Abstract
Purpose
Epidemiological studies support a protective role of habitual coffee and caffeine consumption against the risk of non-alcoholic fatty liver disease (NAFLD). We aimed to investigate the causal relationship between coffee intake and the risk of NAFLD.
Methods
We performed a two-sample Mendelian randomization (MR) analysis using SNPs associated with habitual coffee intake in a published genome-wide association study (GWAS) as genetic instruments and summary-level data from a published GWAS of NAFLD (1122 cases and 399,900 healthy controls) in the UK Biobank. The causal relationship was estimated with the inverse weighted method using a 4-SNP and 6-SNP instrument based on the single largest non-UK Biobank GWAS (n = 91,462) and meta-analysis (n = 121,524) of GWAS data on habitual coffee intake, respectively. To maximize power, we also used up to 77 SNPs associated with coffee intake at a liberal significance level (p ≤ 1e-4) as instruments.
Results
We observed a non-significant trend towards a causal protective effect of coffee intake on NAFLD based upon either the 4-SNP (OR: 0.76; 95% CI 0.51, 1.14, p = 0.19) or 6-SNP genetic instruments (OR: 0.77; 95% CI 0.48, 1.25, p = 0.29). The result also remains non-significant when using the more liberal 77-SNP instrument.
Conclusion
Our findings do not support a causal relationship between coffee intake and NAFLD risk. However, despite the largest-to-date sample size, the power of this study may be limited by the non-specificity and moderate effect size of the genetic alleles on coffee intake.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nonalcoholic fatty liver disease (NAFLD) is defined as the development of an abnormal accumulation of fat in the liver without significant alcohol intake, which may further progress to a wide spectrum of liver damage ranging from steatosis, non-alcoholic steatohepatitis (NASH), fibrosis and cirrhosis. The treatment option for NAFLD is still limited and currently, no pharmacotherapy is approved by the FDA to date. Physical activity and dietary interventions are still considered to be effective strategies to reduce liver fat at the initial, reversible stage of NAFLD such as hepatic steatosis and NASH [1,2,3].
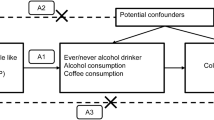
Coffee is the most popular and widely consumed beverage in the world. It has been estimated that approximately 3.5 billion cups of coffee are consumed around the world each day [4,5,6]. Multiple epidemiological studies have demonstrated the protective association of coffee intake with the development of NAFLD, and the potential beneficial effects of coffee have also been examined with animal models [7,8,9,10]. However, there is thus far no sufficient evidence in human studies to clarify the causal association between coffee intake and the risk of NAFLD. One strategy to address this question is to perform a randomized controlled trial (RCT) to examine whether coffee intake can directly reduce the development of NAFLD. However, this would require a large sample size over a long period of time (given the chronic development of NAFLD) to generate any results. Over the past several years, Mendelian randomization (MR) has increasingly been used to effectively estimate the causal relationship between a modifiable environmental exposure of interest and a medically relevant trait or disease [11]. The MR analysis was designed based on the Mendelian inheritance rule where the parental genetic alleles (i.e., risk allele or non-risk allele) are randomly distributed to the offspring during the process of meiosis, which is considered to be analogous to RCT. This strategy was deemed to be convenient, low cost and less likely to be confounded by covariables [12]. The MR analysis uses genetic variants as the risk instrumental variables (IVs) of exposure (i.e., coffee intake), to examine whether this genetically-instrumented exposure is causally associated with a clinical outcome (i.e., NAFLD).
Genome-wide association studies (GWAS) have identified multiple loci that are strongly associated with coffee consumption [13, 14]. The identification of these genetic variants (e.g., SNPs) provides an opportunity to apply the MR analysis to test the causal relationship between coffee intake and NAFLD risk. Once confirmed, this strategy would provide strong evidence to rationalize the use of coffee intake to prevent the development of NAFLD. In this study, we apply a two-sample MR framework using SNPs associated with coffee consumption in published GWAS [13] to test the causal relationships between coffee intake and NAFLD risk as estimated using summary-level data from our recent GWAS in the UK Biobank [15].
Materials and methods
GWAS summary data for habitual coffee consumption
The most recent genome-wide meta-analysis for self-reported consumption of coffee included a significant proportion of UK Biobank samples (UK Biobank samples/total samples = 335,909/375,833 = 89.4%) [14], which may largely overlap with the cohort for the NAFLD GWAS (1122 cases and 399,900 healthy controls from UK Biobank, see more details on NAFLD GWAS in the following section). To minimize the bias induced by the participant overlap in two-sample MR [16], we obtained the summary statistics of the genetic associations with habitual coffee consumption from the largest UK Biobank-independent genome-wide meta-analysis [13]. The summary data of individuals of European descent (discovery stage: n = 91,462, validation stage: n = 30,062) were used for the MR analysis. Details on the study design, data analysis, and ethical approval were described in the original publication [13]. The original study performed a trans-ethnic meta-analysis for coffee consumption including individuals of European ancestry and African Americans. As we focused on the causal relationship between coffee intake and NAFLD among individuals of European ancestry, we performed a meta-analysis combining the summary-level data of the European individuals in the discovery (n = 91,462) and validation (n = 30,062) stages. The combined effects were analyzed through the “metafor” R package [17] assuming a fixed-effect model. Due to limited data availability, the meta-analyses were performed on the top ten significant (p < 1e-5) SNPs associated with coffee intake identified from the discovery stage. The results of the meta-analysis are shown in supplemental Table 1.
GWAS summary data for NAFLD
The summary-level association data for NAFLD were obtained from our previous GWAS study on NAFLD using the UK Biobank [15]. Individuals with ICD code [ICD-9 571.8 “Other chronic nonalcoholic liver disease” and ICD-10 K76.0 “Fatty (change of) liver, not elsewhere classified”] but without hepatitis B or C infection or other liver diseases were characterized as NAFLD cases. In total, there were 1122 cases and 399,900 healthy controls analyzed for the genome-wide associations with NAFLD. Basic demographic and clinical information for cases and controls is summarized in Table 1. We performed the association analysis using SAIGE [18] adjusting for sex, birth year, and the first four genetic PCs as covariates.
Construction of the genetic predictors for coffee intake
We constructed two genetic instruments for coffee intake based on the association statistics obtained from the discovery stage and the meta-analysis. Specifically, the first one included four independent (LD R2 < 0.01 based on the phase 3 data of the 1 kg European individuals) and genome-wide significant (p < 5e-08) SNPs identified in the discovery stage (n = 91,462) (Table 2). The second one consisted of six independent (LD R2 < 0.01) and genome-wide significant (p < 5e-08) SNPs identified through the meta-analysis (Table 3).
To assess the possibility of an insufficiently powered IV, we considered a third IV based on SNP–coffee associations at a liberal significance level (ranging from p = 5e-8 to p = 1e-4 in the discovery GWAS), which consisted of up to 77 SNPs.
We evaluated the strengths of the two genetic instruments using the F statistics = \(\left( {\frac{n - k - 1}{k}} \right)\left( {\frac{{R^{2} }}{{1 - R^{2} }}} \right)\), where n is the sample size, k is the number of genetic variants, and R2 is the variance in coffee intake explained by the genetic instrument. The strengths of the first (4 SNPs) and the second (6 SNPs) genetic instruments used for MR analysis were 124 and 119, respectively. Both F statistics were larger than the empirical strength threshold of 10 [19].
MR analysis
The inverse variance weighted (IVW) [20] method was used to estimate the causal effect of coffee intake on NAFLD risk. Since the IVW method requires that all instrumental variables meet the MR assumptions, we used two orthogonal methods (weighted median estimator [21] and MR-Egger [22]) to perform additional sensitivity analyses. The weighted median estimator provides consistent causal estimation as long as more than half of the instrumental variables are valid. The MR-Egger estimate is unbiased provided that the genetic instrument is not dependent on the pleiotropic effects. The intercept of the MR-Egger estimate is an indicator of the existence of the pleiotropic effects. We considered the absence of pleiotropic effects if the intercept was not significantly different from 0 (p > 0.05). Moreover, we used the MR-PRESSO global test [23] to evaluate the pleiotropy and identify outlier variants. The causal relationship is considered to be significant if (1) the p value of IVW method is less than 0.05, (2) the directions of estimates by the IVW, weighted median, and MR-Egger methods are the same and (3) both the MR-Egger intercept test and the MR-PRESSO global test are not significant (p > 0.05). The IVW, weighted median, and MR-Egger methods were performed using the “Mendelian Randomization” package [24], and MR-PRESSO global test was performed using the “MRPRESSO” package [23]. All of the data were analyzed and visualized using R v.3.5.0 (https://www.r-project.org/).
Results
No statistically significant causal effect of coffee consumption on NAFLD risk was observed in analysis using either the 4-SNP score (OR: 0.76; 95% CI 0.51, 1.14, p = 0.19, Table 4, Fig. 1a), or 6-SNP score (OR: 0.77; 95% CI 0.48, 1.25, p = 0.29, Table 4, Fig. 1b).
Results from sensitivity analysis indicated that the causal estimates were unlikely to be biased by the pleiotropic effects (MR-Egger intercept test p = 0.69 and 0.54 for 4-SNP and 6-SNP score, respectively, MR-PRESSO global test p = 0.97 and 0.84 for 4-SNP and 6-SNP score, respectively). To assess the possibility of an insufficiently powered IV, we considered a third IV based on SNP–coffee associations at a liberal significance level (ranging from p = 5e-8 to p = 1e-4). Again, no statistically significant causal relationship was observed (Table 5).
Discussion
We performed the first two-sample MR analysis of coffee intake and the risk of NAFLD based on the summary-level data of large GWASs of coffee intake (exposure) and NAFLD (outcome). We observed no evidence in support of a causal relationship between coffee intake and NAFLD risk.
Coffee contains more than 1500 chemical components including caffeine, phenolic polymer, polysaccharides, chlorogenic acids, organic acids, et al. [25, 26]. Studies have demonstrated compounds in coffee exhibit antioxidant and anti-inflammatory properties [27, 28]. It has been suggested that coffee intake or components of coffee may have beneficial effects on metabolic disorders, e.g., obesity and diabetes. Multiple studies have indicated that caffeine intake leads to weight loss by enhancing thermogenesis and increased production of energy among type 2 diabetes patients with overweight [29]. Habitual coffee consumption may also be able to attenuate the genetic risk for increased BMI and obesity [30]. In addition to weight loss, coffee and its components have also demonstrated to enhance insulin secretion and sensitivity. Loopstra-Masters et al. [31] showed that caffeinated coffee intake can increase the insulin sensitivity while decaffeinated coffee was positively correlated with beta cell function in a population-based study included 954 multi-ethnic non-diabetic adults from the Insulin Resistance Atherosclerosis Study. As another biological component of coffee, cafestol was shown to significantly increase insulin secretion in insulinoma cells of the INS-1E rat [32]. Another study also suggested that coffee may also upregulate the function of skeletal muscle [33].
With regard to NAFLD, epidemiological studies have indicated that coffee intake is significantly associated with reduced risk of NAFLD [10, 34]. Animal studies also indicated that caffeine or other nutritional components in coffee may exert certain health benefits such as reducing angiogenesis and the production of reactive oxygen species [35, 36], improving insulin sensitivity, decreasing body weight and liver triglycerides [7,8,9,10, 37, 38], as well as reducing the pro-fibrotic activity of hepatic stellate cells and pro-inflammatory activity of Kupffer cells [39, 40]. Coffee may also alter the diversity of the gut microbiota, thus modulating the gut–liver axis for energy uptake and metabolism [8, 41]. Based on these observations, there is increasing interest in using coffee as supplementation for NAFLD prevention. However, despite these lines of evidence, the causal association between coffee intake and reduced NAFLD risk in humans remains unclear. Findings of the current study do not support a significant causal relationship and echoed the work done by Nordestgaard et al. [42] where genetically derived high coffee intake was not causally associated with obesity, metabolic syndrome and type 2 diabetes. Also, Hosseinabadi et al. [43] found that green coffee extract supplementation had no effect on liver steatosis grade, serum level of ALT, AST, LDL-C, total cholesterol and adiponectin in NAFLD clinical trials, albeit that BMI and serum HDL-C shows significant changes when compared to the control group.
The discrepancies between the epidemiological observations and the non-significant causal relationship between coffee consumption and NAFLD in our study could be due to multiple reasons. As we have summarized previously [44], the genetic alleles identified in GWAS of coffee drinking may be associated with caffeine metabolism, reward-response and potentially taste and thus not strong and specific genetic markers of coffee drinking per se. Pleiotropy is of particular concern. Indeed, seven of 14 SNPs reaching genome-wide significance are also strongly associated with other traits [44]. To address this potential bias, we used up to 77 different genetic variants to explore the causal association between coffee intake and NAFLD but obtained similar results. Finally, despite the very large sample size, we may still have been underpowered to rule-in or rule-out a causal relationship. These reasons may be an intrinsic issue of coffee genetics since a number of MR analyses have been published to date studying the causal relationship between coffee intake and many clinical outcomes but the majority of these studies did not show evidence for such a causal linkage [45,46,47,48]. It should be also noted that the NAFLD phenotype in our study is based on the ICD codes which may not reflect the true disease spectrum as observed in clinically characterized NAFLD patients. Unfortunately, although a few GWAS studies on clinically validated NAFLD have been published, the full summary data of these studies are not publically available to support a MR analysis. However, as demonstrated in our previous study [15], the GWAS based on these ICD codes-defined NAFLD produced a signature of genetic variants at the genome-wide level that is highly similar to the well-established genetic alleles and underlying genes identified in previous GWASs for NAFLD (e.g., PNPLA3, TM6SF2, etc.), suggesting that our GWAS data are reliable for MR analyses.
Conclusion
Our findings provided no statistically compelling evidence to support a causal relationship between coffee intake and NAFLD risk. However, our study may be limited by the choice of instrument variables that are not necessarily associated with coffee consumption. The study may be underpowered as well. More studies with a better-defined phenotype and well-characterized populations or clinical studies are needed to further clarify the true impact of coffee intake and the NAFLD risk.
References
Jeznach-Steinhagen A, Ostrowska J, Czerwonogrodzka-Senczyna A, Boniecka I, Shahnazaryan U, Kurylowicz A (2019) Dietary and pharmacological treatment of nonalcoholic fatty liver disease. Medicina (Kaunas). https://doi.org/10.3390/medicina55050166
Perdomo CM, Fruhbeck G, Escalada J (2019) Impact of nutritional changes on nonalcoholic fatty liver disease. Nutrients. https://doi.org/10.3390/nu11030677
Suarez M, Boque N, Del Bas JM, Mayneris-Perxachs J, Arola L, Caimari A (2017) Mediterranean diet and multi-ingredient-based interventions for the management of non-alcoholic fatty liver disease. Nutrients. https://doi.org/10.3390/nu9101052
Storey ML, Forshee RA, Anderson PA (2006) Beverage consumption in the US population. J Am Diet Assoc 106(12):1992–2000. https://doi.org/10.1016/j.jada.2006.09.009
Carlstrom M, Larsson SC (2018) Coffee consumption and reduced risk of developing type 2 diabetes: a systematic review with meta-analysis. Nutr Rev 76(6):395–417. https://doi.org/10.1093/nutrit/nuy014
Saab S, Mallam D, Cox GA 2nd, Tong MJ (2014) Impact of coffee on liver diseases: a systematic review. Liver Int 34(4):495–504. https://doi.org/10.1111/liv.12304
Wijarnpreecha K, Thongprayoon C, Ungprasert P (2017) Coffee consumption and risk of nonalcoholic fatty liver disease: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 29(2):e8–e12. https://doi.org/10.1097/MEG.0000000000000776
Vitaglione P, Mazzone G, Lembo V, D'Argenio G, Rossi A, Guido M, Savoia M, Salomone F, Mennella I, De Filippis F, Ercolini D, Caporaso N, Morisco F (2019) Coffee prevents fatty liver disease induced by a high-fat diet by modulating pathways of the gut-liver axis. J Nutr Sci 8:e15. https://doi.org/10.1017/jns.2019.10
Shokouh P, Jeppesen PB, Hermansen K, Norskov NP, Laustsen C, Jacques Hamilton-Dutoit S, Qi H, Stodkilde-Jorgensen H, Gregersen S (2017) A combination of coffee compounds shows insulin-sensitizing and hepatoprotective effects in a rat model of diet-induced metabolic syndrome. Nutrients. https://doi.org/10.3390/nu10010006
Chen YP, Lu FB, Hu YB, Xu LM, Zheng MH, Hu ED (2018) A systematic review and a dose-response meta-analysis of coffee dose and nonalcoholic fatty liver disease. Clin Nutr. https://doi.org/10.1016/j.clnu.2018.11.030
Zheng J, Baird D, Borges MC, Bowden J, Hemani G, Haycock P, Evans DM, Smith GD (2017) Recent developments in mendelian randomization studies. Curr Epidemiol Rep 4(4):330–345. https://doi.org/10.1007/s40471-017-0128-6
Paternoster L, Tilling K, Smith GD (2017) Genetic epidemiology and Mendelian randomization for informing disease therapeutics: conceptual and methodological challenges. PLoS Genet. https://doi.org/10.1371/journal.pgen.1006944
Coffee, Caffeine Genetics C, Cornelis MC, Byrne EM, Esko T, Nalls MA, Ganna A, Paynter N, Monda KL, Amin N, Fischer K, Renstrom F, Ngwa JS, Huikari V, Cavadino A, Nolte IM, Teumer A, Yu K, Marques-Vidal P, Rawal R, Manichaikul A, Wojczynski MK, Vink JM, Zhao JH, Burlutsky G, Lahti J, Mikkila V, Lemaitre RN, Eriksson J, Musani SK, Tanaka T, Geller F, Luan J, Hui J, Magi R, Dimitriou M, Garcia ME, Ho WK, Wright MJ, Rose LM, Magnusson PK, Pedersen NL, Couper D, Oostra BA, Hofman A, Ikram MA, Tiemeier HW, Uitterlinden AG, van Rooij FJ, Barroso I, Johansson I, Xue L, Kaakinen M, Milani L, Power C, Snieder H, Stolk RP, Baumeister SE, Biffar R, Gu F, Bastardot F, Kutalik Z, Jacobs DR Jr, Forouhi NG, Mihailov E, Lind L, Lindgren C, Michaelsson K, Morris A, Jensen M, Khaw KT, Luben RN, Wang JJ, Mannisto S, Perala MM, Kahonen M, Lehtimaki T, Viikari J, Mozaffarian D, Mukamal K, Psaty BM, Doring A, Heath AC, Montgomery GW, Dahmen N, Carithers T, Tucker KL, Ferrucci L, Boyd HA, Melbye M, Treur JL, Mellstrom D, Hottenga JJ, Prokopenko I, Tonjes A, Deloukas P, Kanoni S, Lorentzon M, Houston DK, Liu Y, Danesh J, Rasheed A, Mason MA, Zonderman AB, Franke L, Kristal BS, International Parkinson’s Disease Genomics C, North American Brain Expression C, Consortium UKBE, Karjalainen J, Reed DR, Westra HJ, Evans MK, Saleheen D, Harris TB, Dedoussis G, Curhan G, Stumvoll M, Beilby J, Pasquale LR, Feenstra B, Bandinelli S, Ordovas JM, Chan AT, Peters U, Ohlsson C, Gieger C, Martin NG, Waldenberger M, Siscovick DS, Raitakari O, Eriksson JG, Mitchell P, Hunter DJ, Kraft P, Rimm EB, Boomsma DI, Borecki IB, Loos RJ, Wareham NJ, Vollenweider P, Caporaso N, Grabe HJ, Neuhouser ML, Wolffenbuttel BH, Hu FB, Hypponen E, Jarvelin MR, Cupples LA, Franks PW, Ridker PM, van Duijn CM, Heiss G, Metspalu A, North KE, Ingelsson E, Nettleton JA, van Dam RM, Chasman DI (2015) Genome-wide meta-analysis identifies six novel loci associated with habitual coffee consumption. Mol Psychiatry 20(5):647–656. https://doi.org/10.1038/mp.2014.107
Zhong VW, Kuang A, Danning RD, Kraft P, van Dam RM, Chasman DI, Cornelis MC (2019) A genome-wide association study of bitter and sweet beverage consumption. Hum Mol Genet 28(14):2449–2457. https://doi.org/10.1093/hmg/ddz061
Liu Z, Zhang Y, Graham S, Wang X, Cai D, Huang M, Pique-Regi R, Dong XC, Chen YE, Willer C, Liu W (2020) Causal relationships between NAFLD, T2D and obesity have implications for disease subphenotyping. J Hepatol 73(2):263–276. https://doi.org/10.1016/j.jhep.2020.03.006
Burgess S, Davies NM, Thompson SG (2016) Bias due to participant overlap in two-sample Mendelian randomization. Genet Epidemiol 40(7):597–608. https://doi.org/10.1002/gepi.21998
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor package. J Stat Softw 36(3):1–48
Zhou W, Nielsen JB, Fritsche LG, Dey R, Gabrielsen ME, Wolford BN, LeFaive J, VandeHaar P, Gagliano SA, Gifford A, Bastarache LA, Wei WQ, Denny JC, Lin M, Hveem K, Kang HM, Abecasis GR, Willer CJ, Lee S (2018) Efficiently controlling for case-control imbalance and sample relatedness in large-scale genetic association studies. Nat Genet 50(9):1335–1341. https://doi.org/10.1038/s41588-018-0184-y
Staiger D, Stock JH (1997) Instrumental variables regression with weak instruments. Econometrica 65(3):557–586. https://doi.org/10.2307/2171753
Burgess S, Butterworth A, Thompson SG (2013) Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol 37(7):658–665. https://doi.org/10.1002/gepi.21758
Bowden J, Smith GD, Haycock PC, Burgess S (2016) Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol 40(4):304–314. https://doi.org/10.1002/gepi.21965
Bowden J, Smith GD, Burgess S (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 44(2):512–525. https://doi.org/10.1093/ije/dyv080
Verbanck M, Chen CY, Neale B, Do R (2018) Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. https://doi.org/10.1038/s41588-018-0099-7
Yavorska OO, Burgess S (2017) MendelianRandomization: an R package for performing Mendelian randomization analyses using summarized data. Int J Epidemiol 46(6):1734–1739. https://doi.org/10.1093/ije/dyx034
Metro D, Cernaro V, Santoro D, Papa M, Buemi M, Benvenga S, Manasseri L (2017) Beneficial effects of oral pure caffeine on oxidative stress. J Clin Transl Endocrinol 10:22–27. https://doi.org/10.1016/j.jcte.2017.10.001
Nishitsuji K, Watanabe S, Xiao J, Nagatomo R, Ogawa H, Tsunematsu T, Umemoto H, Morimoto Y, Akatsu H, Inoue K, Tsuneyama K (2018) Effect of coffee or coffee components on gut microbiome and short-chain fatty acids in a mouse model of metabolic syndrome. Sci Rep 8(1):16173. https://doi.org/10.1038/s41598-018-34571-9
Jung S, Kim MH, Park JH, Jeong Y, Ko KS (2017) Cellular antioxidant and anti-inflammatory effects of coffee extracts with different roasting levels. J Med Food 20(6):626–635. https://doi.org/10.1089/jmf.2017.3935
Choi B, Koh E (2017) Spent coffee as a rich source of antioxidative compounds. Food Sci Biotechnol 26(4):921–927. https://doi.org/10.1007/s10068-017-0144-9
Santos RM, Lima DR (2016) Coffee consumption, obesity and type 2 diabetes: a mini-review. Eur J Nutr 55(4):1345–1358. https://doi.org/10.1007/s00394-016-1206-0
Wang T, Huang T, Kang JH, Zheng Y, Jensen MK, Wiggs JL, Pasquale LR, Fuchs CS, Campos H, Rimm EB, Willett WC, Hu FB, Qi L (2017) Habitual coffee consumption and genetic predisposition to obesity: gene-diet interaction analyses in three US prospective studies. BMC Med 15(1):97. https://doi.org/10.1186/s12916-017-0862-0
Loopstra-Masters RC, Liese AD, Haffner SM, Wagenknecht LE, Hanley AJ (2011) Associations between the intake of caffeinated and decaffeinated coffee and measures of insulin sensitivity and beta cell function. Diabetologia 54(2):320–328. https://doi.org/10.1007/s00125-010-1957-8
Mellbye FB, Jeppesen PB, Hermansen K, Gregersen S (2015) Cafestol, a bioactive substance in coffee, stimulates insulin secretion and increases glucose uptake in muscle cells: studies in vitro. J Nat Prod 78(10):2447–2451. https://doi.org/10.1021/acs.jnatprod.5b00481
Jang YJ, Son HJ, Kim JS, Jung CH, Ahn J, Hur J, Ha TY (2018) Coffee consumption promotes skeletal muscle hypertrophy and myoblast differentiation. Food Funct 9(2):1102–1111. https://doi.org/10.1039/c7fo01683b
Molloy JW, Calcagno CJ, Williams CD, Jones FJ, Torres DM, Harrison SA (2012) Association of coffee and caffeine consumption with fatty liver disease, nonalcoholic steatohepatitis, and degree of hepatic fibrosis. Hepatology 55(2):429–436. https://doi.org/10.1002/hep.24731
Espindola KMM, Ferreira RG, Narvaez LEM, Silva Rosario ACR, da Silva AHM, Silva AGB, Vieira APO, Monteiro MC (2019) Chemical and pharmacological aspects of caffeic acid and its activity in hepatocarcinoma. Front Oncol 9:541. https://doi.org/10.3389/fonc.2019.00541
Sidoryk K, Jaromin A, Filipczak N, Cmoch P, Cybulski M (2018) Synthesis and antioxidant activity of caffeic acid derivatives. Molecules. https://doi.org/10.3390/molecules23092199
Shokouh P, Jeppesen PB, Hermansen K, Laustsen C, Stodkilde-Jorgensen H, Hamilton-Dutoit SJ, Sondergaard Schmedes M, Qi H, Stokholm Norlinger T, Gregersen S (2018) Effects of unfiltered coffee and bioactive coffee compounds on the development of metabolic syndrome components in a high-fat-/high-fructose-fed rat model. Nutrients. https://doi.org/10.3390/nu10101547
Caro-Gomez E, Sierra JA, Escobar JS, Alvarez-Quintero R, Naranjo M, Medina S, Velasquez-Mejia EP, Tabares-Guevara JH, Jaramillo JC, Leon-Varela YM, Munoz-Durango K, Ramirez-Pineda JR (2019) Green coffee extract improves cardiometabolic parameters and modulates gut microbiota in high-fat-diet-fed ApoE(-/-) mice. Nutrients. https://doi.org/10.3390/nu11030497
Arauz J, Zarco N, Hernandez-Aquino E, Galicia-Moreno M, Favari L, Segovia J, Muriel P (2017) Coffee consumption prevents fibrosis in a rat model that mimics secondary biliary cirrhosis in humans. Nutr Res 40:65–74. https://doi.org/10.1016/j.nutres.2017.03.008
Seo HY, Kim MK, Lee SH, Hwang JS, Park KG, Jang BK (2018) Kahweol Ameliorates the liver inflammation through the inhibition of NF-kappaB and STAT3 activation in primary kupffer cells and primary hepatocytes. Nutrients. https://doi.org/10.3390/nu10070863
Bajaj JS, Idilman R, Mabudian L, Hood M, Fagan A, Turan D, White MB, Karakaya F, Wang J, Atalay R, Hylemon PB, Gavis EA, Brown R, Thacker LR, Acharya C, Heuman DM, Sikaroodi M, Gillevet PM (2018) Diet affects gut microbiota and modulates hospitalization risk differentially in an international cirrhosis cohort. Hepatology 68(1):234–247. https://doi.org/10.1002/hep.29791
Nordestgaard AT, Thomsen M, Nordestgaard BG (2015) Coffee intake and risk of obesity, metabolic syndrome and type 2 diabetes: a Mendelian randomization study. Int J Epidemiol 44(2):551–565. https://doi.org/10.1093/ije/dyv083
Hosseinabadi S, Rafraf M, Asghari S, Asghari-Jafarabadi M, Vojouhi S (2020) Effect of green coffee extract supplementation on serum adiponectin concentration and lipid profile in patients with non-alcoholic fatty liver disease: a randomized, controlled trial. Complement Ther Med 49:102290. https://doi.org/10.1016/j.ctim.2019.102290
Cornelis MC, Munafo MR (2018) Mendelian randomization studies of coffee and caffeine consumption. Nutrients. https://doi.org/10.3390/nu10101343
Georgiou AN, Ntritsos G, Papadimitriou N, Dimou N, Evangelou E (2020) Cigarette smoking, coffee consumption, alcohol intake, and risk of crohn’s disease and ulcerative colitis: a mendelian randomization study. Inflamm Bowel Dis. https://doi.org/10.1093/ibd/izaa152
Nicolopoulos K, Mulugeta A, Zhou A, Hypponen E (2020) Association between habitual coffee consumption and multiple disease outcomes: a Mendelian randomisation phenome-wide association study in the UK Biobank. Clin Nutr. https://doi.org/10.1016/j.clnu.2020.03.009
Qian Y, Ye D, Huang H, Wu DJH, Zhuang Y, Jiang X, Mao Y (2020) Coffee consumption and risk of stroke: a mendelian randomization study. Ann Neurol 87(4):525–532. https://doi.org/10.1002/ana.25693
Lu H, Wu PF, Zhang W, Xia K (2020) Coffee consumption is not associated with risk of multiple sclerosis: a Mendelian randomization study. Mult Scler Relat Disord 44:102300. https://doi.org/10.1016/j.msard.2020.102300
Acknowledgements
This study is supported in part by the NIH/NIDDK Grant (R01DK106540) (W.L.), and the start-up fund of the Office of Vice President for Research of Wayne State University (W.L.). The authors would like to thank all the genetics consortiums for making the GWAS summary data publicly available.
Funding
This study is supported in part by the NIH/NIDDK Grant (R01DK106540) (W.L.), and the start-up fund of the Office of Vice President for Research of Wayne State University (W.L.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Y., Liu, Z., Choudhury, T. et al. Habitual coffee intake and risk for nonalcoholic fatty liver disease: a two-sample Mendelian randomization study. Eur J Nutr 60, 1761–1767 (2021). https://doi.org/10.1007/s00394-020-02369-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-020-02369-z