Abstract
Background
We investigated whether the increase of plasma natriuretic peptides (NPs) in atrial fibrillation (AF) is independent of the effect of AF on the left atrial (LA) hemodynamics.
Methods
Hemodynamically stable patients scheduled for AF ablation underwent assessment of B-type natriuretic peptide (BNP) and mid-regional pro-atrial natriuretic peptide (MR-proANP), echocardiography, and direct measurement of left atrial (LA) pressure. Concentrations of the NPs were compared between patients in AF (n = 31) and controls in sinus rhythm (SR; n = 31) who were matched for age, gender, heart rate, left ventricular ejection fraction, LA volume index, and directly measured mean LA pressure. Eighteen patients underwent serial measurement of NPs and LA pressure during native SR and after 20 min of pacing-induced AF.
Results
Compared to the patients in SR, the patients in AF had 2.6 times higher unadjusted BNP [median (inter-quartile range), 101 (63, 129) vs. 38 (26, 79) ng/L] and two times higher unadjusted MR-proANP [183 (140, 230) vs. 91 (67, 135) pmol/L; both p < 0.001]. Concentrations of both NPs correlated with mean LA pressure in the patients in SR (r = 0.75 for BNP and 0.62 for MR-proANP, both p < 0.001) but not in the patients in AF (r = 0.18 and 0.04, respectively, both p > 0.3). Both NPs increased significantly during induced AF [adjusted median (IQR) relative change, BNP: 27 (22; 40)%, MR-proANP: 75 (64; 99)%, both p < 0.001] without a significant change in the LA pressure.
Conclusions
The increase of NPs in AF was independent of its effect on the LA hemodynamics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Plasma concentrations of natriuretic peptides (NPs) are usually increased in patients in atrial fibrillation (AF) compared to patients in sinus rhythm (SR) [1]. It is still unclear whether this phenomenon is caused by AF itself or whether it is related to hemodynamic overload and cardiac remodeling induced by AF. Previous studies were inconclusive in clarifying the mechanisms behind the increase of NPs in AF because they either used non-invasive methods [2,3,4,5,6,7,8,9] or they focused on patients with heart failure [4, 10]. However, a better understanding of how AF affects the release of NPs may have important clinical implications, especially for the diagnosis of early stages of heart failure with preserved ejection fraction (HFpEF). In these patients, symptoms and clinical findings are often ambiguous but AF is highly prevalent [1, 10].
The present study aimed to determine whether the effect of AF on the release of NPs is independent of its effect on the LA hemodynamics. To this end, plasma concentrations of B-type natriuretic peptide (BNP) and mid-regional pro-atrial natriuretic peptide (MR-proANP) were compared between hemodynamically stable patients in AF and a control group of patients in SR who were matched for directly measured LA pressure and key clinical and structural variables. In addition, a subset of the patients underwent measurement of the NPs along with assessment of the LA hemodynamics during SR and after inducing AF. At last, the study investigated whether the presence of AF would affect the relationship between NPs’ plasma concentrations and mean LA pressure.
Methods
Study population and protocol
This was a prospective, single-center study. The study protocol was approved by our institutional ethical committee in accordance with the standards of the Declaration of Helsinki, and all patients signed a consent to the investigation. The initial study population included 106 hemodynamically stable patients scheduled for catheter ablation of AF who were either in AF (n = 32) or in SR (n = 74) on admission. Excluded were patients with dilated, hypertrophic or restrictive cardiomyopathy, patients with significant valvular heart disease (previous valve surgery, or more than a moderate degree of stenosis or insufficiency of any valve), and patients with congenital heart disease.
On the day before ablation, all patients underwent a thorough clinical evaluation and transthoracic echocardiography. Heart rhythm was monitored by Holter ECG from admission throughout the entire study protocol for at least 18 h. Patients in whom the heart rhythm alternated during this period were excluded. At the beginning of the ablation procedure, after obtaining transseptal access, all patients underwent direct measurement of LA pressure and blood sampling for assessment of BNP and MR-proANP. In 18 consecutive patients, the blood sampling and measurement of the LA pressure were performed during native SR and after 20 min of interrupted AF, which was induced by rapid pacing from the coronary sinus.
Because in the initial non-selected population the patients who presented in AF differed in some characteristics from the patients in SR (Tables 1, 2), they were matched with the patients in SR using propensity-score matching (described in detail below). The final study population consisted of 31 patients who presented with AF and a control group of 31 patients in SR who had similar clinical, structural, and hemodynamic characteristics (Tables 1, 2).
Assessment of cardiac function and hemodynamics
Transthoracic echocardiography was performed by experienced operators (Vivid 7, GE Healthcare, UK). In case of present AF, all measurements were obtained by averaging of at least five consecutive beats.
LA pressure was measured before the LA mapping through an 8-F fluid-filled transseptal sheath placed in the LA cavity. The pressure transducer was zeroed at the mid-thoracic level. Mean LA pressure was calculated from the electronic mean of the pressure curve over at least three complete breath cycles. The height of the V-wave and LA pulse pressure (V-wave to Y-nadir) were measured manually at end-expirium, using the Prucka CardioLab System (GE Healthcare). LA meridional wall stress and LA diastolic stiffness were calculated as previously described [11]. The minimal and maximal LA volumes for calculation of the LA stiffness were obtained by echocardiography using the area–length method [12]. Central venous pressure was measured via femoral venous sheath. Exact LA volume and relative extent of low LA bipolar voltage (using 0.15 mV cut-off) were determined by point-by-point electroanatomic mapping (CARTO-3, Biosense Webster, Israel) as previously described [13].
Assessment of natriuretic peptides
EDTA-anticoagulated peripheral blood plasma was obtained immediately before the hemodynamic assessment. The samples were stored at − 70 °C until batch analysis. BNP was assessed by a chemiluminescent immunoassay (Architect, Abbott Diagnostics, USA) with a sensitivity of 10 ng/L. MR-proANP was assessed by a luminometric immunoassay (Kryptor, BRAHMS, Germany) with a sensitivity of 2.1 pmol/L. The coefficient of variation was < 10% for both assays. BNP < 35 ng/L and MR-proANP < 116 pmol/L were regarded normal [14, 15].
Statistical analysis
Initially, factors associated with increased NP concentrations were identified in the non-matched population by stepwise multivariable linear regression analysis. The covariates in the models were selected by backward elimination of all significant univariable predictors. The NP values were log-transformed before the analysis because of a right-skewed distribution [16]. The identified independent factors included age, female gender, presence of AF, mean LA pressure, LV ejection fraction (LVEF), LA volume (for both NPs), and glomerular filtration rate (only for MR-proANP). These factors, along with the patient’s heart rate, were subsequently used for propensity-score matching of the patients in AF with the patients in SR (using the nearest neighbor matching with the ratio of 1:1).
Because of the different size of the matched and the non-matched study populations, the differences between the patients in AF and SR were expressed by standardized mean difference, and between-group comparisons were performed by logistic regression. Factors associated with increased NPs were identified by linear regression, similarly as in the non-matched population. The effect of AF on the relationship between LA pressure and NP concentrations was evaluated by linear regression with an interaction term (log(NP) = AF present + LA mean pressure + AF present * LA mean pressure). Other baseline comparisons were performed by the Student’s t test, Mann–Whitney U test, χ2 test, Fisher’s test, or Pearson’s correlation, as appropriate. Serial change in the NP concentrations and LA hemodynamic variables was compared by paired t test and by multivariable linear regression. p value < 0.05 was considered significant. All analyses were conducted in R 3.2 (R-Foundation, Vienna, Austria) with the use of the MatchIt 3.0 package [17].
Results
Characteristics of the study population
The matched study population (n = 62) consisted of mostly mid-age men with paroxysmal AF and a relatively short history of AF-related symptoms (Table 1). Four patients (6%) had a previous history of decompensated heart failure, but all the episodes occurred > 3 months before the study. The patients had overall preserved LVEF and all were euvolemic at the time of the study, which was documented by the low right atrial pressure (Table 2). In the patients who presented with AF, the arrhythmia persisted for a median of 3 months [inter-quartile range (IQR) 1–9 months] before inclusion into the study.
Factors associated with increased plasma NPs
Table 3 shows multivariable analysis of independent factors of increased NPs identified in the matched population. For both NPs, the presence of AF emerged as the strongest factor, accounting for ~ 25% of the NPs’ variance. Other factors which were significantly associated with increased NPs in univariable but not in multivariable analysis included higher age, CHA2DS2-VASc score, E/E′ ratio, E-wave velocity, mitral insufficiency grade, LA wall stress, and right atrial pressure. In addition, BNP was associated with greater LA pulse pressure, V-wave height, and LA wall stress; and MR-proANP was associated with greater LA volume. No association was found between NP concentrations and heart rate. Within the whole matched population, the concentrations of both NPs correlated with the relative extent of LA low bipolar voltage [r = 0.2, p = 0.02 for log(BNP), and r = 0.4, p < 0.001, for log(MR-proANP)], but no correlation was found between the NPs and low LA voltage extent when the SR and AF patients were analyzed separately.
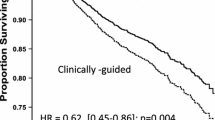
Relationship between plasma NPs and mean LA pressure in AF
Importantly, while in the patients in SR there was a strong correlation between mean LA pressure and log-transformed BNP and MR-proANP concentrations (r = 0.75 and 0.62, respectively, both p < 0.001), no correlation was found between the NPs and the mean LA pressure in the patients in AF (r = 0.18 and 0.04, respectively, both p > 0.3; Fig. 1). Moreover, in multivariable analysis, the presence of AF caused a significant interaction effect on the relationship between NPs and mean LA pressure (p value for interaction = 0.01 for both NPs).
Correlation of mean left atrial pressure and natriuretic peptide plasma concentrations according to the presence of atrial fibrillation. The figure shows good correlation of unadjusted plasma B-type natriuretic peptide (BNP) and mid-regional pro-atrial natriuretic peptide (MR-proANP) and mean left atrial (LA) pressure in the patients in sinus rhythm (SR; blue triangles) but lacking correlation in the patients in atrial fibrillation (AF; red circles)
Comparison between patients in AF and SR
Tables 1 and 2 show comparison between the patients in AF and the matched controls in SR. By design, both groups did not differ in age, gender, key comorbidities, heart rate, LVEF, LV diastolic characteristics, LA volume, or LA hemodynamics, though the patients who presented in AF had expectedly more often persistent than paroxysmal form of AF and higher E-wave velocity.
Despite the similar clinical and hemodynamic profile, the patients in AF had on average 2.6 times higher BNP and 2 times higher MR-pro ANP unadjusted concentrations than the patients in SR (Table 1; Fig. 2). Concentrations of both NPs remained significantly increased in the patients in AF even after adjusting the NP values for all other independent confounders. Median BNP adjusted for gender, mean LA pressure, and LA volume was 78 (63, 112) ng/L in AF vs. 47 (35, 69) ng/L in SR (p < 0.001); median MR-proANP adjusted for LVEF and mean LA pressure was 172 (155, 186) pmol/L in AF vs. 101 (88, 117) pmol/L in SR (p < 0.001). Unadjusted BNP and MR-proANP, respectively, were in normal range only in 3 (10%) and 5 (16%) of the patients in AF vs. in 14 (45%) and 21 (67%) of the patients in SR (p < 0.01 for both).
Comparison of natriuretic peptide concentrations between patients in atrial fibrillation and matched patients in sinus rhythm. The figure shows comparison of unadjusted plasma B-type natriuretic peptide (BNP) and mid-regional pro-atrial natriuretic peptide (MR-proANP) between patients in atrial fibrillation (AF) and matched controls in sinus rhythm (SR). Four data points with BNP values between 330 and 395 ng/l are not shown for visualization purpose. The p values were calculated by Mann–Whitney U test
Change in plasma NPs after induction of AF
Eighteen patients underwent serial assessment of the NPs and hemodynamics during native SR and after 20 min of sustained pacing-induced AF. While there was no significant change in the central venous pressure or mean LA pressure, plasma concentrations of both NPs increased significantly during AF (Fig. 3). The elevation of NPs remained significant even after adjusting for CVP, heart rate, mean LAP, and baseline NP concentrations [adjusted median (IQR) relative change for BNP: 27 (22; 40) %; NT-proBNP: 13 (9; 15) %; MR-proANP: 75 (64; 99) %; all p < 0.001 by Wilcoxon signed-rank test].
Change in the natriuretic peptide concentrations after inducing atrial fibrillation. The figure shows paired measurements of BNP, MR-proANP and mean left atrial (LA) pressure during native sinus rhythm (SR) and after 20 min of uninterrupted pacing-induced atrial fibrillation (AF). The thick red lines represent mean values with standard error. The p values were calculated by paired t test. The graphs highlight significant increase in both natriuretic peptides during AF that was not explained by an increase in the LA pressure
Discussion
This study found 2.6 times higher BNP and 2 times higher MR-pro ANP in stable patients with preserved LVEF who were in AF than in matched controls in SR. More importantly, the study demonstrated that the increase of the NPs in AF was not related to alteration in the LA hemodynamics, as both patient groups had comparable LA pressure, LA volume, and LA meridional wall stress. These observations were further supported by showing that NP concentrations but not LA pressure increased significantly after experimental induction of AF. Lastly, the increase of NPs in AF seemed not to be related to chronic histopathological changes in the LA tissue, which was indicated by the lack of correlation between NP concentrations and LA low-voltage area, and by the comparable LA stiffness between the AF and SR groups.
From a clinical perspective, the most important finding was that plasma concentrations of both NPs correlated well with invasively measured mean LA pressure in the patients in SR, but no such correlation was found in the patients in AF. This finding has implications for clinical use of NPs as a surrogate of left-sided pressure overload, particularly in the diagnosis of latent heart failure with preserved LVEF (HFpEF) [18]. AF occurs in 25–60% of these patients [1, 19, 20] and it is difficult to distinguish whether the patient’s symptoms are related to the heart failure or to AF alone [1, 21]. The lack of a correlation between NPs and LA pressure in AF suggests that the diagnostic performance would unlikely improve by applying higher concentration cut-offs. Moreover, the intrinsic increase of NPs in AF not reflecting the hemodynamics implies that clinical trials on HFpEF should be careful with including patients based on increased NPs [22], as this could lead to enrollment of disproportionately more patients with AF [1]. The higher prevalence of AF in such a trial could, in turn, translate to unsatisfactory response to the tested therapy, and it could bias the study results if the NPs represented an outcome measure [23].
Previous studies could not determine conclusively whether the increase of NPs in AF is independent of the impaired LA hemodynamics because they employed only non-invasive methods [2,3,4,5,6,7,8,9]. The only study investigating this phenomenon invasively enrolled unselected patients with established HFpEF. Nevertheless, the study found that the relationship between NT-proBNP and AF was independent of pulmonary capillary wedge pressure [10]. The original feature of our study was that the patients in AF and SR were matched according to the same level of LA pressure which was measured directly in the LA cavity. Our study was also the first to perform serial assessment of NPs in parallel with invasive hemodynamic assessment. While previous studies evaluated decrease of NPs after restoring SR [24,25,26], our study was the first to demonstrate an actual increase of NPs after the onset of AF.
Evidence from experimental studies indicates that the primary trigger for the release of NPs from myocytes is cellular stretch, which is partially mediated by mechanoreceptors and mechano-sensitive ion channels [27,28,29,30]. This likely explains the intrinsic acute release of NPs in AF, as cellular stretch will increase even without an increase in atrial pressure. Although the underlying cellular signaling has not yet been fully elucidated, it may involve activation of the CaMII kinase or calcineurin/NFAT pathways [27, 28]. It is conceivable that chronic activation of these pathways during AF could cause a relative depletion of intracellular calcium, which in turn might explain the blunted release of NPs in response to the increase of LA pressure in patients with AF [29]. At last, the increase of NPs in AF might be related to the heart rhythm irregularity and ensuing greater cyclic rises in LA hemodynamic stress, which could stimulate the NP release more potently than a gradual elevation of the mean LA pressure [31]. On the other hand, the hypothesis would partially contradict to the fact that the average LA pulse pressure and V-wave height did not differ between AF and SR patients. Further research is needed to clarify the mechanisms responsible for the increase of NPs in AF.
Limitations
Our study did not reevaluate the relationship between NPs and LA pressure after restoring the SR. This would have required a prolonged waiting period after the ablation procedure with a catheter inserted in the LA until the concentration of NPs stabilizes. Serial measurement of NPs and hemodynamics were performed only in a subset of the patient and only after 20-min AF. The main reason was to avoid unnecessary prolongation of the ablation procedure. The LA voltage is incomparable between AF and SR, as it is affected by the LA cycle length [32]. Therefore, the relationship between the LA voltage and NPs could be evaluated only separately within the AF and SR groups. Our study included only hemodynamically stable patients with overall preserved LVEF. While this had the advantage in that the study population was homogeneous and well defined, our results cannot be fully extrapolated to patients with decompensated heart failure with reduced LVEF.
Conclusions
In hemodynamically stable patients with preserved LVEF, the presence of AF was associated with significant increase in plasma concentrations of BNP and MR-proANP. This association was independent of the LA structure and hemodynamics. Moreover, the presence of AF disturbed the relationship between NP concentrations and mean LA pressure. The latter has implications for the use of NPs for diagnosis of latent HFpEF in patients with AF.
References
Kotecha D, Lam CS, Van Veldhuisen DJ, Van Gelder IC, Voors AA, Rienstra M (2016) Heart failure with preserved ejection fraction and atrial fibrillation: vicious twins. J Am Coll Cardiol 68(20):2217–2228. https://doi.org/10.1016/j.jacc.2016.08.048
Bai M, Yang J, Li Y (2009) Serum N-terminal-pro-brain natriuretic peptide level and its clinical implications in patients with atrial fibrillation. Clin Cardiol 32(12):E1–E5. https://doi.org/10.1002/clc.20478
Bakowski D, Wozakowska-Kaplon B, Opolski G (2009) The influence of left ventricle diastolic function on natriuretic peptides levels in patients with atrial fibrillation. Pacing Clin Electrophysiol 32(6):745–752. https://doi.org/10.1111/j.1540-8159.2009.02360.x
Corell P, Gustafsson F, Kistorp C, Madsen LH, Schou M, Hildebrandt P (2007) Effect of atrial fibrillation on plasma NT-proBNP in chronic heart failure. Int J Cardiol 117(3):395–402. https://doi.org/10.1016/j.ijcard.2006.03.084
Lee SH, Jung JH, Choi SH, Lee N, Park WJ, Oh DJ, Rhim CY, Lee KH (2006) Determinants of brain natriuretic peptide levels in patients with lone atrial fibrillation. Circ J 70(1):100–104
Letsas KP, Filippatos GS, Pappas LK, Mihas CC, Markou V, Alexanian IP, Efremidis M, Sideris A, Maisel AS, Kardaras F (2009) Determinants of plasma NT-pro-BNP levels in patients with atrial fibrillation and preserved left ventricular ejection fraction. Clin Res Cardiol 98(2):101–106. https://doi.org/10.1007/s00392-008-0728-8
Rossi A, Enriquez-Sarano M, Burnett JC Jr, Lerman A, Abel MD, Seward JB (2000) Natriuretic peptide levels in atrial fibrillation: a prospective hormonal and Doppler-echocardiographic study. J Am Coll Cardiol 35(5):1256–1262
Silvet H, Young-Xu Y, Walleigh D, Ravid S (2003) Brain natriuretic peptide is elevated in outpatients with atrial fibrillation. Am J Cardiol 92(9):1124–1127
Ulimoen SR, Enger S, Tveit A (2009) Impact of atrial fibrillation on NT-proBNP levels in a 75-year-old population. Scand J Clin Lab Invest 69(5):579–584. https://doi.org/10.1080/00365510902853305
Lam CS, Rienstra M, Tay WT, Liu LC, Hummel YM, van der Meer P, de Boer RA, Van Gelder IC, van Veldhuisen DJ, Voors AA, Hoendermis ES (2017) Atrial fibrillation in heart failure with preserved ejection fraction: association with exercise capacity, left ventricular filling pressures, natriuretic peptides, and left atrial volume. JACC Heart Fail 5(2):92–98. https://doi.org/10.1016/j.jchf.2016.10.005
Melenovsky V, Hwang SJ, Redfield MM, Zakeri R, Lin G, Borlaug BA (2015) Left atrial remodeling and function in advanced heart failure with preserved or reduced ejection fraction. Circ Heart Fail 8(2):295–303. https://doi.org/10.1161/CIRCHEARTFAILURE.114.001667
Degiovanni A, Boggio E, Prenna E, Sartori C, De Vecchi F, Marino PN, From the Novara Atrial Fibrillation Study G (2018) Association between left atrial phasic conduit function and early atrial fibrillation recurrence in patients undergoing electrical cardioversion. Clin Res Cardiol 107(4):329–337. https://doi.org/10.1007/s00392-017-1188-9
Sramko M, Wichterle D, Melenovsky V, Clemens M, Fukunaga M, Peichl P, Aldhoon B, Cihak R, Kautzner J (2017) Resting and exercise-induced left atrial hypertension in patients with atrial fibrillation: the causes and implications for catheter ablation. J Am Coll Cardiol EP. https://doi.org/10.1016/j.jacep.2016.12.010
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Tzikas S, Keller T, Wild PS, Schulz A, Zwiener I, Zeller T, Schnabel RB, Sinning C, Lubos E, Kunde J, Munzel T, Lackner KJ, Blankenberg S (2013) Midregional pro-atrial natriuretic peptide in the general population/Insights from the Gutenberg Health Study. Clin Chem Lab Med 51(5):1125–1133. https://doi.org/10.1515/cclm-2012-0541
Ballo P, Betti I, Barchielli A, Balzi D, Castelli G, De Luca L, Gheorghiade M, Zuppiroli A (2016) Prognostic role of N-terminal pro-brain natriuretic peptide in asymptomatic hypertensive and diabetic patients in primary care: impact of age and gender: results from the PROBE-HF study. Clin Res Cardiol 105(5):421–431. https://doi.org/10.1007/s00392-015-0937-x
Ho D, Imai K, King G, Stuart EA (2011) MatchIt: Nonparametric preprocessing for parametric causal inference. J Stat Softw. https://doi.org/10.18637/jss.v042.i08
Francis GS, Felker GM, Tang WH (2016) A test in context: critical evaluation of natriuretic peptide testing in heart failure. J Am Coll Cardiol 67(3):330–337. https://doi.org/10.1016/j.jacc.2015.10.073
Miro O, Gil VI, Martin-Sanchez FJ, Jacob J, Herrero P, Alquezar A, Llauger L, Aguilo S, Martinez G, Rios J, Dominguez-Rodriguez A, Harjola VP, Muller C, Parissis J, Peacock WF, Llorens P, Research Group on Acute Heart Failure of the Spanish Society of Emergency Medicine R (2018) Short-term outcomes of heart failure patients with reduced and preserved ejection fraction after acute decompensation according to the final destination after emergency department care. Clin Res Cardiol. https://doi.org/10.1007/s00392-018-1237-z
Riedel O, Ohlmeier C, Enders D, Elsasser A, Vizcaya D, Michel A, Eberhard S, Schlothauer N, Berg J, Garbe E (2018) The contribution of comorbidities to mortality in hospitalized patients with heart failure. Clin Res Cardiol 107(6):487–497. https://doi.org/10.1007/s00392-018-1210-x
Tschope C, Birner C, Bohm M, Bruder O, Frantz S, Luchner A, Maier L, Stork S, Kherad B, Laufs U (2018) Heart failure with preserved ejection fraction: current management and future strategies: expert opinion on the behalf of the Nucleus of the “Heart Failure Working Group” of the German Society of Cardiology (DKG). Clin Res Cardiol 107(1):1–19. https://doi.org/10.1007/s00392-017-1170-6
Morbach C, Buck T, Rost C, Peter S, Gunther S, Stork S, Prettin C, Erbel R, Ertl G, Angermann CE, Handheld BNPRN (2018) Point-of-care B-type natriuretic peptide and portable echocardiography for assessment of patients with suspected heart failure in primary care: rationale and design of the three-part handheld-BNP program and results of the training study. Clin Res Cardiol 107(2):95–107. https://doi.org/10.1007/s00392-017-1181-3
Greene SJ, Fonarow GC, Solomon SD, Subacius HP, Ambrosy AP, Vaduganathan M, Maggioni AP, Bohm M, Lewis EF, Zannad F, Butler J, Gheorghiade M (2016) Influence of atrial fibrillation on post-discharge natriuretic peptide trajectory and clinical outcomes among patients hospitalized for heart failure: insights from the ASTRONAUT trial. Eur J Heart Fail. https://doi.org/10.1002/ejhf.674
Wozakowska-Kaplon B (2010) Changes in plasma natriuretic peptide levels in patients with atrial fibrillation after cardioversion. Int J Cardiol 144(3):436–437. https://doi.org/10.1016/j.ijcard.2009.03.085
Charitakis E, Walfridsson H, Alehagen U (2016) Short-term influence of radiofrequency ablation on NT-proBNP, MR-proANP, copeptin, and MR-proADM in patients with atrial fibrillation: data from the observational SMURF Study. J Am Heart Assoc. https://doi.org/10.1161/JAHA.116.003557
Vinch CS, Rashkin J, Logsetty G, Tighe DA, Hill JC, Meyer TE, Rosenthal LS, Aurigemma GP (2004) Brain natriuretic peptide levels fall rapidly after cardioversion of atrial fibrillation to sinus rhythm. Cardiology 102(4):188–193. https://doi.org/10.1159/00008100981009
Schotten U, Verheule S, Kirchhof P, Goette A (2011) Pathophysiological mechanisms of atrial fibrillation: a translational appraisal. Physiol Rev 91(1):265–325. https://doi.org/10.1152/physrev.00031.2009
Heijman J, Voigt N, Nattel S, Dobrev D (2014) Cellular and molecular electrophysiology of atrial fibrillation initiation, maintenance, and progression. Circ Res 114(9):1483–1499. https://doi.org/10.1161/CIRCRESAHA.114.302226
Zhang YH, Youm JB, Earm YE (2008) Stretch-activated non-selective cation channel: a causal link between mechanical stretch and atrial natriuretic peptide secretion. Prog Biophys Mol Biol 98(1):1–9. https://doi.org/10.1016/j.pbiomolbio.2008.05.005
De Jong AM, Maass AH, Oberdorf-Maass SU, Van Veldhuisen DJ, Van Gilst WH, Van Gelder IC (2011) Mechanisms of atrial structural changes caused by stretch occurring before and during early atrial fibrillation. Cardiovasc Res 89(4):754–765. https://doi.org/10.1093/cvr/cvq357
Edwards BS, Zimmerman RS, Schwab TR, Heublein DM, Burnett JC Jr (1988) Atrial stretch, not pressure, is the principal determinant controlling the acute release of atrial natriuretic factor. Circ Res 62(2):191–195
Fiala M, Wichterle D, Chovancik J, Bulkova V, Wojnarova D, Nevralova R, Januska J (2010) Left atrial voltage during atrial fibrillation in paroxysmal and persistent atrial fibrillation patients. Pacing Clin Electrophysiol 33(5):541–548. https://doi.org/10.1111/j.1540-8159.2009.02646.x
Funding
This study was funded by the grant of the Ministry of Health of the Czech Republic—“Conceptual development of a research organization (IKEM IN 00023001)”. MS was supported by a research fellowship grant from the European Society of Cardiology and a research grant of the Czech Society of Cardiology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JK served as an advisory board member for Biosense Webster, Boston Scientific, Medtronic, Liva Nova and St. Jude Medical. Other authors have nothing to declare.
Rights and permissions
About this article
Cite this article
Sramko, M., Wichterle, D., Melenovsky, V. et al. Independent effect of atrial fibrillation on natriuretic peptide release. Clin Res Cardiol 108, 142–149 (2019). https://doi.org/10.1007/s00392-018-1332-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1332-1