP (2013) Osteotomy around the knee: evolution, principles and results. Knee Surg Sports Traumatol Arthrosc 21(1):3–22
Spahn G, Wittig R (2002) Primary stability of various implants in tibial opening wedge osteotomy: a biomechanical study. J Orthop Sci 7(6):683–687
Sprenger TR, Doerzbacher JF (2003) Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty-two years. J Bone Joint Surg Am 85-A(3):469–474
Staubli AE, De Simoni C, Babst R, Lobenhoffer P (2003) TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia—early results in 92 cases. Injury 34(Suppl 2):B55–B62
Sterett WI, Steadman JR (2004) Chondral resurfacing and high tibial osteotomy in the varus knee. Am J Sports Med 32(5):1243–1249
Tang WC, Henderson IJ (2005) High tibial osteotomy: long term survival analysis and patients’ perspective. Knee 12(6):410–413
Tunggal JA, Higgins GA, Waddell JP (2010) Complications of closing wedge high tibial osteotomy. Int Orthop 34(2):255–261
W-Dahl A, Robertsson O, Lohmander LS (2012) High tibial osteotomy in Sweden, 1998–2007. Acta Orthop 83(3):244–248
Zaki SH, Rae PJ (2009) High tibial valgus osteotomy using the Tomofix plate—medium-term results in young patients. Acta Orthop Belg 75(3):360–367
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bode, G., von Heyden, J., Pestka, J. et al. Prospective 5-year survival rate data following open-wedge valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 23, 1949–1955 (2015). https://doi.org/10.1007/s00167-013-2762-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2762-y