Abstract
Infections of cardiac implantable electronic devices (CIEDs) have increased over the past decade. However, the impact of the climate on CIED infections is unknown. To determine whether there is a seasonal variation in CIED infections. In this single-center observational study, retrospective analysis of prospectively collected data was performed. Timone Hospital in Marseille (south-east France) is a tertiary care institution and the regional reference center for management of CIED infections. All consecutive patients with CIED extractions for infectious reasons were included over a 12-year period. We noted the mean temperature (°C), precipitation (mm) and the incidence of CIED infections over this period. Among 612 patients [mean (standard deviation) age, 72.4 (13.0) years; 74.0% male], 238 had endocarditis alone (38.9%), 249 had pocket infection alone (40.7%), and 125 had both (20.4%). We found bacterial documentation in 428 patients (70.0%), commensal in 245 (40.0%). The incidence of CIED infections was positively associated with high temperature (regression coefficient = 0.075; P = 0.01) and precipitation (regression coefficient = 0.022; P < 0.01). Seasonal variation was specific of pocket infections, whether they were associated with endocarditis or not. Subgroups with infection seasonality were: women, elderly people (> 75 years), late CIED infection and skin commensal bacterial infections. We found a seasonal variation in pocket infections, whether associated with endocarditis or not. Infections were associated with elevated temperatures and precipitation. Therefore, specific prevention strategy should be discussed in high-risk patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Implantation of cardiac implantable electronic devices (CIEDs), which include permanent pacemakers and implantable cardioverter–defibrillators (ICDs), has increased dramatically [1]. This is largely due to the expanded indications for CIED implantation based on the results of large clinical trials of ICDs for primary prevention, as well as the aging of the general population [2]. However, studies have suggested that the number of infections associated with CIEDs is increasing, more than the rate of implantations [3].
CIED infection is a serious condition that can occur immediately after an implantation or many years later. Preventive strategies are a desirable goal, but CIED pathogenesis remains unclear and mechanisms are still debated. For example, it has been proposed that dormant bacteria in the CIED pocket could reactivate [4]. A change in environmental heat and humidity associated with climate and seasons could also be relevant. Climate and seasonal variability have long been associated with infectious diseases [5,6,7]. However, the impact of climate, seasonality, environmental temperature and humidity on CIED infection is unknown.
Therefore, the aim of this study was to determine whether there is a seasonal variation in the incidence of CIED infections, which could be explained by meteorological variations in temperature and precipitation.
Methods
Study design
This single-center study was conducted in Timone hospital, Marseille, in the south-east of France, in the region of the Provence Alpes Côte d’Azur (PACA). It is a tertiary care institution and the regional reference center for CIED infection management. A retrospective analysis of prospectively collected data was undertaken.
Patients
The ethics committee of the Timone Hospital approved this study. We included all consecutive patients with complete CIED extraction for reasons of infection, from January 2003 to May 2015. The date of the extraction procedure was considered as the date of the infection.
CIED infections were categorized as “pocket infections” if local inflammation was present or if hardware protruded through the skin and/or as “device-related endocarditis” according to the modified Duke criteria [8].
Data collection
Clinical data
For all patients, data were collected prospectively and entered into a specific electronic database that was already in use for each lead extraction performed at our center. Data included demographic data (age, gender); underlying heart disease; type, date, and indication of first CIED implantation; date since last intervention on the device; age, number, and location of leads; and whether the pocket was infected or not, regardless of the type of CIED infection. CIED infection was considered “early” if it occurred < 1 year after the last intervention.
Microbiology
In all patients, cultures from at least three blood samples (all efforts were made to obtain the blood cultures before initiating antibiotic therapy at the hospital) and swabs from the device pocket, generator, and leads were taken for microbial analyzes: phenotypic identification (Vitek, Biomerieux, France) and whole-cell identification by matrix-assisted laser desorption ionization-time of flight (MALDI-ToF) mass spectrometry (Microflex, Bruker Daltonics, Germany). Coagulase-negative Staphylococcus, Corynebacterium, and Propionibacterium were considered commensal; others were considered pathogenic. In case of double bacteria documentation (commensal and pathogenic), we primarily considered the bloodstream documentation. For device and leads culture, because of the risk of non-specific contamination by commensal organism during extraction, we considered only pathogenic bacteria [9].
Weather temperature and seasons
Average monthly meteorological statements were obtained from the Marseille-Marignane weather station [10]. In particular, temperature (°C) and precipitation amount (mm) were noted.
Outcomes
The post hoc primary outcome of interest was the bimonthly incidence of CIED infections.
Statistical analysis
A descriptive analysis of the clinical and microbiologic characteristics of the study sample was performed. Qualitative variables are expressed as numbers and percentages, and quantitative variables as means and standard deviations (SDs) or medians and interquartile ranges (IQRs). A descriptive analysis of the infections incidence over time was performed using seasonal decomposition by a moving averages strategy. Considering infections incidence data by month resulted in the rejection of the hypothesis of normality of the time series; hence, data were grouped by 2-month windows.
The change in infections incidence over time was analyzed using multivariable Box–Jenkins method-based seasonal autoregressive integrated moving average (SARIMAX) models, which allow exposure and effect, trend changes, and seasonal changes to be accounted for. Pre-estimation of univariate SARIMAX models was based on stationarity, autocorrelation, and partial autocorrelation functions. Goodness of fit was assessed using Akaike and Bayesian information criterion, and the Box–Jenkins principle of parsimony.
Multivariable models were systematically adjusted on time (with linear and a quadratic term to take into account the decrease of activity), cumulative precipitation, and temperature. Various multivariable models were constructed, for the various subgroups defined according to the following characteristics: gender (male/female); age (< 75/> 75 years); type of CIED infection (early/late); endocarditis/pocket infection; and bacteriologic identification. The final multivariable SARIMAX models were tested for goodness of fit, residual autocorrelation (Barlett's test with noise test, Portmanteau Q test), and residual normality. A full statistical description of the SARIMAX model can be found in the online-only Supplement.
All tests were two-sided, and P < 0.05 was considered significant. All data were analyzed using R software.
Results
Baseline characteristics
During the 12-year study period, 824 CIEDs were removed: 612 for reasons of infection. The demographic and clinical characteristics of these patients are summarized in Table 1. The mean (SD) age was 72.4 (13.0) years. In this cohort, 410 (67.0%) patients were implanted with a pacemaker and 202 (33.0%) with an ICD. The mean (SD) number of leads per patient was 2.3 (0.8). The median time between the last intervention and the extraction was 578 days (IQR 156–1422 days). The median lead age was 1739 days (IQR 420–3206 days). A total of 239 patients (39.1%) had early CIED infections.
Microbiology
Microbiologic ecology is summarized in Tables 2 and 3. Concordance between blood culture and material culture existed for 99 patients (56.0%) who presented with at least one positive blood culture. Considering early infection (n = 237), the proportions of commensal [n = 84 (35.4%)] and pathogenic infection [n = 73 (30.8%)] were similar, whereas we found a tendency of increasing proportion of commensal infection for later infection (n = 375; commensal: n = 161 (42.9%); pathogenic: n = 110 (29.3%); P = 0.27).
Climate
The weather in PACA is Mediterranean, class CSa by the Köppen–Geiger climate classification [11]. It is characterized as a warm, temperate climate with hot, dry summers and mild, wet winters. Data from the Marseille-Marignane weather station17 confirm this trend, with hot summers (June/July and August/September), mild winters (December/January and February/March) and with maximum precipitation in October/November. Climatic data are summarized in Fig. 1, along with the numbers of infections during each 2-month period throughout the study.
Incidence of infections, cumulative precipitation, and mean temperature during each 2-month period throughout the study. The climate in Provence Alpes Côte d’Azur is warm and temperate with hot, dry summers and mild, wet winters. Our data confirm this trend, with hot summers (June/July and August/September), mild winters (December/January and February/March), with maximum precipitation in October/November
Incidence of CIED infections and meteorological variations
The incidence of CIED infections was positively associated with precipitation (regression coefficient=0.023; P < 0.01) and elevated temperature (regression coefficient = 0.076; P = 0.01) (Table 4). After adjustment of time and meteorological variation, a seasonality [seasonal autoregressive (SAR)/seasonal average moving (SAM) coefficient] persisted.
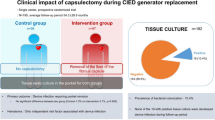
Subgroup analysis revealed that seasonal variations were specific to CIED infections with pocket infection (with or without endocarditis). Endocarditis without pocket infection did not have any seasonal variation (Fig. 2 and Table 4). The association of CIED infections incidence with high temperature and/or precipitation was significant in various subgroups: women, those aged > 75 years old, patients with late CIED infection, and those with skin commensal bacterial infection.
a Pocket infection and b non-pocket infection incidences according to mean bimonthly temperature (°C) and cumulative precipitation (mm). In a, the “pocket infections” incidence curve shows two significant peaks: the first one in June/July (elevated temperature) and the second one in October/November (increased precipitation). In b the “non-pocket infection” incidence curve shows no significant peak. F/M, February/March; A/M, April/May; J/J, June/July; A/S, August/September; O/N, October/November; D/J, December/January
Discussion
To our knowledge, this 12-year epidemiologic study of 612 patients with CIED infection is the first to show seasonal variation in the incidence of CIED infections. We found a positive association for periods with elevated temperature (June/July) and precipitation (October/November). This seasonal variation specifically concerns pocket infection (with or without endocarditis), but not endocarditis alone. The increasing incidence of CIED infections with high temperature and precipitation is particularly pronounced in women, patients aged > 75 years, those with late CIED infection, and patients with skin commensal bacterial infections.
Device-related infection is the result of complex interactions between the device, the microbe, and the host. Based on clinical presentation, pathophysiologic mechanisms of CIED infection (endocarditis vs pocket infection) are supposed to be different [4, 12].
Infections of the indwelling transvenous leads (endocarditis) without pocket infection are thought to be caused by transient bacteremia [13]. Seasonal variations of bacteremia have already been described in the literature. Nevertheless, these mainly concern Gram-negative organisms [14], which are rarely responsible for CIED infections. This could explain why we did not find any seasonal variation in the incidence of CIED endocarditis without pocket infection. However, for pocket infections, the mechanism is local contamination of the pocket and could be secondary to skin infection [13]. This is probably the same mechanism for endocarditis secondary to pocket infection, in which lead infection could be the result of contiguity transmission from the pocket.
Early CIED infections are more likely due to organisms that are introduced at the time of surgery (whether it is commensal or pathogenic bacteria). With regard to this mechanism, it seems pertinent that early pocket infections are independent of seasonal variation. On the other hand, our study shows a tendency of increasing proportion of commensal infection for later infection [15]. With the reservations relative to this non-significant result, this tendency may supports our hypothesis of seasonality.
Biofilm formation is known to be a potential mechanism for device infection [12, 16]. Several steps have been described, of which colonization is the first. The microorganisms must adhere to the exposed surfaces of the device for long enough to become irreversibly attached. The rate of cell attachment depends on the number and types of cells in the environment the device is exposed to and the physicochemical characteristics of the surface. Once these cells have irreversibly attached, they produce extracellular polysaccharides to develop a biofilm. The rate of growth is influenced by the nutrient composition of the environment, antimicrobial drug concentration, and ambient temperature. Then, phagocytic enzymes will damage the tissue around the biofilm, and planktonic bacteria will be released from the biofilm, causing dissemination and acute infection in neighboring tissue [16, 17].
Asymptomatic colonization of CIEDs with commensal bacteria has already been described [13, 18]. This “asymptomatic colonization” can occur after bacterial transcutaneous crossing favored by enhanced epidermal permeability [19, 20]. An experimental animal study showed that exposure to a dry environment enhances epidermal permeability barrier function [21]. Epidermal thickness, the number of layers, and the lipid content of the stratum corneum, lamellar body secretory system, and lamellar membranes are all increased by low humidity. We could therefore expect that a weakened epidemiologic barrier during high humidity could promote “asymptomatic colonization” of pocket CIED infection, with skin commensal bacteria.
The ecology of the skin surface is highly variable depending on topographic location, endogenous host factors, and exogenous environmental factors.[19, 22] Since Ratkowsky et al. proposed a linear relationship between the square root of the growth rate of bacteria and the absolute temperature [23, 24], it has been demonstrated that the densest bacterial populations are located in hot and wet areas, rich in growth factors and with a pH close to 7 [19]. Furthermore, higher temperatures induce acceleration of microbial colonization and microbial interactive effects of the biofilm [25, 26]. Thus, higher temperatures may facilitate CIED infection by enhancing bacterial growth on the skin surface and in the biofilm.
Seasonal variation in CIED infection was particularly pronounced in two subgroups: women and elderly patients. The reduced strength of the skin tissue in such people could explain an increased sensitivity to climatic conditions and, thus, seasonal variation [27, 28].
Our study has some limitations. First, we considered the date of the extraction procedure to be the same as the date of the infection, but, realistically, there is a delay between the onset of infection and the extraction procedure. A retrospective study from the Cleveland Clinic that included 412 consecutive patients who underwent CIED removal for infection (including endocarditis with and without pocket infection) reported a median time interval between onset of infection and device removal of 24 days [29]. However, the diagnosis of pocket infection is easier, so the delay between onset of infection and device removal should be shorter. On the other hand, in cases of isolated endocarditis, clinical signs are often poor (e.g., fever of unknown origin), so diagnosis can be challenging and delayed. Several months may elapse between infection onset and diagnosis. This is probably another reason why we did not see any seasonal variation among patients with endocarditis without pocket infection. Second, our study has limitations attributable to its retrospective single-center nature. However, please note that our data were collected prospectively. Third, we only investigated two components of the climate: temperature and precipitation. It is, however, likely that any interaction between weather and infection is not limited to these two components [30].
Conclusion
Our observational study is the first to report a seasonal trend in CIED infections. Pocket infection incidence (with or without endocarditis) was positively associated with elevated temperature and increased precipitation periods. Subgroups of patients strongly influenced by seasonality and meteorological variations were women, those aged > 75 years old, patients with late infections, and those with commensal bacteria. These results could justify enhanced surveillance during warm, wet seasons and may even justify prophylactic measures in selected high-risk patients. Understanding and controlling biofilm formation could also have a significant impact on rethinking the surface design of CIEDs.
References
Uslan DZ, Tleyjeh IM, Baddour LM, Friedman PA, Jenkins SM, St Sauver JL, Hayes DL (2008) Temporal trends in permanent pacemaker implantation: a population-based study. Am Heart J 155:896–903
Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA, Cleland J, Deharo JC, Delgado V, Elliott PM, Gorenek B, Israel CW, Leclercq C, Linde C, Mont L, Padeletti L, Sutton R, Vardas PE (2013) ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace 15:1070–1118
Cabell CH, Heidenreich PA, Chu VH, Moore CM, Stryjewski ME, Corey GR, Fowler VG Jr (2004) Increasing rates of cardiac device infections among Medicare beneficiaries: 1990–1999. Am Heart J 147:582–586
Blaser MJ, Kirschner D (2007) The equilibria that allow bacterial persistence in human hosts. Nature 449:843–849
Altizer S, Ostfeld RS, Johnson PT, Kutz S, Harvell CD (2013) Climate change and infectious diseases: from evidence to a predictive framework. Science 341:514–519
Balato N, Megna M, Ayala F, Balato A, Napolitano M, Patruno C (2014) Effects of climate changes on skin diseases. Expert Rev Anti Infect Ther 12:171–181
Paynter S, Ware RS, Sly PD, Williams G, Weinstein P (2015) Seasonal immune modulation in humans: observed patterns and potential environmental drivers. J Infect 70:1–10
Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, Dulgheru R, El Khoury G, Erba PA, Iung B, Miro JM, Mulder BJ, Plonska-Gosciniak E, Price S, Roos-Hesselink J, Snygg-Martin U, Thuny F, Tornos Mas P, Vilacosta I, Zamorano JL (2015) ESC guidelines for the management of infective endocarditis: the Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 36:3075–3128
Deharo JC, Quatre A, Mancini J, Khairy P, Le Dolley Y, Casalta JP, Peyrouse E, Prévôt S, Thuny F, Collart F, Raoult D, Habib G, Franceschi F (2012) Long-term outcomes following infection of cardiac implantable electronic devices: a prospective matched cohort study. Heart 98:724–731
INFOCLIMAT. Climatologie de l'année, 2003 à Marseille-Marignane (Marseille Provence). https://www.infoclimat.fr/climatologie/annee/2003/marseille-marignane-marseille-provence/valeurs/07650.html. Accessed 6 Jan 2017
Kottek M, Grieser J, Beck C, Rudolf B, Rubel F (2006) World Map of the Köppen-Geiger climate classification updated. Meteorologische Zeitschrift 15:259–263
Donlan RM (2001) Biofilms and device-associated infections. Emerg Infect Dis 7:277–281
Pichlmaier M, Marwitz V, Kuhn C, Niehaus M, Klein G, Bara C, Haverich A, Abraham WR (2008) High prevalence of asymptomatic bacterial colonization of rhythm management devices. Europace 10:1067–1072
Eber MR, Shardell M, Schweizer ML, Laxminarayan R, Perencevich EN (2011) Seasonal and temperature-associated increases in gram-negative bacterial bloodstream infections among hospitalized patients. PLoS One 6:e25298
Sandoe JA, Barlow G, Chambers JB, Gammage M, Guleri A, Howard P, Olson E, Perry JD, Prendergast BD, Spry MJ, Steeds RP, Tayebjee MH, Watkin R (2015) British Society for Antimicrobial Chemotherapy, British Heart Rhythm Society, British Cardiovascular Society, British Heart Valve Society, British Society for Echocardiography. Guidelines for the diagnosis, prevention and management of implantable cardiac electronic device infection. Report of a joint Working Party project on behalf of the British Society for Antimicrobial Chemotherapy (BSAC, host organization), British Heart Rhythm Society (BHRS), British Cardiovascular Society (BCS), British Heart Valve Society (BHVS) and British Society for Echocardiography (BSE). J Antimicrob Chemother 70:325–359
Hall-Stoodley L, Stoodley P (2005) Biofilm formation and dispersal and the transmission of human pathogens. Trends Microbiol 13:7–10
Costerton JW, Stewart PS, Greenberg EP (1999) Bacterial biofilms: a common cause of persistent infections. Science 284:1318–1322
Rohacek M, Weisser M, Kobza R, Schoenenberger AW, Pfyffer GE, Frei R, Erne P, Trampuz A (2010) Bacterial colonization and infection of electrophysiological cardiac devices detected with sonication and swab culture. Circulation 121:1691–1697
Ruocco E, Donnarumma G, Baroni A, Tufano MA (2007) Bacterial and viral skin diseases. Dermatol Clin 25:663–676
Grassly NC, Fraser C (2006) Seasonal infectious disease epidemiology. Proc Biol Sci 273:2541–2550
Denda M, Sato J, Masuda Y, Tsuchiya T, Koyama J, Kuramoto M, Elias PM, Feingold KR (1998) Exposure to a dry environment enhances epidermal permeability barrier function. J Invest Dermatol 111:858–863
Grice EA, Segre JA (2011) The skin microbiome. Nat Rev Microbiol 9:244–253
Ratkowsky DA, Olley J, McMeekin TA, Ball A (1982) Relationship between temperature and growth rate of bacterial cultures. J Bacteriol 149:1–5
Ratkowsky DA, Lowry RK, McMeekin TA, Stokes AN, Chandler RE (1983) Model for bacterial culture growth rate throughout the entire biokinetic temperature range. J Bacteriol 154:1222–1226
Fink R, Oder M, Rangus D, Raspor P, Bohinc K (2015) Microbial adhesion capacity. Influence of shear and temperature stress. Int J Environ Health Res 25:656–669
Diaz Villanueva V, Font J, Schwartz T, Romani AM (2011) Biofilm formation at warming temperature: acceleration of microbial colonization and microbial interactive effects. Biofouling 27:59–71
Andersen LK, Davis MD (2016) Sex differences in the incidence of skin and skin-related diseases in Olmsted County, Minnesota, United States, and a comparison with other rates published worldwide. Int J Dermatol 55:939–955
Somerville-Millar DA, Noble WC (1974) Resident and transient bacteria of the skin. J Cutan Pathol 1:260–264
Tarakji KG, Chan EJ, Cantillon DJ, Doonan AL, Hu T, Schmitt S, Fraser TG, Kim A, Gordon SM, Wilkoff BL (2010) Cardiac implantable electronic device infections: presentation, management, and patient outcomes. Heart Rhythm. 7:1043–1047
Muller SA (2011) Climate change, dermatology and ecosystem services; trends and trade-offs. Int J Dermatol 50:504–507
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Maille, B., Koutbi, L., Resseguier, N. et al. Seasonal variations in cardiac implantable electronic device infections. Heart Vessels 34, 824–831 (2019). https://doi.org/10.1007/s00380-018-1292-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1292-4