Abstract
Purpose
The effects of regular coffee intake on weight gain and development of diabetes are reviewed. The pathophysiology of obesity and type 2 diabetes as well as the necessity of preventive options based on the increasing prevalence of these two disorders worldwide is briefly discussed. The relationship between weight gain and development of diabetes is also presented. The two major constituents in the brewed coffee, chlorogenic acids and caffeine, are responsible for many of the beneficial effects suggested by numerous epidemiological studies of coffee consumption and the development of diabetes.
Methods
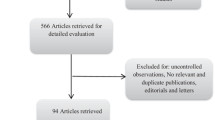
A wide search of various databases, such as PubMed and Google Scholar, preceded the writing of this manuscript, focusing on key words that are part of the title. It was selected mainly review papers from in vivo, ex vivo, in vitro experimental studies in animals and human tissues as well as wide population-based epidemiological studies in the last 10 years.
Conclusion
As of today, there are mounting evidences of the reduced risk of developing type 2 diabetes by regular coffee drinkers of 3–4 cups a day. The effects are likely due to the presence of chlorogenic acids and caffeine, the two constituents of coffee in higher concentration after the roasting process.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This abbreviated review on the effects of coffee on weight gain and development of type 2 diabetes mellitus (T2DM) is a collection of the latest data of experimental studies in vitro and in vivo, as well as large epidemiological studies during the last decade. It starts by discussing the importance of those two pathological disorders, obesity and diabetes, and its growing prevalence in the worldwide population. It proceeds with a brief review on the pathophysiological mechanisms that link those two disorders and provides an overview of the necessary conditions for the development and diagnosis of T2DM. The main body of the review is summarized in Fig. 6 where the possible mechanisms of coffee preventive effects on weight gain and T2DM are presented. The mechanisms are displayed according to their relationship with metabolism of carbohydrates and lipids. Other mechanisms that are not specifically affecting one of those metabolisms, but involving major pathways, such as activation of AMPK, hormonal regulation and the role of sex-hormone-binding globulin, are also presented. It closes with a recent mechanism possibly involving the contents of chlorogenic acids in the coffee. It is based on the fact that chlorogenic acids increase the levels of a major adipocytokine secreted by adipose tissue. These elevated plasma levels are consistently inversely related to the occurrence of diseases such as diabetes, metabolic syndrome and cardiovascular disorders.
Obesity and type 2 diabetes
Obesity may be defined as accumulation of fat to an extent that the health of the individual is impaired [1]. Truncal obesity, which is fat mainly distributed around abdomen and viscera, is particularly correlated with the prevalence of diabetes and cardiovascular diseases [1–6]. Diabesity [3, 7–9]—the term used to describe the coexistence of T2DM and obesity—is responsible for more than 90 % of the world’s 382 million people with T2DM, and this number is set to rise beyond 592 million in less than 25 years. Yet, with 175 million cases currently undiagnosed, a vast amount of people with diabetes is progressing unaware toward complications. Moreover, with 80 % of the total number affected living in low- and middle-income countries, the epidemic is gathering pace at alarming rates (Figs. 1, 2) [10, 11]. Still, according to International Diabetes Federation (IDF) Atlas 6th edition, type 2 diabetes is the fourth to fifth leading cause of death in most high-income countries, with almost 50 % of the people with diabetes ranging from 40 to 59 years of age. Spending on diabetes accounts for 10.8 % of total health expenditure worldwide and caused 5.1 million deaths in 2013. This means that every 6 s a person dies from diabetes. In addition, more than 21 million live births were affected by diabetes during pregnancy in 2013. Another important source of information on the prevalence of diabetes in USA is The Behavioral Risk Factor Surveillance System (BRFSS), the largest ongoing telephone health survey in the world. It is a state-based system of health surveys established by the Centers for Disease Control and Prevention (CDC) in 1984. The most recent report shows the age-adjusted prevalence of obesity and the number of diagnosed diabetes among adults in USA with data from 2013 (Fig. 3) [12]. Therefore, we can conclude that diabetes is the one most common non-communicable disease, and it is epidemic in many economically developing and newly industrialized countries.
Estimated number of people with diabetes worldwide and per region in 2013. After International Diabetes Federation. IDF Diabetes Atlas, 6th edn. Brussels, Belgium: International Diabetes Federation, 2013. http://www.idf.org/diabetesatlas
World diabetes expected cases by the year of 2035. After International Diabetes Federation. IDF Diabetes Atlas, 6th edn. Brussels, Belgium: International Diabetes Federation, 2013. http://www.idf.org/diabetesatlas
Age adjusted prevalence of obesity and diagnosed diabetes among US adults. After CDC’s Division of Diabetes Translation. National Diabetes Surveillance System available at http://www.cdc.gov/diabetes/statistics. Maps of trends in diabetes and obesity. Power Point Slides on Diabetes
There are four main tools to measure obesity: (1) body mass index (BMI), (2) waist-to-hip ratio (WHR)—showing a more precise correlation with the prevalence of diabetes (Tables 1, 2 [1]), (3) measurement of the waist circumference (WC) and (4) waist-to-height ratio (WHtR). A waist circumference of over 94 cm in men (37 in.) and 80 cm in women (31.5 in.) predicts a BMI greater than 25 with 96 % of specificity [13]. A systematic review and meta-analysis of studies involving more than 300,000 adults in several ethnic groups shows the superiority of WHtR over WC and BMI for distinguishing adults with hypertension, type 2 diabetes, dyslipidemia, metabolic syndrome and general cardiovascular outcomes [14, 15]. The distribution of fat is itself a critical determinant of insulin sensitivity. A more peripheral distribution of fat (subcutaneous tissue deposit) found in lean individuals is considered a normal adiposity and a physiological fat storage.
Adipocytes regulate fat mass, nutrient and energy homeostasis by releasing fatty acids in the circulation through the breakdown of triglycerides in exchange of glucose, when the latter is limited [3, 15]. In the presence of insulin resistance, the extra-energy is not channeled into insulin-sensitive subcutaneous adipose tissue, but rather into undesirable sites such as the liver, the heart and the skeletal muscle as a visceral adipose tissue, known as fat ectopic deposition [3, 15]. The consequences of this distorted distribution of fat are: visceral obesity, insulin resistance, atherogenic dyslipidemia and a prothrombotic inflammatory profile—the defining features of what is known as metabolic syndrome [3–5, 15].
Figure 4 shows the mechanism of how fat induces insulin resistance. Hypertrophied intra-abdominal adipocytes are characterized by a hyperlipolytic state that is resistant to the antilipolytic effect of insulin [3, 16]. Non-esterified fatty acids (NEFAs) are released in the circulation as a product of lipolysis. The increased flux to the liver and muscle will promote lipotoxicity with the corresponding consequences of altered insulin actions leading to insulin resistance and deterioration of glucose homeostasis.
Obesity and type 2 diabetes are both linked to insulin resistance, but for obesity and insulin resistance to be associated with type 2 diabetes another factor needs to be present—beta-cells dysfunction. In other words, beta-cells must be unable to fully compensate for decreased insulin sensitivity [2, 5].
Insulin resistance is manifested by hyperinsulinemia, increased glucose production in the liver and decreased glucose disposal. In the adipocytes, insulin triggers an increased release of hormone-sensitive lipase (HSL), resulting in an increase in NEFAs that can be delivered to the liver where they will have three destinies: (1) conversion into ATP in the mitochondria; (2) conversion back to triglycerides and incorporation into very-low-density lipoprotein (VLDL); and (3) storage. Also, the increased levels of glucose in the liver favor the conversion of the excess of glucose into fatty acids. The fatty acid synthesis, in turn, increases the levels of malonyl CoA, which then inhibits carnitine palmitoyltransferase 1 (CPT-1). Thus, blocking the transport of the fatty acids into the mitochondria, thereby increasing further the levels of triglycerides, ultimately released as VLDL [17].
A possible mechanism to explain the link between obesity, insulin resistance and type 2 diabetes could be what is depicted in Fig. 5 [5]. A crucial defect in the beta-cells reduces the amount of insulin secretion. In consequence, this signals the brain to increase food intake (hunger), which determines an increased need of insulin and to insulin resistance. The insulin-sensitive tissues such as liver, muscle and fat will increase the glucose production through activation of glycogenolysis and gluconeogenesis, and beta-oxidation of lipids and lipolysis, respectively. Consequently, the increased levels of NEFAs lead to an increase in the synthesis of triglycerides and eventually transformed them into VLDL or stored in the liver. Ultimately, this will promote dyslipidemias and cardiovascular disorders such as hypertension, angina and thrombosis.
Coffee consumption and bioactive components
Coffee is a complex mixture of chemical compounds, and its composition varies according to: (a) coffee bean species (Coffeea arabica and Coffea canephora var. robusta), (b) roasting process (speed, time and temperature) and brewing process (water-to-coffee grounds ratio, coffee grind size, water temperature, duration and methods) [18].
The composition of the green coffee includes, but not limited to: phenolic compounds, mainly chlorogenic acids or CGAs (6.5–10 %), carbohydrates (45–52 %), proteins (11 %), minerals (4.2–4.4 %), caffeine (1.2–2.2 %), trigonelline (0.7–1.0 %) and lipids (10–16 %) in special diterpenes such as cafestol and kahweol [19]. The roasted coffee has a somewhat different composition due to chemical transformations during the roasting process, which results in the development of its characteristic aroma, flavor and color [20]. The most important chemical transformations are: conversion of CGAs to 1–5 γ-quinolactones or quinides (CGLs), mainly 3- and 4-caffeoyl-1,5-quinides (3CQL and 4 CQL); and the formation of melanoidins by the combination of sugars and amino acids through the Maillard reaction of caramelization of carbohydrates [21, 22]. Consequently, roasted coffee is composed of carbohydrates (38–42 % dry basis), which are responsible for the ‘body’ of the coffee; melanoidins (23 %), responsible for the color of the coffee; and lipids (11–17 %), protein (10 %), minerals (4.5–4.7 %), CGAs (2.7–3.1 %), caffeine (1.3–2.4 %) as well as hundreds of volatile compounds that contribute to the coffee aroma [23]. The total CGA content in commercial ground roasted coffee ranges considerably, varying from 0.3 to 3.5/100 g. Decaffeination may increase or decrease the CGA content in about 10 %, depending on the method used for this purpose [18].
Caffeine
The development of T2DM in overweight patients (BMI > 25) is highly prevalent, and as a consequence, diet and exercise are always part of any antidiabetic treatment. Caffeine causes weight loss in patients with diabetes by increasing thermogenesis [24–29], which means increased production of energy (ATP); and by its ergogenic properties [30–34]. In other words, caffeine enhances endurance and exercise strength, by the ability to increase physical exercise without a concomitant increase in effort sensation.
Chronic caffeinated coffee consumption in a mouse model of obesity and T2DM demonstrated that equivalent doses of caffeine in the coffee administered to mice diminished weight gain in high-fat-diet-fed mice and abolished weight gain in normal-diet-fed mice [35].
Cafestol and Kahweol
Cafestol and kahweol are diterpenes from coffee that poorly pass the cellulose paper filter. A cup of unfiltered coffee has levels around 6–12 mg (French press and Turkish coffee), while a cup of filtered coffee contains only 0.2–0.6 mg of diterpenes. However, in vitro studies using small concentrations of cafestol (10−10 to 10−6 M) have shown a dual action: a significant increase in insulin secretion (insulinoma cells) and also in the glucose uptake (skeletal muscle cells), suggesting that cafestol may contribute, even in the low concentrations present in filtered coffee, to the preventive effects on T2DM in coffee drinkers [36].
Animal and in vitro studies indicate that cafestol and kahweol can operate by modulating multiple enzymes involved in the detoxification process of carcinogens responsible for hepatocellular carcinoma [37]. Different mechanisms appear to be involved in this chemoprotective effect: an induction of conjugating enzymes (e.g., glutathione S-transferases, glucuronosyl S-transferases), an increased expression of proteins involved in cellular antioxidant defense (e.g., gamma-glutamylcysteine synthetase and heme oxygenase-1) and an inhibition of the expression and/or activity of cytochromes P450 involved in carcinogen activation (e.g., CYP2C11, CYP3A2) [38–40].
Chlorogenic acids (CGAs)
Chlorogenic acids are the most common bioactive compounds in plant foods such as coffee, apple, tea and berries, as well as in beverages, such as wine [41]. Coffee is the major source of CGAs in the American diet. CGAs refer to a family of isomers with no chloride in the formula. CGAs are esters formed by the binding of quinic acid and trans-cinnamic acids (mainly caffeic, ferulic and p-coumaric acids). 5-Caffeoylquinic acid (5 CQA) also known as chlorogenic acid is the most abundant CGA in coffee [20, 42]. CGAs are partly absorbed in the small intestine [43] and partly in the large intestine after being metabolized by bacteria [44]. According to a study in rats, metabolites from coffee appear in the blood in two phases: 30 min to 2 h and then 8–12 h after coffee administration. This indicates that coffee bioactive compounds are initially absorbed in the stomach and small intestine (first phase) and further fermented by the gut microbiota and absorbed/excreted in the colon during the second phase [45–47]. It has been reported that around 90 % of the CGA from coffee would be available to reach gastrointestinal (GI) mucosa and suffer hydrolysis by esterases, conjugation or absorption in the free form. One-third of the CGAs is absorbed intestinally, and the remainder will be metabolized by colonic microflora into glucuronides and sulfates derivatives from caffeic acid and subsequently absorbed and distributed to the tissues (enterohepatic cycle) [48]. A more detailed description of CGAs’ fate in the human body can be found in Farah and Duarte [18].
Melanoidins
Coffee brew contains many polyphenols and phenolic compounds, well known for their antioxidant properties [49–51]. During the roasting process, antioxidants such as chlorogenic acids are partly decomposed or incorporated into melanoidins. The latter represents a heterogeneous group of polymers with a variable range of molecular weight. They have been proposed to impart antioxidant activity through an ability to chelate metal ions [52]. Recent studies [53] of the antiradical activity of roasted coffee arabica showed that the highest antiradical activity was associated with a low molecular weight fraction (<3 kD) of the coffee brew, suggesting a predominant role of phenolics non-bound to melanoidins. Lastly, it is important to mention the main by-product of coffee brewing, known as spent coffee, which is also a rich source of phenolic acids. Coffee companies produce annually >2 billion tons of spent grounds, most of which is disposed without recycling [54–56]. Several applications have been proposed for coffee by-products as a source of bioactive compounds such as antioxidant (food preservative), antitumor and antiallergic action [20].
Coffee consumption, gut microbiota, metabolomics profile versus obesity
Current research suggests that altered gut microbiota profile is associated with obesity and T2DM [45, 57]. Humans, rats and mice gut microbiota are made up of two main phylotypes—Bacterioidetes (B) and Firmicutes (F). There is some consistency within reports that obesity and high-fat feeding are associated with an abundance of Firmicutes as opposed to Bacteroidetes, when compared to lean individuals [45]. In vitro studies [58] using equivalent amount of CGA (80.8 mg) showed a significant increase in the growth of Bifidobacterium (B type), Clostridium coccoides–Eubacterium rectale group. Similar results were observed in a study in diet-induced obese rats under chronic use of coffee [45]. They showed that the gut microbiota change had positive impact on the serum metabolome resulting in: (a) decreased body weight, adiposity, liver triglycerides and energy intake; (b) increase in the metabolites indicative of carbohydrate and fatty acid metabolism. Coffee reduced some, but not all the detrimental effects of high-fat diet since they found coffee consumption to be associated with insulin resistance. The authors discussed that this resistance could be due to an antagonist effect of caffeine and suggest that future studies should examine the effect of caffeine and other coffee bioactive compounds independently.
Coffee and type 2 diabetes: possible mechanisms of preventive effect
There is a body of evidence through in vitro/ex vivo models, in vivo experiments and in clinical trials of a positive modulation of human health attributed to phenolic compounds or CGAs and caffeine [59]. Figure 6 summarizes the majority of mechanisms that explain the beneficial effects of regular coffee consumption associated with reduced risk of developing type 2 diabetes mellitus. White squares represent in vivo studies and black squares in vitro studies. The studies mentioned here were based on the administration of caffeinated, decaffeinated or simply coffee with no distinction between the two. Some of them involved administration of specific amounts of caffeine and/or chlorogenic acid. Therefore, the conclusions are in reference to effects of the two main components of coffee: chlorogenic acids and caffeine.
In this section, a summary of the latest data on those experiments is discussed. It is focused on the effects of GCAs on glucose and lipid metabolism, since the possible mechanisms to explain the preventive effect of coffee on the development of obesity and T2DM are related to both pathways. It is of note that some of the mechanisms proposed for coffee effects on diabetes are shared with actual drugs currently used to treat T2DM and disorders of the lipid metabolism. Examples of those drugs are inside the parenthesis aside of the corresponding mechanism in Fig. 6.
CGAs and glucose metabolism
Several mechanisms have been proposed for the effects of CGAs on the metabolism of glucose. As depicted in Fig. 6, we can divide those studies into the three different tissue groups: GI (absorption of glucose); skeletal muscle, liver and adipose tissue (main sites of glucose storage); and pancreas (hormonal regulation of glucose metabolism).
The effects of CGAs on glucose absorption are evidenced by: (1) inhibition of α-amylase, enzyme responsible for the breakdown of starch present in the saliva and pancreatic juice inhibiting sugar absorption from the dietary starch [60, 61]; (2) preventing the action of alpha-1, 4-glucosidase, enzyme responsible for the degradation of glycogen (glucose storage form) present on the brush border cells of the small intestine [62, 63]; (3) modulation of gastrointestinal peptides such as gastric inhibitory polypeptide (GIP) and glucagon-like peptide 1 (GLP-1) (incretin hormones with opposing effects on glucose absorption), shifting glucose absorption to a more distal region in the GI tract [62, 64]; (4) stimulation of the translocation of glucose transporter 4 (GLUT4), increasing glucose uptake by the peripheral tissues [62, 65]; (5) glucose-6-phosphatase (Glu-6-Pase) inhibition, enzyme responsible for hydrolyzing the phosphate from glucose-6-phosphate releasing free glucose into the systemic circulation. In consequence, there will be a reduction in the levels of glucose in the blood [62, 66, 67]; (6) upregulation of TCA and urea cycles, promoting a metabolic shift and causing increased ATP turnover [68]; and (7) mitigation of insulin resistance by decreasing plasma glucose levels and increasing tyrosine phosphorylation of insulin receptor substrate-1 (IRS-1) [66].
CGAs and Lipid Metabolism
The effects of the CGAs in the lipid metabolism are also depicted in Fig. 6. The first mechanism involves the downregulation of sterol regulatory element-binding protein (SREBP)-1C. The mRNA levels of this protein in the mouse liver were significantly lower in coffee (poly) phenols (CPP) or CPP-fed mice than in high-fat control mice. These findings indicate that CPP enhance energy metabolism and reduce lipogenesis by downregulating SREBP-1c and related molecules, which leads to the suppression of body fat accumulation [69, 70]. SREBP-1c is the main genetic switch controlling lipogenesis. Omega-3 fatty acids (fish oil) elicit hypotriglyceridemic effects in part by coordinately suppressing hepatic lipogenesis through reducing levels of SREBP-1c in the liver [71, 72]. This is another example of CGAs preventive effect on type 2 diabetes that share the same mechanism with the current therapy in the treatment of obesity, type 2 diabetes and metabolic disorder.
The next two mechanisms depicted in Fig. 6 are well known by their application in the treatment of dyslipidemias. Fibrates’ mechanism of action is primarily as a ligand for the nuclear transcription receptor peroxisome proliferator-activated receptor alpha (PPAR-α) [73]. This receptor when activated acts as a lipid sensor and regulates lipid metabolism. The liver is its major target tissue, and its key genes are enzymes involved in the β-oxidation of fatty acid [74]. CGA’s and caffeic acid stimulated the expression of PPAR-α in high-fat diet-induced obese mice, showing antiobesity property by improving lipid metabolism [74]. The same paper from Ae-Sim Cho et al. looked at the activities of hepatic lipid-regulating enzymes, such as 3-hydroxy-3-methylglutaryl coenzyme A reductase (HMG-Co-A reductase) and fatty acid synthase (FAS). They found an inhibitory effect of those enzymes in the group of mice fed with caffeic acid and chlorogenic acid. They concluded that CGA and caffeic acid were inhibitors of fatty acid and cholesterol synthesis as well as stimulants of fatty acid oxidation in the liver, the same mechanism of action of statins.
Carnitine palmitoyltransferase (CPT) is a rate-limiting enzyme that catalyzes the transport of fatty acids to the mitochondria for β-oxidation. A study in mice fed with green bean coffee extract showed that neochlorogenic acid or 5-O-caffeoylquinic acid (5-CQA) and feruloylquinic acid mixture, members of the CGAs family present in the coffee extract, can enhance hepatic CPT activity [75]. This positive effect of coffee to increase lipid beta-oxidation is in addition to the effect of coffee on another protein, PPAR-α, which is also upregulated by CGAs and acts as a transcriptional factor upregulating the expression of CPT [76].
A study that included 16 subjects exhibiting pre-obesity levels (BMI between 25 and 30), euthyroid, non-diabetic, non-hypertensive and not receiving steroids between ages of 22–46 was targeting the effects of high CGA green coffee extract (350 mg CGA 3xday) on body fat accumulation and weight loss [61]. They found that out of 16 initially classified as overweight, six finished the study in the normal BMI category and 10 out of 16 showed at least 10 % weight loss. They concluded that, compared with the currently approved treatment for weight loss, such as sibutramine, orlistat and rimonabant, CGA green coffee bean extract has effects superior of the prescription drugs.
An animal study in mice aimed to investigate the effect of CGAs and caffeine present in green coffee extract on fat accumulation and body weight [75]. The results showed that after 14 days consuming green coffee bean extract (10 % caffeine and 26 % of CGA) caused a suppressive effect on weight gain and visceral fat accumulation in mice.
As a result from the previous mechanisms of CGAs on the lipid metabolism, there will be an increase in fatty acid oxidation due to an upregulation of PPAR-α and a reduction in synthesis of fatty acid, due to inhibition of HMG-Co-A reductase and FAS enzymes in the liver as displayed in Fig. 6.
There are, though, a couple of theories that try to embrace the majority of the effects seen with coffee, the adenosine monophosphate kinase (AMPK) activation theory and the sex-hormone-binding globulin (SHBG) theory.
AMPK theory
AMPK is a heterotrimeric enzyme, composed of one active subunit alpha and two regulatory subunits beta and gamma. The change in the ratio AMP/ATP triggers its activation that consists in phosphorylation of residue Trh172 of the α-subunit rescuing the energy balance. As a result of AMPK activation, the cellular metabolism switches from anabolic to catabolic processes [77]. This kinase is a main point for metabolic control in all eukaryotes with vital functions in several organs and tissues (Fig. 7) [77–83]. Considering AMPK’s pivotal role in the control of carbohydrate, lipid and protein homeostasis, it is considered a key player in various diseases such as obesity, type 2 diabetes, dyslipidemias, just to mention a few [77, 84–87].
SHBG theory
Sex-hormone-binding globulin (SHBG) has been associated with type 2 diabetes, metabolic syndrome and hormone-dependent cancers. Goto et col. [88] studied the correlation of levels of SHBG and the use of estrogen with body mass index and lifestyle factors such as physical activity, smoking, alcohol consumption coffee intake and dietary factors in a population of 13,547 postmenopausal women who were enrolled in the Women’s Health Initiative Study between 1993 and 1998 in 40 centers in the USA. A self-administered food frequency questionnaire was applied to estimate average daily dietary intake over the previous 3-month period. The lifestyle factors included, beside others mentioned above are: the intake of coffee, decaffeinated coffee and tea. The results showed that higher regular coffee intake (≥2 cups per day compared with no cups of coffee per day), but not decaffeinated coffee or tea, was associated with higher SHBG concentration. The same positive relationship with SHBG levels was found for physical activity and negative relationship with BMI. Previous studies on SHBG effects [89] had shown that increased BMI, waist circumference and hip circumference were associated with increased levels of estrone, estradiol and free estradiol and negatively associated with SHBG. They concluded that there is a consistent and significant (p ≤ 0.05) association between adiposity and elevated concentrations of estrogens and androgens, as well as between increased physical activity and decreased concentration of these hormones. These indications suggest that these hormones can be modified by lifestyle changes.
The suggested molecular mechanism for the positive relationship between caffeinated coffee and SHBG levels could be based on the fact that SHBG is primarily synthesized and metabolized in the liver, where coffee is known to present components such as caffeine, cafestol and kahweol that alter enzyme activity and expression in the liver [90]. Also the fact that a recent study [91] concluded that caffeinated coffee and caffeine intakes, but not with decaffeinated coffee, were positively associated with SHBG levels. Nevertheless, this theory needs further experimental investigation.
Other coffee constituents and effects on glucose metabolism
Coffee is also rich in trigonelline, a pyridine alkaloid derived from the methylation of nicotinic acid or niacin. Trigonelline represents 1 % of the dry weight of roasted coffee beans [92–94] and 50–100 mg of a cup of coffee [95, 96]. The administration of trigonelline to a rat model of diabetes mellitus resulted in reduced glucose levels in a tolerance glucose test [97], and similar results from other animal studies showed that trigonelline exerts a hypoglycemic effect [95, 98]. In addition, it was also reported beneficial effects in rats displaying peripheral neuropathy [99]. It was found in animal studies, which could be added to the overall effect of coffee. Trigonelline regulates key enzymes of glucose and lipid metabolism, such as glucokinase, glucose-6-phosphatase, fatty acid synthase and carnitine palmitoyltransferase in diabetics rats [94, 100], which could explain the effects of trigonelline on diabetes. In addition, niacin, its parent molecule, is indicated in the treatment of dyslipidemias due to its inhibition of VLDL secretion and consequent decreased production of LDL and triglycerides [73].
Among the minerals present in coffee, magnesium contributes with 7 mg/cup of the American coffee, according to the nutritional tables of the US Department of Agriculture [95]. Magnesium displayed in many studies a positive effect on glucose metabolism by increasing insulin sensitivity [94, 95, 101]. Magnesium acts as a cofactor of various enzymes involved in the metabolism of glucose [62, 102], possibly playing a role in glucose homeostasis and in the prevention of T2DM [62, 103, 104].
Other possible mechanisms
One of the first effects of coffee to be noticed and maybe the only one explored by pharmaceutical industry is the antioxidant property of the chlorogenic acids and other cinnamates present in the coffee, making coffee the main source of those antioxidants in American diet [105]. The antioxidative property could also contribute to the overall effect of coffee in the prevention of diabetes, considering that oxidative stress plays a role in the development of insulin resistance and T2DM [67, 106, 107]. There are other studies that interpret this effect of coffee as an indirect rather direct effect on our own endogenous antioxidant defenses through an increase in glutathione and GST activity [94].
The white adipose tissue, as opposed to the brown one, is involved in energy homeostasis and energy control. It plays a key role by secreting various biomolecules called adipokines or adipocytokines [108]. Adiponectin is the most abundant peptide secreted by the adipocytes, and its actions are mediated by two main receptors: AdipoR1, involved in the stimulation of AMPK in the muscle, and AdipoR2, involved with PPAR-γ in the liver. Those two receptors mediate an increased fatty acid oxidation in the liver and glucose uptake by the muscle [109, 110]. Serum adiponectin levels are inversely related to body fat mass and to the degree of insulin resistance, and therefore, it is accepted that adiponectin ameliorates sensitivity to insulin and glucose tolerance [109, 111]. Chlorogenic acid and caffeic acid supplemented diet on high-fat diet-induced obese mice lowered plasma triglycerides and total cholesterol and chlorogenic acids supplementation significantly increased the plasma adiponectin levels [74]. A review article on the mechanisms of adiponectin as a target for metabolic syndrome, diabetes and coronary diseases concluded that considering that the levels of adiponectin are consistently inversely related to these ailments, the search for pharmacologic agents that could improve its plasma levels should be target of intense research [109].
Coffee and type 2 diabetes: epidemiological evidence of preventive effect
Innumerous reports from epidemiological studies have been published claiming that regular coffee intake, caffeinated or decaffeinated, averaging 3–4 cups a day, reduces significantly the risk of developing T2DM [67, 91, 112–119]. There are some reports, though, that their findings are not conclusive or fail to show a significant correlation [120]. A review article on epidemiological studies of the association between habitual coffee consumption and diabetes risk, healthy glucose metabolism or both, concluded that only three of the 20 studies did not find a protective effect and none found a deleterious effect [121]. They also found that the majority of the studies suggest that long-term consumption of coffee and decaffeinated coffee can reduce the risk of diabetes. This implies that there are some evidences that one or more non-caffeine constituents in coffee or both may be better suited for enhancing glucose tolerance and insulin sensitivity than in caffeinated coffee.
A more recent review on the role of coffee in modulating diabetes risk [95] researched the number of publications between 1950 and 2010 in Medline tagging the words of coffee and diabetes and showed that the first paper was published in 1970s [122] and the first epidemiological report on inverse association between coffee consumption and risk of T2DM came only in 2002 [112]. Since then, the author says the number of studies has increased exponentially and by the time it was published they found 437 articles (PubMed, February 17, 2012). The same search today yield 651 articles (PubMed, February 5, 2016).
Discussion
The estimated contents of the bioactive compounds of coffee in the majority of the studies are based on the average amount value cited in the literature. Nevertheless, a review article from Crozier et al. [123] claims that there is a great variation in batch-to-batch coffee bean composition, probably due to the usual blending of two different species of coffee, arabica and robusta beans, and the roasting, grinding and coffee making/barista processes. Very few studies predetermine the amount of CGAs and/or caffeine in the coffee administered or consumed during the study. Additionally, the use of ‘one cup’ as a measure of the volume of coffee cannot be considered as a reproducible measure, since the size of the cup varied among studies and among coffee drinkers within the study populations [94]. Zanotti et al. [41] discuss that most of the in vitro studies currently published presents data obtained from exposure to coffee constituents in their natural form occurring in the plant food. It constitutes a significant bias since they do not consider the fast modification of those chemicals by human and microbial enzymes into metabolites after ingestion. Overall, it exempts the derivatives and metabolites of coffee bioactive compounds to be at least partially responsible for the observed beneficial/toxic effects [41, 43, 124, 125]. It can get even more complicated, if we consider that the lack of commercial availability of different isoforms of CQAs (3- and 4-CQA) and quinolactones or quinides (3- and 4-CQL), which are predominant in the coffee brew, as well as standards for sulfated and glucuronidated forms of the CGAs and derivatives are also unavailable. ([18, 105, 123]. Therefore, all these factors are certainly weaknesses of most of the current studies on coffee consumption. However, at the same time they also explain why there is so limited literature available on the disposition of those plant-derived compounds in the human body, healthy or diseased. Consequently, it was not yet possible to determine the therapeutic concentrations of those bioactive compounds or in which amount they should be present in coffee to promote health benefits. They concluded that future in vitro studies should target the cellular activity of their principal metabolites through bioavailability studies. In a most recent review [94], Crozier et al. conclude that a large part of the conflict in the epidemiological studies is because research has not specifically focused, during the design stage, on the beverages, so that the level of detail collected in the surveys is inadequate to quantify and characterize long-term consumption.
Conclusion
The pathophysiological mechanisms involved in obesity and development of type 2 diabetes are very complex and overlay with metabolism of three major nutrients: carbohydrates, lipids and proteins. The two first ones being more closely interrelated considering that carbohydrates is our number one source of energy and lipids the way we storage energy in our body. A multitude of mechanisms is proposed to account for the beneficial effects of coffee consumption on the development of obesity and T2DM. Some theories, such as the theory of the activation of AMPK, in which AMPK works as a switch between anabolism (ATP expenditure) and catabolism (ATP production), sound very comprehensive.
In conclusion, coffee has a complex chemical composition that fluctuates according a range of factors (type of beans, blend, roasting, grounding, brewing). After ingestion, coffee constituents go through biotransformations that occur during their disposition in the human body (absorption, metabolization and enterohepatic cycling), which there is little information about the possible effects of the metabolites. Studies investigating the bioavailability, metabolism and bioactivity of the different compounds present/produced in the coffee are urgently needed. As of today, there is mounting evidence of the reduced risk of developing type 2 diabetes by regular coffee drinkers of 3–4 cups a day. The effects are likely due to the presence of chlorogenic acids and caffeine, the two constituents of coffee in higher concentration after the roasting process.
References
Leong KS, Wilding JP (1999) Obesity and diabetes. Bailliere’s Best Pract Res Clin Endocrinol Metab 13(2):221–237
Bailey CJ (2011) The challenge of managing coexistent type 2 diabetes and obesity. BMJ 342:d1996. doi:10.1136/bmj.d1996
Despres JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444(7121):881–887. doi:10.1038/nature05488
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444(7121):860–867. doi:10.1038/nature05485
Kahn SE, Hull RL, Utzschneider KM (2006) Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444(7121):840–846. doi:10.1038/nature05482
Larsson B, Svardsudd K, Welin L, Wilhelmsen L, Bjorntorp P, Tibblin G (1984) Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913. Br Med J (Clin Res Ed) 288(6428):1401–1404
Astrup A, Finer N (2000) Redefining type 2 diabetes: ‘diabesity’ or ‘obesity dependent diabetes mellitus’? Obes 1(2):57–59
Pincock S (2006) Paul Zimmet: fighting the “diabesity” pandemic. Lancet 368(9548):1643. doi:10.1016/S0140-6736(06)69682-7
Zimmet P, Alberti KG, Shaw J (2001) Global and societal implications of the diabetes epidemic. Nature 414(6865):782–787. doi:10.1038/414782a
International Diabetes F (2013) IDF Atlas 6th edition. Paper presented at the Sixty-Six World Health Assembly
International Diabetes F (2013) IDF Atlas, 6th edn. IDF, Brussels, Belgium
CDC, System NDS (2012) The diabetes report card 2012. www.cdc.gov/diabetes/statistics
Han TS, van Leer EM, Seidell JC, Lean ME (1995) Waist circumference action levels in the identification of cardiovascular risk factors: prevalence study in a random sample. BMJ 311(7017):1401–1405
Ashwell M, Gunn P, Gibson S (2012) Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev 13(3):275–286. doi:10.1111/j.1467-789X.2011.00952.x
Savva SC, Lamnisos D, Kafatos AG (2013) Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes Metab Syndr Obes Targets Ther 6:403–419. doi:10.2147/DMSO.S34220
Galgani JE, Moro C, Ravussin E (2008) Metabolic flexibility and insulin resistance. Am J Physiol Endocrinol Metab 295(5):E1009–E1017. doi:10.1152/ajpendo.90558.2008
Elkaim Y News studies confirm the surprising relationship between sugar, insulin resistance and heart disease (2011). http://www.supernutritionacademy.com/sugar-insulin-resistance-and-heart-disease/. Accessed 8 Aug 2015
Farah A, Duarte G (2015) Bioavailability and metabolism of chlorogenic acids from coffee. In: Preedy VR (ed) Coffee in health and disease prevention. Elsevier, New York
Santos RML (2009) An unashamed defense of coffee: 101 reasons to drink coffee without guilt. XLibris, USA
Esquivel P, Jimenez VM (2012) Functional properties of coffee and coffee by-products. Food Res Intern 46:488–495
Bekedam EK, Schols HA, Cammerer B, Kroh LW, van Boekel MA, Smit G (2008) Electron spin resonance (ESR) studies on the formation of roasting-induced antioxidative structures in coffee brews at different degrees of roast. J Agric Food Chem 56(12):4597–4604. doi:10.1021/jf8004004
del Castillo MD, Ames JM, Gordon MH (2002) Effect of roasting on the antioxidant activity of coffee brews. J Agric Food Chem 50(13):3698–3703
Rivera J (2014) Unlocking coffee’s chemical composition Part I and II. http://www.coffeechemistry.com. Accessed 15 Dec 2015
Astrup A, Toubro S, Cannon S, Hein P, Breum L, Madsen J (1990) Caffeine: a double-blind, placebo-controlled study of its thermogenic, metabolic, and cardiovascular effects in healthy volunteers. Am J Clin Nutr 51(5):759–767
Goldstein E, Jacobs PL, Whitehurst M, Penhollow T, Antonio J (2010) Caffeine enhances upper body strength in resistance-trained women. J Int Soc Sports Nutr 7:18. doi:10.1186/1550-2783-7-18
Arciero PJ, Bougopoulos CL, Nindl BC, Benowitz NL (2000) Influence of age on the thermic response to caffeine in women. Metab Clin Exp 49(1):101–107
Astrup A, Toubro S (1993) Thermogenic, metabolic, and cardiovascular responses to ephedrine and caffeine in man. Int J Obes Relat Metab Disord J Int Assoc Study Obes 17(Suppl 1):S41–S43
Dulloo AG, Duret C, Rohrer D, Girardier L, Mensi N, Fathi M, Chantre P, Vandermander J (1999) Efficacy of a green tea extract rich in catechin polyphenols and caffeine in increasing 24-h energy expenditure and fat oxidation in humans. Am J Clin Nutr 70(6):1040–1045
Greenberg JA, Axen KV, Schnoll R, Boozer CN (2005) Coffee, tea and diabetes: the role of weight loss and caffeine. Int J Obes (Lond) 29(9):1121–1129. doi:10.1038/sj.ijo.0802999
Paluska SA (2003) Caffeine and exercise. Curr Sports Med Rep 2(4):213–219
Graham TE (2001) Caffeine, coffee and ephedrine: impact on exercise performance and metabolism. Can J Appl Physiol Revue canadienne de physiologie appliquee 26(Suppl):S103–S119
Magkos F, Kavouras SA (2005) Caffeine use in sports, pharmacokinetics in man, and cellular mechanisms of action. Crit Rev Food Sci Nutr 45(7–8):535–562. doi:10.1080/1040-830491379245
Nehlig A, Debry G (1994) Caffeine and sports activity: a review. Int J Sports Med 15(5):215–223. doi:10.1055/s-2007-1021049
Spriet LL (1995) Caffeine and performance. Int J Sport Nutr 5(Suppl):S84–S99
Rustenbeck I, Lier-Glaubitz V, Willenborg M, Eggert F, Engelhardt U, Jorns A (2014) Effect of chronic coffee consumption on weight gain and glycaemia in a mouse model of obesity and type 2 diabetes. Nutr Diabetes 4:e123. doi:10.1038/nutd.2014.19
Mellbye FB, Jeppesen PB, Hermansen K, Gregersen S (2015) Cafestol, a bioactive substance in coffee, stimulates insulin secretion and increases glucose uptake in muscle cells: studies in vitro. J Nat Prod 78(10):2447–2451. doi:10.1021/acs.jnatprod.5b00481
Morisco F, Lembo V, Mazzone G, Camera S, Caporaso N (2014) Coffee and liver health. J Clin Gastroenterol 48(Suppl 1):S87–S90. doi:10.1097/MCG.0000000000000240
Cavin C, Holzhaeuser D, Scharf G, Constable A, Huber WW, Schilter B (2002) Cafestol and kahweol, two coffee specific diterpenes with anticarcinogenic activity. Food Chem Toxicol Int J Publ Br Ind Biol Res Assoc 40(8):1155–1163
Cavin C, Mace K, Offord EA, Schilter B (2001) Protective effects of coffee diterpenes against aflatoxin B1-induced genotoxicity: mechanisms in rat and human cells. Food Chem Toxicol Int J Publ Br Ind Biol Res Assoc 39(6):549–556
Gross-Steinmeyer K, Eaton DL (2012) Dietary modulation of the biotransformation and genotoxicity of aflatoxin B(1). Toxicology 299(2–3):69–79. doi:10.1016/j.tox.2012.05.016
Zanotti I, Dall’Asta M, Mena P, Mele L, Bruni R, Ray S, Del Rio D (2015) Atheroprotective effects of (poly)phenols: a focus on cell cholesterol metabolism. Food Funct 6(1):13–31. doi:10.1039/c4fo00670d
Tresserra-Rimbau A, Medina-Remon A, Estruch R, Lamuela-Raventos RM (2015) Coffee polyphenols and high cardiovascular risk parameters. In: Preedy VR (ed) Coffee in health and disease prevention. Elsevier Inc., New York, pp 387–394
Olthof MR, Hollman PC, Katan MB (2001) Chlorogenic acid and caffeic acid are absorbed in humans. J Nutr 131(1):66–71
Olthof MR, Hollman PC, Buijsman MN, van Amelsvoort JM, Katan MB (2003) Chlorogenic acid, quercetin-3-rutinoside and black tea phenols are extensively metabolized in humans. J Nutr 133(6):1806–1814
Cowan TE, Palmnas MS, Yang J, Bomhof MR, Ardell KL, Reimer RA, Vogel HJ, Shearer J (2014) Chronic coffee consumption in the diet-induced obese rat: impact on gut microbiota and serum metabolomics. J Nutr Biochem 25(4):489–495. doi:10.1016/j.jnutbio.2013.12.009
Lafay S, Gil-Izquierdo A, Manach C, Morand C, Besson C, Scalbert A (2006) Chlorogenic acid is absorbed in its intact form in the stomach of rats. J Nutr 136(5):1192–1197
Redeuil K, Smarrito-Menozzi C, Guy P, Rezzi S, Dionisi F, Williamson G, Nagy K, Renouf M (2011) Identification of novel circulating coffee metabolites in human plasma by liquid chromatography-mass spectrometry. J Chromatogr A 1218(29):4678–4688. doi:10.1016/j.chroma.2011.05.050
Fumeaux R, Menozzi-Smarrito C, Stalmach A, Munari C, Kraehenbuehl K, Steiling H, Crozier A, Williamson G, Barron D (2010) First synthesis, characterization, and evidence for the presence of hydroxycinnamic acid sulfate and glucuronide conjugates in human biological fluids as a result of coffee consumption. Org Biomol Chem 8(22):5199–5211. doi:10.1039/c0ob00137f
Natella F, Nardini M, Giannetti I, Dattilo C, Scaccini C (2002) Coffee drinking influences plasma antioxidant capacity in humans. J Agric Food Chem 50(21):6211–6216
Serafini M, Testa MF (2009) Redox ingredients for oxidative stress prevention: the unexplored potentiality of coffee. Clin Dermatol 27(2):225–229. doi:10.1016/j.clindermatol.2008.04.007
Svilaas A, Sakhi AK, Andersen LF, Svilaas T, Strom EC, Jacobs DR Jr, Ose L, Blomhoff R (2004) Intakes of antioxidants in coffee, wine, and vegetables are correlated with plasma carotenoids in humans. J Nutr 134(3):562–567
Wang H-Y, Quian H, Yao W-R (2011) Melanoidins produced by the Maillard reaction: structure and biological activity. Food Chem 128:573–584
Troup GJ, Navarini L, Suggi Liverani F, Drew SC (2015) Stable radical content and anti-radical activity of roasted Arabica coffee: from in-tact bean to coffee brew. PLoS ONE 10(4):e0122834. doi:10.1371/journal.pone.0122834
Jimenez-Zamora A, Pastoriza S, Rufian-Henares J (2015) Revalorization of Coffee Byproducts. LWT Food Sci Technol 61:12–18
Cruz R, Mendes E, Torrinha A, Morais S, Pereira JA, Baptista P, Casal S (2014) Revalorization of spent coffee residues by direct agronomic approach. Food Res Int 73:190–196
Monente C, Ludwig IA, Irigoyen A, De Pena MP, Cid C (2015) Assessment of total (free and bound) phenolic compounds in spent coffee extracts. J Agric Food Chem 63(17):4327–4334. doi:10.1021/acs.jafc.5b01619
Backhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, Semenkovich CF, Gordon JI (2004) The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci USA 101(44):15718–15723. doi:10.1073/pnas.0407076101
Mills CE, Tzounis X, Oruna-Concha MJ, Mottram DS, Gibson GR, Spencer JP (2015) In vitro colonic metabolism of coffee and chlorogenic acid results in selective changes in human faecal microbiota growth. Br J Nutr 113(8):1220–1227. doi:10.1017/S0007114514003948
Del Rio D, Rodriguez-Mateos A, Spencer JP, Tognolini M, Borges G, Crozier A (2013) Dietary (poly)phenolics in human health: structures, bioavailability, and evidence of protective effects against chronic diseases. Antioxid Redox Signal 18(14):1818–1892. doi:10.1089/ars.2012.4581
Narita Y, Inouye K (2009) Kinetic analysis and mechanism on the inhibition of chlorogenic acid and its components against porcine pancreas alpha-amylase isozymes I and II. J Agric Food Chem 57(19):9218–9225. doi:10.1021/jf9017383
Vinson JA, Burnham BR, Nagendran MV (2012) Randomized, double-blind, placebo-controlled, linear dose, crossover study to evaluate the efficacy and safety of a green coffee bean extract in overweight subjects. Diabetes Metab Syndr Obes Targets Ther 5:21–27. doi:10.2147/DMSO.S27665
Akash MS, Rehman K, Chen S (2014) Effects of coffee on type 2 diabetes mellitus. Nutrition 30(7–8):755–763. doi:10.1016/j.nut.2013.11.020
Matsui T, Ueda T, Oki T, Sugita K, Terahara N, Matsumoto K (2001) alpha-Glucosidase inhibitory action of natural acylated anthocyanins. 1. Survey of natural pigments with potent inhibitory activity. J Agric Food Chem 49(4):1948–1951
Johnston KL, Clifford MN, Morgan LM (2003) Coffee acutely modifies gastrointestinal hormone secretion and glucose tolerance in humans: glycemic effects of chlorogenic acid and caffeine. Am J Clin Nutr 78(4):728–733
Song SJ, Choi S, Park T (2014) Decaffeinated green coffee bean extract attenuates diet-induced obesity and insulin resistance in mice. Evid Based Complement Altern Med 2014:718379. doi:10.1155/2014/718379
Jia H, Aw W, Egashira K, Takahashi S, Aoyama S, Saito K, Kishimoto Y, Kato H (2014) Coffee intake mitigated inflammation and obesity-induced insulin resistance in skeletal muscle of high-fat diet-induced obese mice. Genes Nutr 9(3):389. doi:10.1007/s12263-014-0389-3
van Dam RM (2006) Coffee and type 2 diabetes: from beans to beta-cells. Nut Metab Cardiovasc Dis 16(1):69–77. doi:10.1016/j.numecd.2005.10.003
Takahashi S, Saito K, Jia H, Kato H (2014) An integrated multi-omics study revealed metabolic alterations underlying the effects of coffee consumption. PLoS ONE 9(3):e91134. doi:10.1371/journal.pone.0091134
Fukushima Y, Kasuga M, Nakao K, Shimomura I, Matsuzawa Y (2009) Effects of coffee on inflammatory cytokine gene expression in mice fed high-fat diets. J Agric Food Chem 57(23):11100–11105. doi:10.1021/jf901278u
Murase T, Misawa K, Minegishi Y, Aoki M, Ominami H, Suzuki Y, Shibuya Y, Hase T (2011) Coffee polyphenols suppress diet-induced body fat accumulation by downregulating SREBP-1c and related molecules in C57BL/6 J mice. Am J Physiol Endocrinol Metab 300(1):E122–E133. doi:10.1152/ajpendo.00441.2010
Davidson MH (2006) Mechanisms for the hypotriglyceridemic effect of marine omega-3 fatty acids. Am J Cardiol 98(4A):27i–33i. doi:10.1016/j.amjcard.2005.12.024
Kim HJ, Takahashi M, Ezaki O (1999) Fish oil feeding decreases mature sterol regulatory element-binding protein 1 (SREBP-1) by down-regulation of SREBP-1c mRNA in mouse liver. A possible mechanism for down-regulation of lipogenic enzyme mRNAs. J Biol Chem 274(36):25892–25898
Malloy MJ, Kane JP (2015) Agents used in dyslipidemia. In: Katzung BG, Trevor AJ (eds) Basic and clinical pharmacology, 13th edn. McGraw Hill, United States
Cho AS, Jeon SM, Kim MJ, Yeo J, Seo KI, Choi MS, Lee MK (2010) Chlorogenic acid exhibits anti-obesity property and improves lipid metabolism in high-fat diet-induced-obese mice. Food Chem Toxicol Int J Publ Br Ind Biol Res Assoc 48(3):937–943. doi:10.1016/j.fct.2010.01.003
Shimoda H, Seki E, Aitani M (2006) Inhibitory effect of green coffee bean extract on fat accumulation and body weight gain in mice. BMC Complement Altern Med 6:9. doi:10.1186/1472-6882-6-9
Yamauchi R, Kobayashi M, Matsuda Y, Ojika M, Shigeoka S, Yamamoto Y, Tou Y, Inoue T, Katagiri T, Murai A, Horio F (2010) Coffee and caffeine ameliorate hyperglycemia, fatty liver, and inflammatory adipocytokine expression in spontaneously diabetic KK-Ay mice. J Agric Food Chem 58(9):5597–5603. doi:10.1021/jf904062c
Kodiha M, Stochaj U (2011) Targeting AMPK for therapeutic intervention in type 2 diabetes. Medical complications of type 2 diabetes, vol 1. InTech Europe, Croatia
Hardie DG (2008) AMPK: a key regulator of energy balance in the single cell and the whole organism. Int J Obes (Lond) 32(Suppl 4):S7–S12. doi:10.1038/ijo.2008.116
Kim AS, Miller EJ, Young LH (2009) AMP-activated protein kinase: a core signalling pathway in the heart. Acta Physiol (Oxf) 196(1):37–53. doi:10.1111/j.1748-1716.2009.01978.x
Lopaschuk GD (2008) AMP-activated protein kinase control of energy metabolism in the ischemic heart. Int J Obes (Lond) 32(Suppl 4):S29–S35. doi:10.1038/ijo.2008.120
Ronnett GV, Ramamurthy S, Kleman AM, Landree LE, Aja S (2009) AMPK in the brain: its roles in energy balance and neuroprotection. J Neurochem 109(Suppl 1):17–23. doi:10.1111/j.1471-4159.2009.05916.x
Steinberg GR, Kemp BE (2009) AMPK in health and disease. Physiol Rev 89(3):1025–1078. doi:10.1152/physrev.00011.2008
Zhang BB, Zhou G, Li C (2009) AMPK: an emerging drug target for diabetes and the metabolic syndrome. Cell Metab 9(5):407–416. doi:10.1016/j.cmet.2009.03.012
Fogarty S (1804) Hardie DG (2010) Development of protein kinase activators: AMPK as a target in metabolic disorders and cancer. Biochim Biophys Acta 3:581–591. doi:10.1016/j.bbapap.2009.09.012
Lage R, Dieguez C, Vidal-Puig A, Lopez M (2008) AMPK: a metabolic gauge regulating whole-body energy homeostasis. Trends Mol Med 14(12):539–549. doi:10.1016/j.molmed.2008.09.007
Towler MC, Hardie DG (2007) AMP-activated protein kinase in metabolic control and insulin signaling. Circ Res 100(3):328–341. doi:10.1161/01.RES.0000256090.42690.05
Viollet B, Lantier L, Devin-Leclerc J, Hebrard S, Amouyal C, Mounier R, Foretz M, Andreelli F (2009) Targeting the AMPK pathway for the treatment of type 2 diabetes. Front Biosci (Landmark Ed) 14:3380–3400
Goto A, Chen BH, Song Y, Cauley J, Cummings SR, Farhat GN, Gunter M, Van Horn L, Howard BV, Jackson R, Lee J, Rexrode KM, Liu S (2014) Age, body mass, usage of exogenous estrogen, and lifestyle factors in relation to circulating sex hormone-binding globulin concentrations in postmenopausal women. Clin Chem 60(1):174–185. doi:10.1373/clinchem.2013.207217
McTiernan A, Wu L, Chen C, Chlebowski R, Mossavar-Rahmani Y, Modugno F, Perri MG, Stanczyk FZ, Van Horn L, Wang CY (2006) Relation of BMI and physical activity to sex hormones in postmenopausal women. Obesity (Silver Spring) 14(9):1662–1677. doi:10.1038/oby.2006.191
Anderson DC (1974) Sex-hormone-binding globulin. Clin Endocrinol 3(1):69–96
Goto A, Song Y, Chen BH, Manson JE, Buring JE, Liu S (2011) Coffee and caffeine consumption in relation to sex hormone-binding globulin and risk of type 2 diabetes in postmenopausal women. Diabetes 60(1):269–275. doi:10.2337/db10-1193
Slow S, Miller WE, McGregor DO, Lee MB, Lever M, George PM, Chambers ST (2004) Trigonelline is not responsible for the acute increase in plasma homocysteine following ingestion of instant coffee. Eur J Clin Nutr 58(9):1253–1256. doi:10.1038/sj.ejcn.1601957
Wu X, Skog K, Jagerstad M (1997) Trigonelline, a naturally occurring constituent of green coffee beans behind the mutagenic activity of roasted coffee? Mutat Res 391(3):171–177
Ludwig IA, Clifford MN, Lean ME, Ashihara H, Crozier A (2014) Coffee: biochemistry and potential impact on health. Food Funct 5(8):1695–1717. doi:10.1039/c4fo00042k
Natella F, Scaccini C (2012) Role of coffee in modulation of diabetes risk. Nutr Rev 70(4):207–217. doi:10.1111/j.1753-4887.2012.00470.x
van Dijk AE, Olthof MR, Meeuse JC, Seebus E, Heine RJ, van Dam RM (2009) Acute effects of decaffeinated coffee and the major coffee components chlorogenic acid and trigonelline on glucose tolerance. Diabetes Care 32(6):1023–1025. doi:10.2337/dc09-0207
Yoshinari O, Igarashi K (2010) Anti-diabetic effect of trigonelline and nicotinic acid, on KK-A(y) mice. Curr Med Chem 17(20):2196–2202
Mishkinsky J, Joseph B, Sulman FG (1967) Hypoglycaemic effect of trigonelline. Lancet 2(7529):1311–1312
Nuhu AA (2014) Bioactive micronutrients in coffee: recent analytical approaches for characterization and quantification. ISRN Nutr 2014:384230. doi:10.1155/2014/384230
Yoshinari O, Sato H, Igarashi K (2009) Anti-diabetic effects of pumpkin and its components, trigonelline and nicotinic acid, on Goto-Kakizaki rats. Biosci Biotechnol Biochem 73(5):1033–1041. doi:10.1271/bbb.80805
de Valk HW (1999) Magnesium in diabetes mellitus. The Netherlands J Med 54(4):139–146
Belin RJ, He K (2007) Magnesium physiology and pathogenic mechanisms that contribute to the development of the metabolic syndrome. Magnes Res 20(2):107–129
Barbagallo M, Dominguez LJ, Galioto A, Ferlisi A, Cani C, Malfa L, Pineo A, Busardo A, Paolisso G (2003) Role of magnesium in insulin action, diabetes and cardio-metabolic syndrome X. Mol Asp Med 24(1–3):39–52
Paolisso G, Scheen A, D’Onofrio F, Lefebvre P (1990) Magnesium and glucose homeostasis. Diabetologia 33(9):511–514
Clifford MN (1999) Chlorogenic acids and other cinnamates-nature, occurrence and dietary burden. J Sci Food Agric 79:362–372
Ceriello A, Motz E (2004) Is oxidative stress the pathogenic mechanism underlying insulin resistance, diabetes, and cardiovascular disease? The common soil hypothesis revisited. Arterioscler Thromb Vasc Biol 24(5):816–823. doi:10.1161/01.ATV.0000122852.22604.78
Lenzen S (2008) Oxidative stress: the vulnerable beta-cell. Biochem Soc Trans 36(Pt 3):343–347. doi:10.1042/BST0360343
Robinson K, Prins J, Venkatesh B (2011) Clinical review: adiponectin biology and its role in inflammation and critical illness. Crit Care 15(2):221. doi:10.1186/cc10021
Fisman EZ, Tenenbaum A (2014) Adiponectin: a manifold therapeutic target for metabolic syndrome, diabetes, and coronary disease? Cardiovasc Diabetol 13:103. doi:10.1186/1475-2840-13-103
Yamauchi T, Iwabu M, Okada-Iwabu M, Kadowaki T (2014) Adiponectin receptors: a review of their structure, function and how they work. Best Pract Res Clin Endocrinol Metab 28(1):15–23. doi:10.1016/j.beem.2013.09.003
Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K (2006) Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Investig 116(7):1784–1792. doi:10.1172/JCI29126
van Dam RM, Feskens EJ (2002) Coffee consumption and risk of type 2 diabetes mellitus. Lancet 360(9344):1477–1478. doi:10.1016/S0140-6736(02)11436-X
van Dam RM, Hu FB (2005) Coffee consumption and risk of type 2 diabetes: a systematic review. JAMA 294(1):97–104
Hiltunen LA (2006) Are there associations between coffee consumption and glucose tolerance in elderly subjects? Eur J Clin Nutr 60(10):1222–1225. doi:10.1038/sj.ejcn.1602441
Paynter NP, Yeh HC, Voutilainen S, Schmidt MI, Heiss G, Folsom AR, Brancati FL, Kao WH (2006) Coffee and sweetened beverage consumption and the risk of type 2 diabetes mellitus: the atherosclerosis risk in communities study. Am J Epidemiol 164(11):1075–1084. doi:10.1093/aje/kwj323
van Dam RM (2006) Coffee consumption and the decreased risk of diabetes mellitus type 2. Ned Tijdschr Geneeskd 150(33):1821–1825
van Dam RM (2006) Green tea, coffee, and diabetes. Ann Intern Med 145(8):634 (author reply 634–635)
van Dam RM, Willett WC, Manson JE, Hu FB (2006) Coffee, caffeine, and risk of type 2 diabetes: a prospective cohort study in younger and middle-aged U.S. women. Diabetes Care 29(2):398–403
Huxley R, Lee CM, Barzi F, Timmermeister L, Czernichow S, Perkovic V, Grobbee DE, Batty D, Woodward M (2009) Coffee, decaffeinated coffee, and tea consumption in relation to incident type 2 diabetes mellitus: a systematic review with meta-analysis. Arch Intern Med 169(22):2053–2063. doi:10.1001/archinternmed.2009.439
Hamer M, Witte DR, Mosdol A, Marmot MG, Brunner EJ (2008) Prospective study of coffee and tea consumption in relation to risk of type 2 diabetes mellitus among men and women: the Whitehall II study. Br J Nutr 100(5):1046–1053. doi:10.1017/S0007114508944135
Greenberg JA, Boozer CN, Geliebter A (2006) Coffee, diabetes, and weight control. Am J Clin Nutr 84(4):682–693
Naismith DJ, Akinyanju PA, Szanto S, Yudkin J (1970) The effect, in volunteers, of coffee and decaffeinated coffee on blood glucose, insulin, plasma lipids and some factors involved in blood clotting. Nutr Metab 12(3):144–151
Crozier TW, Stalmach A, Lean ME, Crozier A (2012) Espresso coffees, caffeine and chlorogenic acid intake: potential health implications. Food Funct 3(1):30–33. doi:10.1039/c1fo10240k
Monteiro M, Farah A, Perrone D, Trugo LC, Donangelo C (2007) Chlorogenic acid compounds from coffee are differentially absorbed and metabolized in humans. J Nutr 137(10):2196–2201
Stalmach A, Steiling H, Williamson G, Crozier A (2010) Bioavailability of chlorogenic acids following acute ingestion of coffee by humans with an ileostomy. Arch Biochem Biophys 501(1):98–105. doi:10.1016/j.abb.2010.03.005
Acknowledgments
The authors would like to acknowledge the fundamental support from Mrs. Valerie Yaughn, Director of the Library at South University, Savannah Campus, in helping to find peer-reviewed papers that were of interest and Julius Hornstein, who offered to revise my manuscript. Dr. Darcy Lima passed away last July 2015, and I wanted to acknowledge his infinite encouragement to write this and many other papers, book chapters and books we wrote together. He will be forever remembered and his memory a continuous source of support and a model to be followed.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
D. R. A. Lima: Deceased.
Rights and permissions
About this article
Cite this article
Santos, R.M.M., Lima, D.R.A. Coffee consumption, obesity and type 2 diabetes: a mini-review. Eur J Nutr 55, 1345–1358 (2016). https://doi.org/10.1007/s00394-016-1206-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-016-1206-0