Abstract
Sildenafil inhibits cyclic GMP-specific phosphodiesterase type-5A (PDE5A) and can prevent cardiac hypertrophy and left ventricular (LV) dysfunction in mice subjected to severe pressure-overload. The pathophysiological role of sildenafil in adverse remodeling in the hypertensive heart after chronic renin–angiotensin aldosterone system stimulation is unknown. Therefore, we studied the efficacy of the PDE5A inhibitor sildenafil for treating advanced cardiac hypertrophy and LV remodeling due to angiotensin (Ang)II-induced heart failure (HF) in vivo. C57BL6/J mice were subjected to AngII-induced cardiac hypertrophy for 3 weeks and cardiac dysfunction, cardiac inflammatory stress response, adverse remodeling as well as apoptosis were documented. Mice were subsequently treated with sildenafil (100 mg/kg/day) or placebo with delay of 5 days for treating AngII infusion-induced adverse events. Compared to controls, AngII infusion resulted in impaired systolic (dP/dt max −46 %, SV −16 %, SW −43 %, E a +51 %, EF −37 %, CO −36 %; p < 0.05) and diastolic (dP/dt min −36 %, LV end diastolic pressure +73 %, Tau +21 %, stiffness constant β +74 %; p < 0.05) LV function. This was associated with a significant increase in cardiac hypertrophy and fibrosis. Increased inflammatory response was also indicated by an increase in immune cell infiltration and apoptosis. Treatment with sildenafil led to a significant improvement in systolic and diastolic LV performance. This effect was associated with less LV hypertrophy, remodeling, cardiac inflammation and apoptosis. PDE5A inhibition with sildenafil may provide a new treatment strategy for cardiac hypertrophy and adverse remodeling in the hypertensive heart.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) represents a complex multifactorial syndrome, characterized by structural and functional abnormalities of the myocardium [29, 47]. Arterial hypertension and cardiac hypertrophy are major risk factors for HF by inducing adverse remodeling, which is one hallmark for poor outcome in patients. Consequently, therapeutic suppression of left ventricular (LV) hypertrophy and adverse remodeling are associated with improved mortality [4, 43]. Therefore, beneficial therapeutic options would be of major interest. An abnormal nitric oxide (NO) pathway is significantly involved in several pathophysiological abnormalities encountered in HF syndrome. Accordingly, NO activation may be one novel therapeutic target [10, 24]. Phosphodiesterase type 5A (PDE5A) inhibition is an attractive pharmacological strategy that enhances in vivo NO signaling by increasing guanosine 3′,5′-cyclic monophosphate (cGMP) availability in the myocardium [31]. The cGMP-specific PDE5A inhibitor sildenafil, which is used clinically for the treatment of either erectile dysfunction or pulmonary arterial hypertension, prevented the development of severe cardiac hypertrophy in animal models, such as the thoracic aortic constriction model in mice [36]. Moreover, selective inhibition of PDE5A improved myocardial infarct size and LV dilation in ischemic cardiomyopathy [34], doxorubicin-induced cardiomyopathy [7], and diabetic cardiomyopathy [9, 18]. Additionally, others investigated that sildenafil could preserve lung endothelial function and prevents pulmonary vascular remodeling in a rat model of diastolic HF [52]. Clinical studies of sildenafil in patients suffering from HF have reported enhanced exercise capacity, reduced pulmonary vascular resistance and improved endothelial function [17, 38].
However, the precise role of the PDE5A inhibitor sildenafil in pathological remodeling in the hypertensive heart after chronic renin–angiotensin aldosterone system (RAAS) stimulation still remains unclear. Therefore, we examined the efficiency of PDE5A inhibition in angiotensin (Ang)II-induced HF in vivo. Here, we show evidence that treatment with sildenafil improves LV performance, inflammatory immune response and adverse remodeling in AngII-induced cardiac dysfunction and fibrosis in mice.
Materials and methods
Drugs and dose determination
Experimental animal groups were randomly assigned and AngII (1.8 mg/kg/day/s.c.; Bachem, Weil am Rhein, Germany) or sterile ringer solution (Merck, Darmstadt, Germany) was continuously infused via osmotic pumps (Alzet, model 2004, Cupertino, CA, USA) over a period of 3 weeks. With delay of 5 days, animals received sildenafil citrate (100 mg/kg/day; Viagra, Pfizer, USA) or placebo. Although this dose is high for humans, the mouse metabolizes sildenafil at a higher rate [44], and this dose yields a free plasma concentration of 10–15 nM, within the specific and therapeutic range for PDE5A [36].
Oral treatment with sildenafil was provided by mixing drug into semi-soft rodent chow (Bioserv; 4–6 g/day) that also provided full daily nutrition. WT mice and AngII mice also received vehicle mixed in the food. In order to exclude beneficial effects of sildenafil due to its blood pressure lowering effects, we examined in a sub-study the effects of the direct vasodilator hydralazine, which acts through blood pressure reduction only. Animal groups were randomly assigned and AngII (1.8 mg/kg/day/s.c.; Bachem, Weil am Rhein, Germany) or sterile ringer solution (Merck, Darmstadt, Germany) was continuously infused via osmotic pumps (Alzet, model 2004, Cupertino, CA, USA) over a period of 3 weeks. With delay of 5 days, animals received hydralazine in drinking water (10 mg/kg/day; Barr Pharmaceuticals, Montvale, NJ, USA) [51] to achieve similar blood pressure lowering effects to sildenafil treatment. The experimental groups consisted of WT, WT + HY, AngII, AngII + HY (n = 10–14 per group; Fig. 9).
Surgical procedures and hemodynamic measurements
Eight- to ten-week-old male C57BL6/J mice were randomly divided into four groups (n = 7–11 per group). The experimental groups consisted of WT, WT + Sil, AngII, AngII + Sil. After 3 weeks, all animals were anesthetized (thiopental 125 mg/g i.p.; Merial, Hallbergmoos, Germany), intubated, and artificially ventilated with a rodent ventilator type 7025 (Ugo Basile, Comerio, VA, Italy). Heart rate, systolic blood pressure, LV contractility (dP/dt max), stroke volume (SV), stroke work (SW), afterload (E a), LV relaxation (dP/dt min), LV relaxation time (Tau), LV end diastolic pressure (LVEDP), ejection fraction (EF) and cardiac output (CO) as indices of global, systolic and diastolic LV function were recorded via a microconductance catheter (1.2F) system in closed chest animals as described previously [2, 50]. This investigation conforms to the Guide for the Care and Use of Laboratory Animals published by the US NIH (NIH Publication No. 85-23, revised 1996).
Tissue preparation
After mice were killed, LV tissues were excised, immediately snap frozen in liquid nitrogen and stored at −80 °C for biological and immunohistological analyses.
RNA isolation from heart tissue
Total RNA was extracted from LV sections by the TRIzol method (Invitrogen, Carlsbad, CA, USA) as described previously [2]. Further purification was accomplished using the RNeasy Mini kit (Qiagen, Hilden, Germany). The yield of purified total RNA was determined by measuring the ultraviolet absorbance at 260 nm on a NanoDrop ND-1000 spectrophotometer (Agilent Technologies, Boeblingen, Germany). RNA was reverse transcribed (1 μg RNA) using the High Capacity cDNA Archive kit (Applied Biosystems, Darmstadt, Germany).
TaqMan low-density arrays of heart tissue
TaqMan low-density arrays were carried out as described previously [1, 19] using specific gene expression assays (Applied Biosystems) for CX3C chemokine receptor 1 (CX3CR1), CX3C motif ligand 1 (CX3CL1), tumor necrosis factor (TNF)-α, interleukin (IL)-6, interleukin (IL)-18, nitric oxide synthase (NOS)2, Bax, Bcl-2, atrial natriuretic peptide (ANP), β-myosin heavy chain (β-MHC), cGMP-dependent protein kinase 1α (PKG1α), phosphodiesterase 5A (PDE5A), matrix metalloproteinase (MMP)13, tissue inhibitor of metalloproteinases (TIMP)1, collagen (Col)1A2, collagen (Col)3A1, disintegrin and metalloproteinase with thrombospondin motif-1 (ADAMTS1) and disintegrin and metalloproteinase with thrombospondin motif-2 (ADAMTS2).
Immunohistological measurements
As described previously [32, 46, 48], murine tissue of the left ventricle was embedded in Tissue-Tek (Dako) and immunohistochemistry was performed with specific antibodies directed against CD11b (Pharmigen), CD68 (Abcam), receptor of advanced glycation end products (RAGE, Abcam), receptor for activated protein kinase c (RACK1, Abcam), collagen I (Chemicon), collagen III (Chemicon), α-smooth muscle actin (SMA, Abcam), monocyte chemoattractant protein-1 (MCP-1, Abnova), MMP13 (GeneTex), TIMP1 (Abcam) and PKG1α (Bios). Quantification was performed by digital image analyses [32]. In brief, the ratio between the heart tissue area and the specific chromogen-positive area was calculated (area fraction, %). The amount of infiltrating cells was calculated by measuring the number of cells per area of heart tissue (cells/mm2). For cell size determination, ImageJ software was used to calculate cardiomyocyte surface area of at least 200 cells per experimental group. Statistical significance of observed differences in cardiomyocyte cell size was determined by Student’s t test and ANOVA (p < 0.05).
TUNEL assay
Apoptotic cells were detected in cryosections by end-labeling the fragmented DNA using the DeadEnd™ Colorimetic TUNEL System (Promega, USA) according to the manufacturer’s instructions. TUNEL-positive cells were calculated as cells per area of heart tissue [2].
Statistical analyses
Statistical analysis was performed using SPSS Version 12.0. Data are expressed as the mean ± SEM. Statistical differences were assessed using the Kruskal–Wallis test in conjunction with the Mann–Whitney U post hoc test. Bonferroni correction was applied to the post hoc Mann–Whitney test to adjust for multiple comparisons. The calculated results were similar. Differences were considered statistically significant at a value of p < 0.05.
Results
Cardiac function
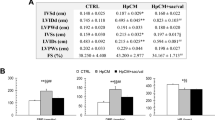
Three weeks after exogenous AngII infusion, heart rate, systolic blood pressure, systolic and diastolic LV function were determined in all experimental groups (Table 1).
Chronic infusion of AngII (1.8 mg/kg/day/s.c.) resulted in impaired cardiac output and significant reduction of systolic function (dP/dt max −46 %, SV −16 %, SW −43 %, E a +51 %, EF −37 %, CO −36 %; p < 0.05) and diastolic function (dP/dt min −36 %, LVEDP +73 %, Tau +21 %, stiffness constant β +74 %; p < 0.05), indicating a significant global cardiac dysfunction (Table 1). Interestingly, treatment with sildenafil ameliorated systolic LV dysfunction (dP/dt max +29 %, SW +31 %, E a −43 %, EF + 26 %, CO +34 %; p < 0.05) and improved diastolic dysfunction (dP/dt min +19 %, LVEDP −38 %, stiffness constant β −48 %; p < 0.05) to values similar to the controls (Table 1).
Cardiac cytokine activation
We measured the inflammatory cytokine activation in hearts from those cytokines associated with the inflammatory immune response in chronic HF [14]. Quantification of expression of CX3CR1 receptor (Fig. 1c; 2.5-fold) and of the pro-inflammatory cytokines CX3CL1 (Fig. 1f), TNF-α (Fig. 1a), IL-6 (Fig. 1b), IL-18 (Fig. 1d) and NOS2 (Fig. 1e) displayed a 2.1-, 4.8-, 8.5-, 2.1- and 1.5-fold elevation after 3 weeks of AngII treatment, respectively. Treatment with sildenafil reduced the AngII-driven increase of all these pro-inflammatory factors and CX3CR1 receptor expression (p < 0.05). Sildenafil alone did not affect any cytokine and receptor expression levels.
Fractalkine expression and cytokine activation. Relative mRNA expression of CX3CR1, CX3CL1, TNF-α, IL-6, IL-18 and NOS2 of cardiac tissue 21 days after treatment. Data are from 7 to 11 mice/group; one data point per heart. Data expressed as mean ± SEM. *p < 0.05. AngII angiotensin II, Sil sildenafil
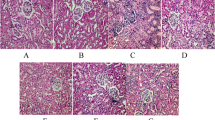
Cardiac immune cell infiltration and RAGE expression
AngII induced an intensified cardiac immune response, as indicated by increases in CD11b-positive, CD68-positive cell infiltration and RAGE protein expression (4.9-, 4.8-, 3.9-fold) in the myocardium (Figs. 2, 3). Here as well, treatment with sildenafil displayed a significant reduced cardiac immune cell infiltration and RAGE expression (p < 0.05). Sildenafil alone did not show any effect on cardiac immune cell infiltration and RAGE expression.
Cardiac immune cell infiltration, RAGE, PDE5A and PKG1α expression levels. Quantification of CD11b-positive and CD68-positive cells per area (cells/mm2), relative mRNA and protein expression levels of RAGE, PDE5A, PKG1α per area (area fraction, %) of cardiac tissue 21 days after treatment. Protein and cell quantification was performed by digital image analyses. Data are from 7 to 11 mice/group; one data point per heart. Data expressed as mean ± SEM. *p < 0.05. AngII angiotensin II, Sil sildenafil
Cardiac immune cell infiltration, apoptosis and RAGE expression. Representative images and quantification of CD11b-, CD68-, TUNEL-positive cells per area (cells/mm2) and RAGE protein expression per area (area fraction, %) of cardiac tissue 21 days after treatment. Specific epitopes of CD11b-, CD68-, RACK1-, TUNEL- and RAGE-positive cells or protein expression are colored red. Quantification was performed by digital image analyses. Data are from 7 to 11 mice/group; one data point per heart. Data expressed as mean ± SEM. *p < 0.05. AngII angiotensin II, Sil sildenafil. Scale bar 100 μm
Cardiac apoptosis
AngII-diseased mice showed a significantly increased amount of TUNEL-positive apoptotic cells, Bax/Bcl-2 mRNA expression ratio and RACK1 protein expression when compared to controls (p < 0.05). Sildenafil-treated mice displayed a significant reduction of TUNEL-positive apoptotic cells, Bax/Bcl-2 mRNA expression ratio and RACK1 protein expression when compared to the animal group without treatment (Figs. 3, 4; p < 0.05). Sildenafil alone did not show any effect on cardiac apoptosis.
Cardiac apoptosis. TUNEL-positive cells per area (cells/mm2), RACK1 protein expression per area (area fraction, %) and relative mRNA expression of Caspase3 and Bax/Bcl-2 ratio of cardiac tissue 21 days after treatment. Data are from 7 to 11 mice/group; one data point per heart. Data expressed as mean ± SEM. *p < 0.05. AngII angiotensin II, Sil sildenafil
Extracellular matrix alteration
Cardiac fibrosis as determined by collagen I, collagen III, ADAMTS1, ADAMTS2, MMP13, TIMP1, MMP13/TIMP1 ratios, TGF-β, α-SMA and MCP-1 gene and protein expression levels (Figs. 5–8). In detail, AngII treatment resulted in a 1.4-, 2.2-, 2.1-, 2.2-, 2.4-, 3.9- and 1.9-fold elevation of Col1A2 (Fig. 6a), Col3A1 (Fig. 6b), ADAMTS1 (Fig. 6c), ADAMTS2 (Fig. 6d), MMP13 (Fig. 5a), TIMP1 (Fig. 5b) and TGF-β (Fig. 8d) mRNA and in a 1.6-, 1.7-, 32.4-and 21.4-fold elevation of collagen I (Fig. 7a), collagen III (Fig. 7b), α-SMA (Fig. 7c) and MCP-1 (Fig. 7d) protein expression, respectively. These increased mRNA and protein expression levels were reduced or improved when animals were treated with sildenafil (p < 0.05). In addition, sildenafil neutralized MMP13/TIMP1 mRNA and protein expression ratios (Fig. 5c, d) when compared to the untreated animals (p < 0.05). Furthermore, sildenafil treatment alone led to no changes in cardiac fibrosis and remodeling.
Cardiac remodeling. Quantification of collagen I, collagen III, α-SMA and MCP-1 protein expression per area (area fraction, %) of cardiac tissue 21 days after treatment. Protein quantification was performed by digital image analyses. Data are from 7 to 11 mice/group; one data point per heart. Data expressed as mean ± SEM. *p < 0.05. AngII angiotensin II, Sil sildenafil. Scale bar 100 μm
PKG1α and PDE5A expression in the myocardium
Three weeks after exogenous AngII infusion, PKG1α and PDE5A mRNA and protein expression levels were measured in all experimental groups. Here, AngII-diseased mice displayed reduced PKG1α mRNA and protein expression levels (1.2-, 1.6-fold; p < 0.05). Moreover, exogenous AngII infusion did lead to an increased PDE5A mRNA expression level. Interestingly, treatment with sildenafil significantly restores PKG1α and PDE5A mRNA and protein expression levels when compared to control mice (Fig. 2d–f).
Cardiac hypertrophy
To investigate possible anti-hypertrophic effects of sildenafil, we examined cardiomyocyte diameter, ANP and β-MHC mRNA expression levels in this setting. After 3 weeks of AngII treatment, cardiomyocyte diameter, ANP and β-MHC mRNA expression levels were significantly increased when compared to controls (8.4-, 5-, 4.2-fold; Fig. 8a–c). Surprisingly, treatment with sildenafil did lead to a reduction of cardiomyocyte diameter, ANP and β-MHC mRNA expression levels in the myocardium (p < 0.05). Moreover, cardiac hypertrophy—indexed by LV weight/body weight ratio—was elevated 3 weeks after AngII-induced LV dysfunction. This was significantly attenuated by treatment with sildenafil (−16 %; Table 1).
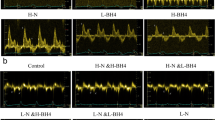
Animal study with hydralazine treatment for controlling a possible blood pressure effect
Three weeks after exogenous AngII infusion, systolic blood pressure and cardiac function were determined in all experimental groups (Fig. 9a). Exogenous AngII infusion over a period of 3 weeks led to significant increase in systolic blood pressure (+24 %). Treatment with hydralazine led to a non-significant reduction in systolic blood pressure (−8 %). This reduction in systolic blood pressure was similar to the blood pressure lowering effects to sildenafil treatment (Table 1). Moreover, chronic infusion of AngII resulted in impaired global cardiac dysfunction (dP/dt max −48 %, E a +46 %, EF −35 %; p < 0.05) an increase in cardiomyocyte diameter (+81 %). Treatment with hydralazine did not improve cardiac dysfunction and did not reduce cardiomyocyte diameter in this experimental setting (Fig. 9a).
Animal study with hydralazine treatment for controlling a possible blood pressure effect. Hemodynamic results and cardiomyocyte diameter 21 days after treatment (a). Protein expression levels of collagen I, collagen III, α-SMA and MMP13/TIMP1 ratio in hearts 21 days after treatment (b). CD11b-positive, CD68-positive and TUNEL-positive cells and MCP-1 protein content in heart tissue 21 days after treatment (c). Data are from 10 to 14 mice/group; one data point per heart. Data expressed as mean ± SEM. *p < 0.05. AngII angiotensin II, HY hydralazine
Moreover, AngII infusion over a period of 3 weeks led to a significant increase in protein expression levels of collagen I (2.1-fold), collagen III (3.1-fold) and α-SMA (33-fold) and to a significant reduction in MMP13/TIMP1 protein expression ratio (1.9-fold; Fig. 9b). Treatment with hydralazine did not reduce collagen I, collagen III and α-SMA protein expression levels. In addition, hydralazine treatment did not enhance the MMP13/TIMP1 protein expression ratio in this setting (Fig. 9b).
AngII induced an intensified cardiac immune response and apoptosis, as indicated by increases in CD11b-positive (3.8-fold), CD68-positive (4.6-fold), TUNEL-positive cells (5.8-fold) and MCP-1 protein content (28-fold) in the myocardium (Fig. 9c). Here as well, treatment with hydralazine displayed no changes in cardiac immune cell infiltration, MCP-1 protein expression and apoptosis, indexed by the amount of TUNEL-positive cells, in this experimental setting (Fig. 9c).
Discussion
To the best of our knowledge, this study demonstrates for the first time the beneficial effects of PDE5A inhibition with sildenafil by improving LV dysfunction, inflammatory stress response and cardiac remodeling in experimental AngII-induced heart failure (HF) in vivo.
Chronic AngII infusion resulted in cardiac inflammation and matrix remodeling. Consequently, systolic and diastolic LV dysfunction was observed after AngII infusion. We demonstrated that selective PDE5A inhibition with sildenafil led to a significant enhancement of cardiac remodeling in AngII-induced HF. Treatment with sildenafil reduced cardiac inflammation followed by an improved remodeling process as well as cardiac apoptosis. Moreover, sildenafil treatment led to a reduction of cardiac immune cell infiltration in the myocardium, all resulting in improved LV function despite AngII infusion.
Fibrosis is one hallmark in the development of HF, also seen in this AngII model. Cardiac remodeling and extracellular matrix (ECM) dysregulation were indicated by changes in cardiac hypertrophy and fibrosis induced by exogenous AngII infusion [22, 37]. Here, 3 weeks after AngII infusion mice displayed a significant increase in interstitial collagen I and collagen III, hallmarks of myocardial fibrosis. Contrarily, after onset of the disease PDE5A inhibition with sildenafil normalized these values to those of controls showing a treatment effect of this drug. During connective tissue remodeling, fibroblasts get activated and can transform to α-SMA-expressing myofibroblasts [27, 39, 45]. These myofibroblasts produce newly created ECM leading to accumulation of collagen in the myocardium [49]. A pathological persistence of the myofibroblast is a hallmark of pro-fibrotic diseases in other organs as well as the heart [12, 23]. This is known to be an important trigger for diastolic dysfunction and increased LV stiffness. One of the most important findings with respect to ECM regulation is the fact that sildenafil treatment led to a significant reduction in the number of α-SMA-myofibroblasts and to an improvement in the MMP/TIMP regulation by normalizing MMP13 and TIMP1 mRNA and protein expression levels and its ratio resulting in improved collagen turnover by normalizing the collagen derogatory capacity. Future studies have to reveal whether these changes are directly PDE5A-dependent or whether this is due to limited inflammation in the diseased heart, since inflammatory cells are known to trigger the transdifferentiation into myofibroblasts and therefore fuel the profibrotic process. Moreover, we investigated the pathophysiological role of ADAMTS1 and ADAMTS2, metalloproteinases with thrombospondin motifs, during adverse remodeling in this setting. In detail, the disintegrin-like adhesion domain of these proteins interacts with integrin-like receptors on cells to promote cell–matrix attachment or disrupt interaction between integrin receptors and the ECM. In recent studies, Kuno and colleagues [21] demonstrated that ADAMTS1 was a catalytically active metalloproteinase, which should theoretically result in less collagen accumulation. In our study, we found that ADAMTS1 and ADAMTS2 were only mildly increased in cardiac tissue after AngII infusion, whereas treatment with sildenafil led to a significantly increased expression of these proteins. Reports from others showed that the ADAMTS1 deficient mice displayed interstitial fibrosis in the cortical and medullary regions of the kidney [28]. In light of those and our findings, we speculate that ADAMTS1 and ADAMTS2 probably play a role in counterbalancing excessive cardiac fibrosis, which is supported by in vitro findings [25], but this has to be further investigated in the future.
Also, inflammation is important in the development of HF and linked to poor outcome. Compared to untreated animals mRNA expression levels of TNF-α, IL-6, IL-18 and NOS2 of sildenafil-treated animals were significantly reduced 3 weeks after AngII infusion. Moreover, the fractalkine CX3CL1 and its receptor CX3CR1 have been identified to be a mediator in experimental and human HF [16]. Interestingly, we observed also increased mRNA expression levels of the fractalkine CX3CL1 and its receptor CX3CR1 in AngII mice, whereas treatment with sildenafil neutralized these expression levels to those of controls. Furthermore, we investigated a significant reduction in cardiac immune cell infiltration and cytokine activation after sildenafil treatment. Interestingly, sildenafil treatment displayed additional antiinflammatory and antiapoptotic effects with significantly reduced CD11b-positive and CD68-positive immune cell infiltration, MCP-1 and RAGE protein content and the number of TUNEL-positive cells in the myocardium. In addition, treatment with sildenafil improved cardiac apoptosis indexed by Bax/Bcl-2 mRNA expression ratio and RACK1 protein expression. Recently, it was also shown that the activation through RAGE critically contributes to the development of post-ischemic cardiomyopathy driving the progressive course of HF [42]. Moreover, Sakaguchi and colleagues [33] were able to show a RAGE-S100-protein-induced proliferation and migration of α-SMA-positive myofibroblasts and the consequent enhanced expression and activation of ECM proteins and metalloproteinases in their model. Our results concerning MCP-1 expressions are in line with other studies reporting that MCP-1 is consistently upregulated in various HF models such as experimental myocardial infarction [3, 5, 6] and may play an important role in regulating leukocyte trafficking and cardiac tissue repair [8]. In conclusion, while AngII infusion resulted in an inflammatory phenotype of the heart, sildenafil could neutralize this inflammatory setting resulting in improved remodeling.
Cardiac hypertrophy is probably one of the most important risk factors for HF [20]. In this study, AngII resulted in cardiac hypertrophy indexed by an increase in ANP, β-MHC, cardiomyocyte diameter and LV weight/body weight ratio, whereas treatment with sildenafil leads to normalization in all these parameters. These results clearly indicate that sildenafil acts also anti-hypertrophic during AngII-induced cardiac overload. In line with this, recent work by Kass and colleagues [30, 36] demonstrated that selective inhibition of PDE5A with sildenafil markedly prevented the LV hypertrophy and dysfunction induced by severe chronic pressure overload secondary to transverse aortic constriction in mice. Furthermore, PDE5A inhibition has also been reported to ameliorate LV hypertrophy produced by chronic isoproterenol infusion [13].
Small-molecule approaches that reverse cardiac hypertrophy to the extent here observed are rare, suggesting that the underlying mechanisms linked to the modulation of PDE5A, cGMP and cGMP-dependent protein kinase (PKG)-1 documented in this and other studies are powerful and are likely to interfere with several pathways [26]. The simplicity of the orally available therapy and the wide clinical knowledge and safety evidence of PDE5A inhibitors suggest that this may be an important therapeutic approach for chronic HF and cardiac hypertrophy caused by high blood pressure in humans [11, 15, 35].
PDE5A inhibition regulated adverse LV remodeling, inflammation and hypertrophy. Therefore, it resulted in less systolic and diastolic cardiac dysfunction leading to improved ejection fraction as well as cardiac output, both also affecting afterload. Toischer et al. [40, 41] reported that this hemodynamic load is a critical regulator of myocardial function, gene expression, and phenotype appearance. In order to verify that the observed cardiobeneficial effects of sildenafil treatment are not secondary to the non-significant blood pressure reduction seen in this study, we examined in a sub-study the effects of the direct vasodilator hydralazine, which acts through blood pressure reduction. Matched blood pressure reduction by hydralazine did not affect LV function, inflammation and remodeling in this experimental setting compared to placebo-treated AngII animals (Fig. 9). Therefore, we conclude that sildenafil possesses the documented cardioprotective effects independent of blood pressure reduction in this study.
In summary, the present study identifies the PDE5A inhibition with sildenafil as a promising strategy to improve LV dysfunction and adverse remodeling in AngII-induced chronic HF. Further investigation is necessary to prove that these cardiobeneficial effects seen after sildenafil treatment in hypertensive heart disease can be transferred to a clinical setting.
References
Abruzzo LV, Lee KY, Fuller A, Silverman A, Keating MJ, Medeiros LJ, Coombes KR (2005) Validation of oligonucleotide microarray data using microfluidic low-density arrays: a new statistical method to normalize real-time RT-PCR data. Biotechniques 38:785–792
Becher PM, Lindner D, Miteva K, Savvatis K, Zietsch C, Schmack B, Van Linthout S, Westermann D, Schultheiss HP, Tschope C (2012) Role of heart rate reduction in the prevention of experimental heart failure: comparison between if-channel blockade and beta-receptor blockade. Hypertension 59:949–957. doi:10.1161/HYPERTENSIONAHA.111.183913
Damas JK, Aukrust P, Ueland T, Odegaard A, Eiken HG, Gullestad L, Sejersted OM, Christensen G (2001) Monocyte chemoattractant protein-1 enhances and interleukin-10 suppresses the production of inflammatory cytokines in adult rat cardiomyocytes. Basic Res Cardiol 96:345–352
Devereux RB, Wachtell K, Gerdts E, Boman K, Nieminen MS, Papademetriou V, Rokkedal J, Harris K, Aurup P, Dahlof B (2004) Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA 292:2350–2356. doi:10.1001/jama.292.19.2350
Dewald O, Zymek P, Winkelmann K, Koerting A, Ren G, Abou-Khamis T, Michael LH, Rollins BJ, Entman ML, Frangogiannis NG (2005) CCL2/monocyte chemoattractant protein-1 regulates inflammatory responses critical to healing myocardial infarcts. Circ Res 96:881–889. doi:10.1161/01.RES.0000163017.13772.3a
Dobaczewski M, Frangogiannis NG (2009) Chemokines and cardiac fibrosis. Front Biosci 1:391–405
Fisher PW, Salloum F, Das A, Hyder H, Kukreja RC (2005) Phosphodiesterase-5 inhibition with sildenafil attenuates cardiomyocyte apoptosis and left ventricular dysfunction in a chronic model of doxorubicin cardiotoxicity. Circulation 111:1601–1610. doi:10.1161/01.CIR.0000160359.49478.C2
Frangogiannis NG (2004) The role of the chemokines in myocardial ischemia and reperfusion. Curr Vasc Pharmacol 2:163–174
Giannetta E, Isidori AM, Galea N, Carbone I, Mandosi E, Vizza CD, Naro F, Morano S, Fedele F, Lenzi A (2012) Chronic inhibition of cyclic GMP phosphodiesterase 5A improves diabetic cardiomyopathy: a randomized, controlled clinical trial using magnetic resonance imaging with myocardial tagging. Circulation 125:2323–2333. doi:10.1161/CIRCULATIONAHA.111.063412
Guazzi M (2008) Sildenafil and phosphodiesterase-5 inhibitors for heart failure. Curr Heart Fail Rep 5:110–114
Guazzi M, Samaja M, Arena R, Vicenzi M, Guazzi MD (2007) Long-term use of sildenafil in the therapeutic management of heart failure. J Am Coll Cardiol 50:2136–2144. doi:10.1016/j.jacc.2007.07.078
Hammoud L, Lu X, Lei M, Feng Q (2011) Deficiency in TIMP-3 increases cardiac rupture and mortality post-myocardial infarction via EGFR signaling: beneficial effects of cetuximab. Basic Res Cardiol 106:459–471. doi:10.1007/s00395-010-0147-7
Hassan MA, Ketat AF (2005) Sildenafil citrate increases myocardial cGMP content in rat heart, decreases its hypertrophic response to isoproterenol and decreases myocardial leak of creatine kinase and troponin T. BMC Pharmacol 5:10. doi:10.1186/1471-2210-5-10
Heymans S, Hirsch E, Anker SD, Aukrust P, Balligand JL, Cohen-Tervaert JW, Drexler H, Filippatos G, Felix SB, Gullestad L, Hilfiker-Kleiner D, Janssens S, Latini R, Neubauer G, Paulus WJ, Pieske B, Ponikowski P, Schroen B, Schultheiss HP, Tschope C, Van Bilsen M, Zannad F, McMurray J, Shah AM (2009) Inflammation as a therapeutic target in heart failure? A scientific statement from the Translational Research Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 11:119–129. doi:10.1093/eurjhf/hfn043
Hirata K, Adji A, Vlachopoulos C, O’Rourke MF (2005) Effect of sildenafil on cardiac performance in patients with heart failure. Am J Cardiol 96:1436–1440. doi:10.1016/j.amjcard.2005.06.091
Husberg C, Nygard S, Finsen AV, Damas JK, Frigessi A, Oie E, Waehre A, Gullestad L, Aukrust P, Yndestad A, Christensen G (2008) Cytokine expression profiling of the myocardium reveals a role for CX3CL1 (fractalkine) in heart failure. J Mol Cell Cardiol 45:261–269. doi:10.1016/j.yjmcc.2008.05.009
Kim KH, Kim YJ, Ohn JH, Yang J, Lee SE, Lee SW, Kim HK, Seo JW, Sohn DW (2012) Long-term effects of sildenafil in a rat model of chronic mitral regurgitation: benefits of ventricular remodeling and exercise capacity. Circulation 125:1390–1401. doi:10.1161/CIRCULATIONAHA.111.065300
Koka S, Xi L, Kukreja RC (2012) Chronic treatment with long acting phosphodiesterase-5 inhibitor tadalafil alters proteomic changes associated with cytoskeletal rearrangement and redox regulation in type 2 diabetic hearts. Basic Res Cardiol 107:249. doi:10.1007/s00395-012-0249-5
Krupinski J, Turu MM, Martinez-Gonzalez J, Carvajal A, Juan-Babot JO, Iborra E, Slevin M, Rubio F, Badimon L (2006) Endogenous expression of C-reactive protein is increased in active (ulcerated noncomplicated) human carotid artery plaques. Stroke 37:1200–1204. doi:10.1161/01.STR.0000217386.37107.be
Kuhn C, Frank D, Dierck F, Oehl U, Krebs J, Will R, Lehmann LH, Backs J, Katus HA, Frey N (2012) Cardiac remodeling is not modulated by overexpression of muscle LIM protein (MLP). Basic Res Cardiol 107:262. doi:10.1007/s00395-012-0262-8
Kuno K, Terashima Y, Matsushima K (1999) ADAMTS-1 is an active metalloproteinase associated with the extracellular matrix. J Biol Chem 274:18821–18826
Landmesser U, Wollert KC, Drexler H (2009) Potential novel pharmacological therapies for myocardial remodelling. Cardiovasc Res 81:519–527. doi:10.1093/cvr/cvn317
Leask A (2010) Potential therapeutic targets for cardiac fibrosis: TGFbeta, angiotensin, endothelin, CCN2, and PDGF, partners in fibroblast activation. Circ Res 106:1675–1680. doi:10.1161/CIRCRESAHA.110.217737
Lee DI, Vahebi S, Tocchetti CG, Barouch LA, Solaro RJ, Takimoto E, Kass DA (2010) PDE5A suppression of acute beta-adrenergic activation requires modulation of myocyte beta-3 signaling coupled to PKG-mediated troponin I phosphorylation. Basic Res Cardiol 105:337–347. doi:10.1007/s00395-010-0084-5
Lind T, Birch MA, McKie N (2006) Purification of an insect derived recombinant human ADAMTS-1 reveals novel gelatin (type I collagen) degrading activities. Mol Cell Biochem 281:95–102. doi:10.1007/s11010-006-0637-y
McKinsey TA, Kass DA (2007) Small-molecule therapies for cardiac hypertrophy: moving beneath the cell surface. Nat Rev Drug Discov 6:617–635. doi:10.1038/nrd2193
Miller CL, Cai Y, Oikawa M, Thomas T, Dostmann WR, Zaccolo M, Fujiwara K, Yan C (2011) Cyclic nucleotide phosphodiesterase 1A: a key regulator of cardiac fibroblast activation and extracellular matrix remodeling in the heart. Basic Res Cardiol 106:1023–1039. doi:10.1007/s00395-011-0228-2
Mittaz L, Ricardo S, Martinez G, Kola I, Kelly DJ, Little MH, Hertzog PJ, Pritchard MA (2005) Neonatal calyceal dilation and renal fibrosis resulting from loss of Adamts-1 in mouse kidney is due to a developmental dysgenesis. Nephrol Dial Transplant 20:419–423. doi:10.1093/ndt/gfh603
Mudd JO, Kass DA (2008) Tackling heart failure in the twenty-first century. Nature 451:919–928. doi:10.1038/nature06798
Nagayama T, Hsu S, Zhang M, Koitabashi N, Bedja D, Gabrielson KL, Takimoto E, Kass DA (2009) Sildenafil stops progressive chamber, cellular, and molecular remodeling and improves calcium handling and function in hearts with pre-existing advanced hypertrophy caused by pressure overload. J Am Coll Cardiol 53:207–215. doi:10.1016/j.jacc.2008.08.069
Nagendran J, Archer SL, Soliman D, Gurtu V, Moudgil R, Haromy A, St Aubin C, Webster L, Rebeyka IM, Ross DB, Light PE, Dyck JR, Michelakis ED (2007) Phosphodiesterase type 5 is highly expressed in the hypertrophied human right ventricle, and acute inhibition of phosphodiesterase type 5 improves contractility. Circulation 116:238–248. doi:10.1161/CIRCULATIONAHA.106.655266
Riad A, Bien S, Gratz M, Escher F, Westermann D, Heimesaat MM, Bereswill S, Krieg T, Felix SB, Schultheiss HP, Kroemer HK, Tschope C (2008) Toll-like receptor-4 deficiency attenuates doxorubicin-induced cardiomyopathy in mice. Eur J Heart Fail 10:233–243. doi:10.1016/j.ejheart.2008.01.004
Sakaguchi T, Yan SF, Yan SD, Belov D, Rong LL, Sousa M, Andrassy M, Marso SP, Duda S, Arnold B, Liliensiek B, Nawroth PP, Stern DM, Schmidt AM, Naka Y (2003) Central role of RAGE-dependent neointimal expansion in arterial restenosis. J Clin Invest 111:959–972. doi:10.1172/JCI17115
Salloum FN, Abbate A, Das A, Houser JE, Mudrick CA, Qureshi IZ, Hoke NN, Roy SK, Brown WR, Prabhakar S, Kukreja RC (2008) Sildenafil (Viagra) attenuates ischemic cardiomyopathy and improves left ventricular function in mice. Am J Physiol Heart Circ Physiol 294:H1398–H1406. doi:10.1152/ajpheart.91438.2007
Schwartz BG, Levine LA, Comstock G, Stecher VJ, Kloner RA (2012) Cardiac uses of phosphodiesterase-5 inhibitors. J Am Coll Cardiol 59:9–15. doi:10.1016/j.jacc.2011.07.051
Takimoto E, Champion HC, Li M, Belardi D, Ren S, Rodriguez ER, Bedja D, Gabrielson KL, Wang Y, Kass DA (2005) Chronic inhibition of cyclic GMP phosphodiesterase 5A prevents and reverses cardiac hypertrophy. Nat Med 11:214–222. doi:10.1038/nm1175
Tamargo J, Lopez-Sendon J (2011) Novel therapeutic targets for the treatment of heart failure. Nat Rev Drug Discov 10:536–555. doi:10.1038/nrd3431
Tantini B, Manes A, Fiumana E, Pignatti C, Guarnieri C, Zannoli R, Branzi A, Galie N (2005) Antiproliferative effect of sildenafil on human pulmonary artery smooth muscle cells. Basic Res Cardiol 100:131–138. doi:10.1007/s00395-004-0504-5
Tiede K, Melchior-Becker A, Fischer JW (2010) Transcriptional and posttranscriptional regulators of biglycan in cardiac fibroblasts. Basic Res Cardiol 105:99–108. doi:10.1007/s00395-009-0049-8
Toischer K, Kochhauser S, van Nguyen P, Leineweber K, Hasenfuss G, Kogler H (2012) Mechanical load-dependent cardiac ER stress in vitro and in vivo: effects of preload and afterload. FEBS Lett 586:1363–1369. doi:10.1016/j.febslet.2012.03.055
Toischer K, Rokita AG, Unsold B, Zhu W, Kararigas G, Sossalla S, Reuter SP, Becker A, Teucher N, Seidler T, Grebe C, Preuss L, Gupta SN, Schmidt K, Lehnart SE, Kruger M, Linke WA, Backs J, Regitz-Zagrosek V, Schafer K, Field LJ, Maier LS, Hasenfuss G (2010) Differential cardiac remodeling in preload versus afterload. Circulation 122:993–1003. doi:10.1161/CIRCULATIONAHA.110.943431
Volz HC, Laohachewin D, Seidel C, Lasitschka F, Keilbach K, Wienbrandt AR, Andrassy J, Bierhaus A, Kaya Z, Katus HA, Andrassy M (2012) S100A8/A9 aggravates post-ischemic heart failure through activation of RAGE-dependent NF-kappaB signaling. Basic Res Cardiol 107:250. doi:10.1007/s00395-012-0250-z
Wachtell K, Okin PM, Olsen MH, Dahlof B, Devereux RB, Ibsen H, Kjeldsen SE, Lindholm LH, Nieminen MS, Thygesen K (2007) Regression of electrocardiographic left ventricular hypertrophy during antihypertensive therapy and reduction in sudden cardiac death: the LIFE Study. Circulation 116:700–705. doi:10.1161/CIRCULATIONAHA.106.666594
Walker DK, Ackland MJ, James GC, Muirhead GJ, Rance DJ, Wastall P, Wright PA (1999) Pharmacokinetics and metabolism of sildenafil in mouse, rat, rabbit, dog and man. Xenobiotica 29:297–310. doi:10.1080/004982599238687
Watsky MA, Weber KT, Sun Y, Postlethwaite A (2010) New insights into the mechanism of fibroblast to myofibroblast transformation and associated pathologies. Int Rev Cell Mol Biol 282:165–192. doi:10.1016/S1937-6448(10)82004-0
Westermann D, Mersmann J, Melchior A, Freudenberger T, Petrik C, Schaefer L, Lullmann-Rauch R, Lettau O, Jacoby C, Schrader J, Brand-Herrmann SM, Young MF, Schultheiss HP, Levkau B, Baba HA, Unger T, Zacharowski K, Tschope C, Fischer JW (2008) Biglycan is required for adaptive remodeling after myocardial infarction. Circulation 117:1269–1276. doi:10.1161/CIRCULATIONAHA.107.714147
Westermann D, Riad A, Richter U, Jager S, Savvatis K, Schuchardt M, Bergmann N, Tolle M, Nagorsen D, Gotthardt M, Schultheiss HP, Tschope C (2009) Enhancement of the endothelial NO synthase attenuates experimental diastolic heart failure. Basic Res Cardiol 104:499–509. doi:10.1007/s00395-009-0014-6
Westermann D, Rutschow S, Jager S, Linderer A, Anker S, Riad A, Unger T, Schultheiss HP, Pauschinger M, Tschope C (2007) Contributions of inflammation and cardiac matrix metalloproteinase activity to cardiac failure in diabetic cardiomyopathy: the role of angiotensin type 1 receptor antagonism. Diabetes 56:641–646. doi:10.2337/db06-1163
Westermann D, Savvatis K, Lindner D, Zietsch C, Becher PM, Hammer E, Heimesaat MM, Bereswill S, Volker U, Escher F, Riad A, Plendl J, Klingel K, Poller W, Schultheiss HP, Tschope C (2011) Reduced degradation of the chemokine MCP-3 by matrix metalloproteinase-2 exacerbates myocardial inflammation in experimental viral cardiomyopathy. Circulation 124:2082–2093. doi:10.1161/CIRCULATIONAHA.111.035964
Westermann D, Walther T, Savvatis K, Escher F, Sobirey M, Riad A, Bader M, Schultheiss HP, Tschope C (2009) Gene deletion of the kinin receptor B1 attenuates cardiac inflammation and fibrosis during the development of experimental diabetic cardiomyopathy. Diabetes 58:1373–1381. doi:10.2337/db08-0329
Yamamoto E, Kataoka K, Dong YF, Nakamura T, Fukuda M, Tokutomi Y, Matsuba S, Nako H, Nakagata N, Kaneko T, Ogawa H, Kim-Mitsuyama S (2009) Aliskiren enhances the protective effects of valsartan against cardiovascular and renal injury in endothelial nitric oxide synthase-deficient mice. Hypertension 54:633–638. doi:10.1161/HYPERTENSIONAHA.109.133884
Yin J, Kukucka M, Hoffmann J, Sterner-Kock A, Burhenne J, Haefeli WE, Kuppe H, Kuebler WM (2011) Sildenafil preserves lung endothelial function and prevents pulmonary vascular remodeling in a rat model of diastolic heart failure. Circ Heart Fail 4:198–206. doi:10.1161/CIRCHEARTFAILURE.110.957050
Acknowledgments
We thank Kerstin Puhl, Georg Zingler, and Nadine Orrin for excellent technical assistance. This study was funded by the Deutsche Forschungsgesellschaft (SFB TR-19; A2, Z3).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
D. Westermann and P. M. Becher contributed equally to this work.
Rights and permissions
About this article
Cite this article
Westermann, D., Becher, P.M., Lindner, D. et al. Selective PDE5A inhibition with sildenafil rescues left ventricular dysfunction, inflammatory immune response and cardiac remodeling in angiotensin II-induced heart failure in vivo. Basic Res Cardiol 107, 308 (2012). https://doi.org/10.1007/s00395-012-0308-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-012-0308-y