Abstract
Purpose
Unilateral agenesis of the internal carotid artery (ICA) is a rare anatomical variant. We identified a case of unilateral ICA agenesis with interparaclinoid and contralateral carotid-ACA anastomoses.
Methods
A 65-year-old female with a long history of depressive episodes underwent MR imaging including MR angiography at National Hospital Organization Kyushu Medical Center. MR imaging was performed using a 3.0-T MR scanner to rule out vascular Parkinsonism, although drug-induced Parkinsonism was suspected from her medical history.
Results
The proximal left ICA was not visible on MR angiography, and an anterior communicating artery (ACoA) aneurysm was identified. The left middle cerebral artery was supplied from the right ICA via an interparaclinoid anastomosis. This interparaclinoid anastomosis showed no communication with the basilar, posterior communicating, or posterior cerebral arteries. A communicating artery connecting the interparaclinoid anastomosis and anterior cerebral artery (ACA) branched off from the presumed transition point between the interparaclinoid anastomosis and left ICA. Both right and left ophthalmic arteries (OAs) originated from the clinoid segment of the ICA. The communicating artery connecting the interparaclinoid anastomosis and ACA arose proximal to the left OA, and the communicating artery was identified as the carotid-ACA anastomosis.
Conclusion
Neuroradiologists, physicians, and neurosurgeons need to be aware of this extremely unusual anatomical variant to determine appropriate treatment strategies in cases of aneurysmal growth or anterior cranial base surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Agenesis of the internal carotid artery (ICA) is usually found incidentally without clinical symptoms. An association between ICA agenesis and anterior communicating artery (ACoA) aneurysm has been reported [1, 7]. The increased incidence of cerebral aneurysm formation among patients with ICA agenesis and carotid-anterior cerebral artery (ACA) anastomosis may be due to the increased hemodynamic burden on the normal side and anastomosis, respectively. It is important to be familiar with an uncommon anatomical variation with ICA agenesis and carotid-ACA anastomosis to determine appropriate treatment strategies or monitor the growth of aneurysms. Herein, we report a case of unilateral ICA agenesis with interparaclinoid and contralateral carotid-ACA anastomoses.
Case report
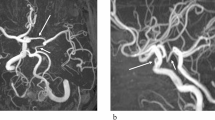
A 65-year-old female with a long history of depressive episodes underwent MR imaging including MR angiography at National Hospital Organization Kyushu Medical Center. One month before this admission, she had noticed a gradual worsening of gait disturbance and difficulty moving her left arm. Routine laboratory testing showed all results within normal limits, except for slightly elevated serum levels of total cholesterol (264 mg/dL; reference range, 128–211 mg/dL) and C-reactive protein (0.72 mg/dL; reference range, 0–0.3 mg/dL). MR imaging was performed using a 3.0-T MR scanner (Ingenia; Philips Medical Systems, Best, the Netherlands) to rule out vascular Parkinsonism, although drug-induced Parkinsonism was suspected from her medical history. Scanning parameters for 3-dimensional time-of-flight MR angiography were: repetition time, 23.0 ms; echo time, 3.45 ms; flip angle, 18°; slice thickness, 1.0 mm; slice interval, 0.5 mm; matrix size, 364 × 267; field of view, 200 × 200 mm; number of excitations, 1. The proximal left internal carotid artery (ICA) was not visible on MR angiography (Fig. 1A–C), and an anterior communicating artery (ACoA) aneurysm 2 mm in diameter was identified. The left middle cerebral artery was supplied from the right ICA via an interparaclinoid anastomosis. This interparaclinoid anastomosis showed no communication with the basilar, posterior communicating, or posterior cerebral arteries. A communicating artery connecting the interparaclinoid anastomosis and anterior cerebral artery (ACA) branched off from the presumed transition point between the interparaclinoid anastomosis and left ICA. Both right and left ophthalmic arteries (OAs) originated from the clinoid segment of the ICA (Fig. 1C). The communicating artery connecting the interparaclinoid anastomosis and ACA arose proximal to the left OA, and the communicating artery was identified as the carotid-ACA anastomosis. Imaging follow-up was selected based on the small size of the ACoA aneurysm. Her symptoms have remained stable since the first visit to our hospital.
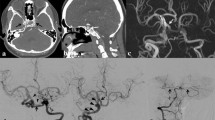
Representative MR angiography images (A–C) and schematic illustrations of Lie’s type D (D) and our case (E). A The anterior–posterior view of 3D partial volume-rendering reveals the left ICA is not visible. The ACoA aneurysm (arrowhead) 2 mm in diameter are also identified. Solid and dotted arrows indicate carotid-anterior cerebral artery (ACA) and interparaclinoid anastomoses, respectively. B The oblique view of partial maximum intensity projection indicates the left MCA is supplied from the right ICA via the interparaclinoid anastomosis (dotted arrow). The interparaclinoid anastomosis shows no communication with the basilar, posterior communicating, or posterior cerebral arteries. The solid arrow represents the carotid-ACA anastomosis. C The inferior-superior view of partial maximum intensity projection shows the positional relationship among the interparaclinoid anastomosis (dotted arrow), carotid-ACA anastomosis (solid arrow), and bilateral OAs (arrowheads). Bilateral OAs originate from the clinoid segment of the ICA. D and E The arrowhead indicates the presumed transition point between the interparaclinoid anastomosis and left ICA. The dotted artery represents the carotid-ACA anastomosis. The ACoA aneurysm was also shown by an ellipse. ACA anterior cerebral artery, ACoA anterior communicating artery, ECA external carotid artery, iCa intercavernous anastomosis, ICA internal carotid artery, iPa interparaclinoid anastomosis, MCA middle cerebral artery, OA ophthalmic artery, PCA posterior cerebral artery, VA vertebral artery
Discussion
Unilateral agenesis of the ICA is a rare anatomical variant [2, 5, 8, 9]. The absence of one or both ICAs may be entirely asymptomatic under normal conditions, due to the presence of collateral vessels [7]. The primitive ICA originates from the dorsal aorta and the third aortic arch at the 4- to 5-mm embryonic stage [3], and is completely formed by about gestational week 6 [3, 7]. Agenesis of the ICA is therefore most likely to result from atresia or involution of the third aortic arches and the distal portion of the dorsal aorta in this period. The carotid canal develops in association with the ICA. Thus, if the embryonic primordium of the ICA fails to develop before embryonic week 3–5, the ICA and the carotid canal cannot develop [7]. ICA agenesis has been classified into six types (A–F) by Lie [5]. Among these, Lie’s type D represents intercavernous or trans-sellar anastomosis [6, 9]. The interparaclinoid anastomosis in the present case resembles but differs from anatomical variants reported by Uchino et al. [9] or the Lie’s type D. Compared with the case reported by Uchino et al. [9], neither the right ICA nor the interparaclinoid anastomosis showed any communication with the basilar, posterior communicating, or posterior cerebral arteries. In addition, the interparaclinoid anastomosis in our case was well developed. Schematic illustrations indicate the difference between Lie’s type D (Fig. 1D) and our case (Fig. 1E). According to a proposal by Lasjaunias, the ICA constitutes seven segments: cervical, ascending intrapetrous, horizontal intrapetrous, ascending foramen lacerum, horizontal intra-cavernous, clinoid, and termination [4]. Each segment is located between embryonic arteries [4]. The present patient showed an interparaclinoid anastomosis that would originate more distally from the ICA than the Lie’s type D. The anatomical variant, in this case, should be distinguished from any previously reported types from Lie’s classification.
We also observed the communicating artery connecting the interparaclinoid anastomosis and ACA originating from a presumed transition point between the interparaclinoid anastomosis and the left ICA. The communicating artery in the patient was determined as carotid-ACA anastomosis. We believe carotid-ACA anastomosis is a more appropriate term than the infraoptic course of the ACA because some subjects with carotid-ACA anastomosis show a normally positioned A1 segment of the ACA [10]. The left OA in our case arose from the left ICA distal to the communicating artery. According to the hypothesis of Lasjaunias, each segment of the ICA is located between embryonic arteries and can thus potentially cause communicating arteries [4]. The carotid-ACA anastomosis in this case thus probably branched off from the junction of the cavernous-clinoid segment.
An association between ICA agenesis and ACoA aneurysm has been reported [1, 7]. The carotid-ACA anastomosis is another risk factor underlying aneurysmal formation [10]. The increased incidence of cerebral aneurysm formation among patients with ICA agenesis and carotid-ACA anastomosis may be due to the increased hemodynamic burden on the normal side and anastomosis, respectively. Increased regional blood flow along with congenital defects of the vessel wall and systemic hypertension are important factors in the development of intracranial aneurysms [7]. We will therefore continue careful and regular monitoring of this patient.
Conclusion
We identified a case of unilateral ICA agenesis with interparaclinoid and contralateral carotid-ACA anastomoses. Neuroradiologists, physicians, and neurosurgeons need to be aware of this anatomical variant, which should be distinguished from any previously reported variations.
References
Bernini FP, Cioffi FA, Muras I, Rinaldi F, Vaino R (1980) Agenesis of the right internal carotid artery associated with an aneurysm of the anterior communicating artery. Case report. Acta Neurochir (Wien) 54:257–263. https://doi.org/10.1007/BF01407093
Dinc H, Alioglu Z, Erdol H, Ahmetoglu A (2002) Agenesis of the internal carotid artery associated with aortic arch anomaly in a patient with congenital Horner’s syndrome. Am J Neuroradiol 23:929–931
Given CA 2nd, Huang-Hellinger F, Baker MD, Chepuri NB, Morris PP (2001) Congenital absence of the internal carotid artery: case reports and review of the collateral circulation. Am J Neuroradiol 22:1953–1959
Lasjaunias PL (2000) Segmental identity and vulnerability in cerebral arteries. Interv Neuroradiol 6:113–124. https://doi.org/10.1177/159101990000600205
Lie TA (1968) Congenital anomalies of the carotid arteries. Including the carotid-basilar and carotid-vertebral anastomoses: An angiographic study and a review of the literature. Excerpta Medica, Amsterdam
Mellado JM, Merino X, Ramos A, Salvado E, Sauri A (2001) Agenesis of the internal carotid artery with a trans-sellar anastomosis: CT and MRI findings in late-onset congenital hypopituitarism. Neuroradiology 43:237–241. https://doi.org/10.1007/s002340000460
Orakdogen M, Berkman Z, Ersahin M, Biber N, Somay H (2007) Agenesis of the left internal carotid artery associated with anterior communicating artery aneurysm: case report. Turk Neurosurg 17:273–276
Turnbull I (1962) Agenesis of the internal carotid artery. Neurology 12:588–590. https://doi.org/10.1212/wnl.12.9.588
Uchino A, Saito N, Kohyama S (2015) Agenesis of the internal carotid artery with paraclinoid-supraclinoid anastomosis and basilar artery-posterior communicating artery anastomosis diagnosed by magnetic resonance angiography. Surg Radiol Anat 37:685–687. https://doi.org/10.1007/s00276-014-1388-1
Uchino A, Saito N, Tanahashi N (2018) Bilateral carotid-anterior cerebral artery anastomoses associated with bilateral ophthalmic arteries arising from the anastomotic arteries diagnosed by magnetic resonance angiography: a case report. Surg Radiol Anat 40:721–725. https://doi.org/10.1007/s00276-017-1953-5
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
KY: guarantor of integrity of the entire study, manuscript preparation, literature research. MY: manuscript editing. AU: literature research, manuscript editing. TN: manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamashita, K., Yasaka, M., Uchino, A. et al. Unilateral agenesis of internal carotid artery with interparaclinoid and contralateral carotid-anterior cerebral artery anastomoses diagnosed by magnetic resonance angiography: a case report. Surg Radiol Anat 44, 289–292 (2022). https://doi.org/10.1007/s00276-021-02844-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-021-02844-0