Abstract
The extracellular heterodimeric protein S100A8/A9 activates the innate immune system through activation of the receptor of advanced glycation end products (RAGE) and Toll-like receptors. As activation of RAGE has recently been associated with sustained myocardial inflammation and heart failure (HF) we studied the role of S100A8/A9 in the development of post-ischemic HF. Hypoxia led to sustained induction of S100A8/A9 accompanied by increased nuclear factor (NF-)κB binding activity and increased expression of pro-inflammatory cytokines in cardiac fibroblasts and macrophages. Knockdown of either S100A8/A9 or RAGE rescued the induction of pro-inflammatory cytokines and NF-κB activation after hypoxia. In a murine model of post-ischemic HF both cardiac RNA and protein levels of S100A8/A9 were elevated as soon as 30 min after hypoxia with sustained activation up to 28 days after ischemic injury. Treatment with recombinant S100A8/A9 resulted in reduced cardiac performance following ischemia/reperfusion. Chimera experiments after bone marrow transplantation demonstrated the importance of RAGE expression on immune cells for their recruitment to the injured myocardium aggravating post-ischemic heart failure. Signaling studies in isolated ventricles indicated that MAP kinases JNK, ERK1/2 as well as NF-κB mediate signals downstream of S100A8/A9-RAGE in post-ischemic heart failure. Interestingly, cardiac performance was not affected by administration of S100A8/A9 in RAGE−/−-mice, which demonstrated significantly improved cardiac recovery compared to WT-mice. Our study provides evidence that sustained activation of S100A8/A9 critically contributes to the development of post-ischemic HF driving the progressive course of HF through activation of RAGE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemic heart disease is the leading cause of heart failure (HF) in industrialized countries [18, 19]. Despite aggressive primary therapy after myocardial infarction (MI), prognosis remains poor in patients with severe left ventricular dysfunction. Next to infarction size, which is a critical determinant of heart failure, there are many other factors such as cardiac hypertrophy, fibrosis and expression of various cytokines which are associated with disease progression [42, 62].
There is a growing experimental evidence and recognition that inflammation plays an important role in cardiac repair following infarction [40, 56, 63]. Moreover, inflammation may persist beyond the initial repair phase and later also extend into the non-infarcted remote myocardium, contributing to long-term adverse remodeling subsequently leading to disease progression of chronic heart failure [27]. However, the underlying molecular mechanisms of sustained myocardial inflammation are only poorly understood so far.
S100A8 [also referred to as myeloid related protein (MRP)8] and S100A9 (also referred to as MRP 14) are members of the S100 family of calcium-modulated proteins that are highly abundant in myeloid cells. In these cells, the expression of the S100A8 and S100A9 is known to be upregulated and they are secreted in inflammatory conditions leading to an activation of signaling pathways via the receptor for advanced glycation endproducts (RAGE) and Toll-like receptor-4 (TLR-4) to induce chemotaxis of neutrophils and amplify the pro-inflammatory cascade [3, 25, 29, 31, 32, 60]. High levels of serum S100A8/A9 in chronic inflammatory conditions such as rheumatoid arthritis[16], inflammatory bowel disease[39] and chronic bronchitis as well as in acute MI[34] and vascular injury [12, 55] suggest that they might also play a role in post-ischemic remodeling, which is, at least to some extent, dependent on inflammation of the myocardium.
In the present study, we demonstrate that non-cardiomyocytes in the infarcted area such as infiltrating inflammatory cells in the acute stage as well as granulation tissue cells during the sub-acute stage of MI are essential in sustaining the pro-inflammatory cellular response through increased expression of S100A8/A9 driving adverse left ventricular remodeling.
Methods
Murine model of ischemia/reperfusion (I/R) injury and application of recombinant S100A8/A9 protein
C57BL/6 wild-type (WT) mice (10–12 weeks old, purchased from Charles River) and RAGE−/− mice in a C57BL/6 background [3, 4, 11, 37] were anesthetized with isoflurane (2–3% v/v and buprenorphine 0.1 mg/kg SC tid for 1 day) and subjected to I/R according to the protocols approved by the Animal Care and Use Committee of the University of Heidelberg. The coronary artery occlusion for 30 min and reperfusion procedure was performed as described previously [21, 61].
Human recombinant S100A8 and S100A9 proteins were obtained from BMA Biomedicals (Switzerland). The heterodimerization to obtain a S100A8/S100A9 complex and endotoxin removal was performed as previously described [14]. 400 μg/kg body weight of the recombinant S100A8/A9 complex was administered intraperitoneally 1 h before induction of I/R injury and once daily for the following 2 days [57].
Bone-marrow transplantation
Donor mice were age-matched to 6 weeks old recipient mice. Briefly, recipient mice were ablated with lethal irradiation (10 Gy) in one dose. One day later, ablated mice were transplanted with 5 × 106 donor bone marrow (BM) cells in 150 μl phosphate-buffered saline (PBS) by tail vein injection. BM cells were obtained by flushing femurs of donor mice with PBS. A 40 μm strainer was used to remove cell aggregates and single cells were washed twice in RPMI-1640 medium before injection. The transplanted BM was allowed to regenerate for 4 weeks before I/R injury. BM-transplanted mice had free access to Ciprofloxacin-supplemented (100 mg/l) water for 4 weeks after BMT to prevent bacterial infections.
Echocardiography
Transthoracic echocardiography was performed as previously described in detail [23]. Echocardiography was performed on conscious mice with a 15 MHz linear transducer. For chimeric animals, data recording was done using a Hdi5000cv ultrasonograph, for all other recordings, a Sonos 5500 machine was used (both Philips, Netherlands).
Immunohistochemistry (IHC) and histological evaluation
Hematoxylin and eosin (H&E) and Masson’s trichrome staining were performed using standard protocols. The following primary antibodies were used: goat polyclonal anti-mouse Calgranulin A, 1/100 (Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA), 1/100; goat polyclonal anti-mouse Calgranulin B, 1/100 (Santa Cruz Biotechnology Inc.); goat polyclonal anti-CD68, 1/10 (clone: T-16, Santa Cruz Inc.); Cy3-conjugated monoclonal anti-alpha smooth muscle actin (ASMA), 1/200 (clone: 1A4, DakoCytomation, Glostrup, DK), rabbit polyclonal anti-myeloperoxidase (MPO), 1/10,000 (DakoCytomation). Isotype- and concentration-matched control antibodies (Dako, Hamburg, Germany) served as negative controls. Immunoenzyme staining was performed on 2-μm sections of formalin-fixed, paraffin-embedded murine hearts. Heat-induced antigen-retrieval was achieved by incubating the slides in a pressure cooker for 5 min in citrate buffer, pH 6.1 (Calgranulin A and B, CD68, ASMA, MPO). Slides were further processed using the standard avidin–biotin-complex anti-alkaline phosphatase procedure (Vectorlabs, Burlingame, CA, USA) according to the manufacturer’s instructions. The primary Ab was added overnight at 4°C. A donkey anti-goat or donkey anti-rabbit biotinylated Ab, 1/100 (Dako), was used as a secondary reagent (30 min at room temperature). Naphthol AS-biphosphate (Sigma, St. Louis, MO, USA) with New-fuchsin (Merck, Darmstadt, Germany) served as the substrate for alkaline phosphatase. Evidence of inflammation and fibrosis was evaluated in a blinded manner by an investigator who used light microscopy according to a 6-tier scoring system as described previously in detail: grade 0, no inflammation; grade 1, cardiac infiltration in up to 5% of cardiac sections; grade 2: 6–10%; grade 3: 11–30%; grade 4: 31–50%; and grade 5: >50%.
Double immunofluorescence staining was performed using a combination of Calgranulin A or Calgranulin B and Cy3-conjugated ASMA antibodies. Incubations were performed overnight at 4°C. Cy2-conjugated donkey anti-goat antibody, 1/250 (green fluorescence; Dianova) was used as secondary reagents (30 min at room temperature). Slides were viewed with a laser scanner microscope (Leica Microsystems, Mannheim, Germany). Positive cells were counted and are given as cells per square millimeter. Values represent mean values ± SD from six mice of each group.
Cell culture, induction of hypoxia and siRNA transfection
Cardiac fibroblasts were prepared as published in detail [61]. Isolation of macrophages was performed by their ability to adhere to culture plates [4]. Isolated macrophages and fibroblasts were stimulated with 1 μmol/L S100A8/A9 (24 μg/ml heterodimeric S100A8/A9) protein [14]. Hypoxia experiments were performed in an O2/CO2 controlled incubator (NUNC, Wiesbaden, Germany) adjusted to 1.5% O2 and 5% CO2 at 37°C. siRNA for S100A8 and S100A9 was purchased from Qiagen (SI03648995 and SI04317012). Knockdown efficiency was confirmed using quantitative PCR and AllStars negative siRNA (Qiagen) served as negative control (data not shown). Using HiPerfect (Qiagen) the siRNAs were transfected at a final concentration of 10 nM.
Electrophoretic mobility shift assay (EMSA)
Nuclear proteins were harvested, and 10 μg of nuclear proteins was assayed for NF-κB binding activity using radioactive-labeled oligonucleotides for the defined NF-κB consensus sequence (5′-AGT TGA GGG GAC TTT CCC AGG C-3′) at 50,000 cpm (Cerénkov). Binding reaction and separation of the protein–DNA complexes from unbound DNA by electrophoresis were performed as previously described in detail [4]. Nuclear proteins after 48 h of S100A8/A9 treatment and a 200-fold molar excess of unlabeled consensus sequence were used as the specific competitor in the control lane.
Western blot
Total protein extracts from mouse heart tissue or from cells were prepared as previously described [3]. The antibodies and the dilutions were as follows: p-SAP/JNK #9255 (1:2,000); SAP/JNK #9252 (1:1,000); p-ERK ½ #9101 (1:1,000); ERK ½ #4695 (1:1,000); phos-p38 #9211(1:1,000); p38 #9212 (1:1,000; all from Cell Signaling Technology) and S100A8/9 (1:30; ab17050, Abcam). The antibody for the detection of S100A8/A9 recognizes an epitope on the S100A8/A9 complex which is not exposed on the individual subunits. Horseradish peroxidase-coupled rabbit or mouse IgGs (1:2,000) were used as secondary antibodies.
Enzyme-linked immunosorbent assay for S100A8/A9
Cell culture supernatant was used to analyze the S100A8/A9 secretion of fibroblasts and macrophages. The assay was purchased from Immundiagnostik (Bensheim) and performed according to the manufacturer’s instructions.
Real-time RT-PCR
Total RNA was extracted from each heart into Trizol (Invitrogen). To determine the mRNA-expression levels 1 μg total RNA was used to perform reverse transcription and quantitative real-time PCR using LightCycler (Roche) as described previously [3, 61]. The primer sequences were as follows: IL-6 forward 5′-GATGCTACCAAACTGGATATAATC-3′ and IL-6 reverse 5′-GGTCCTTAGCCACTCCTTCTGTG-3′; TNF-α forward 5′-CCATTCCTGAGTTCTGCAAAG-3′ and reverse 5′-GCAAATATAAATAGAGGGGGGC-3′; β-ACTIN forward 5′-CCCTAAGGCCAACCGTGAAA-3′, and reverse 5′-ACGACCAAGGCATACAGGGA-3′; ANP forward 5′-TGGCCCTCGGAGCCTACGAA-3′, and reverse 5′-ATGAAGGCAGGAAGCCGCAGC-3′; TGFβ forward 5′-GCACTGCGCTGTCTCGCAAG-3′, and reverse 5′- ACGCCGGGTAGCGATCGAGTG-3′; S100A8/A9 forward 5′-AATGGTGGAAGCACAGTTGG-3′, and reverse 5′-GCTCAGCTGATTGTCCTGGT-3′.
Measurement of lactate dehydrogenase
A spectrophotometric kit (Sigma-Aldrich) was used for the assessment of lactate dehydrogenase (LDH) in supernatant of cells, which were exposed to hypoxia.
Statistical analysis
Data are expressed as mean ± SD. Data were analyzed using ANOVA followed by pair wise testing using Tukey’s HSD test. Values of P < 0.05 were considered significant. All calculations with exception of the survival analysis were carried out with the statistical software SPSS version 17.0. Survival analysis was done using R version 2.14.0.
Results
S100A8/A9 expression in macrophages and fibroblasts in vitro
Cells of the immune system such as macrophages as well as fibroblasts are crucial players in the initiation and propagation of the pro-inflammatory response following MI [13, 20, 30, 45]. Since hypoxia initiates ischemic injury we investigated the effect of hypoxia (1.5%O2) on the release of S100A8 and S100A9 in isolated macrophages and cardiac fibroblasts. Macrophages showed a rapid, time-dependent increase in both S100A8/A9 expression (mRNA-expression and S100A8/A9-immunoblotting in whole cell extracts; Fig. 1a, b, d) and release (S100A8/A9 measured in supernatant; Fig. 1c) that peaked after 24 h of hypoxia on the RNA level (Fig. 1a, b) and after 48 h of hypoxia on the protein level (Fig. 1d). A similar time-dependent expression pattern of S100A8 and S100A9 could be demonstrated in isolated cardiac fibroblasts with a peak after 48 h of hypoxia on the RNA and protein level (Fig. 1f–i). LDH measured as tissue injury parameter in the supernatant of hypoxic macrophages was significantly increased (P < 0.001) after 24 h of hypoxia and after 48 h in cardiac fibroblasts (P < 0.001) indicating an additional passive release of S100A8/A9 from necrotic cells at later time points in vitro (Supplementary Figure 1a, b). Macrophages and cardiac fibroblasts exposed to normoxia (21%O2) demonstrated a basal level of S100A8/A9 expression that did not vary significantly after 48 h of incubation (data not shown).
S100A8/A9 expression in macrophages and cardiac fibroblasts in hypoxia. Isolated macrophages (a–e, k) and cardiac fibroblasts (f–k) were exposed to hypoxia (1.5% O2) for the duration indicated. RT-PCR (a, b, f, g), ELISA of the corresponding supernatants (c, h) and Western Blot analyses (d, i) of S100A8/A9 expression were analyzed at given intervals. The corresponding densitometric analyses are shown as bar graphs (d, i). Activation of NF-κB binding activity was determined in macrophages (e) and fibroblasts (j) following co-incubation with rS100A8/A9 (10 μmol/l) at given time points. Isolated macrophages and fibroblasts from WT and RAGE−/− mice were exposed to hypoxia (1.5% O2) at given time points and activation of NF-κB binding activity was assayed (k). siRNA knockdown of S100A8/A9 was performed in macrophages and fibroblasts as indicated (k). EMSA gels and the corresponding densitometric analyses are shown (e, j, k). (a–c, f–h *P < 0.001, **P < 0.0001; d, j *P < 0.001; e, j *P < 0.001, **P < 0.0001, n = 5–10 per group)
To characterize the direct effects of the interaction of S100A8/A9 with RAGE, we performed co-incubation studies with rS100A8/A9 in isolated macrophages (Fig. 1e) and cardiac fibroblasts (Fig. 1j). Stimulation of both macrophages and fibroblasts with rS100A8/A9 resulted in a time-dependent activation of NF-κB binding activity with a peak after 48 h (Fig. 1e, j). Furthermore, knockdown of S100A8/A9 with siRNA and knockout of RAGE in cells isolated from RAGE−/− mice both led to a reduced activation of NF-κB in hypoxic macrophages and fibroblasts (Fig. 1k).
Expression of S100A8/A9 in post-ischemic heart
To test whether the S100A8/A9-RAGE axis is involved in post-infarction remodeling ischemia was induced by ligation of the left anterior descending (LAD) followed by either 7 or 28 days of reperfusion in WT and RAGE−/− mice (Fig. 2a–l). Sham-operated hearts demonstrated transverse striation and only scarce staining for S100A8 (Fig. 2a, g) and S100A9 (Fig. 2d, j). Cardiac sections of WT mice after 7 days of reperfusion presented with signs of infarction such as necrosis, loss of nuclei and loss of transverse striation (Fig. 2b, e) as well as mixed inflammatory cellular infiltrate consisting primarily of macrophages (Fig. 2n, u), a small number of neutrophils (Fig. 2m, u) and myofibroblasts (Fig. 2q, r, w) which revealed a strong expression of S100A8 and S100A9 in WT animals. Cardiac sections of WT hearts after 28 days revealed sustained positive staining for S100A8 and S100A9 of myofibroblasts (Fig. 2c, f, s, t, x) as well as a reduced amount of mixed S100A8 and S100A9 positive inflammatory infiltrate (Fig. 2o, p, v) compared to 7 days of reperfusion. In contrast, immunohistochemistry analysis confirmed a reduced number of infiltrating immune cells expressing S100A8 and S100A9 in RAGE−/− hearts 7 (Fig. 2h, k) and 28 days after infarction (Fig. 2i, l) suggesting S100A8/A9-RAGE-dependent activation of an inflammatory microenvironment in post-MI hearts.
S100A8/A9 expression in WT (b, c, e, f) and RAGE−/− (h, i, k, l) reperfused myocardium versus the corresponding sham-treated controls (a, d, g, j) after 7 or 28 days of I/R injury (H&E staining). The reperfused myocardium displays sustained increase of S100A8 and S100A9 expression. For further characterization of the recruited innate cells within the reperfused myocardium of WT mice, staining for granulocytes (anti-MPO and H&E staining) and macrophages (anti-cd68 and H&E staining) 7 days (m, n) and 28 days (o, p) following MI was performed. Quantitative analysis is shown as cells per square millimeter (u, v). Representative images of reperfused myocardium from at least six WT mice that were subjected to double immunofluorescence staining using a combination of S100A8 (anti-S100A8, green) or S100A9 (anti-S100A9, green) and Cy3-conjugated ASMA (anti-ASMA, red) 7 days (q, r) and 28 days (s, t) following MI. Nuclear staining was done with DAPI (blue). Corresponding cell counts of either S100A8 or S100A and ASMA double positive cells are shown (w, x). Original magnification ×40, bar 20 μm
Next, we performed expression analysis of S100A8 and S100A9 in isolated ventricles at given time points using real-time PCR. Compared with sham-treated animals I/R injury resulted in rapidly increased expression of S100A8 and S100A9 peaking at 6 h after reperfusion (P < 0.0001, Fig. 3a, b). It is remarkable that expression of both S100A8 and S100A9 remained significantly up-regulated even 28 days following MI on RNA (P < 0.0001, Fig. 3a, b) and protein level (Fig. 3c).
S100A8/A9 and RAGE in post-MI remodeling
To strengthen the concept of S100A8/A9-RAGE-dependent perpetuation of inflammation, we tested the influence of RAGE deficiency on post-ischemic remodeling. After 28 days post MI the heart sections of WT animals showed increased cellularity and widened extracellular space when compared with sham-operated mice (Fig. 4a, b, g). Additional treatment of WT animals with rS100A8/A9 led to a significantly enhanced influx of inflammatory cells into the infarcted area (Fig. 4c) translating into an increased inflammation score (Fig. 4g). When inflammatory cells were classified as either CD68- or MPO-positive cells, treatment with S100A8/A9 leads to an increase of both, CD68- and MPO-positive cells 28 days post MI (Supplementary Figure 2a and b). In addition, treatment with rS100A8/A9 also leads to a sustained activation of key mediators of cardiac I/R injury, TNF-α [35] and IL-6 [22, 36] (Fig. 4h, i) in the reperfused left ventricles. However, RAGE−/− mice displayed only slight inflammation (Fig. 4e) that was not noticeably influenced by rS100A8/A9 (Fig. 4f) treatment with a significantly reduced inflammation score (Fig. 4g) compared to WT animals. Quantification of CD68- and MPO-positive cells in the myocardium of RAGE−/− mice did not reveal any difference in numbers between groups with and without S100A8/A9 treatment (Supplementary Figure 2a and b). In this context, RAGE-deficient hearts displayed only marginal activation of TNF-α and IL-6 (Fig. 4h, i) after 28 days following myocardial infarction.
H&E staining with original magnification ×32 (a–f). WT (a–c) and RAGE−/− mice (d–f) were subjected to I/R injury and analyzed after 4 weeks. Groups c and f were treated with rS100A8/A9. Images are representative heart sections from 5 to 10 mice per group. Effects on severity of cardiac inflammation are shown as an histoscore of inflammation (g, *P < 0.01, **P < 0.0001). Cardiac TNF-α (h, *P < 0.001) and IL-6 (i, *P < 0.001, **P < 0.0001) mRNA levels are shown. Results are expressed as relative increase of mRNA levels versus sham-operated WT animals
Sham heart sections stained for collagen showed predominantly perivascular, thin perimysial and endomysial strands (Fig. 5a, d). In contrast, mice subjected to ischemia displayed interstitial collagen deposition in the infarcted area (Fig. 5b). In this context, rS100A8/A9 treatment further promoted adverse myocardial remodeling leading to extensive replacement fibrosis (Fig. 5c, g) and enhanced myocardial expression of TGF-β (Fig. 5h), an essential mediator of remodeling [47]. Furthermore, treatment with S100A8/A9 leads to an increase in ASMA-positive myofibroblasts in the myocardium 28 days after MI (Supplementary Figure 3). In contrast, fibrosis was moderate in RAGE-deficient hearts (Fig. 5e–g) along with significantly attenuated myocardial expression of TGF-β in RAGE−/− mice (Fig. 5h) and no detectable increase in ASMA-positive cells after treatment with S100A8/A9 (Supplementary Figure 3).
Masson’s trichrome staining with original magnification ×32 (a–f). WT (a–c) and RAGE−/− mice (d–f) were subjected to I/R injury and analyzed after 4 weeks. Groups c and f were treated with rS100A8/A9. Effects on the severity of cardiac remodeling are shown in a histoscore for fibrosis (g, *P < 0.01, **P < 0.001). Cardiac TGF-β1 (h, *P < 0.001, **P < 0.0001) mRNA levels are shown. Results are expressed as relative increase of mRNA levels versus sham-operated WT animals
Impact of the S100A8/A9-RAGE axis on cardiac function
Fractional shortening in mice treated with rS100A8/A9 was significantly reduced (P < 0.001, Fig. 6a) whereas heart weight/body weight (HW/BW) ratios were increased after 7 and 28 days (p < 0.001, Fig. 6b). At the same time rS100A8/A9 treatment also significantly increased the gene expression of atrial natriuretic peptide (ANP, p < 0.001, Fig. 6c) in ischemic hearts compared to untreated WT mice. Interestingly, RAGE−/− mice were largely protected form ischemic remodeling demonstrated by a nearly preserved systolic contractile function (Fig. 6a), only moderate signs of post-ischemic hypertrophy (Fig. 6b) and reduced left ventricular dilation (Supplementary Figure 4) compared to WT mice. In addition, RAGE-deficient hearts showed only moderate expression of ANP indicating attenuated cardiac remodeling, which was not influenced by rS100A8/A9 therapy (Fig. 6c), and reduced infarct size in relation to the area at risk (Fig. 6d, p < 0.001). However, we did not observe any significant differences in mortality within 28 days of observation post I/R between WT mice, WT mice that were treated with S100A8/A9, RAGE−/− mice and RAGE−/− mice that were treated with S100A8/A9 (Supplementary Figure 5).
WT and RAGE−/− mice were subjected to I/R injury. Echocardiographic assessment of the left ventricular function demonstrated as fractional shortening (FS) (a *P < 0.01, **P < 0.001 vs. WT-sham), heart weight/body weight ratio (HW/BW) (b, *P < 0.001, **P < 0.0001 vs. WT-sham), atrial natriuretic peptide (ANP) (c, *P < 0.001, **P < 0.0001 vs. WT-sham), and the ratio of infarct size and area at risk (inf/AAR) (d, *P < 0.01, **P < 0.001 vs. WT) were determined in each group at given time points
RAGE expression in immune cells is required for post-ischemic remodeling
To investigate whether RAGE expression on either myocardial cells such as endothelial cells and cardiomyocytes or immune cells is required for S100A8/A9-mediated post-ischemic remodeling, we analyzed mouse chimera after BMT. As expected, WT mice reconstituted with WT-bone marrow cells (WT → WT) and RAGE-deficient mice reconstituted with RAGE−/− bone marrow cells (RAGE−/− → RAGE−/−) phenocopied the response of WT and RAGE−/− mice to reperfusion injury (Fig. 7a, b, e, f). RAGE−/− mice reconstituted with WT-bone marrow cells (WT → RAGE−/−) showed no significant difference in infiltration by neutrophils and macrophages compared with WT → WT chimera (Fig. 7b). However, WT mice reconstituted with RAGE−/− bone marrow cells (RAGE−/− → WT) revealed reduced infiltration by neutrophils and macrophages compared with WT → RAGE−/− chimera or WT → WT mice (Fig. 7b). In summary, we provide experimental evidence that RAGE expression on immune cells, but not on myocardial cells endothelial cells, cardiomyocytes or myofibroblasts is required for innate immune cell recruitment and induction of post-ischemic remodeling which is in line with published data [4, 48]. Noteworthy, IHC analyses of the heart sections revealed reduced S100A8/A9 protein levels for WT → RAGE−/− compared with WT → WT chimera (Fig. 7a, c, d) within the first 7 days after MI demonstrating that RAGE signaling is required for efficient S100A8/A9 expression in the myocardium. Furthermore, despite initial comparable inflammation indexes of WT → RAGE and WT → WT hearts, WT → RAGE mice also demonstrated reduced amount of S100A8/A9 positive cells next to significantly attenuated fibrosis compared to WT → WT animals (Fig. 7e–h). This further corroborates the important role of S100A8/A9 in cardiac post-ischemic remodeling and particularly indicates an involvement of RAGE expressed on non-immune cells in fibrosis. Echocardigraphic analyses of these four groups showed preserved cardiac function in RAGE−/− → RAGE−/− and RAGE−/− → WT mice whereas WT → RAGE−/− and WT → WT heart function was considerably impaired (Fig. 7i).
RAGE expression in immune cells is required for myocardial infiltration and remodeling. a Representative images are shown of H&E stained myocardial sections (upper row) derived from ablated WT mice reconstituted with bone marrow cells from WT mice (WT → WT) or RAGE−/− mice (RAGE−/− → WT), or ablated RAGE−/− mice reconstituted with bone marrow cells from WT mice (WT → RAGE−/−) or RAGE−/− mice (RAGE−/− → RAGE−/−) which were subjected to MI and 28 days of reperfusion. b The corresponding histoscores were analyzed in all four groups at given time points. (b, *P < 0.001; c–e, *P < 0.001, **P < 0.0001). e Representative images are shown of Masson’s trichrome stained myocardial sections (upper row) derived from ablated WT mice reconstituted with bone marrow cells from WT mice (WT → WT) or RAGE−/− mice (RAGE−/− → WT), or ablated RAGE−/− mice reconstituted with bone marrow cells from WT mice (WT → RAGE−/−) or RAGE−/− mice (RAGE−/− → RAGE−/−) which were subjected to MI and 28 days of reperfusion. The corresponding fibrosis scores in each group are shown (f) at given time points. S100A8 and S100A9 protein expression by IHC (red staining bottom two rows) were analyzed and counted as positive cells per square millimeter (g–h). (f–h *P < 0.001, **P < 0.0001). Original magnification ×20 (a, e, upper row, bar = 50 μm), original magnification ×40 (a, e, bottom two rows, bar = 20 μm)
In summary, our data provide direct evidence that RAGE drives post-ischemic cardiac remodeling upon ligation with its ligands such as S100A8/A9 thus maintaining a pro-inflammatory and pro-fibrotic microenvironment required for post-ischemic remodeling.
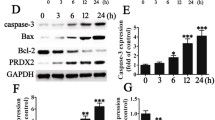
S100A8/A9 modulates inflammatory signaling pathways in post-ischemic remodeling
The mitogen-activated protein (MAP) kinase family has been ascribed a crucial function in the development of post-ischemic heart failure [7, 43, 47]. To study whether S100A8/A9-RAGE influences MAP kinase activation, we analyzed extracellular signal-related kinase (ERK1/2), c-Jun NH2 terminal kinase (JNK) and p38 activation in explanted hearts 4 weeks following the induction of I/R injury. Post-ischemic remodeling was associated with sustained phosphorylation of all MAP kinases in WT hearts 4 weeks after infarction. Treatment with rS100A8/A9 even further enhanced the activation of all MAP kinases. In line with protection from post-MI-induced heart failure shown above, post-ischemic left ventricles from RAGE−/− mice displayed significantly reduced phosphorylation of ERK1/2, JNK and p38 compared to control group (Fig. 8a–d).
MAP-kinase activation was determined in WT and RAGE−/− mice (a–d). WB analyses of phosphorylated (p) and total (t) ERK1/2, JNK and p38 were performed. Each blot shown is representative of three experiments with similar results. b–d Summarize the densitometric analyses of all extracts tested. (b–d *P < 0.001, **P < 0.0001)
Discussion
There is a increasing recognition that inflammation is associated with post-infarction maladaptive left ventricular remodeling including alterations in left ventricular mass, geometry and function driving disease progression in chronic heart failure [10]. Although the clinical features of ischemic heart failure are well described, its underlying pathophysiologic mechanisms, especially the contribution of myocardial inflammation, have not been fully elucidated.
Recent clinical studies have associated elevated serum levels of S100A8/A9 with inflammatory disorders such as rheumatoid arthritis [17], transplant rejection [33], human prostate cancer [26] and acute coronary syndrome [2, 24]. Moreover, increased S100A8/A9 expression has been demonstrated in atherosclerotic plaques in coronary and carotid arteries [2, 41]. However, the underlying molecular mechanisms and the mechanistic implication of S100A8/A9 in the pathophysiology of post-ischemic heart failure have not been characterized so far.
Based on our recent work implicating S100A8/A9 as a crucial mediator of sustained intestinal inflammation [3] and based on the fact that S100A8/A9 has recently been shown to be up-regulated in the sera of acute MI patients [34], we hypothesized that these S100 proteins might be involved in the process of adverse remodeling.
In the present study, we first report that interaction of S100A8/A9 with its receptor RAGE is crucial to the progression of heart failure in both, the early and the late phase of post-MI remodeling. The heterodimeric complex S100A8/A9 is a well-known extracellular factor that engages with RAGE to induce intracellular signaling [3, 29] and has recently emerged as an important mediator in acute and chronic inflammation [28, 60]. One of the unique features of RAGE engagement is the sustained activation of NF-κB overwhelming auto-regulatory feedback inhibitory loops [6]. RAGE-dependent sustained NF-κB activation therefore has been implicated in a number of chronic inflammatory diseases [5, 52, 64]. Because RAGE expression is upregulated by NF-κB and ligation of RAGE results in sustained NF-κB activation, endogenous S100A8/A9 might activate this positive feedback-loop via binding to RAGE resulting in sustained inflammation. To strengthen the concept of RAGE-dependent perpetuation of inflammation, we analyzed the effect of RAGE deficiency on post-infarction remodeling. S100A8/A9 protein levels were largely reduced in RAGE−/− myocardium in early and late stages of myocardial post-MI remodeling. Furthermore, IHC analysis confirmed differential expression on protein levels implying that S100A8/A9 acts not only as a RAGE ligand but also represents target genes of RAGE signaling. This is in accordance with recent findings showing that RAGE maintains cellular activation by induction of its own extracellular ligands [3, 4, 52].
Important pro-inflammatory features of the heterodimeric complex S100A8/A9 have been described by Ryckman et al. [51] describing the chemotactic properties of these S100 proteins in vitro which could be partially reversed by a S100A8/A9-specific blockade [57]. In this context, Viemann et al. [58] demonstrated a thrombogenic inflammatory response to S100A8/A9 in human microvascular endothelial cells as a pre-requirement for transmigration of immune cells. However, a direct role of S100A8/A9 in post-MI remodeling and in the pathophysiology of the development of heart failure was heretofore unrecognized. Strong proof of an involvement of the S100 proteins in the biological response to vascular injury stem from Croce et al. [12], who investigated the effects of S100A9 knockdown in an femoral artery endothelial denudation of the femoral artery. This study showed reduced cellular proliferation, neointimal formation and atherosclerosis due to S100A9 knockdown pointing toward a modulatory role of the S100 proteins in vascular inflammation.
In line with our previous findings [3], transcription and protein expression of S100A8 and S100A9 was highly elevated in isolated macrophages and myofibroblasts in hypoxia and in both early and late stages of post-infarction remodeling in vivo. As a proof of concept study, we found that co-incubation of both isolated primary macrophages and cardiac fibroblasts with rS100A8/A9 alone significantly increased NF-κB binding activity next to an elevated inflammatory and fibrotic activity throughout the study period of 4 weeks compared to untreated control group in vivo. The enhanced recruitment of immune cells mediated via S100A8/A9 may be explained by its regulatory role in leukocyte adhesion through the control of the expression and function of leukocyte integrin adhesion molecule Mac-1 (CD11b/CD18, αMβ2) [15, 46, 51].
In our heart failure model, S100A8/A9 appears to control the inflammatory response at several levels, including regulation of macrophage and neutrophils accumulation and regulation of post-ischemic fibrotic activity.
The early and late stages of post-MI remodeling in our model depend variably on neutrophils, macrophages and myofibroblasts. To investigate whether RAGE expression on myocardial cells such as cardiomyocytes and endothelial cells or immune cells is required for post-ischemic remodeling, we analyzed chimeric mice after bone marrow transplantation. Collectively, we provide experimental evidence that RAGE expression on immune cells, but also to a certain extent on non-immune cells such as endothelial cells or cardiomyocytes is required for innate immune cell recruitment and induction of cardiac remodeling in vivo which is in line with previous data [48]. IHC analysis on heart sections revealed reduced S100 protein levels for WT → RAGE−/− compared with WT → WT chimera demonstrating that RAGE signaling is required for efficient S100A8/A9 expression in the myocardium. Post-ischemic S100A8/A9 levels in isolated cardiomyocytes were only marginally upregulated and significantly lower than observed in immune cells and myofibroblasts 4 weeks following MI (data not shown).
We also went on to show for the first time that S100A8/A9 treatment promotes adverse cardiac remodeling involving increased TGF-β1 expression and enhanced expression of the fetal gen program such as ANP compared to the untreated group. These data are supported by previous work from Vogl et al. [59] who described an essential role of S100A9 in the recruitment of neutrophils into granulation tissue in vivo, in pancreatic tissue during acute pancreatitis [53] and into the skin during IL-8-stimulated inflammation [44]. In this context, a crucial modulatory role of S100A8/A9 in fibroblast function has been described by Rahimi et al. [49] who could see a drastically enhanced S100A8 activity by FGF-2/IL-1β stimulation. This could be one explanation for the elevated fibrosis score of heart sections treated with rS100A8/A9 4 weeks following acute ischemic event revealing less recruitment of mononuclear cells into the myocardium in favor of S100A8/A9-positive myofibroblasts. Our finding that RAGE deficiency attenuates adverse remodeling through reduction of inflammatory activity is consistent with previously described S100A8/A9-RAGE-mediated cardiomyocyte dysfunction in a LPS-induced sepsis model which could be partially reversed by both knockdown of S100A9 and RAGE deficiency [8]. However, these findings were related to the involvement of Toll-like receptors (TLR), especially its isoform TLR-4. In this context, elegant mechanistic analyses concerning phagocyte activation in two sepsis models support the importance of the interaction of TLR-4 and S100A8/A9 [60]. Furthermore, previous studies also demonstrated the involvement of TLR2- and TLR4-mediated signaling in cardiac remodeling [50, 54].
In contrast, in this study RAGE−/− mice were significantly protected despite TLR-4 and TLR-9 expression comparable to that of WT mice (data not shown) [4, 61]. These discrepant findings might be explained by the different nature of the stress model, different time points of our read-outs and by the fact that cardiomyocytes were defined as the primary source of S100A8/A9 expression in this LPS-induced sepsis model [8], whereas we focussed on the activation of neutrophils, mononuclear cells and fibroblasts. We have also not looked into the role of CD8+ T-cells which are regulated by S100A8/A9 and play a major role in the development of autoimmunity [38]. However, using RAGE−/− mice and knockdown of S100A8/A9 we determined that post-MI-induced expression of the S100 proteins is absolutely dependent on S100A8/A9–RAGE interaction. Of note, the effect of RAGE-knockdown did not translate into improved survival in our in vivo I/R model after 28 days (Supplementary Figure 5). This may be due to the fact that group size was too small and the observation period of 28 days was not sufficient to detect this effect.
Further confirmation of an involvement of RAGE in I/R injury derived form Aleshin et al. [1] who observed a protective effect using sRAGE, a soluble antagonist of RAGE, in isolated perfused heart studies. However, both the effect of sRAGE treatment on the inflammatory response and the functional mechanism for RAGE signaling during remodeling remained undefined. In this context, Bucciarelli et al. characterized the role of RAGE in ischemic injury in the diabetic myocardium. RAGE-expression was enhanced in type 1 diabetic rat and murine hearts compared to non-diabetic controls whereas RAGE deficiency protected from diabetes-mediated generation of oxidant stress accompanied by improved myocardial energy metabolism [9].
Taken together, our data support the existence of an S100A8/A9-RAGE driven feed-forward loop in post-ischemic cardiac remodeling driving the development of heart failure. These results may translate into novel treatment modalities in which sustained activation of RAGE is blocked by inhibition of its ligands such as S100A8/A9.
References
Aleshin A, Ananthakrishnan R, Li Q, Rosario R, Lu Y, Qu W, Song F, Bakr S, Szabolcs M, D’Agati V, Liu R, Homma S, Schmidt AM, Yan SF, Ramasamy R (2008) RAGE modulates myocardial injury consequent to LAD infarction via impact on JNK and STAT signaling in a murine model. Am J Physiol Heart Circ Physiol 294:H1823–H1832. doi:10.1152/ajpheart.01210.2007
Altwegg LA, Neidhart M, Hersberger M, Muller S, Eberli FR, Corti R, Roffi M, Sutsch G, Gay S, von Eckardstein A, Wischnewsky MB, Luscher TF, Maier W (2007) Myeloid-related protein 8/14 complex is released by monocytes and granulocytes at the site of coronary occlusion: a novel, early, and sensitive marker of acute coronary syndromes. Eur Heart J 28:941–948. doi:10.1093/eurheartj/ehm078
Andrassy M, Igwe J, Autschbach F, Volz C, Remppis A, Neurath MF, Schleicher E, Humpert PM, Wendt T, Liliensiek B, Morcos M, Schiekofer S, Thiele K, Chen J, Kientsch-Engel R, Schmidt AM, Stremmel W, Stern DM, Katus HA, Nawroth PP, Bierhaus A (2006) Posttranslationally modified proteins as mediators of sustained intestinal inflammation. Am J Pathol 169:1223–1237. doi:10.2353/ajpath.2006.050713
Andrassy M, Volz HC, Igwe JC, Funke B, Eichberger SN, Kaya Z, Buss S, Autschbach F, Pleger ST, Lukic IK, Bea F, Hardt SE, Humpert PM, Bianchi ME, Mairbaurl H, Nawroth PP, Remppis A, Katus HA, Bierhaus A (2008) High-mobility group box-1 in ischemia-reperfusion injury of the heart. Circulation 117:3216–3226. doi:10.1161/CIRCULATIONAHA.108.769331
Bierhaus A, Haslbeck KM, Humpert PM, Liliensiek B, Dehmer T, Morcos M, Sayed AA, Andrassy M, Schiekofer S, Schneider JG, Schulz JB, Heuss D, Neundorfer B, Dierl S, Huber J, Tritschler H, Schmidt AM, Schwaninger M, Haering HU, Schleicher E, Kasper M, Stern DM, Arnold B, Nawroth PP (2004) Loss of pain perception in diabetes is dependent on a receptor of the immunoglobulin superfamily. J Clin Invest 114:1741–1751. doi:10.1172/JCI18058
Bierhaus A, Schiekofer S, Schwaninger M, Andrassy M, Humpert PM, Chen J, Hong M, Luther T, Henle T, Kloting I, Morcos M, Hofmann M, Tritschler H, Weigle B, Kasper M, Smith M, Perry G, Schmidt AM, Stern DM, Haring HU, Schleicher E, Nawroth PP (2001) Diabetes-associated sustained activation of the transcription factor nuclear factor-kappaB. Diabetes 50:2792–2808. doi:10.2337/diabetes.50.12.2792
Boengler K, Hilfiker-Kleiner D, Drexler H, Heusch G, Schulz R (2008) The myocardial JAK/STAT pathway: from protection to failure. Pharmacol Ther 120:172–185. doi:10.1016/j.pharmthera.2008.08.002
Boyd JH, Kan B, Roberts H, Wang Y, Walley KR (2008) S100A8 and S100A9 mediate endotoxin-induced cardiomyocyte dysfunction via the receptor for advanced glycation end products. Circ Res 102:1239–1246. doi:10.1161/CIRCRESAHA.107.167544
Bucciarelli LG, Ananthakrishnan R, Hwang YC, Kaneko M, Song F, Sell DR, Strauch C, Monnier VM, Yan SF, Schmidt AM, Ramasamy R (2008) RAGE and modulation of ischemic injury in the diabetic myocardium. Diabetes 57:1941–1951. doi:10.2337/db07-0326
Cohn JN, Ferrari R, Sharpe N (2000) Cardiac remodeling—concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. Behalf of an International Forum on Cardiac Remodeling. J Am Coll Cardiol 35:569–582 S0735109799006300[pii]
Constien R, Forde A, Liliensiek B, Grone HJ, Nawroth P, Hammerling G, Arnold B (2001) Characterization of a novel EGFP reporter mouse to monitor Cre recombination as demonstrated by a Tie2 Cre mouse line. Genesis 30:36–44. doi:10.1002/gene.1030
Croce K, Gao H, Wang Y, Mooroka T, Sakuma M, Shi C, Sukhova GK, Packard RR, Hogg N, Libby P, Simon DI (2009) Myeloid-related protein-8/14 is critical for the biological response to vascular injury. Circulation 120:427–436. doi:10.1161/CIRCULATIONAHA.108.814582
Dayan V, Yannarelli G, Billia F, Filomeno P, Wang XH, Davies JE, Keating A (2011) Mesenchymal stromal cells mediate a switch to alternatively activated monocytes/macrophages after acute myocardial infarction. Basic Res Cardiol 106:1299–1310. doi:10.1007/s00395-011-0221-9
Ehlermann P, Eggers K, Bierhaus A, Most P, Weichenhan D, Greten J, Nawroth PP, Katus HA, Remppis A (2006) Increased proinflammatory endothelial response to S100A8/A9 after preactivation through advanced glycation end products. Cardiovasc Diabetol 5:6. doi:10.1186/1475-2840-5-6
Eue I, Pietz B, Storck J, Klempt M, Sorg C (2000) Transendothelial migration of 27E10+ human monocytes. Int Immunol 12:1593–1604. doi:10.1093/intimm/12.11.1593
Frosch M, Strey A, Vogl T, Wulffraat NM, Kuis W, Sunderkotter C, Harms E, Sorg C, Roth J (2000) Myeloid-related proteins 8 and 14 are specifically secreted during interaction of phagocytes and activated endothelium and are useful markers for monitoring disease activity in pauciarticular-onset juvenile rheumatoid arthritis. Arthr Rheum 43:628–637. doi:10.1002/1529-0131(200003)43:3<628:AID-ANR20>3.0.CO;2-X
Frosch M, Vogl T, Seeliger S, Wulffraat N, Kuis W, Viemann D, Foell D, Sorg C, Sunderkotter C, Roth J (2003) Expression of myeloid-related proteins 8 and 14 in systemic-onset juvenile rheumatoid arthritis. Arthr Rheum 48:2622–2626. doi:10.1002/art.11177
Fuster V, Badimon L, Badimon JJ, Chesebro JH (1992) The pathogenesis of coronary artery disease and the acute coronary syndromes (1). N Engl J Med 326:242–250. doi:10.1056/NEJM199201233260406
Fuster V, Badimon L, Badimon JJ, Chesebro JH (1992) The pathogenesis of coronary artery disease and the acute coronary syndromes (2). N Engl J Med 326:310–318. doi:10.1056/NEJM199201303260506
Gharaee-Kermani M, Denholm EM, Phan SH (1996) Costimulation of fibroblast collagen and transforming growth factor beta1 gene expression by monocyte chemoattractant protein-1 via specific receptors. J Biol Chem 271:17779–17784. doi:10.1074/jbc.271.30.17779
Goser S, Andrassy M, Buss SJ, Leuschner F, Volz CH, Ottl R, Zittrich S, Blaudeck N, Hardt SE, Pfitzer G, Rose NR, Katus HA, Kaya Z (2006) Cardiac troponin I but not cardiac troponin T induces severe autoimmune inflammation in the myocardium. Circulation 114:1693–1702. doi:10.1161/CIRCULATIONAHA.106.635664
Gwechenberger M, Mendoza LH, Youker KA, Frangogiannis NG, Smith CW, Michael LH, Entman ML (1999) Cardiac myocytes produce interleukin-6 in culture and in viable border zone of reperfused infarctions. Circulation 99:546–551. doi:10.1161/01.CIR.99.4.546
Hardt SE, Geng YJ, Montagne O, Asai K, Hong C, Yang GP, Bishop SP, Kim SJ, Vatner DE, Seidman CE, Seidman JG, Homcy CJ, Vatner SF (2002) Accelerated cardiomyopathy in mice with overexpression of cardiac G(s)alpha and a missense mutation in the alpha-myosin heavy chain. Circulation 105:614–620. doi:10.1161/hc0502.103012
Healy AM, Pickard MD, Pradhan AD, Wang Y, Chen Z, Croce K, Sakuma M, Shi C, Zago AC, Garasic J, Damokosh AI, Dowie TL, Poisson L, Lillie J, Libby P, Ridker PM, Simon DI (2006) Platelet expression profiling and clinical validation of myeloid-related protein-14 as a novel determinant of cardiovascular events. Circulation 113:2278–2284. doi:10.1161/CIRCULATIONAHA.105.607333
Hermani A, De Servi B, Medunjanin S, Tessier PA, Mayer D (2006) S100A8 and S100A9 activate MAP kinase and NF-kappaB signaling pathways and trigger translocation of RAGE in human prostate cancer cells. Exp Cell Res 312:184–197. doi:10.1016/j.yexcr.2005.10.013
Hermani A, Hess J, De Servi B, Medunjanin S, Grobholz R, Trojan L, Angel P, Mayer D (2005) Calcium-binding proteins S100A8 and S100A9 as novel diagnostic markers in human prostate cancer. Clin Cancer Res 11:5146–5152. doi:10.1158/1078-0432.CCR-05-0352
Heymans S, Hirsch E, Anker SD, Aukrust P, Balligand JL, Cohen-Tervaert JW, Drexler H, Filippatos G, Felix SB, Gullestad L, Hilfiker-Kleiner D, Janssens S, Latini R, Neubauer G, Paulus WJ, Pieske B, Ponikowski P, Schroen B, Schultheiss HP, Tschope C, Van Bilsen M, Zannad F, McMurray J, Shah AM (2009) Inflammation as a therapeutic target in heart failure? A scientific statement from the Translational Research Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 11:119–129. doi:10.1093/eurjhf/hfn043
Hiratsuka S, Watanabe A, Aburatani H, Maru Y (2006) Tumour-mediated upregulation of chemoattractants and recruitment of myeloid cells predetermines lung metastasis. Nat Cell Biol 8:1369–1375. doi:10.1038/ncb1507
Hofmann MA, Drury S, Fu C, Qu W, Taguchi A, Lu Y, Avila C, Kambham N, Bierhaus A, Nawroth P, Neurath MF, Slattery T, Beach D, McClary J, Nagashima M, Morser J, Stern D, Schmidt AM (1999) RAGE mediates a novel proinflammatory axis: a central cell surface receptor for S100/calgranulin polypeptides. Cell 97:889–901 S0092-8674(00)80801-6[pii]
Hu Y, Zhang H, Lu Y, Bai H, Xu Y, Zhu X, Zhou R, Ben J, Chen Q (2011) Class A scavenger receptor attenuates myocardial infarction-induced cardiomyocyte necrosis through suppressing M1 macrophage subset polarization. Basic Res Cardiol 106:1311–1328. doi:10.1007/s00395-011-0204-x
Huttunen HJ, Kuja-Panula J, Sorci G, Agneletti AL, Donato R, Rauvala H (2000) Coregulation of neurite outgrowth and cell survival by amphoterin and S100 proteins through receptor for advanced glycation end products (RAGE) activation. J Biol Chem 275:40096–40105. doi:10.1074/jbc.M006993200M006993200
Ihm SH, Chang K, Kim HY, Baek SH, Youn HJ, Seung KB, Kim JH (2010) Peroxisome proliferator-activated receptor-gamma activation attenuates cardiac fibrosis in type 2 diabetic rats: the effect of rosiglitazone on myocardial expression of receptor for advanced glycation end products and of connective tissue growth factor. Basic Res Cardiol 105:399–407. doi:10.1007/s00395-009-0071-x
Ikemoto M, Tanaka T, Takai Y, Murayama H, Tanaka K, Fujita M (2003) New ELISA system for myeloid-related protein complex (MRP8/14) and its clinical significance as a sensitive marker for inflammatory responses associated with transplant rejection. Clin Chem 49:594–600. doi:10.1373/49.4.594
Katashima T, Naruko T, Terasaki F, Fujita M, Otsuka K, Murakami S, Sato A, Hiroe M, Ikura Y, Ueda M, Ikemoto M, Kitaura Y (2010) Enhanced expression of the S100A8/A9 complex in acute myocardial infarction patients. Circ J 74:741–748 JST.JSTAGE/circj/CJ-09-0564[pii]
Kleinbongard P, Heusch G, Schulz R (2010) TNFalpha in atherosclerosis, myocardial ischemia/reperfusion and heart failure. Pharmacol Ther 127:295–314. doi:10.1016/j.pharmthera.2010.05.002
Kubota T, Bounoutas GS, Miyagishima M, Kadokami T, Sanders VJ, Bruton C, Robbins PD, McTiernan CF, Feldman AM (2000) Soluble tumor necrosis factor receptor abrogates myocardial inflammation but not hypertrophy in cytokine-induced cardiomyopathy. Circulation 101:2518–2525. doi:10.1161/01.CIR.101.21.2518
Liliensiek B, Weigand MA, Bierhaus A, Nicklas W, Kasper M, Hofer S, Plachky J, Grone HJ, Kurschus FC, Schmidt AM, Yan SD, Martin E, Schleicher E, Stern DM, Hammerling GG, Nawroth PP, Arnold B (2004) Receptor for advanced glycation end products (RAGE) regulates sepsis but not the adaptive immune response. J Clin Invest 113:1641–1650. doi:10.1172/JCI18704
Loser K, Vogl T, Voskort M, Lueken A, Kupas V, Nacken W, Klenner L, Kuhn A, Foell D, Sorokin L, Luger TA, Roth J, Beissert S (2010) The Toll-like receptor 4 ligands Mrp8 and Mrp14 are crucial in the development of autoreactive CD8+ T cells. Nat Med 16:713–717. doi:10.1038/nm.2150
Lugering N, Stoll R, Schmid KW, Kucharzik T, Stein H, Burmeister G, Sorg C, Domschke W (1995) The myeloic related protein MRP8/14 (27E10 antigen)—usefulness as a potential marker for disease activity in ulcerative colitis and putative biological function. Eur J Clin Invest 25:659–664. doi:10.1111/j.1365-2362.1995.tb01982.x
Mann DL (2002) Inflammatory mediators and the failing heart: past, present, and the foreseeable future. Circ Res 91:988–998. doi:10.1161/01.RES.0000043825.01705.1B
McCormick MM, Rahimi F, Bobryshev YV, Gaus K, Zreiqat H, Cai H, Lord RS, Geczy CL (2005) S100A8 and S100A9 in human arterial wall. Implications for atherogenesis. J Biol Chem 280:41521–41529. doi:10.1074/jbc.M509442200
McKay RG, Pfeffer MA, Pasternak RC, Markis JE, Come PC, Nakao S, Alderman JD, Ferguson JJ, Safian RD, Grossman W (1986) Left ventricular remodeling after myocardial infarction: a corollary to infarct expansion. Circulation 74:693–702. doi:10.1161/01.CIR.74.4.693
Michel MC, Li Y, Heusch G (2001) Mitogen-activated protein kinases in the heart. Naunyn Schmiedebergs Arch Pharmacol 363:245–266
Nacken W, Roth J, Sorg C, Kerkhoff C (2003) S100A9/S100A8: myeloid representatives of the S100 protein family as prominent players in innate immunity. Microsc Res Tech 60:569–580. doi:10.1002/jemt.10299
Nahrendorf M, Swirski FK, Aikawa E, Stangenberg L, Wurdinger T, Figueiredo JL, Libby P, Weissleder R, Pittet MJ (2007) The healing myocardium sequentially mobilizes two monocyte subsets with divergent and complementary functions. J Exp Med 204:3037–3047. doi:10.1084/jem.20070885
Newton RA, Hogg N (1998) The human S100 protein MRP-14 is a novel activator of the beta 2 integrin Mac-1 on neutrophils. J Immunol 160:1427–1435
Nian M, Lee P, Khaper N, Liu P (2004) Inflammatory cytokines and postmyocardial infarction remodeling. Circ Res 94:1543–1553. doi:10.1161/01.RES.0000130526.20854.fa94/12/1543
Orlova VV, Choi EY, Xie C, Chavakis E, Bierhaus A, Ihanus E, Ballantyne CM, Gahmberg CG, Bianchi ME, Nawroth PP, Chavakis T (2007) A novel pathway of HMGB1-mediated inflammatory cell recruitment that requires Mac-1-integrin. EMBO J 26:1129–1139. doi:10.1038/sj.emboj.7601552
Rahimi F, Hsu K, Endoh Y, Geczy CL (2005) FGF-2, IL-1beta and TGF-beta regulate fibroblast expression of S100A8. FEBS J 272:2811–2827. doi:10.1111/j.1742-4658.2005.04703.x
Riad A, Jager S, Sobirey M, Escher F, Yaulema-Riss A, Westermann D, Karatas A, Heimesaat MM, Bereswill S, Dragun D, Pauschinger M, Schultheiss HP, Tschope C (2008) Toll-like receptor-4 modulates survival by induction of left ventricular remodeling after myocardial infarction in mice. J Immunol 180:6954–6961 180/10/6954[pii]
Ryckman C, Vandal K, Rouleau P, Talbot M, Tessier PA (2003) Proinflammatory activities of S100: proteins S100A8, S100A9, and S100A8/A9 induce neutrophil chemotaxis and adhesion. J Immunol 170:3233–3242
Schmidt AM, Yan SD, Yan SF, Stern DM (2001) The multiligand receptor RAGE as a progression factor amplifying immune and inflammatory responses. J Clin Invest 108:949–955. doi:10.1172/JCI14002
Schnekenburger J, Schick V, Kruger B, Manitz MP, Sorg C, Nacken W, Kerkhoff C, Kahlert A, Mayerle J, Domschke W, Lerch MM (2008) The calcium binding protein S100A9 is essential for pancreatic leukocyte infiltration and induces disruption of cell–cell contacts. J Cell Physiol 216:558–567. doi:10.1002/jcp.21433
Shishido T, Nozaki N, Yamaguchi S, Shibata Y, Nitobe J, Miyamoto T, Takahashi H, Arimoto T, Maeda K, Yamakawa M, Takeuchi O, Akira S, Takeishi Y, Kubota I (2003) Toll-like receptor-2 modulates ventricular remodeling after myocardial infarction. Circulation 108:2905–2910. doi:10.1161/01.CIR.0000101921.93016.1C01.CIR.0000101921.93016.1C
Sun C, Liang C, Ren Y, Zhen Y, He Z, Wang H, Tan H, Pan X, Wu Z (2009) Advanced glycation end products depress function of endothelial progenitor cells via p38 and ERK 1/2 mitogen-activated protein kinase pathways. Basic Res Cardiol 104:42–49. doi:10.1007/s00395-008-0738-8
Valeur HS, Valen G (2009) Innate immunity and myocardial adaptation to ischemia. Basic Res Cardiol 104:22–32. doi:10.1007/s00395-008-0756-6
Vandal K, Rouleau P, Boivin A, Ryckman C, Talbot M, Tessier PA (2003) Blockade of S100A8 and S100A9 suppresses neutrophil migration in response to lipopolysaccharide. J Immunol 171:2602–2609
Viemann D, Strey A, Janning A, Jurk K, Klimmek K, Vogl T, Hirono K, Ichida F, Foell D, Kehrel B, Gerke V, Sorg C, Roth J (2005) Myeloid-related proteins 8 and 14 induce a specific inflammatory response in human microvascular endothelial cells. Blood 105:2955–2962. doi:10.1182/blood-2004-07-2520
Vogl T, Ludwig S, Goebeler M, Strey A, Thorey IS, Reichelt R, Foell D, Gerke V, Manitz MP, Nacken W, Werner S, Sorg C, Roth J (2004) MRP8 and MRP14 control microtubule reorganization during transendothelial migration of phagocytes. Blood 104:4260–4268. doi:10.1182/blood-2004-02-04462004-02-0446
Vogl T, Tenbrock K, Ludwig S, Leukert N, Ehrhardt C, van Zoelen MA, Nacken W, Foell D, van der Poll T, Sorg C, Roth J (2007) Mrp8 and Mrp14 are endogenous activators of Toll-like receptor 4, promoting lethal, endotoxin-induced shock. Nat Med 13:1042–1049. doi:10.1038/nm1638
Volz HC, Seidel C, Laohachewin D, Kaya Z, Muller OJ, Pleger ST, Lasitschka F, Bianchi ME, Remppis A, Bierhaus A, Katus HA, Andrassy M (2010) HMGB1: the missing link between diabetes mellitus and heart failure. Basic Res Cardiol 105:805–820. doi:10.1007/s00395-010-0114-3
Weisman HF, Bush DE, Mannisi JA, Weisfeldt ML, Healy B (1988) Cellular mechanisms of myocardial infarct expansion. Circulation 78:186–201. doi:10.1161/01.CIR.78.1.186
Wu J, Li J, Zhang N, Zhang C (2011) Stem cell-based therapies in ischemic heart diseases: a focus on aspects of microcirculation and inflammation. Basic Res Cardiol 106:317–324. doi:10.1007/s00395-011-0168-x
Yan SF, Ramasamy R, Naka Y, Schmidt AM (2003) Glycation, inflammation, and RAGE: a scaffold for the macrovascular complications of diabetes and beyond. Circ Res 93:1159–1169. doi:10.1161/01.RES.0000103862.26506.3D93/12/1159
Acknowledgments
This study was supported by the Carl Baresel Stiftung (MA), the German Research Foundation (MA, AN 403/2-1), the German Heart Foundation (MA, F/36/08) and the European Foundation for the Study of Diabetes (MA).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Volz, H.C., Laohachewin, D., Seidel, C. et al. S100A8/A9 aggravates post-ischemic heart failure through activation of RAGE-dependent NF-κB signaling. Basic Res Cardiol 107, 250 (2012). https://doi.org/10.1007/s00395-012-0250-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-012-0250-z