Abstract
In this prospective multicentric study, we investigated the contribution of positron emission tomography (PET) scanning to the staging of Hodgkin’s lymphoma (HL) by computed tomography (CT) and attempted to determine whether it has any impact on therapeutic approach. One hundred eighty six consecutive patients with HL from six Italian centers were enrolled in this study. They were staged with conventional methods; 2-[fluorine-18]fluoro-2-deoxy-d-glucose PET scanning were prospectively compared to CT. CT and FDG-PET stages were concordant in 156 patients (84%) and discordant in 30 patients (16%). PET stage in comparison to CT stage was higher in 27 patients (14%) and lower in 3 patients (1%). The programmed treatment strategy was modified in 11 out of 30 patients (37%) after the definition of final stage. If we considered the 123 CT staged patients with localized stage, ten patients (8%) with a change of stage from localized to advanced after PET evaluation were treated with different strategy. FDG-PET was shown to be a relevant, non-invasive method that supplements conventional procedures and should therefore be used routinely to stage HL, particularly in early stage patients, where a change in stage may modify disease management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hodgkin’s lymphoma (HL) is a chemo-radiosensitive disease, and very high rates of disease-free survival and overall survival can be obtained with a modern approach. As stage is an important factor in treatment choice, highly accurate procedures are needed to correctly assess the localization of disease, thus preventing overtreatment and undertreatment as well as minimizing the morbidity related to chemotherapy and radiotherapy [1].
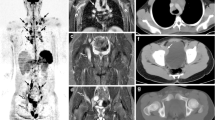
Currently, computed tomography (CT) is the principal staging technique utilized for patients with lymphoma, and it is at the basis of the Cotswold staging classification for HL [2]. It is widespread, readily available, easy to perform, reliable and reproducible, and there is evidence for its diagnostic and therapeutic impact in large series of patients [3]. However, this imaging modality also has several limitations given that interpretation of nodal involvement is based only on anatomic criteria such as size and shape, making it often impossible to discriminate lymphoma lesions from benign CT abnormalities [4]. 2-[Fluorine-18]fluoro-2-deoxy-d-glucose Positron Emission Tomography (FDG-PET) is a functional imaging technique based on glucose metabolic activity, which is increased in most malignant tumors and in HL. FDG-PET scanning in HL has already proven its value in the assessment of residual masses after treatment and for the detection of early relapse [5, 6, 7], and the prognostic significance of an interim PET after two cycles of ABVD has been recently reported [8, 9]. Several studies have investigated the role of FDG-PET in the staging of lymphomas [10–16], but the majority of those comparing the results of PET with other imaging modalities were retrospective and often included both HL and non-HL. A number of studies raised the problem of verification of all abnormal sites, and at least one of these studies attempted to rigorously obtain pathological confirmation of the involvement of positive sites on PET or CT [17]. In that prospective study involving patients who underwent surgical staging, PET showed sensitivity, specificity, and positive and negative predictive values of 100% for all 49 patients who underwent confirmation by excisional biopsy of abnormal lymph nodes or staging laparotomy. This study support our decision to biopsy less frequently the cases with discordant stage. In this multicentric prospective study, we investigated the contribution of PET scanning to the initial staging of HL and attempted to determine whether FDG-PET has any impact on therapeutic decision-making.
Design and methods
Patients
The study population included 186 unselected consecutive patients newly diagnosed with HL and referred from six Italian hematological institutions between January 2002 and June 2005. All patients were staged at baseline with blood tests (liver and renal function, complete and differential blood count, echocardiography), unilateral bone marrow trephine biopsy and aspirate, CT scan, and FDG-PET scan. Bulky disease was defined as a mediastinal mass that exceeded one third of the maximum intra-thoracic diameter or a lymph node mass larger than 7 cm. Treatment for stages I and IIA consisted of three to four courses of ABVD followed by involved field radiotherapy, six to eight cycles of ABVD were performed in patients with more advanced stage disease.
FDG-PET imaging
FDG-PET scans were performed with a GE Advance Nxi (multiring PET) in one center, a Discovery LS CT-PET scanner (GE Medical Systems, Milwaukee, WI, USA) operating in a two-dimensional high sensitivity mode in two centers, a Gemini CT-PET scanner operating in a 3D mode (Philips Electronics N.V., Eindhoven, Netherlands) in one center and a “full ring NaI(Tl)PET scanner” (C-PET ADAC, Philadelphia, PA,USA) in two centers.
A tracer dose of 370 MBq/70 kg was injected after a minimum 6-h fast, via a venous catheter flushed with saline. Glycemia, tested immediately before injection, was below 150 mg/dl in all patients. Whole body PET scans were registered 45–60 min after tracer delivery, post voiding, from ear to proximal femur. Neither bladder catheterization nor hyper-hydration was routinely used. Studies were processed with filtered back projection and iterative reconstruction, both with correction for attenuation. PET scans were qualitatively interpreted by experienced PET physicians. Any site of increased uptake not due to physiological uptake was considered as a possible lymphoma site and was reported on a data sheet.
CT imaging
CT study included both unenhanced and enhanced scanning after the administration of iodinated intravenous contrast medium (140–150 ml, iodine content 300–320 mg/ml). Injection rate was 2.5–3 ml/s, and delay time after starting bolus was 30 s for chest studies and 60 s for abdomen studies. In case of doubts in the interpretation of focal lesions, especially within the splenic or hepatic parenchyma, very delayed scans (up to 2 h) were performed. Oral iodinated contrast (about 1,000 ml) was administered about 30–40 min before examination, for better visualization of intestinal loops. Studies were performed as total body scans, inclusive of neck, chest (with parenchyma and mediastinum representation), abdomen, and pelvis, comprehensive of all lymphatic localizations. Slice thickness was 5–7 mm, and examination parameters were kept similar from scan to scan, so that images obtained were reproducible and comparable with successive controls. The assessment of lymphadenopathy on CT is based only on size, and the size criteria depend on the anatomical site: generally 10 mm in short axis has been used as a practical upper-limit in the chest and abdomen and 15 mm in inguinal, cervical, and supraclavicular nodes. Reports of CT scan done at diagnosis were contained in diagnostic CT scan data sheet.
Data analysis
The stage of the disease was determined by using the modified Ann Arbor system and was obtained with two different methods: with the use of CT scan data sheet only and blinded to PET results (CT stage), or with the use of FDG-PET scan data sheet only, blinded to CT results (PET stage). CT and PET stages were compared by hematologists with the support of radiologists and PET physicians. A concordant stage was defined as the presence of the same stage at CT and PET scan; a discordant stage was defined as the presence of a different stage at CT scan and PET scan. Patients with discordant stages were evaluated further to solve the discrepancy and obtain a final stage. These patients underwent a CT scan review and alternative imaging techniques [magnetic resonance imaging (MRI), ultrasound, others]: if these additional imaging analysis did not prove to be useful to resolve the issue, a biopsy was performed when possible. If the discordances persisted and a biopsy could not be performed, the final stage was finalized according to consensus among the physicians. In the absence of consensus, it was decided to consider the higher stage as final stage. Because bone marrow involvement could not be evaluated by CT scan, the results of PET scan were not used to evaluate bone marrow for staging purposes. In addition to stage analysis, an analysis of involved sites was performed, by comparing the results obtained with CT and PET scans. All data were analyzed using the Statistical Package for Social Science (SPSS) software. The limit of significance for all analyses was defined as a p value of 0.05. All statistical tests were two-sided.
Treatment approach
Patients were treated according to single institution protocols. All physicians were asked to clarify if the treatment was modified on the basis of the “final” stage.
Results
One hundred eighty six patients with newly diagnosed HL were included in this study. The median age was 35.2 years (14–79), male to female ratio was 98:88; bulky disease was recorded in 51 patients. The histological subtypes were LP in 11, NS in 140, MC in 28, LD in 2, and HD not specified in 5 patients. The median interval between CT and FDG-PET scans was 3 days (range, 1–12 days). A total of 910 involved sites were registered with the CT scan; 1,090 involved sites were evaluated with FDG-PET scan. Considering both imaging methodologies, a total of 1,098 involved sites were identified, with a median of 6 sites per patient.
Stage analysis
According to CT scan, 11 patients presented at stage I, 112 at stage II, 42 at stage III, and 21 at stage IV. According to PET scan, 11 patients presented at stage I, 100 at stage II, 38 at stage III, and 37 at stage IV. These data are reported in Table 1. CT and PET stages were concordant in 156 patients (84%). In 30 patients, CT and PET stages were discordant: 27 of them had a higher PET stage, the remaining 3 had a higher CT stage.
Each of the 30 patients whose scans initially yielded discordant stage results underwent MRI or ultrasound scanning and/or a review of their CT scan to further evaluate the discordant sites and obtain a final stage: in 28 patients (93%), these non-invasive evaluations were able to solve the discordances; in the remaining two patients, a consensus was needed. Considering all the discordant stage patients, the obtained final stage was in 1 patient with CT stage I and PET stage III, the final stage was III; in 9 patients with CT stage II and PET stage III, the final stage was III; 13 patients had CT stage III and PET stage IV, in 12 of them the final stage was IV; and in 1 was III; 4 patients had CT stage II and PET stage IV, and the final stage was IV in 3 patients and II in 1 patient; in 1 patient with CT stage III and PET stage II, the final stage was III; 1 patient with CT stage II and PET stage I, the final stage was II and a patient with CT stage IV and PET stage II, the final stage was IV. Therefore, according to the final stage, 25 patients were correctly upstaged by PET, 2 were incorrectly upstaged by PET, and three patients were incorrectly downstaged by PET. As expected, CT review ended frequently in confirmation of the PET result suggesting that PET reading is more easy. Characteristics of these patients are represented in Table 2.
Sites analysis in patients with concordant stage
In 156 patients, CT and PET stages were concordant. In 110 of them (71%), CT and PET showed the same sites of disease; a difference in the number of sites involved was found in 46 patients (29%). In eight patients, CT showed more lesions than FDG-PET: four of them had one more nodal lesion, the other four had one more extranodal site (lung, pericardium, breast, and liver). The patient with breast localization of the disease was submitted to a biopsy, and histological report confirmed the diagnosis of HL. FDG-PET showed more lesions than CT in 38 patients. The extra sites were only nodal in 32 patients, nodal and extranodal (bone and liver) in 2 patients, splenic and extranodal (bone and liver) in 2 patients, nodal and splenic in 1 patient, and splenic alone in 1 patient. FDG-PET was able to identify 75 more nodal sites, 4 spleen, 2 liver, and 2 cortical bone localizations than CT.
Sites analysis in patients with discordant stage
In 30 patients (16%), CT and PET stages were discordant. Higher PET stages were due to the detection of increased FDG uptake in small-size lymph nodes, spleen, cortical bone, liver, lung, and pleura. The extra sites were exclusively nodal in 9 patients, nodal and extranodal in 5 patients, splenic and extranodal in 1 patient, nodal and splenic in 2 patients, extranodal alone in 11 patients, splenic alone in 1 patient, and nodal, extranodal, and splenic in 1 patient. In 12 patients, FDG-PET identified a cortical bone FDG-PET positivity. No statistically significant differences were found between discordant cases and the following characteristics: sex, symptoms, bulky disease, and PET scanner. In particular, different histological subtypes were not associated with upstaging PET (p, 0.6). We also compared centers in which PET/CT was utilized (56 patients) and the others (130 patients): discordant cases were 10 (18%) and 20 (15%), respectively (p, 0.8).
Bone marrow involvement
In 7 of the 11 patients with FDG-PET suspected bone marrow invasion, a focal pattern of FDG uptake was displayed, and 5 out these 7 patients (71%) also had a positive bone marrow trephine biopsy. In the remaining four patients, the marrow FDG uptake showed a diffuse pattern, and in all these cases, bone marrow trephine biopsy was negative for lymphoma infiltration. One patient with positive bone marrow biopsy showed a negative FDG-PET scan.
Treatment approach
Thirteen out of 186 patients (7%) had a change in their treatment strategy due to PET results. Considering the 123 patients with a localized CT stage, that is, stage I through stage IIA, 14 of them were upstaged by PET (11%) and 10 of these underwent a treatment different than that called for before upstaging (8%). In two patients with concordant stage, PET scan led to a change in the radiotherapy approach (wider field).
Discussion
The real impact of FDG-PET imaging on staging and management of lymphoma patients is still under evaluation. Several studies have investigated the role of FDG-PET in the staging of HL. These studies evaluated a limited number of patients, and the majority of them were retrospective and included both HL and non-HL patients [10–16]. Our study is, to date, the largest prospective study evaluating the role of PET scanning for the staging of HL. In our series, 30 out of 186 patients (16%) displayed a different PET stage compared to their CT stage. A CT revision or supplemental examinations led to clarification of these discrepancies, and only two cases required a consensus among hematologists and the CT and PET physicians because of the impossibility to perform a biopsy.
The addition of FDG-PET to conventional staging procedures led to the upstaging of 25 patients (13%).Thirteen of these 25 patients (52%) went from limited to advanced disease. These results are comparable with those reported in the literature and also with the data reported recently by Hutchings et al. [18] in an homogeneous series of 99 consecutive patients with diagnosis of HL. The conclusions of these authors were similar to ours but in a smaller cohort of patients.
The only way to assess with a degree of certainty whether PET positivity identifies a real site of disease is represented by histologic examination. A limit of our study is for sure the absence of histologic confirmation of presence of Hodgkin’s disease in PET positive lesions. We could not biopsy every discordant site; therefore, we decided to proceed with a revision of CT and PET images and with the use of alternative imaging methods. Young et al. [17], comparing FDG-PET, CT, needle biopsies, and staging laparatomies, demonstrated in a well-designed prospective trial that FDG-PET was a safe and effective method to stage HL. Sensitivity, specificity, and positive and negative predictive values were evaluated in relation to histological results, and their values were all 100% for FDG-PET and 20, 83, 50, and 56%, respectively for CT. These data supported our decision to perform biopsies only in very selected cases. Moreover, there is consensus over the fact that CT evaluation is not sensitive for lymph nodes less than 10 mm in diameter, but no alternative methods to the size criteria have been consistently adopted and, to date, lymph nodes larger than 10–15 mm are generally considered as involved without the need of histological confirmation.
To note that in 14 patients, PET was able to detect unknown bone lesions, in 12 out 14, a MRI confirmed this localization. Based on this data, we recommended searching carefully for abnormal uptake in the bone.
Several studies have tested the ability of FDG-PET to evaluate bone marrow infiltration [13, 19]. A recent meta-analysis has demonstrated that FDG-PET has good but not excellent concordance with the results of bone marrow biopsy [20]. Our data confirm that FDG-PET may be complementary to bone marrow biopsy. In particular, focal positivity within the bone marrow on the FDG-PET scan could be used to indicate, and to perform, a targeted bone marrow biopsy.
The clinical implications of stage changes by PET are not always clear-cut [21]. The influence of FDG-PET on treatment strategy varies markedly in different studies, and the impact on patient management still remains to be determined [22]. A minor stage change (e.g., from stage I to II) may not have any added value because the treatment does not get changed. Major stage changes (e.g., from stage II to III or IV) indicate more widespread disease. In our study, 37% of patients (11/30) with discordant stage underwent a change in their treatment strategy; all of these 11 who changed therapy had major stage changes. In two patients with concordant stage but with more PET-positive sites, this data helped tailor radiation therapy.
In contrast with previous reports [12], we observed that histological subtype was not associated in discordant stage with upstaging PET (p, 0.6).
Moreover, the recent introduction of PET/CT seems to have become important to choose the most appropriate staging algorithm. It is interesting to note that in both NHL and HL, PET with CT upstages the original stage, based on CT alone, more often when the original stage is I or II, rather than III or IV [13, 15]. In our experience, we did not observe any differences between the two centers that utilized PET/CT and the others. A recent meta-analysis of 20 studies [23] indicated that FDG-PET is an effective method of staging, showing a high positivity and specificity. According to the authors, clinicians should consider adding FDG-PET to the routine staging workup of patients with lymphoma. In the paper by Cheson et al. [24] recently published, PET is strongly recommended before treatment in potentially curable lymphoma to better define the extension of disease. The authors concluded that this is not mandatory because of limitations imposed by costs and availability. Although our study is lacking on histological confirmation of PET positive lesions, we can conclude that this large prospective and multicentric study demonstrated that FDG-PET is a safe and effective method of staging. The major advantage of PET over conventional imaging in the staging setting is its ability to detect disease in structures lacking morphological abnormality or structures less assessable with CT scan (for example, bone lesions). Hence, upstaging of disease is the most common benefit of integrating PET into the staging of HL as it can lead to changes in the therapeutic approach. It is reasonable to assume that upstaging by PET is an indicator of more widespread disease in about 20% of patients at diagnosis, and PET could be used to modify treatment strategy in more than two thirds of patients with discordant stage.
References
Donaldson SS, Hancock SL, Hoppe RT (1999) The Janeway lecture. Hodgkin’s disease-finding the balance between cure and late effects. Cancer J Sci Am 5:325–333
Lister TA, Crowther D, Sutcliffe SB, Glatstein E, Canellos GP, Young RC, Rosenberg SA, Coltman CA, Tubiana M et al (1989) Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin’s disease: Cotswolds meeting. J Clin Oncol 7:1630–1636
Vinnicombe SJ, Reznek RH (2003) Computerised tomography in the staging of Hodgkin’s disease and non-Hodgkin’s lymphoma. Eur J Nucl Med Mol Imaging 30(Suppl 1):S42–S55
Carrington B (1998) Lymph nodes. In: Husband JE, Reznek RH (eds) Imaging in oncology. Isis Medical Media, Oxford, pp 729–748
Jerusalem G, Beguin Y, Fassotte MF, Najjar F, Paulus P, Rigo P, Fillet G (1999) Whole-body positron emission tomography using 18F-fluorodeoxyglucose for post-treatment evaluation in Hodgkin’s disease and non-Hodgkin’s lymphoma has higher diagnostic and prognostic value than classical computed tomography scan imaging. Blood 94:429–433
Jerusalem G, Beguin Y, Fassotte MF, Belhocine T, Hustinx R, Rigo P, Fillet G (2003) Early detection of relapse by whole-body positron emission tomography in the follow-up of patients with Hodgkin’s disease. Ann Oncol 14:123–130
Rigacci L, Castagnoli A, Dini C, Carpaneto A, Matteini M, Alterini R, Carrai V, Nassi L, Bernardi F, Pieroni E, Bosi A (2005) 18FDG-positron emission tomography in post treatment evaluation of residual mass in Hodgkin’s lymphoma: long term results. Oncol Rep 14:1209–1214
Gallamini A, Rigacci L, Merli F, Nassi L, Bosi A, Capodanno I, Luminari S, Vitolo U, Sancetta R, Iannitto E, Trentin L, Stelitano C, Tavera S, Bigi A, Castagnoli A, Versari A, Gregianin M, Pelosi E, Torchio P, Levis A (2006) The predictive value of positron emission tomography scanning performed after two courses of standard therapy on treatment outcome in advanced stage Hodgkin’s disease. Haematologica 91:475–481
Hutchings M, Loft A, Hansen M, Pedersen LM, Buhl T, Jurlander J, Buus S, Keiding S, D’Amore F, Boesen AM, Berthelsen AK, Specht L (2006) FDG-PET after two cycles of chemotherapy predicts treatment failure and progression-free survival in Hodgkin lymphoma. Blood 107:52–59
Delbeke D, Martin WH, Morgan DS, Kinney MC, Feurer I, Kovalsky E, Arrowsmith T, Greer JP (2002) 2-deoxy-2-[F-18]fluoro-D-glucose imaging with positron emission tomography for initial staging of Hodgkin’s disease and lymphoma. Mol Imaging Biol 4:105–114
Jerusalem G, Beguin Y, Fassotte MF, Najjar F, Paulus P, Rigo P, Fillet G (2001) Whole-body positron emission tomography using 18F-fluorodeoxyglucose compared to standard procedures for staging patients with Hodgkin’s disease. Haematologica 86:266–273
Munker R, Glass J, Griffeth LK, Sattar T, Zamani R, Heldmann M, Shi R, Lilien DL (2004) Contribution of PET imaging to the initial staging and prognosis of patients with Hodgkin’s disease. Ann Oncol 15:1699–1704
Naumann R, Beuthien-Baumann B, Reiss A, Schulze J, Hanel A, Bredow J, Kuhnel G, Hanel M, Laniado M, Kotzerke J, Ehninger G (2004) Substantial impact of FDG PET imaging on the therapy decision in patients with early-stage Hodgkin’s lymphoma. Br J Cancer 90:620–625
Partridge S, Timothy A, O’Doherty MJ, Hain SF, Rankin S, Mikhaeel G (2000) 2-Fluorine-18-fluoro-2-deoxy-D glucose positron emission tomography in the pretreatment staging of Hodgkin’s disease: influence on patient management in a single institution. Ann Oncol 11:1273–1279
Raanani P, Shasha Y, Perry C, Metser U, Naparstek E, Apter S, Nagler A, Polliack A, Ben-Bassat I, Even-Sapir E (2006) Is CT scan still necessary for staging in Hodgkin and non-Hodgkin lymphoma patients in the PET/CT era. Ann Oncol 17:117–122
Schaefer NG, Hany TF, Taverna C, Seifert B, Stumpe KD, von Schulthess GK (2004) Non-Hodgkin lymphoma and Hodgkin disease: coregistered FDG PET and CT at staging and restaging-do we need contrast-enhanced CT. Radiology 232:823–829
Young CS, Young BL, Smith SM (1998) Staging Hodgkin’s disease with 18-FDG PET. Comparison with CT and surgery. Clin Positron Imaging 1:161–164
Hutchings M, Loft A, Hansen M, Pedersen LM, Berthelsen AK, Keiding S, D’Amore F, Boesen AM, Roemer L, Specht L (2006) Positron emission tomography with or without computed tomography in the primary staging of Hodgkin’s lymphoma. Haematologica 91:482–489
Carr R, Barrington SF, Madan B, O’Doherty MJ, Saunders CA, van der Walt J, Timothy AR (1998) Detection of lymphoma in bone marrow by whole body positron emission tomography. Blood 91:3340–3346
Pakos EE, Fotopoulos A, Ioannidis JP (2005) 18F-FDG PET for evaluation of bone marrow infiltration in staging of lymphoma: a meta-analysis. J Nucl Med 46:958–963
Kaplan LD (2002) Fluorine-18 fluorodeoxyglucose positron emission tomography for lymphoma: incorporating new technology into clinical care. Am J Med 112:262–268
Kumar R, Maillard I, Schuster SJ, Alavi A (2004) Utility of fluorodeoxyglucose-PET imaging in the management of patients with Hodgkin’s and non-Hodgkin’s lymphomas. Radiol Clin North Am 42:1083–1100
Isasi CR, Lu P, Blaufox MD (2005) A metaanalysis of 18F-2-deoxy-2-fluoro-D-glucose positron emission tomography in the staging and restaging of patients with lymphoma. Cancer 104:1066–1074
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, Coiffier B, Fisher RI, Hagenbeek A, Zucca E, Rosen ST, Stroobants S, Lister TA, Hoppe RT, Dreyling M, Tobinai K, Vose JM, Connors JM, Federico M, Dihel V (2007) Revised response criteria for malignant lymphoma. J Clin Oncol 25:579–586
Acknowledgements
We wish to thank Massimiliano Cariati for linguistic review of the manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix
Appendix
Participating institutions and principal investigators of the Intergruppo Italiano Linfomi include the following:
SOD Ematologia Azienda Ospedaliero-Universitaria Firenze (R. Alterini, V. Carrai); Oncologia Medica Ospedale Prato (S. Santini); Medicina Nucleare Azienda Ospedaliero-Universitaria Firenze (M. Matteini, L. Vaggelli); Radiodiagnostica 1 Azienda Ospedaliero-Universitaria Firenze (C. Dini); U.O.A Ematologia Azienda Ospedaliera San Giovanni Battista Torino (E. Gallo, U. Vitolo); Medicina Nucleare Azienda Ospedaliera S. Giovanni Battista Torino (E. Pelosi); Servizio di Ematologia Arcispedale S. Maria Nuova Reggio Emilia (Paolo Avanzini, Fiorella Ilariucci); SC Medicina Nucleare Arcispedale S. Maria Muova Reggio Emilia (A. Versari); S.C. Ematologia Azienda Ospedaliera S. Croce e Carle Cuneo (S. Tavera); SC Medicina Nucleare Azienda Ospedaliera S. Croce e Carle Cuneo (A. Biggi); S.C. Ematologia Azienda Ospedaliera SS Antonio e Biagio Alessandria (A. Levis); UO Ematologia Ospedale SS Giovanni e Paolo Venezia (T. Chisesi); UO Medicina Nucleare Ospedale SS Giovanni e Paolo Azienda ULSS 12 Venezia (M. Gregianin).
Rights and permissions
About this article
Cite this article
Rigacci, L., Vitolo, U., Nassi, L. et al. Positron emission tomography in the staging of patients with Hodgkin’s lymphoma. A prospective multicentric study by the Intergruppo Italiano Linfomi. Ann Hematol 86, 897–903 (2007). https://doi.org/10.1007/s00277-007-0356-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-007-0356-9