Abstract
[18F]-fluorodeoxyglucose (FDG)-positron emission tomography/computed tomography (PET/CT) is considered the standard imaging modality in Hodgkin’s disease and aggressive non-Hodgkin’s lymphoma. In the European Society of Medical Oncology guidelines, FDGPET/CT is strongly recommended for staging and restaging Hodgkin’s disease and diffuse large B-cell lymphoma
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Follicular Lymphoma
- Bone Marrow Biopsy
- Salvage Chemotherapy
- Bone Marrow Infiltration
- Standard Imaging Modality
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
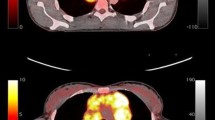
[18F]-fluorodeoxyglucose (FDG)-positron emission tomography/ computed tomography (PET/CT) is considered the standard imaging modality in Hodgkin’s disease and aggressive non-Hodgkin’s lymphoma. In the European Society of Medical Oncology guidelines, FDGPET/ CT is strongly recommended for staging and restaging Hodgkin’s disease and diffuse large B-cell lymphoma [1]. FDG-PET/CT has further been tested in monitoring during therapy, surveillance after first-line therapy, transformation assessment, and response in salvage situations and in drug development studies. However, to understand CT, especially functional imaging, in lymphoma, a profound knowledge about lymphoma biology is mandatory.
General Principles
Lymphomas are grouped into Hodgkin’s (HL) and non- Hodgkin’s (NHL) lymphoma. NHL derives from a diverse group of neoplasms: from B-cell progenitors, T-cell progenitors, mature B cells, mature T cells, or (rarely) natural killer (NK) cells. All of these different types of NHL have different clinical appearance, prognosis, therapy regimes, and FDG avidity. Aggressive NHL usually presents as a rapidly growing mass, often with symptoms of fever, weight loss, night sweats. Typical examples of aggressive NHL comprise diffuse large B-cell lymphoma, adult T-cell lymphoma, and precursor B- and T-cell lymphoblastic lymphomas or leukemias. Indolent lymphomas usually present as slow-growing masses in patients with hepatomegaly, splenomegaly, or cytopenias. Typical examples of indolent NHL are follicular lymphomas, chronic lymphocytic leukemias, and marginal-zone lymphomas. FDG-PET/CT has a different appearance in all of these subtypes.
HL, formerly called Hodgkin’s disease, has a unique composition of inflammatory cells as background and a minority of neoplastic Reed-Sternberg cells. FDGPET/ CT is used in all subforms of HL.
PET/CT in HL and NHL Staging
To plan appropriate therapies in patients with HL and NHL, accurate staging is mandatory. There are no large randomized trials to show the superiority of FDGPET/ CT over CT alone. Sensitivity and specificity of patients with HL and NHL using FDG-PET/CT is 92.2–100% and 98.8–100%, respectively [2–4]. The same studies report a sensitivity of 82–91% and 98–100%, respectively, for contrast-enhanced CT. However, there is no reported prospective study identifying any improved outcome or better overall survival in patients staged either with FDG-PET/CT or contrast-enhanced CT. These data are only valid for HL or aggressive NHL subtypes. There is no large amount of data for patients with rare lymphoma subtypes or indolent NHL.
Bone Marrow Infiltration
Bone marrow infiltration is an important predictor of survival and often guides the choice of the lymphoma therapy. There are several publications about the value of bone marrow infiltration and of FDG-PET/CT. One prospective multicenter trial, by Rigacci et al., compared the value of bone marrow biopsy (BMB) with PET/CT in HL. In a patient collective of 186, 20 patients had discordant results on BMB compared with FDG-PET/CT [5]. However, a large number of HL and NHL patients with infiltration of the bone marrow have advanced disease, positive BMB or imaging does not alter the therapy choice; thus, BMB remains the clinical routine investigation in patients with HL and NHL. In indolent NHL, in particular, FDG-PET has a high false-negative rate in assessing bone marrow infiltration.
PET/CT during Chemotherapy
Several prognostic scores are used to predict survival in lymphoma patients [6, 7]. However, these statistical considerations do not reflect response in a given patient. It is therefore important to monitor early response to determine successful from unsuccessful treatment. Several older studies prompted early midtreatment PET/CT scan to delineate responders. It has been consistently shown that midtreatment scanning has an important prognostic value [8–10]. However, more recent studies assess the role of midtreatment PET/CT more critically. In a study of diffuse large B-cell lymphoma (DLBCL), patients receiving rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone every 21 days or 14 days (R-CHOP 21; RCHOP 14), only the subgroup receiving R-CHOP 21 had a significant difference in progression-free survival [11]. In another study of 50 patients with DLBCL, interim PET/CT was considered a poor predictor [12]. It is unclear why earlier studies had different results than newer prospective trials: it may reflect the change in therapy, specifically the addition of rituximab, which entirely changed the therapeutic landscape in B-cell NHL. In HL, data on midtreatment PET/CT is more consistent: Gallamini et al. showed that PET/CT is the most important factor in prognosis, even more powerful than the International Prognostic Score [13]. Others have shown similar results [14]. There is no role for midtreatment PET/CT scanning in patients with low-grade histologies, such as follicular lymphoma, or in patients with T-cell NHL.
PET/CT in Restaging HL and NHL
The largest amount of reported data using FDG-PET/CT is in HL and NHL restaging. Several studies show the superiority of FDG-PET compared with CT due to its ability to detect viable scar tissue after the end of induction therapy. Several studies report the clinical value of a negative FDG-PET/CT after the end of first-line therapy. Spaepen et al. show that patients achieving complete FDG-negative results after first-line treatment have a median complete remission of 653 days compared with 73 days in patients with FDG avidity in the end-of-treatment scan [15]. This finding has been repeatedly reported by many authors [16, 17]. Despite this interesting finding, in which interim FDG-PET/CT does predict prognosis, there is no paper describing an adaptation of therapy according to the interim scan. There is a phase II study by the Johns Hopkins group that went directly into salvage chemotherapy in patients not achieving complete remission in the interim scan. However, it has never been shown in a randomized trial whether this method results in better overall survival. In patients with incurable lymphomas, such as low-grade follicular lymphomas, no data support the value of the interim PET/CT.
PET/CT in Surveillance after First-Line Therapy
Patients achieving complete remission after completion of first-line therapy often enter a disease-free phase and then enter a phase of regular clinical and radiological workup. PET surveillance is performed to detect early recurrence. Whereas there is no study supporting regular use of surveillance PET, Zinzani et al. [18] studied a series of patients after first-line therapy who were in complete remission after 6, 12, 18, and 24 months. A substantial number of patients with recurrence were detected. The paper provided no additional clinical data, and it is therefore unknown whether PET preceded clinical or laboratory signs of recurrence. It is furthermore not known whether recurrence detected early translates into a better overall survival for lymphoma patients. Petrausch et al. reported two retrospective series of patients with DLBCL [19] and HL [20]. These studies analyzed surveillance according to risk factors. Clinical signs of recurrence are the most important factor for predicting recurrence. According to current published data, regular PET scanning should be avoided.
PET/CT in the Salvage Chemotherapy Setting
In recurrence after first-line therapy, patients enter salvage chemotherapy followed by autologous stem cell transplantation. There is still a curative intent; however, only patients with chemosensitive disease enter the stem cell program. It is therefore important to determine whether patients benefit from salvage chemotherapy, and FDGPET does nicely fit into this treatment step. Several studies report a longer progression-free survival in patients achieving complete response after two or three cycles of salvage chemotherapy. In a meta-analysis of 12 studies with a total of 630 patients, functional imaging using PET did outperform conventional CT [21]. Still, the definitive procedure of how to treat PET-positive patients after salvage chemotherapy remains unclear. In all studies, there is a relevant subset of patients with positive PET before stem cell transplantation that achieve complete response after completion of therapy. It is therefore questionable whether patients with positive PET after salvage chemotherapy should not be transplanted. However, other risk factors must be considered as well, and alternative consolidation strategies, newer agents, and clinical trials must be considered. In patients undergoing allogeneic transplantation, there is no role for positive or negative pretransplantation scan, and the results do not predict relapse or overall survival [22].
Interpretation of PET/CT in Lymphoma
FDG-PET/CT has become a standard tool in clinical trials. It is therefore important to identify clear and precise rules of FDG-PET/CT interpretation. One question regards the use of maximum standard uptake value (SUVmax) changes compared with visual assessment in patients with lymphoma. Reduction in of 66% of SUVmax translates into better prognostic prediction compared with visual assessment [23]. That trial, among others, showed the need for harmonization of response standards in FDG-PET/CT. The International Working Group (IWG) response criteria for assessment were developed to compare results among different clinical trials [24]. Cheson et al. added the PET information in patients with aggressive NHL in a retrospective analysis, showing that PET can increase the number of complete remissions. The earlier category of complete response unconfirmed (Cru) was eliminated, and the IWGPET was initiated [25] and is now considered the standard, which is verified by several groups [26].
Conclusion
For more than a decade FDG-PET has been used to stage, restage, and follow patients with NHL and HL. Its strengths are in HL and aggressive NHL staging, early response assessment, and restaging. Few studies report FDG-PET in surveillance. FDG-PET can guide treatment for patients undergoing salvage chemotherapy prior to stem cell transplantation. Response must be assessed using the IWG-PET criteria. Overlooking most of current studies, FDG-PET is still not considered as the mandatory standard in the named indication in patients with HL and NHL. There is still not enough prospective data to definitively predict the impact of FDG-PET/CT in HL and B-cell HL patients. Future study must focus on randomized intervention studies using PET as discriminator to select minimal required therapies to treat lymphoma patients sufficiently. Until these studies are complete, FDGPET/ CT will not be a mandatory standard for all HL and NHL patients. It is furthermore important to understand that most data is published in the field of HL and aggressive B-cell NHL. There is still insufficient data for indolent and T-cell NHL by which to definitely identify the role of FDG-PET in these separate lymphoma entities.
References
Hutchings M, Loft A, Hansen M et al (2006) Positron emission tomography with or without computed tomography in the primary staging of Hodgkin’s lymphoma. Haematologica 91:482–489.
Pelosi E, Pregno P, Penna D et al (2008) Role of whole body [18F] fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) and conventional techniques in the staging of patients with Hodgkin and aggressive non-Hodgkin lymphoma. Radiol Med 113:578–590.
Bangerter M, Moog F, Buchmann I et al (1998) Whole-body 2-[18F]-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) for accurate staging of Hodgkin’s disease. Ann Oncol 9:1117–1122.
Rigacci L, Vitolo U, Nassi L et al (2007) Positron emission tomography in the staging of patients with Hodgkin’s lymphoma: a prospective multicentric study by the Intergruppo Italiano Linfomi. Ann Hematol 86:897–903.
Shipp MA, Harrington DP, Anderson JR et al (1993) Development of a predictive model for aggressive lymphoma: The International Non-Hodgkin’s Lymphoma Prognostic Factors Project. N Engl J Med 329:987–994.
Hasenclever D, Diehl V (1998) A prognostic score for advanced Hodgkin’s disease: International Prognostic Factors Project on advanced Hodgkin’s disease. N Engl J Med 339:1506–1514.
Spaepen K, Stroobants S, Dupont P et al (2002) Early restaging positron emission tomography with 18F-fluorodeoxyglucose predicts outcome in patients with aggressive non-Hodgkin’s lymphoma. Ann Oncol 13:1356–1363.
Haioun C, Itti E, Rahmouni A et al (2005) [18F]fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) in aggressive lymphoma: an early prognostic tool for predicting patient outcome. Blood 106:1376–1381.
Mikhaeel NG, Hutchings M, Fields PA et al (2005) FDG-PET after two to three cycles of chemotherapy predicts progression-free and overall survival in highgrade non-Hodgkin lymphoma. Ann Oncol 16:1514–1523.
Safar V, Dupuis J, Jardin F et al (2009) Early 18 fluourodeoxyglucose PET scan as a prognostic tool in diffuse large B-cell lymphoma patients treated with an anthracycline-based chemotherapy plus rituximab. Blood 114:45.
Cashen A, Dehdashti F, Luo J et al (2008) Poor predictive value of FDG-PET/CT performed after 2 cycles of R-CHOP in patients with diffuse large B-cell lymphoma (DLCL). Blood 112:144.
Gallamini A, Hutchings M, Rigacci L et al (2007) Early interim 2-[18F]fluoro-2-D-glucose positron emission tomography is prognostically superior to international prognostic score in advanced stage Hodgkin’s lymphoma: a report from a joint Italian-Danish study. J Clin Oncol 25:3746–3752.
Cerci JJ, Pracchia LF, Linardi CCG et al (2010) 18F-FDG PET after 2 cycles of ABVD predicts eventfree survival in early and advanced Hodgkin lymphoma. J Nucl Med 51:1337–1343.
Spaepen K, Stroobants S, Dupont P et al (2001) Prognostic value of positron emission tomography (PET) with fluorine-18 fluorodeoxyglucose ([18F]FDG) after first-line chemotherapy in non-Hodgkin’s lymphoma: is [18F]FDG-PET a valid alternative to conventional diagnostic methods? J Clin Oncol 19:414–419.
Engert A, Kobe C, Markova J et al (2010) Assessment of residual bulky tumor using FDG-PET in patients with advanced-stage Hodgkin lymphoma after completion of chemotherapy: final report of the GHSG HD15 trial. Blood 116:336.
Cerci JJ, Trindade E, Pracchia LF et al (2010) Cost effectiveness of positron emission tomography in patients with Hodgkin’s lymphoma in unconfirmed complete remission or partial remission after firstline therapy. J Clin Oncol 28:1415–1421.
Zinzani PL, Stefoni V, Tani M et al (2009) The role of FDGPET scan in the follow-up of lymphoma: experience on 421 patients. J Clin Oncol 27:1781–1787.
Petrausch U, Samaras P, Haile SR et al (2010) Risk-adapted FDG-PET/CT-based follow-up in patients with diffuse large Bcell lymphoma after firstline therapy. Ann Oncol 21:1694–1698.
Petrausch U, Samaras P, Veit-Haibach P et al (2010) Hodgkin’s lymphoma in remission afer first-line therapy: which patients need FDG-PET/CT for follow-up? Ann Oncol 21:1053–1057.
Spaepen K, Stroobants S, Dupont P et al (2003) Prognostic value of pretransplantation positron emission tomography using fluorine 18-fluorodeoxyglucose in patients with aggressive lymphoma treated with high-dose chemotherapy and stem cell transplantation. Blood 102:53–59.
Lambert JR, Bomanji JB, Peggs KS et al (2010) Prognostic role of PET scanning before and after reduced-intensity allogeneic stem cell transplantation for lymphoma. Blood 115:2763–2768.
Lin C, Itti E, Haioun C et al (2007) Early 18F-FDG PET for prediction of prognosis in patients with diffuse large B-cell lymphoma: SUV-based assessment versus visual analysis. J Nucl Med 48:1626–1632.
Cheson BD, Horning SJ, Coiffier B et al (1999) Report of an International Workshop to standardize response criteria for non-Hodgkin’s lymphomas. J Clin Oncol 17:1244–1253.
Cheson BD, Pfistner B, Juweid ME et al (2007) Revised response criteria for malignant lymphoma. J Clin Oncol 25:579–586.
Dupuis J, Itti E, Rahmouni A et al (2009) Response assessment after an inductive CHOP or CHOP-like regimen with or without rituximab in 103 patients with diffuse large B-cell lymphoma: integrating 18fluorodeoxyglucose positron emission tomography to the International Workshop Criteria. Ann Oncol 20:503–507.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Italia
About this chapter
Cite this chapter
Schaefer, N.G. (2014). Lymphoma: Management Using PET/CT. In: Hodler, J., von Schulthess, G.K., Kubik-Huch, R.A., Zollikofer, C.L. (eds) Diseases of the Abdomen and Pelvis 2014–2017. Springer, Milano. https://doi.org/10.1007/978-88-470-5659-6_34
Download citation
DOI: https://doi.org/10.1007/978-88-470-5659-6_34
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-5658-9
Online ISBN: 978-88-470-5659-6
eBook Packages: MedicineMedicine (R0)