Abstract
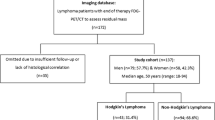
The last 25 years have seen major changes in the imaging investigation and subsequent management of patients with Hodgkin's disease (HD) and non-Hodgkin's lymphoma (NHL); accurate staging is vital for prognostication and treatment in both, and particularly in HD. The choice of imaging modality for staging depends on its accuracy, impact on clinical decision-making, and availability. Modern CT scanners fulfil most of the desired criteria. The advent of CT scanning, along with the development of ever more effective chemotherapeutic regimens, has resulted in the virtual demise of bipedal lymphangiography (LAG) as a staging tool in patients with lymphoma. It has rendered superfluous a battery of other tests that were in routine use. This contribution reviews the evidence for the use of CT in preference to LAG. CT accurately depicts nodal enlargement above and below the diaphragm, has variable sensitivity for intra-abdominal visceral involvement and is generally outstanding in depicting the extent of disease, especially extranodal extension. Despite the advances in CT technology, there are still areas where CT performs less well (e.g. disease in normal-sized lymph nodes, splenic and bone marrow infiltration). The influence of technical factors, such as the use of intravenous contrast medium, is discussed. In some instances, CT is not the imaging modality of choice and the place of newer techniques such as MRI and endoscopic ultrasound will be reviewed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prior to the development of CT scanning, patients with a diagnosis of lymphoma were subjected to a battery of diagnostic tests that included frontal and lateral chest radiography, tomography of the mediastinum and hila, skeletal surveys, isotope liver/spleen scanning, isotope bone scans, lymphangiography (LAG) and excretory urography. On top of this, most patients with Hodgkin's disease (HD) underwent staging laparotomy with its attendant risks. Very few of these tests are now performed routinely for staging.
Staging in malignant lymphoma
In order to assess the efficacy of CT as a staging tool, it is necessary to appreciate the importance of accurate staging in patients with lymphoma. Patients will usually be referred after the diagnosis of lymphoma has been established by lymph node biopsy. Staging should establish the precise local extent of disease that is clinically overt, but it should also identify occult disease elsewhere. Knowledge of the pattern of disease spread facilitates this search. In HD, the extent of disease directly influences choice of the most appropriate therapy, whereas in non-Hodgkin's lymphoma (NHL), therapy is influenced more by the pathological subtype of tumour, bulk of disease and symptomatology. In both HD and NHL, assessment of disease bulk provides important prognostic information, as does the presence of extranodal disease. In NHL in particular, staging provides a baseline assessment against which future imaging studies can be compared. Staging should also highlight clinical problems that may compromise delivery of treatment, such as central venous occlusion or hydronephrosis. Accurate imaging enables radiotherapy planning for localised disease. Finally, correct staging will prevent stage migration effects when phase III trials are being compared.
The Ann Arbor staging system for HD was introduced in 1970, and was modified in 1989 (Table 1) to take account of prognostic factors such as disease bulk and in recognition of the role of CT in the detection of intra-abdominal disease [1]. It can also be applied to NHL, though, as mentioned above, other factors are more important in NHL. In children with NHL, extranodal disease is commoner, with frequent involvement of the gastrointestinal tract, solid abdominal viscera and sites in the head and neck. This is recognised in Murphy's staging classification (Table 2).
Generally, choice of an imaging technique for staging will depend on probability of involvement of a site, the diagnostic performance of the test at that site and the impact a positive result will have on treatment. Sites frequently involved should be screened if the test is sufficiently accurate; if the test is inaccurate, the vigour of the search is dictated by the effect it will have on management. The ideal staging test should be sufficiently sensitive and specific, safe and atraumatic, available in a timely fashion (i.e. 1–2 weeks) and cost-effective. This presupposes that the necessary equipment, personnel and expertise are available, not to mention funding for the test. How well does CT measure up?
Assessing the value of imaging in the staging of lymphoma
There is a large volume of literature on the efficacy and effectiveness of various imaging modalities in a range of clinical situations, including CT [2]. A commonly used strategy for evaluating this is one adopted from Fineberg et al. [3], which uses a five-level evaluative hierarchy (Fig. 1). An acceptable performance at one level depends upon satisfactory performance at the preceding level. The efficacy of a test comprises the technical and diagnostic performance, whereas the effectiveness encompasses diagnostic and therapeutic impact, as described below. The cost-effectiveness provides a measure of how well the test fares in relation to utilisation of resources.
An evaluative framework for the assessment of an imaging technology (adapted from Fineberg et al. [3])
The technical performance is a measure of whether the test routinely results in anatomically faithful, reproducible images, which modern CT scanners do. Diagnostic performance is concerned with whether the test allows correct identification of the presence or absence of disease, i.e. sensitivity and specificity. These intrinsic operating characteristics are independent of disease prevalence, unlike the positive or negative predictive values of the test. Most of the available imaging literature in lymphoma relates to the diagnostic performance. A common feature of recent studies, with the demise of staging laparotomy, is the paucity of pathological "gold standards" against which to judge the diagnostic performance. The latter will also be affected by sampling error and bias. More critically, there is little in the literature on the effect of thresholding on sensitivity and specificity, i.e. receiver operator characteristic (ROC) curve analysis [4]. The effects of such analysis can be far-reaching; thus, alteration of the size criteria for calling a lymph node abnormally enlarged can profoundly affect staging of the patient (and assessment of response to treatment). Correct application of ROC curve statistics should allow selection of the best cut-off criteria in terms of the relative costs of false negative and positive diagnoses. The diagnostic impact of a test can be assessed by the influence of the test on the diagnostic confidence of the clinician and by the extent to which the new modality supersedes older established methods. The way in which CT has replaced LAG is at least in part a reflection of its diagnostic impact. The replacement of cranial CT and myelography with craniospinal MRI is another example of this.
It should be borne in mind that even if a diagnostic imaging test is outstandingly accurate, it is only of value if it influences patient management in terms of planning or delivery of therapy, or allows firm prognostication; the therapeutic impact [5]. A few studies have attempted to assess the therapeutic impact of CT in lymphoma staging, but generally, the rapid acceptance of new techniques (particularly MRI) has meant that it can be difficult to set up properly randomised, prospective controlled trials. Many studies are controlled observational studies with variable reference standards. As with all technology, assessment of the impact of CT on patient outcome will depend on the development of the modality. The influence of improvements in CT technology and scan time on the diagnostic and therapeutic impact of CT in patients with lymphoma was demonstrated by Fineberg et al. [6], who showed that CT had a diagnostic impact in 58% of lymphoma patients and a therapeutic impact in 15%, more often in NHL than HD. The overall impact increased with time as better scanners were introduced.
The health impact of any imaging technology is extremely difficult to measure and there is very little good research assessing the relationship between new techniques and patient outcome (see, for example, Modic [7]). Often, as in the routine use of CT in patients with lymphoma one can only infer that if there is a favourable therapeutic impact, the health of that patient population should improve.
Imaging of lymph node disease
CT scanning and LAG
Shortly after the first body CT scanners were introduced, it became clear that CT could detect intra-abdominal lymph node enlargement, one of the hallmarks of malignant lymphoma [8]. The earliest studies of CT in the evaluation of patients with lymphoma were published in the late 1970s [9, 10, 11, 12, 13, 14, 15, 16]. Kreel [9] reported that CT could demonstrate more accurately than LAG the extent of retroperitoneal disease, and this was confirmed by Schaner et al. [10]. They studied a small group of patients who underwent CT within 1 week of LAG. In many of their patients, who appear to have had advanced disease, LAG underestimated the volume and extent of retroperitoneal disease. CT demonstrated extranodal extension and in some patients, visceral involvement. However, they noted that LAG could detect small tumour deposits in lymph nodes that were not enlarged at CT. These preliminary reports indicated a possible role for CT, not only in staging but also in radiotherapy planning, as well as assessment of response to treatment.
A number of methodological and technical factors are common to these early studies. Numbers were generally small, scan slices were either thick (up to 13 mm) or non-contiguous with large inter-slice gaps (up to 2 cm), and scan times were extremely slow, predisposing to movement artefact. Intravenous contrast medium was either not administered or was administered as a slow infusion rather than a bolus. Thus it did not appear to be helpful in the identification of visceral involvement [12]. Importantly, the criteria for calling lymph nodes abnormal were not always specified, but often only lymph nodes larger than 1.5–2 cm were considered enlarged. Finally, pathological correlation from staging laparotomy was not always available. Therefore, it is not surprising that the general consensus was that, whilst CT was a useful adjunct, especially in advanced disease, it could not replace LAG or obviate the need for staging laparotomy.
LAG remains the only technique that demonstrates the internal architecture of a lymph node, so that it is theoretically possible to detect disease in lymph nodes that are normal in size or only minimally enlarged. Whilst lymph node enlargement is the key feature of lymphoma, it tends to be more marked in NHL than HD. Indeed, in the nodular sclerosing and lymphocyte-depleted pathological subtypes of HD, lymph nodes may even be normal in size. In the late 1970s and early 1980s, nearly all patients with HD were being subjected to staging laparotomy, and so pathological correlation, where available, generally pertains to this patient group. The anatomical and contrast resolution of first- and second-generation CT scanners was limited, as described above, so it is not unexpected that the early studies consistently showed that LAG was as good as or slightly better than CT in the detection of small-volume nodal lymphoma in the retroperitoneum and pelvis. Though CT tended to show the overall extent of disease better and could depict "off-axis" nodes occasionally, LAG was more likely to change the stage of the patient [17, 18, 19, 20, 21].
On the other hand, LAG had many disadvantages as a staging technique. It was invasive, uncomfortable and time-consuming, demanding a high level of technical expertise. It could not opacify lymph nodes above the level of L2 and gave no information on the status of off-axis lymph nodes (splenic hilar, coeliac axis, porta hepatis and mesenteric)—all of which are frequently involved with HD and NHL. Furthermore, it gave no information on extracapsular extension of disease or, of course, on visceral extranodal involvement. In one study of patients with NHL, CT and LAG influenced the clinical stage and pathological equally frequently, and much less often than bone marrow biopsy, but the results of CT and/or LAG were much more likely to influence management [21]. Even in centres where there was great expertise in LAG, overall accuracy was no more than 90% when compared to staging laparotomy (slightly higher for HD) and there was a significant false positive rate of 20%, even in HD [22].
The newer generation helical and multislice scanners are quite capable of detecting lymph nodes of 5 mm or less in diameter, even in locations like the coeliac axis and the porta hepatis. Faster scan times mean that movement artefact is no longer a problem and small prominent mesenteric lymph nodes, for example, are readily seen. In addition, the recognised upper limits of normal for lymph node size have decreased over the years. Currently accepted values are given in Table 3 [23, 24, 25, 26, 27, 28]. Were modern generation CT scans to be compared with LAG, it is likely that CT would be much more sensitive in the detection of nodal enlargement.
Even in 1983, some authors were recommending that CT should be the prime modality for staging and restaging, at least in NHL [29]. Other authors suggested that for HD, CT of the abdomen was sufficient if abnormal, whereas if it was normal, LAG was indicated as well [30, 31]. More recently, a couple of studies have retrospectively re-evaluated the role of abdominal CT and LAG in HD [32, 33]. They found that LAG conferred very little additional information because of the large number of false positive studies. Libson et al. [32] found eight false positives in a total of ten abnormal LAGs. This was attributable to reactive hyperplasia. Stomper et al. [33] used ROC curve analysis to show that increasing the threshold for lymph node enlargement at CT resulted in greater specificity at the expense of reduced sensitivity. Gallium scanning added very little to the positive or negative predictive values of CT and, more importantly, true positive LAG and gallium scans were seen only when lymph nodes were above 10 mm and 20 mm, respectively, i.e. when CT would have identified them as abnormal. It is estimated that the positive predictive value of LAG in nodes smaller than 1 cm is no more than 5%. This, coupled with the development of ever-better salvage chemotherapy, accounts for much of the decline in the number of lymphangiograms performed in most cancer centres [34]. This has been compounded recently by a general lack in radiological expertise in performing and interpreting LAG.
CT appearances of nodal lymphoma
Diagnostic criteria
One of the major limitations of CT scanning in lymphoma is that recognition of nodal involvement depends almost entirely on size criteria. The short axis diameter is accepted as being the most helpful measurement as it is the most reproducible. Detection of disease in normal-sized nodes remains impossible, though clustering of multiple normal-sized but prominent lymph nodes in areas such as the anterior mediastinum and the mesentery is suggestive of pathology. Conversely, CT cannot distinguish between enlargement due to reactive hyperplasia and involvement with lymphoma. The use of intravenous contrast medium is not helpful, a moderate degree of homogeneous enhancement being the rule [35]. Large nodal masses may occasionally demonstrate cystic change or necrosis, particularly in the anterior mediastinum, but this does not have any prognostic significance [36], nor does it necessarily indicate a certain pathological subtype, being seen in, for example, nodular sclerosing HD and mediastinal large B cell lymphoma. Similarly, calcification, though rare before therapy, can occur in large nodal masses with HD and NHL. Though seen in the more aggressive subtypes, it too does not have any prognostic import [37]. It has been suggested that in NHL, high-grade tumours tend to be more heterogeneous on pre- and post-contrast scans than low-grade tumours of comparable size [38], but the clinical implications of this are uncertain.
Alternative imaging techniques such as ultrasound do not confer any real advantages in the assessment of nodal disease. Lymphomatous nodal masses tend to be uniformly hypoechoic and often lobulated. They are usually well seen in the porta hepatis and at the splenic hilum [39], but the sensitivity of ultrasound in detecting lower para-aortic and pelvic lymph node enlargement is around 50%, rendering it inappropriate as a staging technique [39, 40, 41, 42]. Its main use is to ascertain the nature of a palpable mass and as a problem-solving tool (see below).
It was hoped that MRI might be able to detect disease in normal-sized lymph nodes because of its superior tissue contrast. Lymph nodes are readily identified, having intermediate T1 signal and high T2 signal, which is especially conspicuous when fat-suppressed or short-tau inversion recovery (STIR) techniques are used. However, to date it has not proved possible to diagnose involved lymph nodes other than by size criteria [43]. MRI performs as well as CT in the imaging of nodal disease and in some areas, such as the neck, the supraclavicular fossae, and the subcarinal and posterior mediastinal regions, it may perform better [44]. It can also have a role in the pelvis (where venous tributaries may be confused with lymph nodes [45]) and in solving problems related to nodal pathology [46]. There are reports in the literature of MRI-specific lymphographic agents in the form of ultrasmall superparamagnetic iron oxide particles, so in the future it may be possible to detect lymphomatous involvement of normal-sized lymph nodes [47, 48, 49].
Thorax and neck
In the neck, nodes with a short axis diameter greater than 1 cm are considered enlarged, and CT will often demonstrate that the extent of disease is greater than had been clinically suspected. Similarly, in the thorax, nodes over 1 cm are abnormal, though multiple smaller nodes in the anterior mediastinum are regarded with suspicion. Thoracic nodal involvement at presentation is seen much more often with HD than NHL (60–80% vs 20–40%). Careful attention should be given to the paracardiac and internal mammary regions, where nodal disease, if missed, may lie outside radiotherapy fields [50]. Identification of nodes in the posterior mediastinum should prompt a careful search for retrocrural disease [51].
It has been shown that CT will detect abnormalities in up to 7–30% of lymphoma patients with a normal chest radiograph at presentation (Fig. 2). Patients with HD who are shown to have even a moderate volume of unsuspected intrathoracic disease at CT have a poorer prognosis [52]. CT will change clinical stage in up to 16% of patients with HD and NHL, and management may be altered in up to 25%, either because of upstaging or because of greater extent of intrathoracic disease (Fig. 3) [53, 54, 55]. This is particularly the case where radiotherapy is planned [53, 55]. In other reports although there has been a therapeutic impact in up to 14% of patients with HD [56], there has been little effect on management in patients with NHL [57]. However, in the latter series there were many patients with intermediate-grade NHL who would have received systemic chemotherapy regardless, so the absence of therapeutic impact may have been a function of case mix.
Abdomen
Retroperitoneal nodal disease is seen at presentation in up to 25–35% of patients with HD and up to 55% of patients with NHL. Sites commonly involved by NHL include the mesentery, porta hepatis and splenic hilum. The presence of splenic hilar lymph node enlargement can be taken to indicate splenic involvement in NHL and HD; in the latter, the coeliac axis, splenic hilar and portacaval nodes tend to be involved (Fig. 4). In NHL nodes tend to be markedly enlarged, forming conglomerate masses, whereas in HD nodal enlargement may be minimal, complicating recognition of the affected nodes [33]. Since spread in HD tends to be contiguous via the lymphatics from one nodal group to the next, the presence of retrocrural disease should prompt close evaluation of the coeliac axis. By contrast, spread in NHL is haematogenous and, therefore, is often discontiguous. Both HD and NHL can involve any nodal group in the pelvis. The optimal use of intravenous contrast with proper attention to timing helps in the differentiation of nodal enlargement from large venous tributaries, though as mentioned above, MRI can also be helpful.
Imaging of extranodal disease by CT
Lymphoma occurs in extranodal sites in up to 40% of cases, the vast majority being NHL. The incidence is increased in patients with immunodeficiency and in the paediatric population. The abdomen is the commonest site affected, although secondary spread of lymph node disease into adjacent structures (the 'E' lesion) can occur anywhere, and is seen in both HD and NHL. Recognition of extranodal disease is important since in NHL it is an adverse prognostic factor, as recognised in the International Prognostic Index (IPI) [58].
Spleen and liver
Laparotomy data have shown that the spleen is involved in up to 30–40% of patients with HD and 10–40% of those with NHL [59, 60]. In 10% of patients presenting with HD clinically confined to the supradiaphragmatic regions, it is the sole focus of intra-abdominal disease. The sensitivity for detection of splenic involvement by any imaging modality remains disappointingly low. This is partly because involvement often takes the form of diffuse infiltration and nodules larger than 1 cm only occur in a minority. Unfortunately, splenic size is not a helpful pointer in HD since up to 33% of normal-sized spleens contain disease, whereas only 33% of moderately enlarged spleens are shown to contain disease [61]. The early series with pathological correlation quote variable sensitivities, from 11% to 50% [11, 12, 15, 17, 18, 20, 33, 62, 63]. Many of the CT studies were acquired without intravenous contrast material and one study reported that contrast made little difference to the conspicuity of splenic lesions [12]. However, contrast was administered by slow intravenous infusion. Although there are no recent studies with pathological gold standards, there is no doubt that with helical and multislice scanners and powered injectors for rapid bolus administration of intravenous contrast medium, focal lesions of the order of a few millimetres can be identified (Fig. 5). Splenic volumes and indices have not gained widespread acceptance, despite excellent results in some series [64, 65, 66]. They are somewhat cumbersome to use and other authors have found them less helpful [67]; splenic volume can be normal with clear focal involvement and can decrease in response to treatment, even if previously normal [68].
Focal nodules larger than 1 cm can be detected equally reliably by CT, ultrasound and MRI. Nodules tend to be hypodense at CT, enhance less than normal splenic parenchyma, are hypoechoic on ultrasound, and have intermediate T2 signal on MRI. Splenic hilar nodes detected by any modality indicate splenic disease. Early studies with ultrasound suggested that it was equivalent to CT [42, 69], but a more recent paper found that ultrasound was more sensitive than CT (63% vs 37%), detecting nodules down to 3 mm in size and identifying diffuse infiltration more often than CT [39]. Diffuse infiltration cannot be reliably detected by any method. Unfortunately, the intrinsic tissue contrast of MRI does not allow consistent recognition of infiltration [43]. However, intravenous superparamagnetic iron oxide (SPIO) may improve detection of focal and diffuse infiltration [70, 71].
As might be expected, diffuse hepatic infiltration is also difficult to detect with CT or, indeed, MRI [43, 72, 73]. Focal lesions can be identified with all three of the major modalities (Fig. 6), and there is some evidence that SPIO may increase the sensitivity of MRI [74, 75].
Bone marrow disease
A major weakness of CT as a staging tool is that it provides no information on the presence or absence of bone marrow disease, which by definition indicates stage IV disease. This is of course partly circumvented by bone marrow biopsy, which will be carried out as a matter of routine in patients with NHL, in whom infiltration will be found in 20–40% at presentation. Marrow involvement confers a poorer prognosis than involvement of liver, lung or osseous bone [76]. Infiltration of bone marrow is often patchy, particularly in higher-grade lymphomas, which explains the increased diagnostic yield from bilateral as compared with unilateral iliac crest bone marrow biopsies [77]. Though bone marrow biopsy changes pathological stage more often than CT in patients with NHL, this is usually from stage III to stage IV, so the therapeutic impact is often less pronounced than that of CT [21]. In HD, marrow involvement is rare, though it will develop in 5–15% during the course of the illness. Hence bone marrow biopsy or marrow imaging is not indicated at presentation.
MRI is the most sensitive imaging modality for detection of bone marrow disease, with affected areas having low T1 and high STIR signal (Fig. 7). MRI can result in upstaging in as many as 33% of patients with negative iliac crest biopsies. Occasional false-negative studies are seen, usually where there is microscopic infiltration (less than 5%) with low-grade lymphoma. Focal deposits as small as 3–5 mm can be identified [77, 78, 79, 80]. This has some clinical significance, patients with a positive MRI study having a significantly poorer prognosis regardless of the bone marrow biopsy findings [81]. One study compared MRI with immunoscintigraphy using technetium-labelled monoclonal antibodies; overall concordance was just under 90% and both were more sensitive than blind iliac crest biopsies [82]. As yet though, the clinical role of MRI in this context is undefined [83].
Disease at other extranodal sites
Although, as discussed above, there are still problems in the CT evaluation of diffuse hepatosplenic infiltration, CT is an excellent test for the detection and delineation of extranodal disease elsewhere (Fig. 8). It can reveal unsuspected pulmonary parenchymal involvement, altering planning of therapy as previously discussed. Chest wall involvement, either primary or secondary to direct invasion from a mediastinal mass, is well shown, though this is one area where MRI defines the disease better than CT, allowing more accurate planning of radiotherapy portals [84, 85]. A similar advantage for MRI is seen in cardiac involvement [86]. Though lymphomatous breast masses can be seen at CT, primary lymphoma of the breast is better assessed with mammography and ultrasound [87, 88].
Gastrointestinal tract
The gastrointestinal tract is the most common site of primary extranodal lymphoma, which is nearly always NHL. There are strict criteria for the diagnosis of primary gastrointestinal lymphoma, including the absence of hepatosplenic involvement and nodal involvement confined to the drainage area of the affected segment of gut [89]. A modified Ann Arbor classification takes this into account. CT is of proven use in the assessment of extramural disease but mucosal detail is poor (Fig. 9) [90]. Gastric MALT lymphomas, especially low-grade ones, typically result in minimal gastric wall thickening which may not be identified even with a dedicated gastric CT study utilising an oral water load and intravenous smooth muscle relaxants [91]. In this instance, endoscopic ultrasound is of value (Fig. 10) [92]. Multi-organ involvement can be seen in up to 25% of these patients and therefore extensive staging may be necessary [93]. In the small bowel, a distinct advantage of CT is that it can demonstrate the complications of lymphoma, such as obstruction, perforation and intussusception, in addition to mural thickening and secondary aneurysmal dilatation (Fig. 11). Colonic lymphoma can cause stricturing or widespread nodulation, readily recognised by CT.
Detail from a double-contrast barium meal demonstrating an extrinsic impression along the inferior margin of the gastric antrum (arrowheads). b Corresponding CT scan after oral and intravenous contrast demonstrates massive concentric gastric mural thickening with transmural extension into the perigastric fat
Kidney
All forms of renal lymphoma (seen in about 3% of patients undergoing abdominal staging scans) are well demonstrated by CT, including solitary or multiple renal masses, direct infiltration via the renal hilum, diffuse renal infiltration (Fig. 12) and perirenal masses surrounding the kidney (Fig. 13). CT will also document the presence and level of any obstruction, obviating the need for intravenous urography and isotope renography.
Pelvic viscera
Although CT will demonstrate pelvic nodal disease and pelvic masses, MRI is the modality of choice for defining lymphoma of the pelvic viscera, whether primary or secondary [94, 95, 96]. In evaluation of the testis, which may be involved primarily or secondarily with NHL in a focal or diffuse form, ultrasound and MRI appear equivalent [97].
Central nervous and musculoskeletal systems
Finally, MRI is the method of choice for evaluation of the neuraxis and musculoskeletal lymphoma. MRI, with its multiplanar capability, offers outstanding depiction of both intra-axial and extra-axial disease (Fig. 14). Though MRI and CT have equivalent sensitivities in primary intracerebral lymphoma, MRI can demonstrate much more subtle subdural and epidural disease within the cranium and the spinal column [98, 99, 100, 101]. True primary musculoskeletal lymphoma is rare and is nearly always NHL. Isotope scintigraphy is more sensitive than plain radiography, but MRI will demonstrate the extent of marrow involvement and muscle infiltration, often entirely unexpected from the plain films or CT scans (Fig. 15) [102].
Coronal T2-weighted image of the sinuses with fat suppression in a patient with an aggressive paranasal NHL. There is a large mass in the nasal space and right maxillary antrum. Tumour extension into the ethmoid air cells and medial orbit is well shown, as is a breach in the floor of the anterior cranial fossa (arrowheads)
Accuracy of measurements at CT
For the purposes of assessment of response to treatment, the radiologist is often required to measure a large number of marker lesions before and after therapy. Accurate reproducible measurements are possible for well-defined tumour masses (such as nodal masses) with modern CT scanners. However, it should be recognised that there is significant inter-observer variation (up to 15%), even when the same marker lesion is used [103]. This variation is even more pronounced with irregular masses or where there is poor lesion to background contrast, which is often the case even with optimisation of scan parameters such as narrow collimation slices, overlapping reconstructions and adequate contrast enhancement.
CT technique
In the era of second- and third-generation scanners there was much debate in the literature on the desirable scan parameters for staging patients with lymphoma. The importance of adequate bowel opacification with dilute oral contrast (so as to avoid confusion with intra-abdominal and pelvic masses) was well recognised. It was argued that administration of intravenous contrast medium was unnecessary unless there was any doubt regarding the presence of disease in the mediastinum, hila or liver and spleen on the non-contrasted scans [104]. In the interests of scan time and, to a lesser extent, radiation dose, it was also argued that if thin 8-mm slices were used, it was acceptable to have an inter-slice gap, especially in NHL, where affected lymph nodes tend to be large. In one fairly recent study this had little detrimental effect [105] on abdominopelvic staging. It was also suggested that in patients with HD and no evidence of disease in the abdomen, it is not necessary to scan the pelvis [106]. In point of fact, these strategies saved very little in time, resource and radiation dose.
With the advent of helical and multislice scanners these debates have become irrelevant. Most centres will obtain 5-mm collimation contiguous scans through the neck and 7.5-mm scans through the chest, abdomen and pelvis. Intravenous contrast medium facilitates nodal recognition in the neck and in the retroperitoneum in patients with a paucity of adipose tissue. The speed of modern scanners is such that it is possible to obtain scans with optimal parenchymal and vascular enhancement throughout the neck, chest, abdomen and pelvis after a single bolus injection of contrast. It is unrealistic to expect that hepatosplenic involvement could be detected consistently without intravenous contrast.
The necessity for other staging tests such as MRI and endoscopic and testicular ultrasound will then be dictated by symptomatology, the primary site of disease and the tumour subtype. For instance, there is a high incidence of CNS disease with primary testicular and head and neck NHL; NHL of Waldeyer's ring is associated with GI tract involvement and endoscopy may be necessary; in head and neck NHL, MRI will demonstrate intracranial extension far better than CT.
Recent advances
There is as yet no significant literature on the effect that developments in scan technology have had on the staging of lymphoma. Multislice scanners facilitate research into perfusion and permeability of lymphomatous masses, and there has been some experimental work relating permeability to tumour grade and activity [107]. The clinical application of this work remains to be seen. Of more immediate interest is the prospect of multimodality image registration, which has the potential to allow detection of tumour in normal-sized lymph nodes and to define the anatomical location of abnormal tracer uptake [108].
For the foreseeable future it seems unlikely that there will ever be sufficient numbers of MR scanners for whole-body ultrafast MRI to become a routine staging tool, at least in the UK, despite the theoretical advantages in terms of bone marrow status, tumour burden, tissue-specific contrast agents and radiation dosage.
Conclusion
CT remains the basic staging tool for patients with lymphoma, with good reason. It is widely available, quick, reliable and reproducible. There is fairly good evidence for its diagnostic and therapeutic impact. However, it can only define anatomy (albeit exquisitely), and the contrast inherent in the technology is insufficient for the depiction of small volumes of tumour in normal-sized structures and of microscopic diffuse infiltration, particularly in the reticuloendothelial system. Nonetheless, alternative staging techniques are unlikely to be more efficacious or effective unless they can perform better than CT in these areas.
References
Lister TA, Crowther D, Sutcliffe SB, et al. Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin's disease: the Cotswold meeting. J Clin Oncol 1989; 7:1630–1636.
Mackenzie R, Dixon AK. Measuring the effects of imaging: an evaluative framework. Clin Radiol 1995; 50:513–518.
Fineberg HV, Bauman R, Sosman M. Computerised cranial tomography: effect on diagnostic and therapeutic plans. J Am Med Assoc 1977; 238:224–227.
Goldin J, Sayre JW. A guide to clinical epidemiology for radiologists. Part II. Statistical analysis. Clin Radiol 1996; 51:317–324.
Kelsey Fry I. Who needs high technology? Br J Radiol 1984; 57: 765–772
Fineberg HV, Wittenberg J, Ferrucci JT et al. The clinical value of body computed tomography over time and technologic change. Am J Roentgenol 1983; 141:1067–1072.
Modic MT. Outcomes research, appropriateness and pragmatism in neurologic MR imaging. J Magn Reson Imaging 1994; 4:26.
Kreel L. Computerised tomography using the EMI general purpose scanner. Br J Radiol 1977; 50:2–14.
Kreel L. The EMI whole body scanner in the demonstration of lymph node enlargement. Clin Radiol 1976; 27:421–429.
Schaner EG, Head GL, Doppman JL, Young RC. Computed tomography in the diagnosis, staging and management of abdominal lymphoma. J Comput Assist Tomogr 1977; 1:176–180.
Redman HC, Glatstein E, Castellino RA, Federal WA. Computed tomography as an adjunct in the staging of Hodgkin's disease and non-Hodgkin's lymphomas. Radiology 1977; 124:381–385.
Alcorn FS, Mategrano VC, Petasnick JP, Clark JW. Contributions of computed tomography in the staging and management of malignant lymphoma. Radiology 1977; 125:717–723.
Breiman RS, Castellino RA, Harell GS, et al. CT-pathologic correlations in Hodgkin's disease and non-Hodgkin's lymphoma. Radiology 1978; 126:159–166.
Jones SE, Tobias DA, Waldman RS. Computed tomographic scanning in patients with lymphoma. Cancer 1978; 41:480–486.
Best JK, Blackledge G, Forbes WS, et al. Computed tomography of abdomen in staging and clinical management of lymphoma. Br Med J 1978; 2:1675–1677.
Lee JKT, Stanley RJ, Sagel SS, Levitt RG. Accuracy of computed tomography in detecting intraabdominal and pelvic adenopathy in lymphoma. Am J Roentgenol 1978; 131:311–315.
Earl HE, Sutcliffe SB, Kelsey Fry I, et al. Computerised tomographic (CT) abdominal scanning in Hodgkin's disease. Clin Radiol 1980; 31:149–153.
Castellino RA, Hoppe RT, Blank N, et al. Computed tomography, lymphography and staging laparotomy: correlations in initial staging of Hodgkin's disease. Am J Roentgenol 1984; 143:37–41.
Enig B, Jensen BB, Madsen EH et al. Detection of neoplastic lymph nodes in Hodgkin's disease and non-Hodgkin lymphoma. Acta Radiol 1985; 24:491–495.
Strijk SP. Lymphography and abdominal computed tomography in the staging of non-Hodgkin lymphoma. Acta Radiol 1987; 28:263–269.
Pond GD, Castellino RA, Horning S, Hoppe RT. Non-Hodgkin lymphoma: influence of lymphography, CT and bone marrow biopsy on staging and management. Radiology 1989; 170:159–164.
Marglin S, Castellino RA. Lymphographic accuracy in 632 consecutive previously untreated cases of Hodgkin disease and non-Hodgkin lymphoma. Radiology 1981; 140:351–353.
Tart RP, Mukherji SK, Avino AJ, et al. Facial lymph nodes: normal and abnormal CT appearance. Radiology 1993; 188:695–700.
van der Brekel MWM, Stel HV, Castelijns JA, et al. Cervical lymph node metastasis: assessment of radiological criteria. Radiology 1990; 177:379–384.
Glazer GM, Gross BH, Quint LE, et al. Normal mediastinal lymph nodes: number and size according to American Thoracic Society mapping. Am J Roentgenol 1985; 144:261–265.
Dorfmann RE, Alpern MB, Gross BH, Sandler MA. Upper abdominal lymph nodes: criteria for normal size determined with CT. Radiology 1991; 180:319–322.
Callen PW, Korobkin M, Isherwood I. CT evaluation of the retrocrural, prevertebral space. Am J Roentgenol 1977; 129:907–910.
Vinnicombe S, Norman A, Husband JE, et al. Normal pelvic lymph nodes: documentation by CT scanning after bipedal lymphangiography. Radiology 1995; 194:349–355.
Neumann CH, Robert NJ, Canellos G, Rosenthal D. Computed tomography of the abdomen and pelvis in non-Hodgkin lymphoma. J Comput Assist Tomog 1983; 7:846–850.
Shiels PA, Stone J, Ash DV, et al. Priorities for computed tomography and lymphography in the staging and initial management of Hodgkin's disease. Clin Radiol 1984; 35:447–449.
Strijk SP, Boetes C, Rosenbusch G, Ruijs J. Lymphography and abdominal computed tomography in staging Hodgkin's disease. Fortschr Röntgenstr 1987; 146:312–318.
Libson E, Polliack A, Bloom RA. Value of lymphangiography in the staging of Hodgkin lymphoma. Radiology 1994; 193:757–759.
Stomper PC, Cholewinski SP, Park J, Bakshi SP. Abdominal staging of thoracic Hodgkin disease: CT–Lymphangiography–Ga67 scanning correlation. Radiology 1993; 187:381–386.
Moskovic E, Fernando I, Blake P, Parsons C. Lymphography—current role in oncology. Br J Radiol 1991; 64:422–427.
Pombo F, Rodriguez E, Caruncho MV, et al. CT attenuation values and enhancing characteristics of thoracoabdominal lymphomatous adenopathies. J Comput Assist Tomogr 1994; 18:59–62.
Hopper KD, Diehl LF, Cole BA, et al. The significance of necrotic mediastinal lymph nodes on CT in patients with newly diagnosed Hodgkin disease. Am J Roentgenol 1990; 155:267–270.
Apter S, Avigdor A, Gayer G, et al. Calcification in lymphoma occurring before therapy: CT features and clinical correlation. Am J Roentgenol 2002; 178:935–938.
Rodriguez M, Rehn SM, Nyman RS, et al. CT in malignancy grading and prognostic prediction of non Hodgkin's lymphoma. Acta Radiol 1999; 40:191–197.
Munker R, Stengel A, Stäbler A, et al. Diagnostic accuracy of ultrasound and computed tomography in the staging of Hodgkin's disease. Cancer 1995; 76:1460–1466.
Clouse ME, Harrison DA, Grassi CJ, et al. Lymphangiography, ultrasonography and computed tomography in Hodgkin's disease and non Hodgkin's lymphoma. J Comput Assist Tomogr 1985; 9:1–8.
Magnusson A, Erikson B, Hemmingsson A. Investigation of retroperitoneal lymph nodes in Hodgkin's disease. Upsala J Med Sci 1984; 89:205–212.
Neumann CH, Robert RJ, Rosenthal D, Canellos G. Clinical value of ultrasonography for the management of non-Hodgkin lymphoma patients as compared with abdominal computed tomography. J Comput Assist Tomogr 1983; 7:666–669.
Nyman R, Rehn S, Ericsson A, et al. An attempt to characterise malignant lymphoma in spleen, liver and lymph nodes with magnetic resonance imaging. Acta Radiol 1987; 28:527–533.
Dooms GC, Hricak H, Crooks LE, et al. Magnetic resonance imaging of the lymph nodes: comparison with CT. Radiology 1984; 153:719–728.
Lee JKT, Heiken JP, Ling D, et al. Magnetic resonance imaging of abdominal and pelvic lymphadenopathy. Radiology 1984; 153:181–188.
Greco A, Jeliffe AM, Maher JE, Leung AWL. MR imaging of lymphomas: impact on therapy. J Comput Assist Tomogr 1988; 19:785–791.
Weissleder R, Elizondo G, Wittenberg J, et al. Ultrasmall superparamagnetic iron oxide: an intravenous contrast agent for assessing lymph nodes with MR imaging. Radiology 1990; 175:494–498.
Vassallo P, Matei C, Heston WD, et al. AMI-227-enhanced MR lymphangiography: usefulness for differentiating reactive from tumor-bearing lymph nodes. Radiology 1994; 193:501–506.
Bellin MF, Roy C, Kinkel K, et al. Lymph node metastases: safety and effectiveness of MR imaging with ultrasmall superparamagnetic iron oxide particles—initial clinical experience. Radiology 1999; 207:799–808.
Jochelson MS, Balikian JP, Mauch P, et al. Peri- and paracardiac involvement in lymphoma in a radiographic study of 11 cases. Am J Roentgenol 1983; 140:483–488.
Grossman H, Winchester PH, Bragg DG, et al. Roentgenographic changes in childhood Hodgkin's disease. Am J Roentgenol 1970; 108:354–364.
North LB, Fuller LM, Hagemeister FB, et al. Importance of initial mediastinal adenopathy in Hodgkin disease. Am J Roentgenol 1982; 138:229–235.
Gallagher CJ, White FE, Tucker AK, et al. The role of computed tomography in the detection of intrathoracic lymphoma. Br J Cancer 1984; 49:621–629.
Khoury MB, Godwin JD, Halvorsen R, et al. Role of chest CT in non-Hodgkin lymphoma. Radiology 1986; 158:659–662.
Hopper KD, Maj MD, Diehl LF, et al. Hodgkin disease: clinical utility of CT in initial staging and management. Radiology 1988; 169:17–22.
Castellino RA, Blank N, Hoppe RT, Cho C. Hodgkin disease: contributions of chest CT in the initial staging evaluation. Radiology 1986; 160:603–605.
Castellino RA, Hilton S, O'Brien J, Portlock CS. Non-Hodgkin lymphoma: contribution of chest CT in the initial staging evaluation. Radiology 1996; 199:129–132.
Shipp M, Harrington D, Anderson J, et al. Development of a predictive model for aggressive lymphoma: the International NHL Prognostic Factors Project. N Engl J Med 1993; 329:987–994.
Kadin ME, Glatstein EJ, Dorfman RE. Clinicopathologic studies in 117 untreated patients subject to laparotomy for the staging of Hodgkin's disease. Cancer 1977; 27:1277–1294.
Castellino RA, Goffinet DR, Blank N, et al. The role of radiography in the staging of non-Hodgkin's lymphoma with laparotomy correlation. Radiology 1974; 110:329–338.
Castellino RA, Marglin S, Blank N. Hodgkin's disease, the non-Hodgkin's lymphomas and the leukaemias in the retroperitoneum. Semin Roentgenol 1980; 15:288–301.
Blackledge G, Best JKK, Crowther D, Isherwood I. Computed tomography (CT) in the staging of patients with Hodgkin's disease: a report on 136 patients. Clin Radiol 1980; 31:143–147.
Jonsson K, Karp W, Landberg T, et al. Radiologic evaluation of subdiaphragmatic spread of Hodgkin's disease. Acta Radiol 1983; 24:153–159.
Breiman RS, Beck JW, Korobkin M, et al. Volume determinations using computed tomography. Am J Roentgenol 1982; 138:329–333.
Strijk SP, Wagener DJ, Bogman NJ, et al. The spleen in Hodgkin's disease. Diagnostic value of CT. Radiology 1985; 154:753–757.
Strijk SP, Boetes C, Bogman MJ, et al. The spleen in non-Hodgkin's lymphoma. Diagnostic value of CT. Acta Radiol 1987; 28:139–144.
Hess CF, Kurtz B, Hoffmann W, Bamberg M. Ultrasound diagnosis of splenic lymphoma: ROC analysis of multidimensional splenic indices. Br J Radiol 1993; 66:859–864.
Daskalogiannaki M, Prassopoulos P, Katrinakis G, et al. Splenic involvement in lymphomas: evaluation on serial CT examinations. Acta Radiol 2001; 42:326–332.
Carroll BA. Ultrasound of lymphoma. Semin Ultrasound 1982; 111:114–122.
Weissleder R, Hahn PF, Stark DD, et al. Superparamagnetic iron oxide: enhanced detection of focal splenic tumours with MR imaging. Radiology 1988; 169:399–403.
Weissleder R, Elizondo G, Stark DD, et al. The diagnosis of splenic lymphoma by MR imaging: value of superparamagnetic iron oxide. Am J Roentgenol 1989; 152:175–180.
Weinreb JC, Brateman L, Maravilla KR. Magnetic resonance imaging of hepatic lymphoma. Am J Roentgenol 1984; 143:1211–1214.
Richards MA, Webb JAW, Reznek RH, et al. Detection of spread of malignant lymphoma to the liver at low field strength magnetic resonance imaging. Br Med J 1986; 293:1126–1128.
Stark DD, Weissleder R, Elizondo G, et al. Superparamagnetic iron oxide: clinical application as a contrast agent for MR imaging of the liver. Radiology 1988; 168:297–301.
Weissleder R, Stark DD, Elizondo G, et al. MRI of hepatic lymphoma. J Magn Reson Imaging 1988; 6:675–681.
Kaplan HS. Essentials of staging and management of the malignant lymphomas. Semin Roentgenol 1980; 15:219–226.
Döhner H, Gückel F, Knauf W, et al. Magnetic resonance imaging of bone marrow in lymphoproliferative disorders: correlation with bone marrow biopsy. Br J Haematol 1989; 73:12–17.
Shields AF, Porter BA, Churchley S, et al. The detection of bone marrow involvement by lymphoma using magnetic resonance imaging. J Clin Oncol 1987; 5:225–230.
Linden A, Zankovitch R, Theissen P, et al. Malignant lymphoma: bone marrow imaging versus biopsy. Radiology 1994; 193:757–759.
Hoane BR, Shields AF, Porter BA, et al. Comparison of initial lymphoma staging using computed tomography (CT) and magnetic resonance imaging. Am J Haematol 1994; 47:100–105.
Tsunoda S, Takagi S, Tanaka O, et al. Clinical and prognostic significance of femoral marrow magnetic resonance imaging in patients with malignant lymphoma. Blood 1997; 89:286–290.
Altehoefer C, Blum U, Bathman J, et al. Comparative diagnostic accuracy of magnetic resonance imaging and immunoscintigraphy for detection of bone marrow involvement in patients with malignant lymphoma. J Clin Oncol 1997; 15:1754–1760.
Takagi S, Tsunoda S, Tanaka O. Bone marrow involvement in lymphoma: the importance of marrow magnetic resonance imaging. Leuk Lymph 1998; 29:515–522.
Bergin CJ, Healy MV, Zincone GE, Castellino RA. MR evaluation of chest wall involvement in malignanat lymphoma. J Comput Assist Tomogr 1990; 14:928–932.
Carlsen SE, Bergin CJ, Hoppe RT. MR imaging to detect chest wall and pleural involvement in patients with lymphoma: effect on radiotherapy planning. Am J Roentgenol 1993; 160:1191–1195.
Tesoro-Tess JD, Biasi S, Balzarini L, et al. Heart involvement in lymphomas. The value of magnetic resonance imaging and 2D echocardiography at disease presentation. Cancer 1993; 72:2484–2490.
Meyer JE, Kopans DB, Long JC. Mammographic appearance of malignant lymphoma of the breast. Radiology 1980; 135:623–626.
Liberman L, Giess CS, Dershaw DD, Louie DC. Non-Hodgkin lymphoma of the breast: imaging characteristics and correlation with histopathological findings. Radiology 1994; 192:157–160.
Dodd GD. Lymphoma of the hollow abdominal viscera. Radiol Clin North Am 1990; 28:771–783.
Megibow AJ, Balthazar EJ, Naidich DP, et al. Computed tomography of gastrointestinal lymphoma. Am J Roentgenol 1983; 141:541–543.
Kessar P, Norton A, Rohatiner AZ, et al. CT appearances of mucosa-associated lymphoid tissue (MALT) lymphoma. Eur Radiol 1999; 9:693–696.
Fujishima H, Chijiiwa Y. Endoscopic ultrasound staging of primary gastric lymphoma. Abdom Imaging 1996; 21:192–194.
Raderer M, Vorbeck F, Formanek M, et al. Importance of extensive staging in patients with mucosa-associated lymphoid tissue (MALT)-type lymphoma. Br J Cancer 2000; 83:454–457.
Yeoman LJ, Mason MD, Olliff JFC. Non-Hodgkin's lymphoma of the bladder—CT and MRI appearances. Clin Radiol 1991; 44:389–392.
Jenkins N, Husband JE, Sellars N, Gore M. MRI in primary non-Hodgkin's lymphoma of the vagina associated with a uterine congenital anomaly. Br J Radiol 1997; 70:219–222.
Glazer HS, Lee JK, Balfe DM, et al. Non-Hodgkin lymphoma: computed tomographic demonstration of unusual extranodal involvement. Radiology 1983; 149:211–217.
Thurnher S, Hricak H, Carroll PR, et al. Imaging the testis: comparison between MR imaging and ultrasound. Radiology 1988; 167:631–636.
Zimmerman RA. Central nervous system lymphoma. Radiol Clin North Am 1990; 28:697–721.
Chamberlain MC, Sandy AD, Press GA. Leptomeningeal metatstasis: a comparison of gadolinium-enhanced MR and contrast-enhanced CT of the brain. Neurology 1990; 40:435–438.
Yousem DM, Patrone PM, Grossman RI. Leptomeningeal metastases: MR evaluation. J Comput Assist Tomogr 1990; 14:255–261.
MacVicar D, Williams MP. CT scanning in epidural lymphoma. Clin Radiol 1991; 43:95–102.
Stroszczynski C, Oellinger J, Hosten N, et al. Staging and monitoring of malignant lymphoma of the bone: comparison of67Ga scintigraphy and MRI. J Nucl Med 1999; 40:387–393.
Hopper KD, Kasales CJ, Van Slyke MA. Analysis of interobserver and intraobserver variability in CT tumour measurements. Am J Roentgenol 1996; 167:851–854.
Johnson RJ, Husband JE. Lymphoma. In: The use of CT in the initial investigation of common malignancies. Royal College of Radiologists, 1994.
Naik KS, Spencer JA, Craven CM, et al. Staging lymphoma with CT: comparison of contiguous and alternate 10 mm slice techniques. Clin Radiol 1998; 53:523–527.
Aisen MA, Gross BH, Glazer GM, Amendola MA. Distribution of abdominal and pelvic Hodgkin disease: implications for CT scanning. J Comput Assist Tomogr 1985; 9:463–465.
Dugdale PE, Miles KA, Bunce I, et al. CT measurement of perfusion and permeability within lymphoma masses and its ability to assess grade, activity and chemotherapeutic response. J Comput Assist Tomogr 1999; 23:540–547.
Wahl RL, Quint LE, Cieslak RD, et al. "Anatometabolic" tumour imaging: fusion of FDG PET with CT or MRI to localize foci of increased activity. J Nucl Med 1993; 34:1190–1197.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vinnicombe, S.J., Reznek, R.H. Computerised tomography in the staging of Hodgkin's disease and non-Hodgkin's lymphoma. Eur J Nucl Med Mol Imaging 30 (Suppl 1), S42–S55 (2003). https://doi.org/10.1007/s00259-003-1159-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-003-1159-4