Abstract
Cardiac rupture is a fatal complication of myocardial infarction (MI); however, its underlying molecular mechanisms are not fully understood. This study investigated the role of tissue inhibitor of metalloproteinase-3 (TIMP-3)/matrix metalloproteinase (MMP)/epidermal growth factor (EGF)/transforming growth factor (TGF)-β1 pathway in infarct healing and effects of cetuximab on cardiac rupture after MI. Induction of MI was achieved by left coronary artery ligation in wild-type (WT) and TIMP-3−/− mice. TIMP-3 deficiency resulted in a fourfold increase in cardiac rupture and 50% decrease in survival after MI. Hydroxyproline content, collagen synthesis and myofibroblast cell number in the infarct region, and the force required to induce rupture of the infarct scar were significantly decreased, while MMP activity was increased in TIMP-3−/− mice. EGF proteins were increased by threefold in TIMP-3−/− mice following MI, while TGF-β1 mRNA levels were decreased by 68%. Cell proliferation of cultured adult cardiac myofibroblasts was significantly decreased in TIMP-3−/− compared to WT myofibroblasts. EGF treatment significantly decreased collagen synthesis and TGF-β1 expression. Conversely, TGF-β1 treatment increased collagen synthesis in cardiac myofibroblasts. Treatment with cetuximab significantly decreased the incidence of cardiac rupture and improved survival post-MI in TIMP-3−/− mice. We conclude that deficiency in TIMP-3 increases cardiac rupture post-MI via EGF/epidermal growth factor receptor (EGFR) signaling which downregulates TGF-β1 expression and collagen synthesis. Inhibition of EGFR by cetuximab protects against cardiac rupture and improves survival post-MI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The myocardial extracellular matrix (ECM) plays an important role in maintaining the integrity and function of the heart [9]. The major constituents of the myocardial ECM are the fibrillar collagens composed of the tensile collagen I (80%), which is crucial for coordinating contraction, and collagen III (10%), which provides elasticity [3, 9]. Fibrillar collagens are synthesized as precursor peptides that are proteolytically cleaved at the amino- and carboxy-terminals before being inserted into the nascent fibrils [3]. One of the major inducers of collagen expression and synthesis by fibroblasts is transforming growth factor-beta (TGF-β) [3]. Remodeling of the ECM is mediated by the matrix metalloproteinases (MMPs) [40] and their endogenous inhibitors, the tissue inhibitors of metalloproteinases (TIMPs) [2]. An imbalance between the activities of MMPs and TIMPs can impair infarct healing and result in cardiac rupture, a fatal complication following myocardial infarction (MI) [18, 36].
TIMPs are a family of four homologous proteins all of which are expressed in the heart [9]. Unique among the TIMPs, TIMP-3 is ECM bound, a potent inhibitor of all known MMPs, and is expressed at high levels in the healthy heart. However, in the diseased heart, TIMP-3 expression is reduced in association with maladaptive myocardial remodeling in patients with congestive heart failure [7]. Furthermore, loss of TIMP-3 expression in aged mice triggers progressive myocardial remodeling and dysfunction even in the absence of imposed stresses or injuries [8].
Following MI, cardiac fibroblasts initially repopulate the injured area through chemotaxis. This is followed by increased proliferation and differentiation into myofibroblasts, and formation of a granulated scar [3]. Subsequently, remodeling of the ECM occurs and ultimately leads to the formation of a mature scar tissue which is composed of collagen, fibroblasts, newly formed capillaries, and macrophages [4, 21, 37]. TIMP-3 is a potent inducer of cardiac fibroblast proliferation [27]. A recent study showed that incidence of pericardial bleeding, indicative of cardiac rupture, was increased in TIMP-3−/− mice post-MI [38], suggesting a potential role of TIMP-3 in infarct scar healing. Cardiac rupture is an infrequent but lethal complication of MI. Clinical studies have shown that incidence of cardiac rupture occurs in about 4% of all patients admitted with an acute MI, but is responsible for 12% of in-hospital mortality after thrombolytic therapy [1, 19, 33]. Post-mortem examinations showed cardiac ruptures in 31–65% of patients who died of acute MI [20, 30]. Thus, understanding the underlying mechanisms that lead to cardiac rupture will aid in the development of drugs that will decrease mortality following MI.
Cetuximab (Erbitux®) is a human-murine chimeric monoclonal antibody against epidermal growth factor receptor (EGFR) and has been approved for the treatment of head and neck cancer and colorectal cancer [12, 34]. However, its effects on cardiac rupture post-MI have not been previously investigated. We have recently demonstrated that TIMP-3 inhibits epidermal growth factor (EGF)/EGFR signaling via inhibition of MMP activity in the heart [17]. EGF has been implicated in inhibiting collagen synthesis [6, 22, 23] and the expression of TGF-β1 [44] which is a potent inducer of collagen synthesis [3, 13, 24, 25]. In the present study, we hypothesized that TIMP-3 deficiency increases cardiac rupture post-MI via EGF/EGFR signaling which downregulates TGF-β1 expression and collagen synthesis. Furthermore, we hypothesized that treatment with cetuximab to inhibit EGFR signaling protects against cardiac rupture post-MI. Using a clinically relevant mouse model of MI, and cellular, molecular techniques, our study showed that the incidence of cardiac rupture was increased in TIMP-3−/− mice post-MI via EGF/EGFR signaling and downregulation of TGF-β1 expression and collagen synthesis in the infarct myocardium. Moreover, treatment with cetuximab decreased cardiac rupture and improved survival in TIMP-3−/− mice post-MI.
Materials and methods
Animals
Wild-type (WT) mice of the genetic background C57BL/6 were purchased from Charles River Laboratories (Wilmington, MA). TIMP-3−/− mice were generated as described previously [26] and back-crossed more than seven generations into the C57BL/6 background. Animals were provided with food and water ad libitum and maintained in a temperature and humidity controlled facility with 12-h light and dark cycles. A breeding program was carried out to generate adults (males, 2–7 months old) for this study. Animal studies were approved by the University of Western Ontario Institutional Animal Care and Use Committee, and the investigation conformed with the Guide for the Care and Use of Laboratory Animals, published by National Institutes of Health (NIH Publication No. 85-23, revised 1996).
Myocardial infarction
MI was induced by occlusion of the left anterior descending coronary artery as we have previously described [10]. Experiments were conducted at 5 or 30 days post-surgery to mimic early and later stages of heart failure, respectively. Survival was monitored, and incidence of cardiac rupture and the left ventricle (LV) to body weight ratio were recorded. Mice with infarct sizes between 30 and 45% were used in all studies.
Assessment of cardiac rupture
Deceased mice were examined within 12 h. The chest was opened to examine bleeding around the infarct region. Hearts were then removed and the LV chamber was cannulated with a 20 G blunt end IV catheter via the aorta and perfused with 200 μl saline to determine if there was leakage from the infarct region. Histological examination was conducted to confirm the region of cardiac rupture. Briefly, WT and TIMP-3−/− hearts were isolated after death post-MI and fixed in 4% paraformaldehyde and embedded in paraffin. Samples were then sectioned (5 μm), stained with hematoxylin/eosin and visualized using a Zeiss microscope (Observer D1) as in our previous study [11].
MMP activity
MMP activity was measured using the Sensolyte 520 Generic MMP Assay Kit (AnaSpec, CA) as per manufacturer’s instructions. Briefly, LV tissues from sham and peri-infarct tissues from MI were collected 2 days after surgery, homogenized and incubated with the FAM/QXL 520 FRET substrate for 1 h in a black 96-well plate at room temperature in the dark. Measurements were made using a SpectraMax M5 microplate reader at excitation and emission wavelengths of 490 and 520 nm, respectively. A standard curve was created using 5-FAM-Pro-Leu-OH to convert fluorescence values into amount of substrate cleaved. Values are expressed as pmol substrate cleaved/mg protein.
Hydroxyproline content
Hydroxyproline concentration was determined using the colorimetric method described by Woessner [42] with modifications. Briefly, LV infarct regions were isolated from WT and TIMP-3−/− mice 5 days post-MI, dried overnight, weighed the following morning and hydrolyzed in 6 N HCl for 4–5 h at 130°C. The samples were then treated with 5 N NaOH solution. Subsequently, 0.1 M chloramine-T was added and samples were incubated at room temperature for 20 min. This was followed by addition of 6.25 M perchloric acid for 5 min at room temperature, and then incubation of samples in 20% p-dimethylaminobenzaldehyde for 20 min at 60°C. Measurements were made using SpectraMax M5 microplate reader at a wavelength of 565 nm. A standard curve was created using l-hydroxyproline to convert sample colorimetric values into mg of hydroxyproline. Values are expressed as mg hydroxyproline/g dry weight.
Measurement of EGF levels
The LV tissues from sham and infarct regions from MI mice 5 days after surgery were homogenized in phosphate-buffered saline (PBS) and centrifuged. The supernatant was then collected and protein concentrations were measured. EGF protein levels in the LV myocardium were determined using a mouse EGF Quantikine ELISA kit (R&D systems, MN) according to the manufacturer’s instructions. Values are expressed as pg EGF levels per mg myocardial tissue.
Stretch experiments
The left ventricular free wall and infarct region were isolated 5 days after sham or MI surgery. Tissues were cut into 2 × 5 mm pieces with one end attached to a force transducer and the other end attached to a micromanipulator. Increasing tensions were then applied to the tissue and the force was recorded when rupture occurred. The threshold force to induce scar rupture was adjusted by tissue dimensions measured under a Zeiss dissecting scope.
Isolation and culturing of adult cardiac myofibroblasts
Cardiac myofibroblast cultures were prepared from ventricles of WT and TIMP-3−/− mice as previously described [16]. Briefly, hearts were aseptically isolated from adult mice. The ventricles were minced and digested with collagenase and dispase. Fibroblasts at passage 2 were seeded on culture plates and used for all in vitro experiments. After two passages virtually all fibroblasts differentiate into myofibroblasts [41]. Purity of myofibroblasts was verified by FSP-1 (S100A4, Abcam, MA) and α-smooth muscle actin (clone 1A4, Sigma-Aldrich, MO) double staining. Cell proliferation was assessed by Ki67 and FSP-1 double staining.
To determine the effect of EGF and TGF-β1 on collagen expression and synthesis, adult cardiac myofibroblasts at passage 2 were placed in low serum (5% FBS) for 24 h and subsequently treated with either recombinant mouse EGF (rEGF, R&D Applied Biosystems, CA) in DMEM containing 5% FBS and cultured for another 24 h or TGF-β1 (Millipore, MA) and cultured for another 48 h. Cells were then harvested and experiments were conducted.
Myofibroblast proliferation
LV tissues from the infarct region of 5-day MI operated and TIMP-3−/− mice were isolated, embedded in paraffin, sectioned and stained. Briefly, after deparaffinization, heart sections were placed in sodium citrate (pH 6.0) and microwaved for 10 min to allow for antigen retrieval. Subsequently, sections were treated with 0.3% H2O2–H2O for 30 min at room temperature, to inhibit endogenous peroxidase activity. Sections were then blocked in 1.5% goat serum for 30 min, at which point they were incubated with FSP-1 (1:400, S100A4, Abcam, MA) overnight at 4°C. The following day, sections were incubated with a biotinylated goat anti-rabbit IgG (1:500, Vector Laboratories) for 30 min at room temperature, and then incubated with an avidin–biotin-peroxidase amplification system (Vector Laboratories) for 30 min at room temperature. The chromogen diaminobenzidine at a concentration of 0.4 mg/ml (10 min at room temperature) was used to detect FSP-1 staining with hematoxylin as a counterstain. The number of FSP-1 positive cells per mm2 is presented.
Collagen I synthesis
Collagen I synthesis was assessed in the LV myocardium and in conditioned media collected for cultured myofibroblasts using a rat/mouse procollagen I N-terminal peptide (PINP) ELISA kit (IDS-Medicorp, Quebec) according to the manufacturer’s instructions. The LV tissues of sham mice and the infarct regions of WT and TIMP-3−/− mice 5 days post-MI were homogenized in PBS and centrifuged. The supernatant was then collected and protein concentrations were measured. For tissues, 25 μg of total protein was used, while for media 10 μl of conditioned media was used in the assay. Measurements of absorbances were made using SpectraMax M5 microplate reader at a wavelength of 450 nm. Values are expressed as either ng collagen per mg myocardial tissue or ng/ml conditioned media.
Real-time RT-PCR
Total RNA was extracted from cultured adult cardiac myofibroblasts as well as LV tissue of WT and TIMP-3−/− sham and the infarct region of MI mice 5 days post-surgery using Trizol as previously described [31, 32]. cDNA was synthesized using M-MLV reverse transcriptase (Invitrogen, ON). Real-time PCR was conducted using SYBR Green PCR Master Mix as per manufacturer’s instructions (Applied Biological Materials, BC). 28S rRNA (house keeping gene) was used as a loading control since previous studies have shown that it is a reliable loading control especially for use in experiments with hypoxia [45] and MI [14].
Hemodynamic measurements
Cardiac function was measured at 5 and 30 days post-MI using a Millar pressure transducer catheter (Model SPR-839, Size 1.4F) as previously described [28]. Measurements included arterial pressures, heart rate (HR), LV systolic and end-diastolic pressures, as well as the maximal rate of LV pressure development (+dP/dt) and maximal rate of pressure relaxation (−dP/dt). Animals were killed after hemodynamic measurements and cardiac hypertrophy was assessed by determination of the heart weight (mg) to the body weight (g) ratio.
Cetuximab treatment
Following MI, WT and TIMP-3−/− mice were treated with cetuximab (Erbitux®, 10 mg/kg) immediately by an IV injection, which was followed by IV injections at day 3 and 5 post-MI, respectively. Survival was monitored for 30 days after MI. Hemodynamic measurements were made at 5 and 30 days post-MI. Post-mortem examinations were performed in all mice that died after MI to identify cardiac ruptures.
Statistical analysis
Data are presented as mean ± SEM. Unpaired Student’s t test, Chi-square, one- or two-way ANOVA followed by Bonferroni post tests were performed as appropriate. P < 0.05 was considered statistically significant.
Results
Survival and cardiac function post-MI
WT (n = 74) and TIMP-3−/− (n = 81) mice were subjected to MI or sham operations, and survival was followed up to 30 days after surgery. MI resulted in a significant decrease in survival in both WT and TIMP-3−/− mice compared to the sham-operated groups (P < 0.05, Fig. 1a). Furthermore, following MI, survival was significantly decreased in TIMP-3−/− mice as compared to WT (P < 0.001, Fig. 1a). There was no significant difference in infarct size between WT and TIMP-3−/− mice at 5 days (38.6 ± 2.9 vs. 38.3 ± 3.3%) or 30 days (37.9 ± 2.0 vs. 41.3 ± 3.3%) post-MI. To determine if the decrease in survival observed in the TIMP-3−/− mice following MI was due to cardiac dysfunction, hemodynamic analysis was performed at 5 and 30 days post-MI. To that end, we measured HR, mean arterial pressure (MAP), left ventricular systolic pressure (LVSP), left ventricular end-diastolic pressure (LVEDP), and maximal positive and minimal negative first derivative of left ventricular pressure (+dP/dt max and −dP/dt min) using the Millar tip-transducer catheter. Our data demonstrated that there were no significant differences in any of the parameters after sham or MI surgery between WT and TIMP-3−/− mice (P = n.s., Table 1). Furthermore, there was no significant difference in cardiac hypertrophy as measured by heart/body weight ratio between WT and TIMP-3−/− (3.6 ± 0.19 vs. 3.4 ± 0.21 mg/g, P = n.s.) mice at 30 days post-MI. Taken together, these data suggest that the increased mortality in the TIMP-3−/− is not due to cardiac dysfunction.
Survival and cardiac rupture after myocardial infarction (MI) in wild-type (WT) and TIMP-3−/− mice. a Kaplan–Meier survival curves of WT and TIMP-3−/− mice after MI with and without cetuximab treatment. Thirty-day survival was significantly decreased in TIMP-3−/− compared to WT mice post-MI (P < 0.001), which was rescued by cetuximab treatment. b A typical example of LV free wall cardiac rupture (arrow) with hematoxylin and eosin staining. c Incidence of cardiac rupture after MI with and without cetuximab treatment. Numbers in bars are rupture/total mouse numbers. d Determination of the force required to induce infarct scar rupture. The infarct scar was isolated 5 days post-MI and used for the stretch experiment (n = 10–11 per group). Error bars are ±SEM; *P < 0.05, **P < 0.001 versus WT MI without treatment. †P <0.05 versus TIMP-3−/− MI without treatment
Cardiac rupture post-MI
To determine a possible cause for the increase in mortality in TIMP-3−/− mice following MI, a post-mortem was performed. LV free wall cardiac rupture as confirmed by histological examination in addition to evidence of bleeding and perfusion leakage from the infarct region was found in both groups. A typical example of infarct rupture is shown in Fig. 1b. TIMP-3 deficiency resulted in a fourfold increase in the incidence of cardiac rupture following MI as compared to WT mice (P < 0.001, Fig. 1c). Stretch experiments were conducted to determine the force required to induce infarct scar rupture. Our results demonstrated that the force required to induce scar rupture in the TIMP-3−/− mice following MI was significantly lower than that for WT (P < 0.05, Fig. 1d). There was no significant difference in the force inducing rupture between WT and TIMP-3−/− mice (15.7 ± 1.9 vs. 16.4 ± 2.5 g, P = n.s.) following sham operations.
Effects of cetuximab on cardiac rupture, function and survival
Treatment with cetuximab (10 mg/kg) immediately, and at day 3 and 5 post-MI significantly decreased the incidence of cardiac rupture in TIMP-3−/− mice (12 vs. 34%, P < 0.05, Fig. 1c). Although cardiac function was not significantly different at day 5, LVSP and LV +dP/dt were significantly increased after cetuximab treatment in TIMP-3−/− mice 30 days post-MI (P < 0.05, Table 1), indicating a significant improvement in contractile function. Furthermore, treatment with cetuximab significantly improved 30-day survival post-MI in TIMP-3−/− mice (62.5 vs. 22.7%, P < 0.01, Fig. 1a). However, cetuximab treatment did not have any significant effect on cardiac rupture, function or survival in WT mice (P = n.s., Table 1; Fig. 1a, c).
ECM remodeling, EGF and TGF-β1 expression post-MI
To determine a potential mechanism for cardiac rupture in the TIMP-3−/− mice, we measured MMP activity and collagen content. MMP activity was measured at 2 days post-MI since previous studies have shown that MMP activity is elevated shortly post-MI [9]. Collagen content was assessed at 5 days post-MI, a time point at which mortality was the highest as demonstrated by the survival curve (Fig. 1a). Our results showed that MMP activity was significantly increased in WT and TIMP-3−/− mice post-MI as compared to sham controls. Moreover, MMP activity was significantly higher in TIMP-3−/− mice compared to their WT counterparts post-MI (P < 0.01, Fig. 2a). The collagen content as determined by hydroxyproline measurement was significantly increased in both WT and TIMP-3−/− mice following MI as compared to their respective shams. However, TIMP-3−/− mice had significantly lower levels of collagen in the infarct region compared to WT following MI (P < 0.01, Fig. 2b). Furthermore, determination of the collagen expression through real-time PCR analysis revealed that collagen I and III mRNA levels in the infarct myocardium were increased in WT and TIMP-3−/− mice as compared to sham controls. However, the TIMP-3−/− mice had significantly lower collagen expression levels compared to their WT counterparts following MI (P < 0.01, Fig. 3a, b). In addition, since collagen I is the predominant collagen isoform in the heart [3, 9], we measured its synthesis using an ELISA kit that assesses collagen I N-terminal propeptide (PINP) levels. Our data showed that collagen I synthesis was significantly elevated in both WT and TIMP-3−/− mice following MI as compared to their respective shams; however, there was significantly lower collagen I synthesis in the TIMP-3−/− as compared to WT mice post-MI (P < 0.01, Fig. 3c).
Assessment of MMP activity and collagen content in wild-type (WT) and TIMP-3−/− mice. a MMP activity was assessed in the peri-infarct zone 2 days post-MI using a fluorescence based assay. b Collagen content was assessed 5 days post-MI in the infarct region by hydroxyproline measurement. Data are mean ± SEM. N = 4–6 mice per group. *P < 0.01 versus corresponding sham within genotype, † P < 0.01 versus WT MI
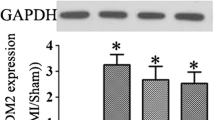
Collagen levels, EGF and TGF-β1 expression in sham LV tissues and in the infarct region after myocardial infarction (MI) in wild-type (WT) and TIMP-3−/− mice 5 days post-MI. Collagen I (a) and III (b) mRNA levels as measured by real-time PCR. Collagen I synthesis (c) and EGF levels (d) as measured by ELISA. e TGF-β1 mRNA as measured by real-time PCR. Data are mean ± SEM. N = 4–6 mice per group. *P < 0.01 versus corresponding sham within genotype, † P < 0.01 versus WT MI
As EGF inhibits collagen synthesis [22, 23] and regulates the expression of TGF-β1 [44], a critical inducer for collagen production [3, 24, 25] and since we have recently demonstrated that TIMP-3 inhibits EGF signaling in the heart [17], we measured EGF and TGF-β1 levels in both WT and TIMP-3−/− mice following MI. Our results showed that EGF levels were significantly increased (P < 0.05, Fig. 3d), while TGF-β1 levels were significantly decreased in the infarct myocardium of TIMP-3−/− mice as compared to WT (P < 0.01, Fig. 3e). These data suggest that TIMP-3 inhibits EGF but promotes TGF-β1 expression. Furthermore, EGF levels were negatively correlated with collagen and TGF-β1 expression (Fig. 3a–e).
Effect of EGF on collagen synthesis and TGF-β1 expression in adult cardiac myofibroblasts
To further demonstrate a negative effect of EGF on collagen and TGF-β1 expression, adult cardiac myofibroblasts were cultured, as these cells produce the majority of the collagen in the heart [3]. Treatment of adult cardiac myofibroblasts with 1 ng/ml EGF (low concentration) had little effect on collagen I or III expression. However, treatment with 10 ng/ml EGF (high concentration) resulted in a significant decrease in collagen I and III expression (P < 0.01, Fig. 4a, b), a decrease in collagen I synthesis (P < 0.01, Fig. 4c) as well as a decrease in TGF-β1 expression (P < 0.01, Fig. 4d) in both WT and TIMP-3−/− myofibroblasts. The decrease was more pronounced in the TIMP-3−/− as compared to WT for collagen I (47 vs. 38%), and collagen III (51 vs. 41%) expression, collagen I synthesis (39 vs. 28%) and TGF-β1 (43 vs. 22%) levels, respectively (P < 0.01, Fig. 4a–d). These data showed that EGF inhibits collagen I and III as well as TGF-β1 expression in the cardiac myofibroblasts.
Effect of EGF on collagen synthesis and TGF-β1 expression in adult cardiac myofibroblasts. WT and TIMP-3−/− adult cardiac myofibroblasts at passage 2 were treated with 1 or 10 ng/ml mouse recombinant EGF for 24 h and the mRNA expression of collagen I (a), and III (b) was assessed by real-time PCR. c Collagen I synthesis was measured by PINP ELISA. d TGF-β1 mRNA expression was measured by real-time PCR. Data are mean ± SEM from 5 to 7 independent experiments. *P < 0.05, **P < 0.01 versus corresponding control within genotype; † P < 0.05, ‡ P < 0.01 versus corresponding WT
Effects of TGF-β1 on collagen synthesis in adult cardiac myofibroblasts
To demonstrate a causal relationship between TGF-β1 and collagen synthesis, cultured adult cardiac myofibroblasts from WT and TIMP-3−/− mice were employed. Treatment of adult cardiac myofibroblasts with 1 ng/ml TGF-β1 (low concentration) resulted in a significant increase in collagen I and III expression (P < 0.05, Fig. 5a, b). Treatment with 10 ng/ml TGF-β1 (high concentration) resulted in a further increase in collagen I expression and synthesis (P < 0.01, Fig. 5a, c), while it had no effect on collagen III compared to controls (P = n.s., Fig. 5b). These effects of TGF-β1 were significantly decreased in TIMP-3−/− compared to WT myofibroblasts (P < 0.01, Fig. 5a–c). These results demonstrated that TGF-β1 promotes collagen synthesis in the cardiac myofibroblasts.
Effect of TGF-β1 on collagen synthesis in adult cardiac myofibroblasts. WT and TIMP-3−/− adult cardiac myofibroblasts at passage 2 were treated with 1 or 10 ng/ml human recombinant TGF-β1 for 48 h and mRNA levels of collagen I (a) and III (b) were assessed by real-time PCR analysis, while collagen I synthesis was determined by PINP ELISA (c). Data are mean ± SEM from 3 to 6 independent experiments. *P < 0.05, **P < 0.01 versus corresponding control within genotype; † P < 0.05, ‡ P < 0.01 versus corresponding WT
TIMP-3 deficiency decreases adult cardiac myofibroblast proliferation
As previous studies have shown that overexpression of TIMP-3 using an adenoviral construct increases cardiac fibroblast proliferation [27], we wanted to determine whether the decrease in collagen synthesis in the TIMP-3−/− may be due to, at least in part, a decrease in (myo)fibroblast proliferation. To that end, the LV tissue sections of WT and TIMP-3−/− mice at 5 days post-MI were subjected to immunostaining using the fibroblast specific protein-1 (FSP-1) (Fig. 6a), which is expressed in the nucleus and the cytoplasm of fibroblasts and myofibroblasts [29]. Our data showed that the number of (myo)fibroblasts was significantly decreased in the infarct region of TIMP-3−/− mice as compared to their WT counterparts after MI (P < 0.01, Fig. 6a). To further study the role of TIMP-3 in cardiac myofibroblast proliferation, adult cardiac myofibroblasts were isolated and cultured for two passages. The culture was determined to be 99% pure through immunostaining of FSP-1 (Fig. 6b). We also stained for α-smooth muscle actin (Fig. 6b), a marker which is expressed in myofibroblasts but not fibroblasts. Our results showed that virtually all cells at passage 2 were myofibroblasts as seen by α-smooth muscle actin and FSP-1 double staining (Fig. 6b). This is consistent with a previous finding that the majority of the fibroblasts in culture differentiate into myofibroblasts by the second passage [41]. Proliferation of the myofibroblasts was assessed by Ki67 and FSP-1 double staining (Fig. 6c) and confirmed using the NucleoCounter at 24 and 48 h post-seeding (Fig. 6d). Our data showed that loss of TIMP-3 resulted in a significant decrease in cardiac myofibroblast proliferation (P < 0.05, Fig. 6c, d).
Adult cardiac myofibroblast proliferation in vivo and in vitro. a (Myo)fibroblast proliferation in the infarct myocardium of wild-type (WT) and TIMP-3−/− mice 5 days post-myocardial infarction (MI) was measured by FSP-1 staining (red arrows) and the total number of (myo)fibroblasts/mm2 is presented (n = 6 per group). b The purity of the adult cardiac myofibroblast culture at passage 2 was verified by FSP-1 staining (green) and α-smooth muscle actin staining (red). c Myofibroblasts were seeded on coverglasses and proliferation was assessed by Ki67 staining (green, white arrows). Myofibroblasts were identified by FSP-1 staining (red) and nuclei were counterstained with Hoechst 33342. d Myofibroblast proliferation was assessed using the NucleoCounter at 24 and 48 h post-seeding. Data are mean ± SEM. N = 4 and 3 independent experiments for c and d, respectively. *P < 0.05, **P < 0.01 versus WT (a, c) or corresponding 24 h within genotype (d); † P < 0.01 versus WT 48 h
Discussion
Cardiac rupture is a fatal complication after MI; however, its underlying molecular mechanisms are not fully understood [36]. The present study demonstrated that TIMP-3 deficiency results in a significant increase in mortality and incidence of cardiac rupture post-MI. Furthermore, TIMP-3 deficiency increased EGF levels, decreased myofibroblast proliferation, decreased TGF-β1 and collagen synthesis and, therefore, decreased overall collagen content in the infarct myocardium. Importantly, we showed for the first time that treatment with cetuximab decreased incidence of cardiac rupture, improved cardiac function and survival in TIMP-3−/− mice post-MI.
TIMP-3 has been shown to play an important physiological role within the heart as its absence triggers progressive myocardial remodeling and dysfunction with characteristic matrix degradation, cytokine activation and myocardial apoptosis similar to human heart failure in aged mice (21–23 months old) even without imposed stresses [7, 8]. Our data showed that mortality was significantly increased in TIMP-3−/− mice following MI as compared to WT. The majority of the observed mortality in TIMP-3−/− mice occurred around day 5 post-MI. To determine whether cardiac dysfunction could contribute to the increase in mortality observed in TIMP-3−/− mice, we performed hemodynamic analysis on WT and TIMP-3−/− mice following sham or MI operations. Importantly, all the mice used in our study were between 2 and 7 months of age to minimize influences of aging in the present study. Our data demonstrated that there were no significant differences in cardiac function between WT and TIMP-3−/− at 5 or 30 days post-MI. Furthermore, there was no significant difference in cardiac hypertrophy between WT and TIMP-3−/− at 30 days post-MI. Therefore, unlike the study by Tian et al. [38], our results suggest that the increased mortality in the TIMP-3−/− is not due to cardiac dysfunction. This discrepancy between our study and that conducted by Tian et al. is not completely clear, but could be due to differences in the severity of the MI model. The infarct sizes used in our study were between 30 and 45%, whereas Tian et al. [38] did not measure infarct size in their study. In our study, there was approximately a 50% decrease in survival in the TIMP-3−/− mice as compared to WT, whereas in their study the decrease was only 20%, suggesting that our model was much more severe. A severe model of MI would, therefore, cause a significant decrease in cardiac function in both groups, thus making it difficult to see differences between WT and TIMP-3−/− mice.
To determine a possible cause for the increased incidence of mortality in the TIMP-3−/− mice following MI, a post-mortem was performed and cardiac rupture as confirmed by histological examination was found to be the primary cause of death. Stretch experiments were then conducted to investigate if TIMP-3−/− mice had weakened scar tissues. Our results demonstrated that the force required to induce scar rupture in the TIMP-3−/− mice following MI was significantly lower than that for WT. These data suggest that there is improper scar healing in the TIMP-3−/− mice. To further study potential mechanisms responsible for the weakened scar tissue in TIMP-3−/− mice, MMP activity and collagen content were measured. We demonstrated that MMP activity was significantly elevated in the TIMP-3−/− mice, and the collagen content was significantly reduced. These results are in agreement with a previous study that showed reduced collagen content and increased MMP activity in the TIMP-3−/− myocardium following MI [38]. Furthermore, determination of the collagen expression revealed that collagen I and III were increased in WT and TIMP-3−/− mice following MI as compared to sham controls. A novel finding in our study is that the TIMP-3−/− mice had significantly lower collagen expression and synthesis levels compared to their WT counterparts following MI. Thus, the decrease in collagen content assessed through measurement of hydroxyproline content is not only due to increased matrix degradation as was previously thought, but also due to decreased collagen synthesis.
We recently demonstrated that TIMP-3 inhibits EGF/EGFR signaling in the heart [17]. EGF has been shown to regulate the expression of TGF-β1, a major inducer of collagen in several cell types [5, 35, 39, 44]. However, the effects of EGF on TGF-β1 expression and collagen synthesis in the heart have not been previously investigated. We, therefore, measured EGF and TGF-β1 levels in the infarct myocardium. Our results demonstrated that myocardial EGF levels were significantly elevated, while those of TGF-β1 were significantly reduced in TIMP-3−/− mice following MI as compared to WT. To further study the effects of EGF and TGF-β1 on collagen expression, adult cardiac myofibroblasts were cultured and treated with recombinant EGF or TGF-β1. Our data demonstrated that treatment with recombinant EGF significantly inhibited collagen synthesis and TGF-β1 expression in cardiac myofibroblasts and the opposite effect on collagen synthesis was observed following TGF-β1 treatment.
TIMP-3 has been shown to promote myofibroblast proliferation [27, 43] which are the main producers of collagen in the heart [3]. In the present study, we wanted to determine whether the decrease in collagen synthesis could be explained, at least in part, by a decrease in myofibroblast proliferation in TIMP-3−/− mice. Our results demonstrated that there was a significant decrease in the number of myofibroblasts in the TIMP-3−/− compared to WT mice post-MI. Furthermore, a decrease in proliferation was also verified in primary cultures of adult cardiac myofibroblasts from TIMP-3−/− mice. Taken together, our data suggest that deficiency in TIMP-3 upregulates EGFR signaling and decreases cardiac myofibroblast proliferation and collagen synthesis in the infarct myocardium.
To further study the role of EGFR signaling in infarct healing post-MI, we employed cetuximab, a chimeric monoclonal antibody against EGFR in the present study. Treatment with cetuximab decreased the incidence of cardiac rupture, and significantly improved cardiac function and survival in TIMP-3−/− mice post-MI. These data suggest a key role of EGFR signaling responsible for cardiac rupture and high mortality in TIMP-3−/− mice post-MI. It should be noted that cetuximab did not have any effects on cardiac rupture, function and survival in the WT mice. The reason for this is not completely clear. Activities of TIMP-3 and MMPs are critical to ECM remodeling and infarct scar healing. In the WT, the activities of TIMP-3 and MMPs appear to be balanced as evidenced by the low incidence of cardiac rupture post-MI. In addition, TIMP-3 inhibited MMP activity and decreased EGF ligand shedding as shown by significantly lower EGF levels in WT compared to TIMP-3−/− mice post-MI. Furthermore, our in vitro studies showed that treatment of cardiac myofibroblasts with a low dose of EGF had little effect on collagen expression, only a high dose of EGF caused a significant decrease in TGF-β1 expression and collagen I synthesis. These data suggest that EGF/EGFR activity may be much lower in WT in comparison to TIMP-3−/− mice. Thus, treatment with cetuximab had no effects in the WT mice. Interestingly, studies have shown that the incidence of cardiac rupture in 129sv mice is more than double in C57BL/6 mice post-MI [15]. The 129sv mice would, therefore, represent an interesting model to study the effects of cetuximab in future investigations.
In conclusion, the present study demonstrated that deficiency in TIMP-3 increases cardiac rupture post-MI via EGF/EGFR signaling and downregulation of TGF-β1 expression and collagen synthesis in the infarct myocardium. Inhibition of EGFR by cetuximab protects against cardiac rupture and improves survival in TIMP-3−/− mice post-MI. Our study suggests that cetuximab may have therapeutic potential in protecting against cardiac rupture after MI, especially in patients with thrombolytic therapy where risk of cardiac rupture is much higher [1].
References
Becker RC, Gore JM, Lambrew C, Weaver WD, Rubison RM, French WJ, Tiefenbrunn AJ, Bowlby LJ, Rogers WJ (1996) A composite view of cardiac rupture in the United States National Registry of Myocardial Infarction. J Am Coll Cardiol 27:1321–1326. doi:10.1016/0735-1097(96)00008-3
Brew K, Dinakarpandian D, Nagase H (2000) Tissue inhibitors of metalloproteinases: evolution, structure and function. Biochim Biophys Acta 1477:267–283. doi:10.1016/S0167-4838(99)00279-4
Brown RD, Ambler SK, Mitchell MD, Long CS (2005) The cardiac fibroblast: therapeutic target in myocardial remodeling and failure. Annu Rev Pharmacol Toxicol 45:657–687. doi:10.1146/annurev.pharmtox.45.120403.095802
Cleutjens JP, Verluyten MJ, Smiths JF, Daemen MJ (1995) Collagen remodeling after myocardial infarction in the rat heart. Am J Pathol 147:325–338
Cosgaya JM, Aranda A (1996) Ras- and Raf-mediated regulation of transforming growth factor beta 1 gene expression by ligands of tyrosine kinase receptors in PC12 cells. Oncogene 12:2651–2660
Creely JJ, DiMari SJ, Howe AM, Hyde CP, Haralson MA (1990) Effects of epidermal growth factor on collagen synthesis by an epithelioid cell line derived from normal rat kidney. Am J Pathol 136:1247–1257
Fedak PW, Altamentova SM, Weisel RD, Nili N, Ohno N, Verma S, Lee TY, Kiani C, Mickle DA, Strauss BH, Li RK (2003) Matrix remodeling in experimental and human heart failure: a possible regulatory role for TIMP-3. Am J Physiol Heart Circ Physiol 284:H626–H634. doi:10.1152/ajpheart.00684.2002
Fedak PW, Smookler DS, Kassiri Z, Ohno N, Leco KJ, Verma S, Mickle DA, Watson KL, Hojilla CV, Cruz W, Weisel RD, Li RK, Khokha R (2004) TIMP-3 deficiency leads to dilated cardiomyopathy. Circulation 110:2401–2409. doi:10.1161/01.CIR.0000134959.83967.2D
Fedak PW, Verma S, Weisel RD, Li RK (2005) Cardiac remodeling and failure. From molecules to man (Part II). Cardiovasc Pathol 14:49–60. doi:10.1016/j.carpath.2005.03.004
Feng Q, Lu X, Jones DL, Shen J, Arnold JM (2001) Increased inducible nitric oxide synthase expression contributes to myocardial dysfunction and higher mortality after myocardial infarction in mice. Circulation 104:700–704. doi:10.1161/hc3201.092284
Feng Q, Song W, Lu X, Hamilton JA, Lei M, Peng T, Yee SP (2002) Development of heart failure and congenital septal defects in mice lacking endothelial nitric oxide synthase. Circulation 106:873–879. doi:10.1161/01.CIR.0000024114.82981.EA
Frampton JE (2010) Cetuximab: a review of its use in squamous cell carcinoma of the head and neck. Drugs 70:1987–2010. doi:10.2165/11205010-000000000-00000
Frantz S, Hu K, Adamek A, Wolf J, Sallam A, Maier SK, Lonning S, Ling H, Ertl G, Bauersachs J (2008) Transforming growth factor beta inhibition increases mortality and left ventricular dilatation after myocardial infarction. Basic Res Cardiol 103:485–492. doi:10.1007/s00395-008-0739-7
Gallagher G, Menzie S, Huang Y, Jackson C, Hunyor SN (2007) Regional cardiac dysfunction is associated with specific alterations in inflammatory cytokines and matrix metalloproteinases after acute myocardial infarction in sheep. Basic Res Cardiol 102:63–72. doi:10.1007/s00395-006-0610-7
Gao XM, Xu Q, Kiriazis H, Dart AM, Du XJ (2005) Mouse model of post-infarct ventricular rupture: time course, strain- and gender-dependency, tensile strength, and histopathology. Cardiovasc Res 65:469–477. doi:10.1016/j.cardiores.2004.10.014
Garcia Arguinzonis MI, Galler AB, Walter U, Reinhard M, Simm A (2002) Increased spreading, Rac/p21-activated kinase (PAK) activity, and compromised cell motility in cells deficient in vasodilator-stimulated phosphoprotein (VASP). J Biol Chem 277:45604–45610. doi:10.1074/jbc.M202873200
Hammoud L, Burger DE, Lu X, Feng Q (2009) Tissue inhibitor of metalloproteinase-3 inhibits neonatal mouse cardiomyocyte proliferation via EGFR/JNK/SP-1 signaling. Am J Physiol Cell Physiol 296:C735–C745. doi:10.1152/ajpcell.00246.2008
Hayashidani S, Tsutsui H, Ikeuchi M, Shiomi T, Matsusaka H, Kubota T, Imanaka-Yoshida K, Itoh T, Takeshita A (2003) Targeted deletion of MMP-2 attenuates early LV rupture and late remodeling after experimental myocardial infarction. Am J Physiol Heart Circ Physiol 285:H1229–H1235. doi:10.1152/ajpheart.00207.2003
Honan MB, Harrell FE Jr, Reimer KA, Califf RM, Mark DB, Pryor DB, Hlatky MA (1990) Cardiac rupture, mortality and the timing of thrombolytic therapy: a meta-analysis. J Am Coll Cardiol 16:359–367. doi:10.1016/0735-1097(90)90586-E
Hutchins KD, Skurnick J, Lavenhar M, Natarajan GA (2002) Cardiac rupture in acute myocardial infarction: a reassessment. Am J Forensic Med Pathol 23:78–82
Jankowski M, Bissonauth V, Gao L, Gangal M, Wang D, Danalache B, Wang Y, Stoyanova E, Cloutier G, Blaise G, Gutkowska J (2010) Anti-inflammatory effect of oxytocin in rat myocardial infarction. Basic Res Cardiol 105:205–218. doi:10.1007/s00395-009-0076-5
Kumegawa M, Hiramatsu M, Hatakeyama K, Yajima T, Kodama H, Osaki T, Kurisu K (1983) Effects of epidermal growth factor on osteoblastic cells in vitro. Calcif Tissue Int 35:542–548. doi:10.1007/BF02405091
Kurata S, Hata R (1991) Epidermal growth factor inhibits transcription of type I collagen genes and production of type I collagen in cultured human skin fibroblasts in the presence and absence of l-ascorbic acid 2-phosphate, a long-acting vitamin C derivative. J Biol Chem 266:9997–10003
Leask A (2007) TGFβ, cardiac fibroblasts, and the fibrotic response. Cardiovasc Res 74:207–212. doi:10.1016/j.cardiores.2006.07.012
Leask A, Abraham DJ (2004) TGF-β signaling and the fibrotic response. FASEB J 18:816–827. doi:10.1096/fj.03-1273rev
Leco KJ, Waterhouse P, Sanchez OH, Gowing KL, Poole AR, Wakeham A, Mak TW, Khokha R (2001) Spontaneous air space enlargement in the lungs of mice lacking tissue inhibitor of metalloproteinases-3 (TIMP-3). J Clin Invest 108:817–829. doi:10.1172/JCI12067
Lovelock JD, Baker AH, Gao F, Dong JF, Bergeron AL, McPheat W, Sivasubramanian N, Mann DL (2005) Heterogeneous effects of tissue inhibitors of matrix metalloproteinases on cardiac fibroblasts. Am J Physiol Heart Circ Physiol 288:H461–H468. doi:10.1152/ajpheart.00402.2004
Lu X, Hamilton JA, Shen J, Pang T, Jones DL, Potter RF, Arnold JM, Feng Q (2006) Role of tumor necrosis factor-alpha in myocardial dysfunction and apoptosis during hindlimb ischemia and reperfusion. Crit Care Med 34:484–491. doi:10.1097/01.CCM.0000199079.64231.C1
Maelandsmo GM, Florenes VA, Nguyen MT, Flatmark K, Davidson B (2009) Different expression and clinical role of S100A4 in serous ovarian carcinoma at different anatomic sites. Tumour Biol 30:15–25. doi:10.1159/000199447
Maggioni AP, Maseri A, Fresco C, Franzosi MG, Mauri F, Santoro E, Tognoni G (1993) Age-related increase in mortality among patients with first myocardial infarctions treated with thrombolysis. The Investigators of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI-2). N Engl J Med 329:1442–1448. doi:10.1056/NEJM199311113292002
Peng T, Lu X, Feng Q (2005) Pivotal role of gp91phox-containing NADH oxidase in lipopolysaccharide-induced tumor necrosis factor-alpha expression and myocardial depression. Circulation 111:1637–1644. doi:10.1161/01.CIR.0000160366.50210.E9
Peng T, Lu X, Lei M, Feng Q (2003) Endothelial nitric-oxide synthase enhances lipopolysaccharide-stimulated tumor necrosis factor-alpha expression via cAMP-mediated p38 MAPK pathway in cardiomyocytes. J Biol Chem 278:8099–8105. doi:10.1074/jbc.M207288200
Pollak H, Nobis H, Mlczoch J (1994) Frequency of left ventricular free wall rupture complicating acute myocardial infarction since the advent of thrombolysis. Am J Cardiol 74:184–186. doi:10.1016/0002-9149(94)90098-1
Rodriguez J, Viudez A, Ponz-Sarvise M, Gil-Aldea I, Chopitea A, Garcia-Foncillas J, Gil-Bazo I (2010) Improving disease control in advanced colorectal cancer: panitumumab and cetuximab. Crit Rev Oncol Hematol 74:193–202. doi:10.1016/j.critrevonc.2009.07.005
Sakata Y, Chancey AL, Divakaran VG, Sekiguchi K, Sivasubramanian N, Mann DL (2008) Transforming growth factor-beta receptor antagonism attenuates myocardial fibrosis in mice with cardiac-restricted overexpression of tumor necrosis factor. Basic Res Cardiol 103:60–68. doi:10.1007/s00395-007-0689-5
Sane DC, Mozingo WS, Becker RC (2009) Cardiac rupture after myocardial infarction: new insights from murine models. Cardiol Rev 17:293–299. doi:10.1097/CRD.0b013e3181bf4ab4
Sun Y, Kiani MF, Postlethwaite AE, Weber KT (2002) Infarct scar as living tissue. Basic Res Cardiol 97:343–347. doi:10.1007/s00395-002-0365-8
Tian H, Cimini M, Fedak PW, Altamentova S, Fazel S, Huang ML, Weisel RD, Li RK (2007) TIMP-3 deficiency accelerates cardiac remodeling after myocardial infarction. J Mol Cell Cardiol 43:733–743. doi:10.1016/j.yjmcc.2007.09.003
Tiede K, Melchior-Becker A, Fischer JW (2010) Transcriptional and posttranscriptional regulators of biglycan in cardiac fibroblasts. Basic Res Cardiol 105:99–108. doi:10.1007/s00395-009-0049-8
Van Linthout S, Seeland U, Riad A, Eckhardt O, Hohl M, Dhayat N, Richter U, Fischer JW, Bohm M, Pauschinger M, Schultheiss HP, Tschope C (2008) Reduced MMP-2 activity contributes to cardiac fibrosis in experimental diabetic cardiomyopathy. Basic Res Cardiol 103:319–327. doi:10.1007/s00395-008-0715-2
Wang B, Omar A, Angelovska T, Drobic V, Rattan SG, Jones SC, Dixon IM (2007) Regulation of collagen synthesis by inhibitory Smad7 in cardiac myofibroblasts. Am J Physiol Heart Circ Physiol 293:H1282–H1290. doi:10.1152/ajpheart.00910.2006
Woessner JF Jr (1961) The determination of hydroxyproline in tissue and protein samples containing small proportions of this imino acid. Arch Biochem Biophys 93:440–447. doi:10.1016/0003-9861(61)90291-0
Yang TT, Hawkes SP (1992) Role of the 21-kDa protein TIMP-3 in oncogenic transformation of cultured chicken embryo fibroblasts. Proc Natl Acad Sci USA 89:10676–10680. doi:10.1073/pnas.89.22.10676
Zarzynska J, Gajewska M, Motyl T (2005) Effects of hormones and growth factors on TGF-beta1 expression in bovine mammary epithelial cells. J Dairy Res 72:39–48. doi:10.1017/S0022029904000639
Zhong H, Simons JW (1999) Direct comparison of GAPDH, beta-actin, cyclophilin, and 28S rRNA as internal standards for quantifying RNA levels under hypoxia. Biochem Biophys Res Commun 259:523–526. doi:10.1006/bbrc.1999.0815
Acknowledgments
This study was supported by operating grants from Canadian Institutes of Health Research (CIHR) awarded to Dr. Qingping Feng. Lamis Hammoud was supported by a Heart and Stroke Foundation of Canada Doctoral Research Award. Dr. Feng is a Heart and Stroke Foundation of Ontario Career Investigator.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
L. Hammoud and X. Lu both contributed equally to this work.
Rights and permissions
About this article
Cite this article
Hammoud, L., Lu, X., Lei, M. et al. Deficiency in TIMP-3 increases cardiac rupture and mortality post-myocardial infarction via EGFR signaling: beneficial effects of cetuximab. Basic Res Cardiol 106, 459–471 (2011). https://doi.org/10.1007/s00395-010-0147-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00395-010-0147-7