Abstract
Introduction
Percutaneous iliosacral screw placement following pelvic trauma is associated with high rates of revisions, screw malpositioning, the risk of neurological damage and inefficient stability. The correct entry point and the small target corridor may be difficult to visualize using only an image intensifier. Therefore, 2D and 3D image-based navigation and reconstruction techniques could be helpful tools. The aim of this systematic review and meta-analysis was to evaluate the best available evidence regarding the rate of malpositioning and revisions using different techniques for screw implantation, i.e., conventional, 2D and 3D image-based navigation and reconstruction techniques, CT navigation.
Methods
A systematic review and meta-analysis were performed using the data available on Ovid Medline. 430 studies published between 1/1948 and 2/2011 were identified by two independent investigators. Inclusion criteria were percutaneous iliosacral screw fixation after traumatic pelvic fractures with included revision rate or positioning of the screw, language of the article English or German. Exclusion criteria were osteoporotic fracture, tumor, reviews, epidemiological studies, biomechanical/cadaveric studies, studies about operative technique. For statistical analysis the random effect model was used.
Results
A total of 51 studies fulfilled the inclusion requirements describing 2,353 percutaneous screw implantations following pelvic trauma in 1,731 patients. The estimated rate of malposition was 0.1 % for 262 screws using CT navigation. This rate was significantly lower (p < 0.0001) than for the conventional technique with malposition rate of 2.6 % (total 1,832 screws). Using 2D and 3D image-based navigation and reconstruction techniques, the malposition rate was 1.3 % (total 445 screws). No significance was observed between the conventional and the 2D and 3D image-based navigation and reconstruction techniques. The rates of revision were not statistically significant with 2.7 % (1,832 implantations) in the conventional group, 1.3 % (445 implantations) in the group of 2D and 3D image-based navigation and reconstruction techniques and 0.8 % (262 implantations) using the CT navigation.
Conclusions
CT navigation has the lowest rate of screw malposition, but on the other hand it could not be used for all type of fractures where surgical procedures (reduction maneuvers, additional osteosynthetic procedures) are necessary. The 2D and 3D image-based navigation and reconstruction techniques provide encouraging results with slightly lower rate of complications compared to the conventional technique and are additional tools to enhance the precision and decrease the rate of revision.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
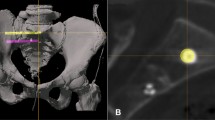
Iliosacral screw placement has become a common technique for the fixation of unstable posterior pelvic ring injuries [1–3]. Despite its widespread acceptance and use, iliosacral screw placement is challenging for various reasons (variable posterior pelvic ring osseous anatomy and upper sacral segment dysmorphisms) [4, 5].
The current standard treatment for these injuries is percutaneous iliosacral screw fixation using the fluoroscopic technique described by Matta and Saucedo [6]. This technique, which was first used on patients when they lay in the prone position, was later modified to allow for its use in the supine position with or without a percutaneous approach. Complications can arise under fluoroscopic guidance due to poor visualization [7]. Imaging is often inadequate due to obesity, bowel gas, intestinal discharge, dysplastic pelvis and low-quality X-ray pictures [8]. Due to relatively high misplacement rates [9], navigated procedures were subsequently introduced to decrease radiation exposure and to increase the safety of screw placement, especially when a percutaneous technique is used [10–13].
To achieve a correct screw placement, various authors have used fluoroscopy [2, 14], computed tomography (CT) [7, 14, 15], fluoroscopic CT and computer-assisted techniques [12, 16, 17]. Conventional fluoroscopy is the current standard in most hospitals for intraoperative visualization [2, 15, 18–21]. Lateral sacral images are required in combination with anteroposterior, inlet and outlet views. One disadvantage of this technique is that visualization using an image intensifier is only possible in one plane at a time. The surgeon must perform a process of interpolation that may be associated with inherent errors. Identifying the correct entry point for the screw and the correct angle of implantation within the very small target corridor in all planes is essential for proper placement. Therefore, the danger of perforation of the sacrum or the sacral foramina is high, and the operative procedure requires exact anatomic knowledge and extensive surgical experience. The technical problems of screw placement are compounded by difficulties in radiographic interpretation caused by obesity, intestinal gases and variations in the anatomy of the posterior pelvis [22]. The incorrect placement of iliosacral screws may result in implant-related and neurovascular complications [13, 23, 24]. Screw malposition rates with fluoroscopic guidance have been reported to range from 2 to 15 % [19, 25], with an incidence of neurological injury between 0.5 and 7.7 % [26]. Moreover, a malposition of the screw of as little as 4º can damage neurovascular structures [25].
The aim of this systematic review was to use the best available evidence to evaluate the rates of malposition, performed revisions, postoperative reductions and clinical follow-ups in clinical trials of iliosacral screw implantation to treat traumatic pelvic fractures. Here different imaging modalities should be analyzed.
Materials and methods
Selection of studies
For this systematic review and meta-analysis, an OVID-based literature search was performed to identify any published clinical studies regarding the surgical treatment of traumatic pelvic fractures using percutaneous iliosacral screw fixation. The following databases were included: MEDLINE, MEDLINE preprints, EMBASE, CINAHL, Life Science Citations, British National Library of Health, and the Cochrane Central Register of Controlled Trials (CENTRAL). The literature search period was from 1/1/1948 to 2/1/2011. The search was performed on 5/26/2012. The literature search was performed using the following systematic strategy:
1. Sacroiliac joint/, 2. Sacrum/, 3. Ilium/, 4. Pelvic bones/in, 5. 1 or 2 or 3 or 4, 6. Bone plates/, 7. Bone screws/, 8. Fracture fixation, internal/, 9. 6 or 7 or 8, 10. 5 and 9, 11. tomography, X-ray/, 12. tomography, X-ray computed/, 13. exp fluoroscopy/, 14. Radiography/, 15. Imaging, three-dimensional/, 16. Image processing, Computer-assisted/, 17. Surgery, computer-assisted/, 18. Surgical procedures, Minimally invasive/, 19. Fractures, bone/ra, 20. navigat*.mp., 21. fluoroscop*.mp., 22. guid*.mp., 23. 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22, 24. 10 and 23.
Assessment protocol
The methods of the analysis and the inclusion criteria were specified in advance and documented in a protocol. Any study that reported clinical information operative treatment of traumatic pelvic fractures using iliosacral screws was considered to be potentially relevant and selected for primary review. Specific attention was placed on identifying studies that described the parameters of the misplacement of the screw, the revision rate and the secondary rotational displacement of the fracture.
The abstracts of the identified studies were evaluated in a primary screening by two independent reviewers, who used the inclusion and exclusion criteria that are given in Fig. 1, where also the dropout criteria were mentioned. Subsequently, two independent reviewers systemically extracted the following data from the 430 studies: the characteristics and design, the level of evidence, the demographic parameters, the fracture classification, the surgical and implantation and navigation technique, the associated surgical procedures, the rate of malposition of screws, the revision rates, the postoperative quality of reduction and secondary rotational displacement. Specific focus was placed on extracting data that described the malposition and revisions rates for the different screw implantation techniques, i.e., conventional intraoperative X-ray, 2D and 3D image-based navigation and reconstruction techniques or CT navigation.
A total of 51 clinical studies of an operative treatment with percutaneous iliosacral screw fixation were identified for further analysis. These studies were evaluated in a primary screening by two independent experienced orthopedic and trauma surgeons.
The level of evidence was categorized according to the definition given by the Oxford Centre for Evidence-based Medicine published by Hanzlik [27]. All of the prospective randomized controlled studies (Levels I and II), and all of the prospective or retrospective studies with or without control groups (Levels III and IV) were accepted for inclusion into the study.
The fracture type according to the AO classification was used to categorize the fractures in each subgroup. Given that various modifications of surgical principles were performed in the included studies, the present study analyzed the major treatment subgroups of the following three primary therapy concepts for screw implantation: “Conventional technique using fluoroscopy guidance only, 2D and 3D image-based navigation and reconstruction techniques or CT navigation.” A specific meta-analysis was performed in these subgroups with the primary endpoint of screw malpositioning and surgical revisions following implantation for multiple reasons, such as loosening, hematoma, malposition, the failure of the osteosynthesis, etc. A more specific analysis was not possible due to the small numbers. Moreover, the postoperative quality of fracture reduction was categorized as excellent, good, fair or poor.
Statistics
The data were independently verified against the original manuscripts in an unblended standardized manner by two reviewers, who used a standard quality-control procedure. Any differences of opinion between the original reviewer and quality-control reviewer were resolved by discussion and reference to the study paper. A consensus was achieved in these cases. The data were analyzed using established statistical software (SPSS software Version 17.0, R-Project 2.15.0, package ‘meta’, by G. Schwarzer). The analyzed standard deviations were computed for the reported means of each study. This analysis took possible study effects into account, and a random effect model was used for the statistical analysis.
Results
The characteristics of the included studies and the patients
A total of 430 clinical studies of percutaneous iliosacral screw fixation in traumatic pelvic fractures were identified. Due to the criteria that are indicated in Fig. 1, 379 studies were excluded. After the screening 51 studies were included, describing 2,353 percutaneous screw implantations into the iliosacral joint in 1,731 patients following traumatic pelvic fractures. The average age of the patients ranged from 19 to 56 years (mean 39.6 ± 10.7 years). In 39 studies (n = 1,394), the gender distribution was mentioned for a total of 866 males (62 %) and 528 females (38 %). The AO classification was only used in 30 studies, for a total of 1,216 patients. 21 fractures were Type A, 342 were Type B and 853 were Type C. The ISS could only be analyzed in eight studies, and the mean was 24 (range 18–32).
The analyzed studies were divided into three subgroups of implantation techniques for further analysis:
-
1.
conventional technique using intraoperative fluoroscopy;
-
2.
2D and 3D image-based navigation and reconstruction technique;
-
3.
the use of CT navigation.
The demographic data are given in Table 1.
Malposition of the screws
A random effect model was used to determine the malposition rates for each group (Fig. 2). The estimated rate of malpositions (events) was significantly lower with the use of CT navigation (0.1 % in 262 implanted screws, group 3) as compared to both the conventional technique (2.6 % in 1,832 screws, group 1) and 2D and 3D image-based navigation and reconstruction techniques (1.3 % in 445 screw implantations, group 2) (p < 0.0001). No statistically significant difference was observed between the conventional and 2D and 3D image-based navigation and reconstruction techniques.
This figure shows the random effect model that was used for the statistical analysis, which returned the results of malposition rates for the implanted screws for each group of studies. The standard deviations were computed from the reported means for each study and were analyzed. This analysis took possible study effects into account
Revision rate following screw implantation
Figure 3 gives the revision rates following screw implantations. No significant difference was observed between the estimated rates of revision. These rates were 2.7 % (of the 1,832 screws in the conventional group), 1.3 % (of 445 screws) in the group of 2D and 3D image-based navigation and reconstruction techniques and 0.8 % (of 262 screws) using the CT navigation. The reasons for the revisions were only partially mentioned in a subset of the studies, and no further analyses were performed.
This figure shows the random effect model that was used for the statistical analysis, which gave the results of the revision rates following screw implantation. The analyzed standard deviations were computed for the reported means of the studies. This analysis took possible study effects into account
Quality of postoperative reduction
The postoperative reduction was evaluated in 11 studies in the conventional group. Excellent or good results were observed in 561 patients (92 %), and fair or poor results were obtained in 49 patients (8 %). The use of CT navigation in five studies with similar fracture distributions led to excellent or good results in 47 patients (88.3 %) and fair or poor results in 4 patients (11.7 %). No data were found regarding postoperative reduction in the group of 2D and 3D image-based navigation and reconstruction techniques.
Secondary rotational displacement in follow-up radiographs
With respect to follow-up radiographs, the results for a secondary rotational displacement with the same definition (>5 mm) were given in 11 studies in the conventional group, in five studies in the group of 2D and 3D image-based navigation and reconstruction techniques and in two studies in which CT navigation was used. The results are given in Table 2 and indicate persistent displacement of the posterior pelvic ring. Considering that a persistent displacement of >5 mm redisplacement may or may not be clinically important, but it provided a measurable and appropriately sensitive threshold for technical failure. The results indicate that the very reliable placement of screws by CT navigation is associated with a poor quality postoperative reduction.
Radiation exposure and clinical follow-up
No sufficient analyses could be performed with respect to radiation exposure given that most studies did not provide data. Moreover, it was only possible in four studies for data regarding a single screw implantation to be distinguished from those data for other operative procedures.
Only seven studies provided the postoperative evaluation of the clinical outcome, with a follow-up period between 15 and 33 months. The following results were obtained with respect to the Majeed score [28]: 184 × excellent or good results (90 %), 14 × fair (7 %), 7 × poor result (3 %). In one study, the Rommens and Hessmann score [29] was used, and the follow-up investigation revealed 16× excellent and good results (84 %), 2× fair (11 %), and 1× poor (5 %) result. A comparison between the defined intervention groups was not possible using the extracted data.
Discussion
In this systematic review and meta-analysis, the primary aim was to investigate the best possible differences between 2D and 3D image-based navigation and reconstruction techniques in percutaneous screw stabilizations of the iliosacral joint following traumatic pelvic fracture compared to the conventional fluoroscopic procedure and CT navigation in terms of malposition and revision rates. The demographic data were similar for all three of the groups.
The CT navigation has the lowest rate of screw malposition, but on the other hand it could not be used for all types of fractures where surgical procedures (reduction maneuvers, additional osteosynthetic procedures) are necessary. The 2D and 3D image-based navigation and reconstruction techniques provide encouraging results with slightly lower rate of complications compared to the conventional technique and are an additional tool to enhance the precision and decrease the rate of revision.
One strength of this study is the analysis by using the random effect model of the best available evidence of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures. Weaknesses of most included studies and therefore of this meta-analysis are that no clear definition of screw malposition and no comparable grading systems are given by most authors and no level of experience of the surgeons are mentioned.
In the years following the introduction of navigation systems, only a small number of authors have reported their clinical experiences or the results of cadaver studies [3, 30–33]. The studies that have reported results regarding the relatively new 2D and 3D image-based navigation and reconstruction techniques were published between 2002 and 2011. These studies therefore reported the first results following the clinical use of this method.
In earlier studies, similar OR times and significant reductions in both the average radiation dose and time were achieved using the 3D image-based navigation and reconstruction techniques [10, 11]. The exact Matta projections of the inlet, outlet and lateral perspectives are difficult to accomplish and are not required with the 2D and 3D image-based navigation and reconstruction techniques. Moreover, earlier studies have indicated lower radiation exposure using computer-assisted surgery in animal studies or for patients with postpartum pelvic pain syndrome [1, 9].
Screw malposition rates with fluoroscopic guidance have been reported to range from 0 to 15 % [19, 25], with an incidence of neurological injury between 0.5 and 7.7 % [26]. Retrospectively, either the bending of the guide wire of the tracked power drive, which cannot be accommodated by the navigation system, or unnoticed manipulations of the reference array can lead to a complete shift of the image in the navigated technique. Although the accuracy of the computer-guided iliosacral screw implantation was investigated by different authors [16, 17], who demonstrated that the navigated system was effective and sufficiently safe to warrant clinical trials, Arand [31] recommended that the following potential technical pitfalls be kept in mind when navigating CT datasets of the pelvis: (1) the intraoperative accuracy of the registration of the preoperative CT scan; (2) the movement of the pelvic bone structure between the preoperative CT scan and during operation; (3) the bending of the guide wire of the tracked power drive, which cannot be accommodated by the navigation system, will lead to misguidance; therefore, only navigated drill sleeves should be used.
CT navigation appears to be a safe technique for implantation, but is only possible when no reduction or other surgical treatment of the pelvic fracture is required. However, Tile B and C type fractures frequently require additional osteosyntheses and reduction maneuvers. Accordingly, in this group, malposition rate was the lowest, whereas the remaining displacement was the greatest. A malposition rate of only 1.3 % was observed when using the modern 2D and 3D image-based navigation and reconstruction techniques, compared to 2.3 % when using the conventional technique. Most authors use the term “malposition” only when a screw revision was performed. Moreover, the experience level of the surgeons who performed the primary screw implantation was not analyzed.
The target corridor and the cortical borders can be extremely difficult to discern using the conventional fluoroscopic standard lateral, inlet, and outlet pelvic views. Moreover, the views could be poorer in obese patients or those with meteoric bowel distension. Therefore, the use of trial drillings and repeated Kirschner wire positioning may occasionally be required before the correct position can be achieved. Given that multiple drilling may lead to a loss of bone stock around the screw this was believed to be a primary reason for the high rate of loosening and performed revisions in earlier studies [11]. When 2D and 3D image-based navigation and reconstruction technique or CT guidance is applied the target corridor is shown in real time during drilling, so nearly no correction during the drilling process, which can cause the loss of bone stock, is required. The accuracy of computer-guided trans-iliosacral screw implantation has been reported to be sufficiently effective and safe in preclinical work [16, 17] to warrant clinical trials. The revision rate following navigated implantation (CT 0.8 %, 2D/3D: 1.3 %) appears to be lower than the rate that is observed for implantations that are performed using the conventional technique (2.7 %) and to be safer for the patient. Revised screws were those patients in each study who were brought back to OR for another additional surgical procedure. Still, these studies were limited in that additional osteosynthesis and reduction techniques were generally not considered in the evaluated trials.
The quality of the reduction could only be investigated in a small number of studies. The observed tendency suggested a better result, with 92.0 % good and excellent results in the conventional group compared to only 88.3 % in the CT navigation group. Nearly no reduction maneuvers can be performed using CT navigation. This circumstance may lead one to conclude that the treating radiologists and trauma surgeons accepted suboptimal reduction quality prior to the implantation of the screw in a higher number of cases than occurred for the other techniques. The acceptance of suboptimal reduction quality may be one reason for the relative high percentage (14.3 %) of cases that showed secondary rotational displacement on follow-up radiographs when CT navigation was used. In contrast, no secondary rotational displacements of 10 mm or more were observed in the group of studies for which 2D and 3D image-based navigation and reconstruction techniques was used.
Conclusion
Overall, the 2D and 3D image-based navigation and reconstruction techniques are additional tools that can be used to enhance the precision and decrease the rate of revisions during the placement of percutaneous iliosacral screws. One fundamental advantage of these methods compared to the CT navigation is that they may be used in many different circumstances, including during the surgical procedures, for any required reduction maneuvers or for any additional osteosynthesis. These techniques provide good results and a low rate of complications and revisions. The authors believe that the 2D and 3D image-based navigation and reconstruction techniques is also an effective tool for teaching young trauma surgeons and to provide additional visual aid in an anatomical region where screw implantation may be challenging.
Nevertheless, the navigation system cannot guarantee 100 % precision. As demonstrated previously, even when these techniques are used to place sacroiliac screws, the malpositioning rate is dependent on the surgeon’s experience with the navigation technique [34].
References
Schep NW, Haverlag R, van Vugt AB (2004) Computer-assisted versus conventional surgery for insertion of 96 cannulated iliosacral screws in patients with postpartum pelvic pain. J Trauma 57(6):1299–1302
Routt ML Jr, Kregor PJ, Simonian PT, Mayo KA (1995) Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma 9(3):207–214
Smith HE, Yuan PS, Sasso R, Papadopolous S, Vaccaro AR (2006) An evaluation of image-guided technologies in the placement of percutaneous iliosacral screws. Spine 31(2):234–238
Sagi HC, Lindvall EM (2005) Inadvertent intraforaminal iliosacral screw placement despite apparent appropriate positioning on intraoperative fluoroscopy. J Orthop Trauma 19(2):130–133 Epub 2005/01/29
Routt ML Jr, Simonian PT, Agnew SG, Mann FA (1996) Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study. J Orthop Trauma 10(3):171–177 Epub 1996/01/01
Matta JM, Saucedo T (1989) Internal fixation of pelvic ring fractures. Clin Orthop Relat Res 242:83–97
Nelson DW, Duwelius PJ (1991) CT-guided fixation of sacral fractures and sacroiliac joint disruptions. Radiology 180(2):527–532
Routt ML Jr, Simonian PT, Mills WJ (1997) Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma 11(8):584–589 Epub 1998/01/07
Tonetti J, Carrat L, Blendea S, Merloz P, Troccaz J, Lavallee S et al (2001) Clinical results of percutaneous pelvic surgery. Computer assisted surgery using ultrasound compared to standard fluoroscopy. Comput Aided Surg 6(4):204–211
Zwingmann J, Konrad G, Kotter E, Sudkamp NP, Oberst M (2009) Computer-navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin Orthop Relat Res 467(7):1833–1838 Epub 2008/11/27
Zwingmann J, Konrad G, Mehlhorn AT, Sudkamp NP, Oberst M (2010) Percutaneous iliosacral screw insertion: malpositioning and revision rate of screws with regards to application technique (navigated vs. Conventional). J Trauma 69(6):1501–1506 Epub 2010/06/08
Gautier E, Bachler R, Heini PF, Nolte LP (2001) Accuracy of computer-guided screw fixation of the sacroiliac joint. Clin Orthop Relat Res 393:310–317
Stockle U, Konig B, Hofstetter R, Nolte LP, Haas NP (2001) Navigation assisted by image conversion. An experimental study on pelvic screw fixation. Unfallchirurg 104(3):215–220
Ebraheim NA, Coombs R, Jackson WT, Rusin JJ (1994) Percutaneous computed tomography-guided stabilization of posterior pelvic fractures. Clin Orthop Relat Res 307:222–228
Goldberg BA, Lindsey RW, Foglar C, Hedrick TD, Miclau T, Hadad JL (1998) Imaging assessment of sacroiliac screw placement relative to the neuroforamen. Spine 23(5):585–589
Barrick EF, O’Mara JW, Lane HE 3rd (1998) Iliosacral screw insertion using computer-assisted CT image guidance: a laboratory study. Comput Aided Surg 3(6):289–296
Tonetti J, Carrat L, Lavallee S, Pittet L, Merloz P, Chirossel JP (1998) Percutaneous iliosacral screw placement using image guided techniques. Clin Orthop Relat Res 354:103–110
Cole JD, Blum DA, Ansel LJ (1996) Outcome after fixation of unstable posterior pelvic ring injuries. Clin Orthop Relat Res 329:160–179
Hinsche AF, Giannoudis PV, Smith RM (2002) Fluoroscopy-based multiplanar image guidance for insertion of sacroiliac screws. Clin Orthop Relat Res 395:135–144
Keating JF, Werier J, Blachut P, Broekhuyse H, Meek RN, O’Brien PJ (1999) Early fixation of the vertically unstable pelvis: the role of iliosacral screw fixation of the posterior lesion. J Orthop Trauma 13(2):107–113
Routt ML Jr, Simonian PT (1996) Closed reduction and percutaneous skeletal fixation of sacral fractures. Clin Orthop Relat Res 329:121–128
Ebraheim NA, Haman SP, Xu R, Stanescu S, Yeasting RA (2000) The lumbosacral nerves in relation to dorsal S1 screw placement and their locations on plain radiographs. Orthopedics 23(3):245–247
Altman DT, Jones CB, Routt ML Jr (1999) Superior gluteal artery injury during iliosacral screw placement. J Orthop Trauma 13(3):220–227
Stephen DJ (1997) Pseudoaneurysm of the superior gluteal arterial system: an unusual cause of pain after a pelvic fracture. J Trauma 43(1):146–149
Templeman D, Schmidt A, Freese J, Weisman I (1996) Proximity of iliosacral screws to neurovascular structures after internal fixation. Clin Orthop Relat Res 329:194–198
van den Bosch EW, van Zwienen CM, van Vugt AB (2002) Fluoroscopic positioning of sacroiliac screws in 88 patients. J Trauma 53(1):44–48
Hanzlik S, Mahabir RC, Baynosa RC, Khiabani KT (2009) Levels of evidence in research published in The journal of bone and joint surgery (American volume) over the last thirty years. J Bone Joint Surg Am 91(2):425–428 Epub 2009/02/03
Majeed SA (1989) Grading the outcome of pelvic fractures. J Bone Joint Surg British Vol 71(2):304–306 Epub 1989/03/01
Rommens PM, Hessmann MH (2002) Staged reconstruction of pelvic ring disruption: differences in morbidity, mortality, radiologic results, and functional outcomes between B1, B2/B3, and C-type lesions. J Orthop Trauma 16(2):92–98 Epub 2002/01/31
Stockle U, Konig B, Schaffler A, Zschernack T, Haas NP (2006) Clinical experience with the Siremobil Iso-C(3D) imaging system in pelvic surgery. Unfallchirurg 109(1):30–40
Arand M, Kinzl L, Gebhard F (2004) Computer-guidance in percutaneous screw stabilization of the iliosacral joint. Clin Orthop Relat Res 422:201–207
Collinge C, Coons D, Tornetta P, Aschenbrenner J (2005) Standard multiplanar fluoroscopy versus a fluoroscopically based navigation system for the percutaneous insertion of iliosacral screws: a cadaver model. J Orthop Trauma 19(4):254–258
Day AC, Stott PM, Boden RA (2007) The accuracy of computer-assisted percutaneous iliosacral screw placement. Clin Orthop Relat Res 463:179–186
Konrad G, Zwingmann J, Kotter E, Sudkamp N, Oberst M (2010) [Variability of the screw position after 3D-navigated sacroiliac screw fixation. Influence of the surgeon’s experience with the navigation technique]. Unfallchirurg 113(1): 29–35. (Epub 2009/10/29). Variabilitat der Schraubenlage bei 3D-navigierter Sakrumverschraubung. Einfluss der operateurspezifischen Navigationserfahrung
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zwingmann, J., Hauschild, O., Bode, G. et al. Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg 133, 1257–1265 (2013). https://doi.org/10.1007/s00402-013-1788-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-013-1788-4