Abstract
Purpose
This study first analyzes implant survival of this single design modular rotating hinge knee and identifies potential risk factors for failure and evaluates joint function using the postoperative WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) score, active flexion and extension deficit.
Methods
131 prostheses implanted for failure of prior total knee arthroplasty (n = 120) or complex primary procedures (n = 11) using a single modular implant (MUTARS—modular universal tumor and revision system GenuX, Implantcast, Buxtehude, Germany) between 2006 and 2014 including 73 patients treated for periprosthetic joint infection with a two-stage revision protocol were retrospectively identified. Implant survival was assessed using the Kaplan–Meier method; potential risk factors were identified using the log-rank test, as well as non-parametric analysis. Postoperative function was assessed using the WOMAC and measurement of range of motion.
Results
After a median follow-up of 62 months, 37 implants required implant revision (28%). Five-year survival was 69.7% [95% CI (confidence interval) 60.9–78.5] with periprosthetic (re-) infection being the main cause for failure (15%), followed by aseptic loosening (9%). In cases of periprosthetic infection, infection-free survival was 83% at 5 years (95% CI 74–92) with twelve patients suffering reinfection (16%).While body mass index (p = 0.75), age (p = 0.16) or indication for rotating hinge knee arthroplasty (p = 0.25) had no influence on survival, Charlson comorbidity score (CCI) (p = 0.07) and number of previous revision surgeries (p = 0.05) correlated with implant failure. There was trend (p = 0.1) for improved survival in fully cemented implants. Mean postoperative WOMAC was 127(range 55–191), 11 patients (15%) had limited knee extension.
Conclusions
Rotating hinge total knee arthroplasty using a single modular implant shows acceptable survival rates and function compared to previous studies with (re-)infection being the most relevant mode of failure. Patients with a high CCI and multiple previous surgeries are at increased risk for failure.
Level of evidence
Retrospective cohort study, III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgeons performing revision TKA are commonly facing bone loss and ligament instability that regularly requires the use of more constraint prosthesis designs to achieve adequate joint stability [3, 22, 27]. For this purpose hinged knee prostheses have been developed. The first designs using a fixed hinge only achieved low short term survivorship rates up to 60% [1, 14] which led to the development of rotating hinge knee implants (RHK) incorporating significant improvements in design and technology used, particularly its ability to rotate, therefore, reducing the forces transmitted to the bone-cement interface and providing for a greater congruency of the articulating surfaces [1, 11, 20, 21, 27].
While traditionally these implant designs were reserved for oncologic reconstructions [20], current designs offer the advantage of modular components and stems, complex hybrid or cemented fixation and the use of augments to reconstruct massive bone defects that are often encountered [3, 8]. Therefore, rotating hinge designs are not only used in megaprosthetic reconstructions [12], but regularly in non-megaprosthetic revision arthroplasty or complex primary procedures with instability or severe deformity [3, 8, 11, 24,25,26,27].
While there are comprehensive studies reporting implant survivorship of modern, third generation rotating hinge designs to be 52–85% at 5 years [3, 27] to 71–92% at 10 years [3, 13], generalizability of these data can be difficult because differences in implant systems used need to be considered as a confounding factor [18].
The study’s purpose was to investigate implant survival rates of this single-design RHK and identify patient- and surgery-related risk factors for failure and for reinfection in patients treated for PJI, as well as to evaluate joint function through postoperative WOMAC score, active flexion ability, and extension deficit.
Methods
Approval of the institutional review board was obtained prior to this investigation (local ethical committee ref. no. 2018-123-f-S). A specific source of funding was not required in this study. It was conducted according to the principles of the World Medical Association Declaration of Helsinki.
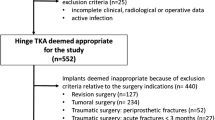
The authors’ institution’s database was retrospectively reviewed and a total of 131 patients who underwent total knee revision arthroplasty (n = 120) or complex primary joint replacement(n = 11) using a single rotating hinge modular knee revision system (MUTARS—modular universal tumor and revision system GenuX, Implantcast GmbH, Buxtehude, Germany) between 2006 and 2014 were identified. Patients with a minimum follow-up period of 24 months were included. Patients who died or developed complications within 24 months following implantation were included as well. Follow-up was derived from the last contact with our institution with seven patients being lost to follow-up and excluded from the study population. Patients who received other (rotating hinge) knee implants, megaprosthetic reconstructions or patients who had reconstructions following primary or metastatic tumor resection were excluded. Functional assessment was performed using the Western Ontario and McMaster Universities Osteoarthritis index [4] that measures pain, stiffness and limitation of function in daily activities as well as measurement of knee range of motion derived from the last clinical examination for all patients with retained implants at latest follow-up. Patients’ previous medical history was analyzed and the Charlson comorbidity index [2] was calculated.
Primary endpoint was defined as prosthetic failure requiring revision and exchange of implant components attached to the host bone (stems, femoral shield, tibial plateau). Secondary endpoints were death, revision with only polyethylene or modular hinge mechanisms exchange and reinfection-free survival for patients treated for periprosthetic joint infection.
Diagnosis of failure and loosening was based on clinical and radiological findings as proposed by the Knee Society’s evaluation system with three views that defines zones around the tibial and femoral components identifying radiolucent lines and their progression in these areas [7]. Joint aspiration was performed in all knees prior to revision surgery and infection was diagnosed using the criteria of the Musculoskeletal Infection Society (MSIS) that asses fistula, positive cultures as well as different serum and synovial markers [21]. Treatment success after staged revision in cases of periprosthetic joint infection was defined based on the Delphi consensus criteria [5, 28] listing reinfection or persistent infection, unhealed wounds or sinus tracts, unplanned surgical intervention for infection and PJI related mortality as reasons for failure.
In cases of revision TKA, previous revision surgeries were analyzed and counted. For septic revision surgeries all previous surgeries for PJI were counted including debridement and component exchanges, one-stage revisions and two-stage revisions with the latter being counted as one exchange.
Surgical procedures and implant features
Surgeries were performed by a senior orthopedic surgeon with special expertise in revision arthroplasty. During the course of the study four different senior surgeons performed the surgeries. A standard medial parapatellar approach was performed in all patients. In case of revision surgery existing components were carefully removed and a thorough debridement was performed removing bradytrophic tissue in cases of infection in all compartments of the knee. In all revisions, a minimum of 3 to 5 microbiological samples were taken and cultured for a minimum of 7–14 days. Intraoperative antibiotics (2nd generation cephalosporin) were withheld until samples were obtained. The implant system used offers multiple reconstruction options with stems, offset adapters and wedges to reconstruct the joint line anatomically. The general approach regarding the use of cement was to perform a “hybrid” fixation cementing the femoral shield and the tibial plateau with a cementless stem whenever possible, but as shown in Table 1 stems were cemented when diminished bone quality was encountered or if only a short stem anchorage due to ipsilateral hardware or diaphyseal deformity was achievable. In planned aseptic revisions gentamicin and clindamycin polymethylmethacrylate (PMMA) bone-cement was used (Copal G+C, Heraeus medical, Wehrheim, Germany) and in cases of resistant bacteria in septic revisions gentamicin and vancomycin PMMA (Copal G+V, Heraeus medical, Wehrheim, Germany) was used. All cases of infection underwent at least 2 weeks of tailored intravenous antibiotics then continuing oral antibiotics for a total of at least 6 weeks in between stages. Antibiotic suppression was not used. Patients’ characteristics are presented in Tables 1 and 2.
Statistical analysis
Data collection and statistical analysis were performed using Excel (Microsoft Corporation, Redmont, Washington, USA) and SPSS Statistics for Windows Version 25 (IBM Corporation, Armonk, NY, USA). All patient records were anonymized prior to analysis.
Descriptive statistics were used to analyze distribution of data, means and ranges were calculated for parametric data; medians and interquartile ranges (IQR) for non-parametric data. Survival analysis was performed using the Kaplan–Meier method [16], differences in survival and influencing factors were assessed using the log-rank test [19]. 95% confidence intervals (CI) were calculated. Contingency tables were analyzed using the χ2-test. Non-parametric analyses were performed using the Mann–Whitney U test. Statistical significance was defined as p ≤ 0.05. A sample size calculation was not performed given the retrospective nature of the study and the fact that the implant system analyzed is no longer used in our department and has been replaced limiting the number of patients available (Fig. 1).
Results
Implant survivorship
The cumulative implant survival rate with implant removal for any cause as the primary endpoint was 91.3% after 2 years (95% CI 86.4–96.2), 69.7% after 5 years (95% CI 60.9–78.5) (Fig. 2).
At the latest follow-up evaluation, 37 implants had to be removed (28%). Reasons for implant removal were periprosthetic joint infection in 20 cases (15%), aseptic loosening in 12 cases (9%), non-reconstructable extensor mechanism deficiency requiring arthrodesis in 3 cases (2%) and periprosthetic fracture in 2 cases (2%). Implant failure occurred after a median of 28 months (IQR 21–47). Postoperative complications that could be treated without implant revision included five hematomas (3.8%), three periprosthetic fractures that were revised with plating (2.2%) and three patella tendon deficiencies (2.2%) that underwent tendon augmentation surgery.
11 patients died during the follow-up period of unrelated cause to our knowledge after a median of 25 months (IQR 15 to 59) although two of these patients underwent revision surgery during the follow-up period. One of these patients was revised due to periprosthetic femoral fracture 6 months after reimplantation in two-stage revision for PJI and the other patient due to low-grade reinfection 23 months after successful reimplantation in two-stage revision for PJI.
The total number of previous surgeries was found to be significantly associated with implant failure (p = 0.047). Patients that required TKA revision had a median of 2 (IQR 1.5–4) previous surgeries compared to a median of 2 (IQR 1–3) in patients with retained prosthesis. Further factors are shown in Table 3. Furthermore, there was a trend for a higher median Charlson comorbidity index in patients in whom the implant needed to be removed (3 vs. 4, p = 0.07).
Aseptic loosening
The cumulative incidence of aseptic loosening was 11% at last follow-up (95% CI 5–17) with all cases of aseptic loosening occurring within 4.7 years postoperative. Isolated loosening of either the tibial or femoral component was found in five patients each, with two patients having loosening of the entire prosthesis. In regard to factors that correlate with aseptic loosening, patient aged over 70 years had a reduced probability of revision for aseptic loosening (6 vs. 18%, p = 0.058) as well as fully cemented implants (0 vs. 14%, p = 0.06).
Periprosthetic reinfection
A total of twelve patients that were treated for PJI suffered reinfection (16%). The infection-free survival was 83% at 5-years (95% CI 74–92). We were not able to identify significant risk factors for reinfection (Table 4), furthermore differences in the Charlson comorbidity index were not associated with reinfection (n.s.).
Functional outcome
In 71 patients functional scores were retrospectively available. The mean WOMAC was 127 (range 55–191). While on the one hand the median active flexion was 90° (IQR 90–100), a deficit in active extension (median 5°, IQR 5–10) was noted in 11 patients (15%), although there was no significant difference in postoperative clinical scores in these patients (p = 0.58). There was no correlation between functional outcome and age (n.s.), BMI (n.s.), indication for RHK implantation in revision cases (n.s.) or mode of implant fixation (n.s.).
Patients who underwent primary TKA using a rotating hinge implant reported a postoperative WOMAC of a median of 103 (IQR 71–131), while in comparison a trend (p = 0.08) for a reduced postoperative functional outcome in patients with revision TKA with a median WOMAC of 129 (IQR 100–162) could be identified.
Discussion
The most important finding in this study is that the implant system used leads to an acceptable 5-year implant survivorship of 69.7% with an infection-free survival of 83% of cases that were treated for PJI. The numbers of previous implant revision surgeries as well as a high comorbidity score were associated with a higher probability of implant failure.
The survivorship of rotating hinge design total knee replacements for non-oncologic indications and the impact of patient- and surgery-related factors is still unclear with reported survival rates greatly varying. No study has analyzed the survivorship of this implant system. A limitation to the existing literature is heterogeneity of implants used in studies that report on RHK.
The overall implant survivorship in the present study was found to be 69.7% at 5 years which is comparable to a study by Farid et al. [8] of 141 single design RHK(OSS model, Biomet, Warsaw, Indiana, USA) who report a 5-year survival of 73% with a comparably high percentage of infection cases(42%) although the authors depict a knee system in their study that would qualify as a megaprostheses in our definition and can’t be compared to the design included in this study. Though the indication for revision surgery was not found to be a significant risk factor for failure in any comparably large study [8, 13, 26], it is discussed that due to the necessity of soft tissue debridement and possibly associated requirement for flap coverage a stable rotating hinge design provides the most durable mode of reconstruction [8, 13] in cases of PJI. This is supported by superior functional results in patients with moderate bone defects that underwent revision TKA utilizing a rotating hinge design following infection compared to other unlinked constraint implants [26].
Mid- to long-term eradication of infection was achieved in 84% of all patients treated for PJI in the present study. In a two-stage revision protocol this is also comparable to the study by Farid et al. [8] who report a reinfection rate of 18% with an overall rate of infection of 15% which is the same as in this study. While these results are favorable in comparison to a study by Smith [27] who report an overall infection rate of 23.7% for their RHK cohort although a reinfection rate is not provided. However, the rate of infection in a large study by Hossain [13] including 74 RHK with 32% of all TKA revision performed for periprosthetic joint infection was only 2.7% in the entire group. A separate rate of reinfection was not provided, but given only two cases of infection in the entire cohort, it most likely is quite low as well. It is to be noted that overall implant survival at 10 years was over 90% for RHK designs in this study and superior to other less constraint prostheses used in the cited study. One possible explanation for limited survivorship might be the high number of previous surgeries in the present study that were found to be a significant risk factor for failure. In this context one has to acknowledge a certain selection bias for patients with PJI and failed prior surgery with debridement and component exchange that were referred for staged revision. Previous surgeries lead to reduced local tissue quality creating a poor environment especially in cases of PJI [3, 9, 22] with some authors suspecting that many aseptic revisions are actually undetected periprosthetic infections that might explain a higher percentage of septic failures [8]. Additionally, particularly in cases of PJI [22] patient related risk factors must be considered as they pose as a predictor of failure. While BMI was not associated with implant failure in this study, the CCI was significantly higher which is in line with previous data on septic knee revision [22].
While periprosthetic infection appears to be the main reason for failure in current TKA [17], aseptic loosening in contemporary rotating hinge design appears to be less common [27] with rates of aseptic loosening of 4.5% after 10 years [3] and 2.7% after a mean of 67 months [13] reported. The rate of aseptic loosening in the present study is higher, but also in line with other previous studies [8]. While this can be partially attributed to the number of previous surgeries, one must discuss implant fixation [6]. While Cottino et al. [3] found a trend for improved survival after using uncemented porous metal cones in revision TKA to improve metaphyseal component anchorage, the authors acknowledge a bias that these cones were used in the most difficult cases and no analysis of outcome with respect to defect size was performed. The use of augments and cones was not analyzed in the present study because of heterogeneity in implant choice and only 8 cases available, although cones and sleeves generallyplay a vital role especially in tibial bone loss and have certainly broadened the armamentarium facing substantial bone loss [15].
Furthermore, implant fixation in RHK designs is greatly dependent on the use of either cemented or uncemented stems [6, 10] with full cementation showing a trend for improved implant survival although rarely used exclusively in older patients. The general approach is the use of an uncemented stems with diaphyseal anchorage combined with offset couplers to restore alignment and facilitate revision surgery facing the still considerable re-revision rate of these implants that would require extensive removal of cement in cases of infection [9, 10, 22]. In contrast, comparably sized studies on RHK designs that report much lower rates of aseptic loosening than the present study relied on cemented stem fixation [3, 13], while Farid et al. [8] who also employed full cementation only in cases of reduced bone quality, reports a rate of loosening comparable to the results presented. However, in the literature there is no consensus on which mode of stem fixation should be used [6, 10] and generalizability of registry studies [23] and other series [29] that favor hybrid fixation is difficult due to heterogenic implant designs without hinged knees and multiple different indications for revision. For future studies, details on metaphyseal bone defects, use of augments, length of stems and mode of fixation should be recorded and compared.
While this is a single center, single design implant study first reporting outcome of this implant with a high percentage of patients treated for periprosthetic joint infection and a median follow-up period of over 5 years, there are limitations to this study: it is limited by its retrospective design with possible recall and selection bias with some patients being lost to follow-up and complications that were treated at an outside hospital not being available for analysis. Additionally, a comprehensive discussion of fixation methods and possible use of augments is hindered by the lack of a uniform bone defect classification. While functional results are acceptable compared to the literature, the lack of preoperative patient reported outcome scores makes the assessment of an improvement impossible. As periprosthetic joint infection is a main cause of concern in revision arthroplasty with treatment and diagnostics constantly evolving, there is a limitation in comparing treatment of historic cases of infection given the diagnostic and therapeutic options nowadays.
It would be desirable for future studies to compare different designs of RHK with large numbers also including condyle replacing implants and distal femoral replacements to see whether there are differences in survival.
Based on the present study’s results patients who undergo TKA using a rotating hinge implant can be counseled more comprehensively regarding the functional and clinical results of these implants and complications that can be expected.
Conclusion
This single design RHK in revision total knee arthroplasty provides acceptable mid- to long-term results compared to the literature although one must be aware of high rates of failure, particularly infection. The number of previous surgeries as well as comorbidity might be associated with increased failure rates, while fully cemented implants showed improved survival.
Abbreviations
- BMI:
-
Body mass index
- CCI:
-
Charlson comorbidity index
- CI:
-
Confidence interval
- IQR:
-
Interquartile range 25–75%
- MSIS:
-
Musculoskeletal infection society
- MUTARS:
-
Modular universal tumor and revision system
- PJI:
-
Periprosthetic joint infection
- PMMA:
-
Polymethylmethacrylate
- RHK:
-
Rotating hinge knee
- TKA:
-
Total knee arthroplasty
- WOMAC:
-
Western Ontario and McMaster universities osteoarthritis index
References
Barrack RL (2001) Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res 392:292–299
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Cottino U, Abdel MP, Perry KI, Mara KC, Lewallen DG, Hanssen AD (2017) Long-term results after total knee arthroplasty with contemporary rotating-hinge prostheses. J Bone Joint Surg Am 99:324–330
Davies GM, Watson DJ, Bellamy N (1999) Comparison of the responsiveness and relative effect size of the western Ontario and McMaster universities osteoarthritis index and the short-form medical outcomes study survey in a randomized, clinical trial of osteoarthritis patients. Arthritis Care Res 12:172–179
Diaz-Ledezma C, Higuera CA, Parvizi J (2013) Success after treatment of periprosthetic joint infection: a Delphi-based international multidisciplinary consensus. Clin Orthop Relat Res 471:2374–2382
Driesman AS, Macaulay W, Schwarzkopf R (2019) Cemented versus cementless stems in revision total knee arthroplasty. J Knee Surg. https://doi.org/10.1055/s-0039-1678686
Ewald FC (1989) The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Farid YR, Thakral R, Finn HA (2015) Intermediate-term results of 142 single-design, rotating-hinge implants: frequent complications may not preclude salvage of severely affected knees. J Arthroplast 30:2173–2180
Fehring KA, Abdel MP, Ollivier M, Mabry TM, Hanssen AD (2017) Repeat two-stage exchange arthroplasty for periprosthetic knee infection is dependent on host grade. J Bone Joint Surg Am 99:19–24
Fleischman AN, Azboy I, Fuery M, Restrepo C, Shao H, Parvizi J (2017) Effect of stem size and fixation method on mechanical failure after revision total knee arthroplasty. J Arthroplast 32:S202–S208
Gehrke T, Kendoff D, Haasper C (2014) The role of hinges in primary total knee replacement. Bone Joint J 96(B):93–95
Holl S, Schlomberg A, Gosheger G, Dieckmann R, Streitbuerger A, Schulz D et al (2012) Distal femur and proximal tibia replacement with megaprosthesis in revision knee arthroplasty: a limb-saving procedure. Knee Surg Sports Traumatol Arthrosc 20:2513–2518
Hossain F, Patel S, Haddad FS (2010) Midterm assessment of causes and results of revision total knee arthroplasty. Clin Orthop Relat Res 468:1221–1228
Inglis AE, Walker PS (1991) Revision of failed knee replacements using fixed-axis hinges. J Bone Joint Surg Br 73:757–761
Kamath AF, Lewallen DG, Hanssen AD (2015) Porous tantalum metaphyseal cones for severe tibial bone loss in revision knee arthroplasty: a five to nine-year follow-up. J Bone Joint Surg Am 97:216–223
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Koh CK, Zeng I, Ravi S, Zhu M, Vince KG, Young SW (2017) Periprosthetic joint infection is the main cause of failure for modern knee arthroplasty: an analysis of 11,134 knees. Clin Orthop Relat Res 475:2194–2201
Kouk S, Rathod PA, Maheshwari AV, Deshmukh AJ (2018) Rotating hinge prosthesis for complex revision total knee arthroplasty: a review of the literature. J Clin Orthop Trauma 9:29–33
Mantel N (1966) Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep Part 1 50:163–170
Pala E, Trovarelli G, Calabro T, Angelini A, Abati CN, Ruggieri P (2015) Survival of modern knee tumor megaprostheses: failures, functional results, and a comparative statistical analysis. Clin Orthop Relat Res 473:891–899
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ et al (2011) New definition for periprosthetic joint infection: from the workgroup of the musculoskeletal infection society. Clin Orthop Relat Res 469:2992–2994
Petis SM, Perry KI, Mabry TM, Hanssen AD, Berry DJ, Abdel MP (2019) Two-stage exchange protocol for periprosthetic joint infection following total knee arthroplasty in 245 knees without prior treatment for infection. J Bone Joint Surg Am 101:239–249
Petursson G, Fenstad AM, Havelin LI, Gothesen O, Lygre SH, Rohrl SM et al (2015) Better survival of hybrid total knee arthroplasty compared to cemented arthroplasty. Acta Orthop 86:714–720
Pour AE, Parvizi J, Slenker N, Purtill JJ, Sharkey PF (2007) Rotating hinged total knee replacement: use with caution. J Bone Joint Surg Am 89:1735–1741
Rohner E, Benad K, Zippelius T, Kloss N, Jacob B, Kirschberg J et al (2018) Good clinical and radiological results of total knee arthroplasty using varus valgus constrained or rotating hinge implants in ligamentous laxity. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5307-6
Shen C, Lichstein PM, Austin MS, Sharkey PF, Parvizi J (2014) Revision knee arthroplasty for bone loss: choosing the right degree of constraint. J Arthroplast 29:127–131
Smith TH, Gad BV, Klika AK, Styron JF, Joyce TA, Barsoum WK (2013) Comparison of mechanical and nonmechanical failure rates associated with rotating hinged total knee arthroplasty in nontumor patients. J Arthroplast 28(62–67):e61
Tan TL, Goswami K, Fillingham YA, Shohat N, Rondon AJ, Parvizi J (2018) Defining treatment success after 2-stage exchange arthroplasty for periprosthetic joint infection. J Arthroplast 33:3541–3546
Wood GC, Naudie DD, MacDonald SJ, McCalden RW, Bourne RB (2009) Results of press-fit stems in revision knee arthroplasties. Clin Orthop Relat Res 467:810–817
Funding
A specific source of funding was not required in this study.
Author information
Authors and Affiliations
Contributions
CT review of literature, conception and design, acquisition of data, analysis and interpretation of data, statistical analysis, drafting of the manuscript; TSB review of literature, conception and design, acquisition of data, analysis and interpretation of data, statistical analysis, drafting of the manuscript; GG conception and design, critical revision of the manuscript; BT acquisition of data, analysis and interpretation of data, critical revision of the manuscript; BM critical revision of the manuscript; JR critical revision of the manuscript; DA critical revision of the manuscript; JS critical revision of the manuscript; RD conception and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, administrative, technical and material support, critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
One author has received travel expenses by Implantcast Gmbh, Buxtehude, Germany outside the submitted work.
Ethical approval
Approval of the institutional review board was obtained prior to this investigation (local ethical committee ref. no. 2018-123-f-S).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Theil, C., Schmidt-Braekling, T., Gosheger, G. et al. Acceptable mid- to long-term survival rates and functional outcomes following a single design rotating hinge total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 28, 1868–1875 (2020). https://doi.org/10.1007/s00167-019-05593-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05593-1