Abstract
Introduction
Data on long-time survival and clinical function of rotating hinge knee prostheses used in revision total knee arthroplasty (TKA) are scarce.
Method
We evaluate the outcome of 42 revision TKA in 38 patients using the Endo-model rotating hinge total knee prosthesis after a minimum of 6 years, with 10-year implant survival as our primary outcome measure. Only revision TKAs performed due to aseptic loosening were included, and the Swedish Knee Arthroplasty Register was consulted in order to ensure that patients unavailable for clinical follow-up had not been revised elsewhere. Mean follow-up was after 8.8 (6–18) years, mean age at revision surgery was 72 (55–88) years, and most patients had severe medical comorbidities (n = 31).
Results
At follow-up, four knees had been re-revised due to aseptic loosening, and five further knees underwent re-revision due to other reasons. With implant revision due to aseptic loosening as the endpoint, 10-year survival was 89.2%, and with implant revision due to any reason 10-year survival was 65.1%. 11 patients (13 knees) eligible for clinical follow-up were evaluated according to the Hospital for Special Surgery score (HSSS), the Knee Society scores (KSS), and by plain radiography. Mean HSSS was 67 (36–90), mean KSS-knee was 85 (73–96), and mean KSS-function was 29 (0–100). Radiography showed that no implant was in need of revision.
Conclusion
Our results indicate that revision arthroplasty of the knee with this rotating hinge prosthesis can be performed with satisfactory or good results in an elderly population with severe comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Historically, the hinged knee prosthesis design represented the first generation of implants in total knee arthroplasty (TKA) [36]. Early loosening, osteolysis, and excessive wear that were due to the highly restricted biomechanics of early hinged designs instigated the development of new devices with rotating hinge mechanics [3, 4]. Rotating hinge implants are still in use even in primary TKA, especially if severe deformities or ligament instability are present [22]. However, since resurfacing devices of the knee dominate in primary TKA, third-generation rotating hinge prostheses are nowadays mostly reserved for difficult revision arthroplasty, salvage procedures after numerous previous surgeries, or tumour surgery.
The amount of revision surgery after TKA has increased in recent years. In the USA, the revision burden for total knee arthroplasty between 1990 and 2002 was 8.2% [17], which is similar to statistics from Sweden [29]. Revision TKA is often performed using unconstrained prosthetic designs. However, the need of more constrained prostheses arises not infrequently in cases of global instability [3, 4, 23], poor soft-tissue balance [1, 30], inadequate alignment of the knee [16, 26, 33], or combined instability and bone loss in rheumatoid arthritis [25]. Even extensor mechanism dysfunction, such as extension lag and dislocation of the patella, can benefit from hinged designs because hinged knee prostheses restore the quadriceps lever arm in knee flexion and improve the lever arm in knee extension [20].
Clinical and radiological results after rotating hinge TKA have previously been reported, but the conclusions are contradictory: Certain authors seem to consider such devices to be useful mainly in salvage procedures after numerous failed revisions [31], whereas others have described encouraging outcomes [2, 11, 12, 15]. Moreover, the existing literature is difficult to interpret because most studies embrace a plethora of different indications for rotating hinge TKA, including aseptic loosening, deep infection, complicated intraarticular fractures, or tumours, to name only the most common causes. Many studies also include patients with very short follow-up, making conclusions on the survival of rotating hinge revision TKA insecure.
At our institution, the Endo-model rotating hinge prosthesis has been in use since 1991, and it is also the most common rotating hinge device in Sweden [34]. Such devices allow for axial rotation between the femoral and tibial components and are therefore thought to reduce forces on the prosthesis anchorage. We have mostly but not exclusively used this implant for difficult revision TKA due to aseptic loosening, deep infection, or intraarticular fractures, and mostly in the presence of severe bone loss, gross hip-knee-angle deviation, or severe ligament instability. It was predominantly chosen in elderly patients.
We performed a retrospective study with the main study objective to perform a minimum 6-year follow-up in order to gain information on implant survival with the endpoints implant revision due to aseptic loosening or due to any reason. Secondary outcome measures were knee function, patient satisfaction, and radiographic results after rotating hinge revision TKA. In order to reduce heterogeneity of the study population, we intended to review only patients operated on the grounds of aseptic loosening, but to exclude patients that received this rotating hinge device due to other reasons.
Patients and methods
Study population and data collection
From 1991 to 2003, 42 revision TKA due to aseptic loosening were performed using the cemented Endo-model rotating hinge TKA (Waldemar Link GmbH & Co, Hamburg, Germany), while unconstrained designs were used in the majority of other revision TKA during this period. The diagnosis of aseptic loosening was based on a thorough clinical and radiographic examination combined with laboratory examinations including leukocyte counts, sedimentation rate, and C-reactive protein. We found no elevation of these parameters in the patients analysed in this study. The procedures were performed in 38 patients (26 women), and four patients had bilateral surgery. Data collection included demographic information, complete medical histories, diagnosis and type of prosthesis used for the initial TKA, indications for revision TKA, and analysis of radiographs prior to and after revision TKA. Furthermore, the Swedish Knee Arthroplasty Register was consulted in order to ensure that deceased patients had not been revised elsewhere, and all 38 patients could be identified. At the time of follow-up, 16 patients (18 knees) of the total cohort had died from unrelated causes. Eleven patients (11 knees) were unable to participate in the clinical follow-up due to advanced age, severe medical comorbidities, or large geographic distances; seven out of these patients were followed up with a telephone interview, and thus only four patients were unavailable at follow-up. Thirteen knees in 11 patients were eligible for both clinical and radiographic follow-up (Table 4).
Surgical procedures
All procedures were carried out following standard revision TKA procedures. Briefly, patients were given cloxacillin (1 g × 3) as peri-operative antibiotic prophylaxis; low-molecular weight heparin (40 mg enoxaparin s.c. ×1 for 10 days) was started the evening before surgery, and spinal anaesthesia rather than general anaesthesia was used in most cases. All procedures were performed through a medial parapatellar arthrotomy, usually under tourniquet control. In a few cases, a rectus snip [9] was required for adequate exposure, and bone allografts were used to restore bone defects if necessary. The patella was not routinely resurfaced, and a lateral release was undertaken when necessary to secure satisfactory patellar tracking. Both components were cemented with cement-containing gentamicin (Palacos R + G®, Heraeus, Hanau, Germany). We used the Endo-Model Link prosthesis with a patellar flange and started including an anti-dislocation mechanism when it was made available by the manufacturer. Therefore, the first nine knees in our series were operated without this device whereas the rest of the knees included an anti-dislocation mechanism.
Clinical outcome measures
Patients available for clinical follow-up were evaluated according to the Hospital for Special Surgery score (HSSS) [14] and the Knee society score (KSS) [13]. Due to the retrospective nature of the study we have no data on pre-operative scores. Anteroposterior and lateral radiographs of the knees were obtained and evaluated by three independent observers, two orthopaedic surgeons and one radiologist, assessing alignment, signs of loosening such as radiolucent lines, osteolysis, and polyethylene wear.
Statistical analysis
Prosthesis survival was analysed using the Kaplan–Meier method, a statistical method that enables calculation of prosthesis survival after a defined period of time (mostly 10-year survival rates are calculated). Calculation of survival rates is possible even if the follow-up time is shorter for a certain cases (so called “right-censoring”) [6]. Follow-up started on the day of revision TKA and ended on the day of re-revision, death, or October 31st, 2009, whichever came first. Survival analysis was performed with revision due to any reason or due to aseptic loosening as the endpoints, and 95% confidence intervals were calculated. The PASW statistics 18 software package was used for all analyses.
Results
Demographics, comorbidities, and previous implants in 38 patients and 42 knees
The mean age at the time of implantation of the rotating hinge prosthesis was 72 (55–88) years, and most patients had significant medical comorbidities at the time of the index procedure (31 patients, see Table 1). Details on the loose prostheses that were removed at the time of implantation of the rotating hinge device are given in Table 2.
Complications, re-revisions, and implant survival in 42 knees
Immediate post-operative complications included two cases of haematoma that required drainage, one superficial dermal necrosis that was treated by a mesh-graft, one myocardial infarction, and one post-operative psychosis. At the time of follow-up, 9 out of 42 rotating hinge prostheses had been re-revised: four were re-revised due to aseptic loosening, and five prostheses underwent re-revision due to other reasons (Table 3). Apart from these implant revisions, three patients underwent re-revisions without implant revision due to periprosthetic fractures or patellar instability: two patients with periprosthetic fractures were operated with open reduction and fixation. One patient developed patellar instability after a trauma resulting in a rupture of the vastus medialis muscle and was operated with a lateral release and medial repair.
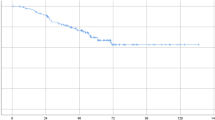
With implant revision due to aseptic loosening as the endpoint, 10-year survival was 89.2%; with implant revision due to any reason 10-year survival was 65.1% (Fig. 1).
Implant survival. a 10-year survival with implant revision due to aseptic loosening as the endpoint was 89.2% (95% confidence interval 77.4–100%; 2 patients at risk). b 10-year survival with implant revision due to any reason as the endpoint was 65.1% (95% confidence interval 40.8–89.4%; 2 patients at risk)
Clinical and radiographic outcome at follow-up in 13 knees
The mean follow-up of the available knees was after 8.8 (6–18) years. The mean HSSS at follow-up was 67 (36–90), the mean KSS-knee was 85 (73–96), and the mean KSS-function was 29 (0–100). Mean knee flexion was 108° (100–120). Of the 18 patients available for either clinical investigation or telephone interview 17 patients claimed that they were satisfied with their knee function, whereas 1 was not satisfied (Table 4).
Radiographic evaluation showed well-fixed implants without radiolucencies (n = 8) or discrete radiolucent lines without progression (n = 5), and no implant was deemed to be in need of revision.
Discussion
The frequency of revision TKA is increasing, and many knee surgeons recommend that unconstrained revision designs should be used in such procedures, not least due to the problems associated with hinged TKA prostheses. However, to our knowledge, there are no controlled studies that demonstrate superiority of the unconstrained approach over rotating hinge prostheses. We have used a rotating hinge device since 1991 in difficult revision TKA in mostly elderly patients, and have now performed a minimum 6-year follow-up of consecutive 42 revision TKA performed due to aseptic loosening of a previous knee prosthesis. We are not aware of other studies reporting on implant survival after rotating hinge revision TKA performed solely due to aseptic loosening and with a minimum follow-up of 6 years.
It was our main objective to investigate implant survival after revision TKA using the Endo-model rotating hinge device. Our results on prosthesis survival after this procedure compare rather favourably with some of the early literature reporting on the clinical outcome after such procedures: For instance, a rate of femoral loosening of 5% after only 2 years and a significant incidence of complications have been reported after the use of different rotating hinge designs [19, 27, 35], and it has even been suggested that “hinged total knee arthroplasty should be reserved for the final salvage option […]” [31].
Our secondary outcome measures were patient satisfaction, knee function, and radiographic appearance in the surviving patients, and we found good to satisfactory results in the patients available for clinical follow-up. Other authors have also presented relatively good knee function after rotating hinge revision TKA: For instance, a postoperative Knee Society Clinical Score of 131 after a mean follow-up of 51 months has been reported, but this study only involved 14 knees operated with a second-generation rotating hinge device [5]. Furthermore, in a retrospective review of 349 revision TKA it was described that the rotating hinge prosthesis provided similar patient satisfaction and survivorship when compared with non-hinged implants [11]. A further study comparing different implant types in revision TKA found no significant differences between implant types with regard to Knee society scores [12]. Another study on 11 knees with Charcot arthropathy showed satisfactory clinical results for most cases [2]. 78 revision TKA using the Endo-model rotating hinge prosthesis with a mean follow-up of 7.8 years (range 4.7–10.8) obtained excellent or good results in 82%, but in that study, a large proportion of revision procedures was performed due to other reasons than aseptic loosening [15]. Moreover, 19 prostheses in that series were rated as failures. Other reports on rotating hinge devices in revision TKA include a description of the Endo-model prosthesis followed for a mean of 4 years, but in that series of 51 knees only 23 were operated on the basis of aseptic loosening of the previous implant [24]. An interesting report on the Endo-model prosthesis combined with impaction grafting in revision TKA of patients with severe bone loss has described encouraging results, although 5 of 30 patients in that study had to be revised due to aseptic loosening [32]. Finally, a series of different rotating hinge devices including 30 Endo-model rotating hinge prostheses was described to have achieved satisfactory results in approximately 80% of the cases, supporting the authors’ suggestion of continued use of this implant in difficult revision TKA [28].
An incidence of extensor mechanism complications of around 10% has been described after revision TKA [27, 31]. In our series, two patients had extensor dysfunction (see above), and the frequency of this complication seems to be within the range of what other authors have reported after revision TKA using rotating hinge devices [5, 15].
There were a few patients that sustained periprosthetic fractures. This is not an entirely unexpected phenomenon in an aged, osteoporotic population. In addition, the more constrained the prosthesis, the higher the fracture risk. In our cases plate osteosynthesis gave excellent results.
Unfortunately, one of our patients dislocated her revision knee prosthesis after 7 years and had to be treated with open reduction. A review of the literature with a focus on the incidence of dislocations of hinged knee prostheses reveals that this is a well-known complication with different hinged designs [7, 8, 27, 37, 38]. At least five cases of femorotibial disconnection of the Endo-model rotating hinge prosthesis have also been reported [15, 21, 37]. Open reduction and exchange of the connecting device has been described as the solution in such cases [18].
The number of points achieved by our patients in the KSS function part seems disappointingly low at first glance, in particular when compared with a postoperative KSS function of 45 points reported by other authors [39]. In that study, however, 9 of 24 knees were primary TKA in younger patients. It has to be remembered that our patients were elderly already at the time of revision surgery and suffered from numerous medical comorbidities. For instance, two of our patients need a wheel-chair due to problems unrelated to their knee revision surgery. Other authors have suggested that one of the factors that leads to poor functional results was the number of associated comorbidities [10]. The relatively low number of points in the KSS function part in our patients is thus mostly explained by comorbidities that impair general mobility, an interpretation that is strengthened by the relatively high KSS knee scores that they achieved. Therefore, we agree that a patient satisfaction questionnaire should be used in conjunction with traditional knee scores for evaluation of outcome of complex, salvage revision knee surgery [24].
A weakness of our study is that many patients were lost to clinical follow-up, mainly due to death from unrelated causes, but in some instances due to the inability to attend a clinical appointment at our unit. The inability to attend was chiefly due to advanced age, the presence of severe medical comorbidities, and—last but not least—large geographic distances, which is related to the fact that our unit is a tertiary referral centre. We attempted to reach all patients who were unable or unwilling to attend for a telephone interview, and we can therefore confirm that among those the majority was satisfied with their operated knee. By contacting the Swedish National Knee Arthroplasty Register we were also able to rule out the possibility that deceased patients or those who were unable to attend had required re-revision of their rotating hinge device elsewhere.
Another possible point of criticism is the absence of pre-operative Knee society score that, due to the retrospective nature of this study, was unavailable.
Finally, we analysed a relatively low number of cases altogether. We could have substantially enhanced this number by including all patients that received a rotating hinge TKA during the investigated time period at our unit. However, we believe that information on a distinct and well-defined group of patients that—as in this study—were operated solely on the basis of aseptic loosening of a previous TKA makes the results more readily interpretable. We could also have included a large number of patients operated upon from 2003 onward, but it was our intention to perform a minimum 6-year follow-up.
Conclusion
The primary outcome measure of this study was implant survival: We found that with revision due to aseptic loosening as the endpoint 10-year implant survival was 89.2%, and with implant revision due to any reason 10-year survival was 65.1%. Secondary outcome measures were knee function, patient satisfaction, and radiographic outcome. Knee function was good to satisfactory in a majority of the surviving patients, whereas global function scores in this elderly population were impaired. Radiography revealed no impending revisions. Our findings indicate that revision TKA with the Endo-model rotating hinge device can be performed with satisfactory or even good results in an aged population with a high degree of medical comorbidities, but the difficulties with revision TKA in such patients are also highlighted. Further studies that directly compare rotating hinge devices with unconstrained designs in revision TKA are warranted.
References
Ayers DC, Dennis DA, Johanson NA, Pellegrini VD (1997) Common complications of total knee arthroplasty. J Bone Joint Surg Am 79A(2):278–311
Bae DK, Song SJ, Yoon KH, Noh JH (2009) Long-term outcome of total knee arthroplasty in charcot joint. J Arthroplast 24(8):1152–1156
Barrack RL (2001) Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res 392:292–299
Barrack RL (2002) Rise of the rotating hinge in revision total knee arthroplasty. Orthopedics 25(10):1020–1058
Barrack RL, Lyons TR, Ingraham RQ, Johnson JC (2000) The use of a modular rotating hinge component in salvage revision total knee arthroplasty. J Arthroplast 15(7):858–866
Biau DJ, Latouche A, Porcher R (2007) Competing events influence estimated survival probability: When is Kaplan-Meier analysis appropriate? Clin Orthop Relat Res 462:229–233
Crova M, Cenna E, Olivero C (2000) Rotating knee prosthesis. Surface or hinge replacement? Orthopäde 29(Suppl 1):S43–S44
David HG, Bishay M, James ET (1998) Problems with the rotaflex: a 10 year review of a rotating hinge prosthesis. J Arthroplast 13(4):402–408
Garvin KL, Scuderi G, Insall JN (1995) Evolution of the quadriceps snip. Clin Orthop Relat Res 321:131–137
Guenoun B, Latargez L, Freslon M, Defossez G, Salas N, Gayet LE (2009) Complications following rotating hinge endo-modell (link) knee arthroplasty. Orthop Traumatol Surg Res 95(7):529–536
Hossain F, Haddad FS (2010) Midterm assessment of causes and results of revision total knee arthroplasty. Clin Orthop Relat Res 468:1221–1228
Hwang SC, Kong JY, Nam DC, Kim DH, Park HB, Jeong ST, Cho SH (2010) Revision total knee arthroplasty with a cemented posterior stabilized, condylar constrained or fully constrained prosthesis: a minimum 2-year follow-up analysis. Clinics Orthop Surg 2(2):112–120
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Insall JN, Ranawat CS, Aglietti P, Shine J (1976) A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am 58(6):754–765
Joshi N, Navarro-Quilis A (2008) Is there a place for rotating-hinge arthroplasty in knee revision surgery for aseptic loosening? J Arthroplast 23(8):1204–1211
Karachalios T, Sarangi PP, Newman JH (1994) Severe varus and valgus deformities treated by total knee arthroplasty. J Bone Joint Surg Br 76(6):938–942
Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M (2005) Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am 87(7):1487–1497
Linhardt O, Anders S, Grifka J, Lerch K (2005) Treatment of mechanical damage of the rotating endo-model knee prosthesis. Orthopäde 34(2):167–170
Lombardi AV Jr, Mallory TH, Eberle RW, Adams JB (1997) Rotating hinge prosthesis in revision total knee arthroplasty: Indications and results. Surg Technol Int 6:379–382
Ostermeier S, Friesecke C, Fricke S, Hurschler C, Stukenborg-Colsman C (2008) Quadriceps force during knee extension after non-hinged and hinged tka: an in vitro study. Acta Orthop 79(1):34–38
Pacha-Vicente D, Malik A, Castellet-Feliu E, Nardi-Vilardaga J (2008) Dislocation of rotating-hinge knee prostheses with antidislocation mechanism. J Arthroplast 23(2):299–303
Petrou G, Petrou H, Tilkeridis C, Stavrakis T, Kapetsis T, Kremmidas N, Gavras M (2004) Medium-term results with a primary cemented rotating-hinge total knee replacement. A 7- to 15-year follow-up. J Bone Joint Surg Br 86(6):813–817
Pietsch M, Hofmann S (2007) From tibiofemoral instability to dislocation in total knee arthroplasty. Orthopäde 36(10):917–927
Pradhan NR, Bale L, Kay P, Porter ML (2004) Salvage revision total knee replacement using the endo-model rotating hinge prosthesis. Knee 11(6):469–473
Radmer S, Andresen R, Sparmann M (2007) Knee arthroplasty using the rotating hinge knee prothesis in patients with rheumatoid arthritis. Aktuelle Rheumatologie 32(1):34–39
Ranawat CS, Luessenhop CP, Rodriguez JA (1997) The press-fit condylar modular total knee system. Four-to-six-year results with a posterior-cruciate-substituting design. J Bone Joint Surg Am 79(3):342–348
Rand JA, Chao EY, Stauffer RN (1987) Kinematic rotating-hinge total knee arthroplasty. J Bone Joint Surg Am 69(4):489–497
Rinta-Kiikka I, Alberty A, Savilahti S, Pajamaki J, Tallroth K, Lindholm TS (1997) The clinical and radiological outcome of the rotating hinged knee prostheses in the long term. Ann Chir Gynaecol 86(4):349–356
Robertsson O, Knutson K, Lewold S, Lidgren L (2001) The swedish knee arthroplasty register 1975–1997: an update with special emphasis on 41, 223 knees operated on in 1988–1997. Acta Orthop Scand 72(5):503–513
Sambatakakis A, Wilton TJ, Newton G (1991) Radiographic sign of persistent soft-tissue imbalance after knee replacement. J Bone Joint Surg-Br 73(5):751–756
Springer BD, Hanssen AD, Sim FH, Lewallen DG (2001) The kinematic rotating hinge prosthesis for complex knee arthroplasty. Clin Orthop Relat Res 392:283–291
Steens W, Loehr JF, Wodtke J, Katzer A (2008) Morselized bone grafting in revision arthroplasty of the knee—a retrospective analysis of 34 reconstructions after 2–9 years. Acta Orthopaedica 79(5):683–688
Stern SH, Moeckel BH, Insall JN (1991) Total knee arthroplasty in valgus knees. Clin Orthop Relat Res 273:5–8
Swedish Knee Arthroplasty Register (2008) Annual report. http://www.knee.nko.se/
Walker PS, Manktelow AR (2001) Comparison between a constrained condylar and a rotating hinge in revision knee surgery. Knee 8(4):269–279
Walldius B (1960) Arthroplasty of the knee using an endoprosthesis. 8 years experience. Acta Orthop Scand 30:137–148
Wang CJ, Wang HE (2000) Early catastrophic failure of rotating hinge total knee prosthesis. J Arthroplast 15(3):387–391
Ward WG, Haight D, Ritchie P, Gordon S, Eckardt JJ (2005) Dislocation of rotating hinge knee prostheses. A report of four cases. J Bone Joint Surg Am 87(5):1108–1112
Westrich GH, Mollano AV, Sculco TP, Buly RL, Laskin RS, Windsor R (2000) Rotating hinge total knee arthroplasty in severly affected knees. Clin Orthop Relat Res 379:195–208
Acknowledgments
We thank the Swedish Knee Arthroplasty Register and especially Dr Otto Robertsson for providing information on the patients included in this study. Institutional support has been provided to NPH by Link Sweden AB, Åkersberga, Sweden. The company named above has not been involved in the study design, data collection, data interpretation, or manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gudnason, A., Milbrink, J. & Hailer, N.P. Implant survival and outcome after rotating-hinge total knee revision arthroplasty: a minimum 6-year follow-up. Arch Orthop Trauma Surg 131, 1601–1607 (2011). https://doi.org/10.1007/s00402-011-1330-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-011-1330-5