Abstract
Introduction
The purpose of the present study was to determine which factors affect the positional accuracy of iliosacral screws inserted using 3D fluoroscopic navigation. Specifically, we asked: (1) does the screw insertion angle in the coronal and axial planes affect the positional accuracy of iliosacral screw insertion using 3D fluoroscopic navigation? (2) Is the positional accuracy of iliosacral screw insertion using 3D fluoroscopic navigation affected by the type of screw (transsacral versus standard iliosacral), site of screw insertion (S1 versus S2), patient position (supine versus prone), presence of a dysmorphic sacrum, or AO/OTA classification (type B versus C)?
Materials and methods
Twenty-seven patients with AO/OTA type B or C pelvic ring fracture were treated by percutaneous iliosacral screw fixation. A total of 55 screws were inserted into S1 or S2 using 3D fluoroscopic navigation combined with preoperative CT-based planning. The positional accuracy of screw placement was assessed by matching postoperative CT images with preoperative CT images. The distance between the central axis of the inserted screw and that of the planned screw placement was measured in the sagittal plane passing through the center of the vertebral body.
Results
The mean deviation between the planned and the inserted screw position was 2.9 ± 1.7 mm (range 0–8.5 mm) at the vertebral body center. Multiple regression analysis showed that the screw insertion angle relative to the vertical line of the bone surface in the axial plane (β = 0.354, p = 0.013) and the use of a transsacral screw (β = 0.317, p = 0.017) were correlated with the positional accuracy of screw placement (adjusted R2 = 0.276, p = 0.002).
Conclusions
A greater screw insertion angle relative to the vertical line on the bone surface and the use of transsacral screws increases the positional error of iliosacral screws inserted using 3D fluoroscopic navigation.
Level of evidence
Level IV, therapeutic study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Iliosacral screw fixation under fluoroscopic guidance has become a popular technique to stabilize unstable pelvic ring fractures [1,2,3]. However, this method requires detailed knowledge and experience to correlate the osseous landmarks of the sacrum with their corresponding fluoroscopic images, and to determine a secure screw corridor by rotating the inlet, outlet, and lateral fluoroscopic views. Several factors reportedly increase the risk of screw malpositioning, including the presence of a dysmorphic sacrum [4], the use of S2 screws [5], the number of S1 screws [6], the extent of the dislocation [6], and the surgeon’s experience [6, 7].
To make iliosacral screw fixation under fluoroscopic guidance safe and reliable, various computer-assisted techniques have been developed; however, even the use of a three-dimensional (3D) fluoroscopic navigation system does not guarantee correct screw placement [8]. The factors influencing the accuracy of iliosacral screw placement using 3D fluoroscopic navigation remain unclarified. The purpose of the present study was to determine the factors that influence the positional accuracy of iliosacral screw insertion using 3D fluoroscopic navigation relative to the preoperative CT-based plan.
Patients and methods
Study design and setting
This was a retrospective cohort study performed in a single level 1 trauma center after approval by the institutional review board (no. 17,311).
Patients
From 2011 to 2016, 28 patients with pelvic ring fracture were treated operatively in our hospital. Pelvic ring fractures were classified according to the AO-Müller/Orthopaedic Trauma Association (AO-OTA) classification [9] as type B1 in three patients, B2 in seven patients, B3 in one patient, C1 in 11 patients, C2 in one patient, and C3 in five patients. One C1 pelvic ring fracture was treated with an anterior sacroiliac plate, as it was a sacroiliac joint dislocation with a large crescent iliac fracture [10]. The remaining 27 patients were treated by percutaneous iliosacral screw fixation and were included as the subjects of the present study. A total of 55 screws were inserted. In the present study, an iliosacral screw stabilizing a unilateral sacroiliac joint was defined as a standard iliosacral screw, and an iliosacral screw stabilizing bilateral sacroiliac joints was defined as a transsacral screw. A unilateral standard iliosacral screw was inserted into S1 in 20 patients, and into S2 in 17 patients. Bilateral standard iliosacral screws were inserted into S1 in three patients. A transsacral screw was inserted into S1 in three patients, and into S2 in seven patients. Two transsacral screws were inserted into S1 in one patient. Twelve sacra (44%) were classified as dysmorphic based on the criteria described by Routt et al. [11].
Preoperative planning
A preoperative CT scan was performed with a 64-line, spiral, HR-CT (Aquilion One, Toshiba Medical Systems, Otawara, Japan) in 1-mm slices. The navigation procedure was performed using a computer navigation system (Stryker Navigation System II-Cart, Stryker, Kalamazoo, MI, USA) and a mobile 3D C-arm equipped with a flat-panel detector (Ziehm Vision FD Vario 3D, Ziehm Imaging, Nuremberg, Germany). The screw position was planned preoperatively using CT-based planning software (OrthoMap 3D, Stryker, Kalamazoo, MI, USA) within the navigation unit. During preoperative CT-based planning, three orthogonal reconstructions were viewed along the planned screw axis. In the sagittal reconstructed plane passing through the nerve root tunnel, the screw position was adjusted to keep the safety margin more than 3 mm from the upper cortical alar and the S1 and S2 nerve root tunnels. Preoperative computed tomography (CT)-based planning of screw insertion was combined with 3D fluoroscopic navigation using an image registration technique [12].
Surgical procedures
The surgical procedure was performed as reported previously [12]. Briefly, the patients were placed in supine or prone position on the radiolucent operating table or the traction table. The navigation computer was placed at each patient’s caudal side. The mobile 3D C-arm approached from the opposite side to the operating surgeon. A reference tracker was fixed to the contralateral anterior or posterior iliac crest using two 4-mm diameter pins (The Apex Pin, Stryker Osteosynthesis, Selzach, Switzerland). The C-arm was connected to the navigation system and calibrated by registering three points on the detector using a pointing device. Intraoperative 3D fluoroscopy scan of the sacrum was performed, with the scan center aimed at the S2 vertebral body. Image matching between the preoperative CT data and the intraoperative 3D fluoroscopic image volume was done after the image data were transferred to the navigation system. The guidewire sleeve was calibrated, and then a guidewire was placed into the S1 and S2 vertebrae according to the preoperative plan with the navigated sleeve while viewing the navigation monitor. The guidewire was advanced until it penetrated the iliosacral joint. The wire placement was checked fluoroscopically on the inlet and outlet views. For iliosacral screw fixation, cannulated 6.5-mm or 8.0-mm diameter partial thread screws (ACE Titanium Cannulated Cancellous Screw, Japan Medical Dynamic Marketing, Inc., Tokyo, Japan or ASNIS III Titanium Cannulated Cancellous Screw, Stryker Japan K.K., Tokyo, Japan) were used; the guidewire diameter for these screws was 3.2 mm. For transsacral screw fixation, cannulated 6.5-mm diameter fully threaded screws (Meira Inc., Nagoya, Japan) were inserted; the guidewire diameter for these screws was 2.8 mm.
Postoperative evaluation
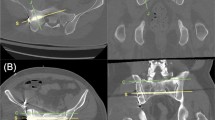
A postoperative CT scan was performed within 1 week after surgery, using the same scan protocol as for the preoperative CT scan. To assess the positional accuracy of the screws placed using the navigation system, the postoperative sacral CT images were matched to preoperative images by maximization of mutual information, and the planned virtual screws were superimposed on the postoperative CT images. The distance between the center of the inserted screw and that of the planned screw was measured in the mid-sagittal plane passing through the center of the vertebral body (Fig. 1).
Preoperatively planned placements of virtual screws (yellow and pink bars) were superimposed on the postoperative computed tomographic images (a) by computational image matching between preoperative and postoperative sacral computed tomographic images. The distance between the center of the inserted screw and that of the planned screw (yellow circle) was measured in the mid-sagittal plane passing through the center of vertebral body (b)
The following seven factors that could potentially have affected the accuracy of screw insertion using navigation were evaluated: the planned screw insertion angle with the vertical axis relative to the iliac cortical surface in the coronal and axial planes (Fig. 2), AO/OTA fracture classification (type B or C), sacral morphology (normal or dysmorphic), site of screw insertion (S1 or S2), patient position (supine or prone), and type of screw (standard iliosacral or transsacral).
To assess the intra- and interobserver reliabilities of screw positional accuracy measurements and screw insertion angle measurements, two assessors (MT and HH) independently measured the positional accuracy and insertion angle of 10 randomly selected screws twice. Intraobserver reliability was calculated using both the first and second measurements. Each assessor’s first measurement was used to calculate the interobserver reliability to control for any learning effect. To determine the reliability of measurements between observers, intraclass correlation coefficients (ICCs) were calculated using a two-way random effects model and absolute agreement type. The ICCs for intraobserver reliability of screw positional accuracy measurements were 0.99 (95% confidence interval (CI) 0.97–0.99) and 0.99 (95% CI 0.99–0.99); the ICC for interobserver reliability was 0.98 (95% CI 0.95–0.99). The ICCs for intraobserver reliability of screw insertion angle measurements were 0.98 (95% CI 0.94–0.99) and 0.98 (95% CI 0.93–0.99); the ICC for interobserver reliability was 0.97 (95% CI 0.89–0.99).
Two assessors (MT and HH) independently performed the postoperative CT-based analyses of screw localization. Perforations were graded according to an established classification method used for pedicle screw placement: grade 0 indicated no perforation, grade 1 indicated a perforation of less than 2 mm, grade 2 indicated a perforation of 2–4 mm, and grade 3 indicated a perforation of greater than 4 mm [13]. The perforation grades determined by the two assessors were identical in all cases.
Statistical analysis
The Mann–Whitney U test was used to compare the positional error of screw placements between two groups classified by each categorical parameter. The Wilcoxon signed-rank test was used to compare the cranial and anterior deviations from the planned screw position. The linear correlation between the positional error and the screw insertion angle was assessed using the Spearman rank correlation test. P values of < 0.05 were considered significant. All seven factors that could potentially have affected the accuracy of screw positioning were reevaluated using multiple regression analysis. The minimum required sample size for the multiple regression analysis was calculated as 49, given the desired probability level of 0.05, the number of predictors in the model (7), the anticipated effect size (0.35), and the desired statistical power level of 0.8. Analyses were performed using IBM SPSS Statistics Version 23 (IBM Corp., Armonk, NY, USA).
Results
The mean deviation between the planned and the actual inserted screw position was 2.9 ± 1.7 mm at the vertebral body center (Fig. 3). The cranial deviation from the planned screw position was 0.1 ± 2.2 mm, and the anterior deviation from the planned screw position was − 0.6 ± 2.4 mm. There was no significant difference between the cranial and anterior components of the screw position deviation (p = 0.089). In the univariate analysis, the accuracy of screw positioning was affected by the AO/OTA fracture classification, patient position, and type of screw (Table 1). The screw insertion angle in the axial plane correlated with the deviation of the screw position at the vertebral body center (Table 2) (Fig. 4). Multiple regression analysis showed that the screw insertion angle in the axial plane and the use of a transsacral screw correlated with the positional accuracy of screws (Table 3).
Scatter diagram showing the correlation between the screw insertion angle in the axial plane and the positional error of screws with the regression line (solid line) and the 95% confidence interval for the regression line (dashed lines). The black closed circles correspond to screws with perforation
One standard iliosacral screw inserted in a normal S2 vertebra with a type B fracture showed grade 1 perforation (< 2 mm). One of two transsacral screws inserted into a normal S1 vertebra with a type C fracture showed grade 2 perforation (2–4 mm). Both these screws that showed perforation were inserted with the patient in the supine position. The screw insertion angles of the malpositioned screws in the axial plane were 35° and 40°, respectively. There were no postoperative complications, including nerve palsy.
Discussion
Using 3D fluoroscopic navigation reportedly results in lower rates of malpositioning of iliosacral screws compared with conventional fluoroscopic guidance [14,15,16] and 2D fluoroscopic navigation [16, 17]. However, the malposition rate associated with 3D fluoroscopic navigation reportedly ranges from 0 to 31%, when malpositioning is defined as perforation of grade 1 or more [14,15,16, 18] (Table 4). This means that there is still room for improvement in the accuracy of 3D fluoroscopic navigation for the insertion of iliosacral screws. To the best of our knowledge, no study has investigated the risk factors for screw malpositioning using 3D fluoroscopic navigation. The present study found that the risk factors for inaccurate positioning of iliosacral screws inserted using 3D fluoroscopic navigation were the screw insertion angle in the axial plane and the use of transsacral screws.
This study had a number of limitations. First, the number of patients was small. However, we inserted both S1 and S2 screws in 24 of 27 patients to achieve rotational stability of the fracture sites. As a result, a total of 55 screws were inserted using the navigation system, which was a sufficient number for statistical analysis of the positional accuracy of screws according to the sample power analysis. Second, the preoperative CT-based planning was combined with 3D fluoroscopic imaging to enable insertion of the iliosacral screws with a sufficient safe bony margin. Thus, the navigational accuracy might be different in other studies using 3D fluoroscopic images only, as the matching error between the preoperative CT images and the intraoperative 3D fluoroscopic images should be considered. A previous experimental study reported a matching accuracy of 1.2 mm [12].
We measured the deviation of the planned screw axis from the vertical axis on the bone surface in the coronal and axial planes. Greater deviation from the vertical axis was seen in the screw insertion angle in the axial plane compared with that in the coronal plane. The navigation system guides the sleeve device for guidewire insertion, not the guidewire or the screw itself, which could be why the screw insertion angle affected the accuracy of screw insertion using the navigation system. Screw perforation was seen in screws with an insertion angle of 35° or more; hence, we recommend predrilling a screw hole using a navigated drilling tool when the screw insertion angle is calculated as 35° or more in preoperative planning. In addition, the flexibility of the guidewire is a concern. The diameter of the guidewire of the standard iliosacral screws was 3.2 mm, and that of the transsacral screws was 2.8 mm, which means that the guidewire of the transsacral screws has more flexibility. This greater guidewire flexibility is, therefore, one possible reason for the greater degree of positional error using transsacral screws. Richter et al. [18] also reported greater screw perforation rates for transsacral screws (45%) than for standard iliosacral screws (4.4%) inserted using navigation combined with robot arm-assisted 3D fluoroscopy.
The presence of an AO-OTA type C fracture was identified in the univariate analysis as a factor influencing the accuracy of screw positioning, but it did not reach statistical significance in the multivariate analysis. In our system, the navigation system tracks movement of the sacral fragment on the contralateral side of the fracture, including the vertebral body and the bilateral neural foramina, so the intraoperative movement of the ipsilateral sacral fragment of the fracture does not influence the navigation positional accuracy around the vertebral body.
The insertion of a screw into S2 is reportedly a risk factor for iliosacral screw malpositioning under fluoroscopic guidance, as the screw corridor for S2 is narrower than for S1 in the normal sacrum [4]. In the present study, although S2 screws were inserted in 24 of 27 patients, the screw perforation rate was not high compared with that reported in other studies using 3D fluoroscopic navigation [14,15,16, 18] (Table 4). In both univariate and multivariate analyses, the use of an S2 screw was not a risk factor for screw malposition. This indicates that 3D fluoroscopic navigation could enable safer screw placement into the S2 vertebra as well as the S1 vertebra.
It has been reported that the screw corridor for the S1 screw is 36% narrower in the dysmorphic sacrum compared with the normal sacrum [4]. Matityahu et al. [16] reported that 3D fluoroscopic navigation enabled safer screw placement into the S1 vertebra, even in dysmorphic sacrum. In our study, the presence of a dysmorphic sacrum was not a risk factor for inaccurate screw insertion into the S1 vertebra.
The number of S1 screws is also reportedly a risk factor for screw perforation [6]. In our study, one grade 2 perforation was seen with one of two transsacral screws inserted into S1 because of a concomitant transverse fracture. This was the only case in the present series with two screws inserted into the S1 vertebra, so the number of S1 screws could not be evaluated as a possible risk factor for screw malpositioning; this case had several risk factors, including the insertion of two screws in the S1 vertebra, the use of a transsacral screw, and a greater insertion angle in the axial plane (40°).
Grossterlinden et al. [19] reported that surgeon experience affects malposition rates in screw placement in cadaveric pelvises, even when using 3D fluoroscopic navigation. It is difficult for less-experienced surgeons to find a safe corridor in the multiple reconstructed planes of 3D fluoroscopic images [7]. In the present series, all screw placements were performed by a single surgeon, so we could not evaluate the effect of surgeon experience on screw position accuracy.
Conclusion
A greater screw insertion angle against the vertical line on the bone surface and the use of transsacral screws increased the positional error of iliosacral screws inserted using 3D fluoroscopic navigation. It is necessary to predrill a screw hole using a navigated drilling tool when preoperative planning indicates that the screw insertion angle is 35° or more.
References
Vanderschot PM, Broens PM, Vermeire JI, Broos PL (1999) Trans iliac-sacral-iliac bar stabilization to treat bilateral sacro-iliac joint disruptions. Injury 30(9):637–640
Matta JM, Saucedo T (1989) Internal fixation of pelvic ring fractures. Clin Orthop Relat Res 242:83–97
Routt ML Jr, Kregor PJ, Simonian PT, Mayo KA (1995) Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma 9(3):207–214
Gardner MJ, Morshed S, Nork SE, Ricci WM, Chip Routt ML Jr (2010) Quantification of the upper and second sacral segment safe zones in normal and dysmorphic sacra. J Orthop Trauma 24(10):622–629. https://doi.org/10.1097/BOT.0b013e3181cf0404
van den Bosch EW, van Zwienen CM, van Vugt AB (2002) Fluoroscopic positioning of sacroiliac screws in 88 patients. J Trauma 53(1):44–48
Grossterlinden L, Rueger J, Catala-Lehnen P, Rupprecht M, Lehmann W, Rucker A, Briem D (2011) Factors influencing the accuracy of iliosacral screw placement in trauma patients. Int Orthop 35(9):1391–1396. https://doi.org/10.1007/s00264-010-1092-7
Takao M, Nishii T, Sakai T, Sugano N (2013) CT-3D-fluoroscopy matching navigation can reduce the malposition rate of iliosacral screw insertion for less-experienced surgeons. J Orthop Trauma 27(12):716–721. https://doi.org/10.1097/BOT.0b013e31828fc4a5
Zwingmann J, Hauschild O, Bode G, Sudkamp NP, Schmal H (2013) Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg 133(9):1257–1265. https://doi.org/10.1007/s00402-013-1788-4
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audige L (2007) Fracture and dislocation classification compendium—2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 21(10 Suppl):S1–S133
Takao M, Nishii T, Sakai T, Sugano N (2014) Navigation-aided visualization of lumbosacral nerves for anterior sacroiliac plate fixation: a case report. Int J Med Robot + Comput Assist Surg: MRCAS 10(2):230–236. https://doi.org/10.1002/rcs.1556
Routt ML Jr, Simonian PT, Agnew SG, Mann FA (1996) Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study. J Orthop Trauma 10(3):171–177
Takao M, Nishii T, Sakai T, Yoshikawa H, Sugano N (2014) Iliosacral screw insertion using CT-3D-fluoroscopy matching navigation. Injury 45(6):988–994. https://doi.org/10.1016/j.injury.2014.01.015
Smith HE, Yuan PS, Sasso R, Papadopolous S, Vaccaro AR (2006) An evaluation of image-guided technologies in the placement of percutaneous iliosacral screws. Spine (Phila Pa 1976) 31(2):234–238
Zwingmann J, Konrad G, Kotter E, Sudkamp NP, Oberst M (2009) Computer-navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin Orthop Relat Res 467(7):1833–1838. https://doi.org/10.1007/s11999-008-0632-6
Zwingmann J, Konrad G, Mehlhorn AT, Sudkamp NP, Oberst M (2010) Percutaneous iliosacral screw insertion: malpositioning and revision rate of screws with regards to application technique (navigated vs. Conventional). J Trauma 69(6):1501–1506. https://doi.org/10.1097/TA.0b013e3181d862db
Matityahu A, Kahler D, Krettek C, Stockle U, Grutzner PA, Messmer P, Ljungqvist J, Gebhard F (2014) Three-dimensional navigation is more accurate than two-dimensional navigation or conventional fluoroscopy for percutaneous sacroiliac screw fixation in the dysmorphic sacrum: a randomized multicenter study. J Orthop Trauma 28(12):707–710. https://doi.org/10.1097/bot.0000000000000092
Thakkar SC, Thakkar RS, Sirisreetreerux N, Carrino JA, Shafiq B, Hasenboehler EA (2017) 2D versus 3D fluoroscopy-based navigation in posterior pelvic fixation: review of the literature on current technology. Int J Comput Assist Radiol Surg 12(1):69–76. https://doi.org/10.1007/s11548-016-1465-5
Richter PH, Gebhard F, Dehner C, Scola A (2016) Accuracy of computer-assisted iliosacral screw placement using a hybrid operating room. Injury 47(2):402–407. https://doi.org/10.1016/j.injury.2015.11.023
Grossterlinden L, Nuechtern J, Begemann PG, Fuhrhop I, Petersen JP, Ruecker A, Rupprecht M, Lehmann W, Schumacher U, Rueger JM, Briem D (2011) Computer-assisted surgery and intraoperative three-dimensional imaging for screw placement in different pelvic regions. J Trauma 71(4):926–932. https://doi.org/10.1097/TA.0b013e31820333dd
Acknowledgements
We thank Prof. Hideki Yoshikawa from Osaka University for his advice and criticism and Kelly Zammit, BVSc, from Edanz Group (http://www.edanzediting.com/ac), for editing a draft of this manuscript.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Takao, M., Hamada, H., Sakai, T. et al. Factors influencing the accuracy of iliosacral screw insertion using 3D fluoroscopic navigation. Arch Orthop Trauma Surg 139, 189–195 (2019). https://doi.org/10.1007/s00402-018-3055-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3055-1