Abstract
Purpose
To assess the safety and efficacy of percutaneous thermal ablation for the treatment of hepatocellular adenomas.
Materials and Methods
This is an ethics board-approved, single-arm, retrospective, cohort study of patients with pathologically proven hepatocellular adenomas treated with percutaneous thermal ablation at a tertiary referral center from 1999 to 2016. Demographic, procedural, and outcome data were collected and summarized with appropriate measures of central tendency and dispersion. Complications were graded per the Society of Interventional Radiology reporting guidelines. Determination of primary and secondary technique efficacies was based on post-procedural imaging.
Results
Thirty-six patients (4 male, 32 female) with a median age of 35 years had 44 procedures for the treatment of 58 tumors. Twenty-two percent of patients had prior history of adenoma-related hemorrhage. The median tumor size was 2.1 cm (range 0.6–6.0). The majority of treatments were done on an outpatient basis, under moderate sedation, using radiofrequency ablation with ultrasound guidance. The median procedure time was 85 min. There were two immediate post-procedural hemorrhages (4.5% per procedure). During a median follow-up of 1.7 years (95% CI 0.2–8.0), there were no instances of malignant transformation, adenoma-related hemorrhages, or deaths. The primary and secondary technique efficacy rates were 88 and 100%, respectively.
Conclusion
Thermal ablation for the treatment of hepatocellular adenoma had a primary and secondary efficacy of 88 and 100%, respectively. The major complication rate was 4.5%. The clinical efficacy during a median follow-up of 1.7 year was 100%.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatocellular adenomas are rare benign hepatic neoplasms with an estimated incidence of 0.3–4 per 100,000 [1]. Their clinical importance is due to a risk of hemorrhage or malignant transformation. Several management options are available including discontinuation of oral contraceptives, surgical resection, and arterial embolization [2,3,4,5,6]. Percutaneous thermal ablation, a minimally invasive procedure used routinely for the treatment of hepatocellular carcinoma, has been recently described as an option for the treatment of hepatocellular adenomas [7,8,9,10]. The purpose of this study was to assess the safety and efficacy of percutaneous thermal ablation for the treatment of hepatocellular adenomas.
Methods
Patients
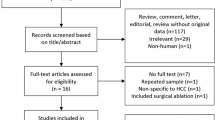
Approval for this study was received from the institutional research ethics board. The study design was a single-arm, retrospective, cohort of patients with pathologically proven hepatocellular adenomas treated with percutaneous thermal ablation at a tertiary referral center from 1999 to 2016. The radiology information system was searched for interventional radiology reports containing the word “hepatic” OR “hepatocellular” AND “adenoma” or “adenomas.” This search returned 83 unique patients. Forty-seven of these patients were excluded because they either did not have a pathological diagnosis of adenoma or were not treated with thermal ablation. Thirty-six patients constituted the final cohort.
Patients were offered ablation after consensus decision was reached at weekly liver tumor multidisciplinary case conference attended by specialists including interventional radiology, abdominal imaging radiology, hepatobiliary surgery, liver transplantation, hepatology, medical oncology, radiation oncology, and pathology. Factors taken into consideration during the decision-making process included patient age, gender, childbearing potential, tumor size, number, and location, previous hemorrhage, potential risk of hemorrhage, potential risk of malignant transformation, and medical and surgical comorbidities. Management options discussed included imaging surveillance, percutaneous ablation, and surgical resection.
Procedures
The procedures were performed under either moderate sedation or general anesthesia by one of 5 interventional radiologists with 1–39 years of experience. Using sterile technique, an RFA electrode or microwave applicator was inserted into each adenoma to be treated under ultrasound, CT, or combined guidance. A summary of the devices used is available in Table 1. The choice of guidance and approach was at the discretion of the operators. Ablation was performed per the manufacturer’s device protocol. Thermal protection using hydrodissection and overlapping ablations were performed at the discretion of the operators.
Patients were followed by liver-specific MR or CT imaging and in interventional radiology clinic typically on a schedule of 3 months, 6 months, 1 year, and then yearly. Follow-up was not standardized and was at the discretion of the operators. Complications were categorized into major and minor subgroups based on the Society of Interventional Radiology Standards criteria [11]. Assessment of primary and secondary technique efficacies was based on the presence of persistent nodular enhancement on post-procedural imaging [12].
Statistical Analysis
Demographic, histopathological, procedural, and outcome data were collected and summarized with appropriate measures of central tendency and dispersion.
Results
The 36 patients (4 male, 32 female) had a median age of 35 years (range 19–76 years). Eight of thirty-six (22%) patients had a prior history of adenoma-related hemorrhage, and 7/36 (19%) had right upper quadrant pain. The rest were asymptomatic. Thirty-three of thirty-six (92%) had one or more of the following risk factors for hepatocellular adenomas: oral contraceptives (65%), BRCA mutation (5%), hemochromatosis (3%), hyperestrogenism (3%), glycogen storage disorder (5%), alpha-1 antitrypsin deficiency (3%), and exogenous steroids (5%). All patients underwent a biopsy of at least one of the treated lesions, except in two cases of adenomatosis where the pathology results were based on a prior surgical resection. The pathological subtypes were as follows: unspecified (69%), inflammatory (22%), telangiectatic (6%), HNF1-α inactivated (3%). HNF1-α inactivation was tested in 13/36 (36%) of cases and was only positive once. β-Catenin activation was tested in 29/36 (81%) of cases and was negative in all cases.
Forty-four procedures were performed for the treatment of 58 tumors. The median tumor size was 2.1 cm (range 0.6–6.0 cm). On average, 1.4 tumors were treated per session (range 1–3). Thirty-seven of forty-four (84%) sessions were performed under moderate sedation, 1 (2%) required deep sedation (performed by an anaesthesiologist), and the remaining 6 (14%) were under general anesthesia. Ultrasound guidance alone was used in 27/44 (61%) of procedures, 16/44 (36%) used a combination of CT and ultrasound, 1/44 (2%) procedure was done with contrast-enhanced ultrasound. Eight of forty-four (18%) procedures required thermal protection of adjacent structures using hydrodissection. Overlapping ablations were performed in 14/44 (32%) of procedures (31% of RFA ablations and 38% of microwave ablations). The median ablation time per tumor treated, defined as the total time during which energy is actually inputted via the needle electrode or antenna, was 12 min (95% CI 3–46). The median procedure time was 85 min (95% CI 56–200). Thirty-eight of forty-four (86%) procedures were done on an outpatient basis. The remaining 6 procedures performed on 5 patients had a length of inpatient hospital stay of 1–6 days (2 patients had procedures that were complicated by hemorrhage, 1 patient had developmental delay, 1 was pregnant, and 1 requested overnight stay).
There were two major complications of immediate post-procedural hemorrhages (4.5% per procedure). The first patient was a 20-year-old woman with a previous history of adenoma-related hemorrhage. She underwent ablation of a 4.2-cm segment 6 adenoma (Fig. 1), using a 4.0-cm LeVeen electrode under CT guidance and general anesthesia. Overlapping ablations were performed. The patient developed increasing abdominal pain following the procedure. A CT scan was performed demonstrating active hemorrhage (Fig. 2). The patient underwent arteriography and had embolization of the right hepatic artery with absorbable gelatin sponge (Gelfoam, Pfizer, Wayne, PA) (Figs. 3 and 4). The bleeding stopped and the patient was discharged on post-procedure day 6. Final pathology was hepatocellular adenoma not otherwise specified. The patient experienced no further hemorrhage or other complications during a follow-up of 4.8 years (Fig. 5).
The second patient had ablation of a 3.1-cm segment 6 adenoma and a 1.2-cm segment 8 adenoma using a Angiodynamics Accu2i pMTA microwave applicator under ultrasound guidance and moderate sedation. The patient developed increasing abdominal pain following ablation. A CT scan was performed on the same afternoon demonstrating recent hemorrhage, but no active extravasation. The patient was managed conservatively with fluids and was discharged on post-procedure day 6. Final pathology was hepatocellular adenoma not otherwise specified. The patient experienced no further hemorrhage or other complications during a follow-up of 2.3 months.
Imaging follow-up was by modality-specific liver protocol, contrast-enhanced, CT or MR imaging as follows: MRI 16/36 (44%), CT 4/36 (11%), initial MRI and subsequent CTs 4/36 (11%), initial CT and subsequent MRIs 11/36 (31%). During a median follow-up of 1.7 years (95% CI 0.2–8.0), there were no instances of malignant transformation, adenoma-related hemorrhages (other than the two procedure-related hemorrhages described in the preceding paragraph), or deaths. The primary and secondary technique efficacy rates were 88 and 100%, respectively.
Discussion
Hepatocellular adenomas are benign neoplasms composed of plates of hepatocytes. Portal tracts and bile ducts are absent. Adenomas can contain areas of necrosis and hemorrhage. A pseudocapsule can be present. The hepatocytes can contain intracellular fat [13].
Hepatocellular adenomas were rare prior to broad use of oral contraceptives. Multiple studies have demonstrated an increased incidence of hepatocellular adenomas among women taking oral contraceptives [14,15,16]. Cessation of oral contraceptive use has been associated with tumor involution or a decrease in lesion size [17, 18]. More recent series have found additional risk factors to be anabolic steroids and other drugs, obesity, hemochromatosis, diabetes mellitus, portal vein abnormalities, and type Ia glycogen storage disease [13].
The two major potential complications of hepatocellular adenomas are hemorrhage and malignant transformation. A systematic review of a total 1176 patients by Van Aalten et al. found that hemorrhage was reported in 27.2% of patients and 15.8% of tumors. Rupture and intraperitoneal bleeding was seen in 17.5% of patients. Six articles in the review reported bleeding in tumors < 5 cm. The smallest reported bleeding tumor was 1 cm [19]. A study by Deneve et al. found that risk factors for hemorrhage are increasing tumor size (odds ratio (OR), 7.8; 95% confidence interval (CI), 2.2–26.3; p < 0.01) and recent (within 6 months) hormone use (OR, 4.5; 95% CI, 1.5–13.3; p < 0.01) [20].
The second potential complication is transformation to hepatocellular carcinoma. Stoot et al. conducted a systematic review which included 1635 hepatocellular adenomas. The risk of malignant transformation was 4.2%. The median size of tumors with malignant degeneration was 10.5 cm (range 4.5–18 cm). They found only 3 cases of transformation in tumors < 5 cm representing 4.2% of all transformed tumors [21].
Several strategies are available for the management of hepatocellular adenomas. The results of a conservative approach for patients with < 5 cm adenomas were reported by van der Windt et al. Among 32 patients followed for a period of 24 months, there were no incidents of hemorrhage, malignancy, or enlargement following discontinuation oral contraceptives [22].
Traditionally, the definitive management of hepatocellular adenomas has been surgical resection. Dokmak et al. treated 122 patients with hepatocellular adenomas. Their median tumor size was 8.4 cm (range 1–22 cm). 12/122 had arterial embolization followed by delayed resection. Fifteen percent of patients had a post-operative complication. Thirteen percent required a blood transfusion with a median of 3 units packed red blood cells. During a median follow-up of 70 months, there were no incidents of mortality or malignant transformation [2]. Smaller series reported a post-surgical complication rate of 4–11%, no mortality, and similar transfusion needs. Median length of stay ranged from 6 to 15 days [4,5,6, 23].
An alternative treatment focused primarily on bleeding tumors has been transarterial embolization. A systematic review was performed by Van Rosmalen et al. of 151 patients treated with embolization. Of the 196 tumors, 95 (48.5%) were non-bleeding. No surgery was performed in 68 patients (45%). Elective embolization was done in 49 patients with 66 adenomas. Forty-one (84%) did not require surgery. Major complications occurred in 8 patients (5.3%). There were no deaths. Complete tumor disappearance was seen in 10% of tumors and regression in 75% [24].
Thermal ablation is a common minimally invasive alternative to surgery which has been recently reported as a treatment method for hepatocellular adenomas. Rhim et al. treated 10 patients with pathologically proven hepatocellular adenomas. The mean tumor size was 2.3 ± 0.8 cm (range: 1.5–4.5 cm). During a mean follow-up of 17.5 months (range 2–35), they reported a 100% primary efficacy. There were no cases of local tumor progression or new recurrence and no mortality or major complications [10].
Van Vledder et al. treated 18 women, the majority of whom had a history of hormonal contraceptive use. Ten patients (56%) had multiple adenomas, with a median number of 2 lesions (range 1–12). The median size was 3.0 cm (0.8–7.3). Forty-five adenomas were treated in 32 sessions (open, n = 4; percutaneous, n = 28). They reported a primary efficacy of 57.8% and major complications in 2 patients (11%) [10, 25].
Smolock et al. treated 6 patients with 12 adenomas. The mean treated tumor size was 2.7 cm ± 2.0. During a mean follow-up of 12.6 months ± 7.1, the primary efficacy was 100%. They reported no complications or delayed hemorrhage or malignant transformation [26]. Several other case reports exist in the literature with favorable results [7, 27,28,29,30,31].
Our study found a major complication rate of 4.5% per procedure. This is similar to the results obtained with surgery and embolization. It should be noted that transfusion requirements were common in the surgical literature and it is unclear if they were always counted/considered as complications. Our results are also similar to small studies performed on ablation. We found no incidents of malignant transformation or delayed hemorrhage, which again compares well to the other treatment options.
There are limitations to our study. The most important is a lack of a comparison arm. Our median tumor size was 2.1 cm, with a maximum of 6.0 cm. The risk of complications of hemorrhage or malignant transformation for tumors of this size is low. Conservative management has been previously reported to be successful and may be the optimal choice. This underlines the need for a prospective trial comparing outcomes of the different treatment strategies. Other limitations include a small sample size, operator variability, and the retrospective nature of the study.
A recent development in the understanding of hepatocellular adenomas has been the Bordeaux system. This has classified adenomas into four subtypes merging histology as well as immunohistochemical marker expression. The four are: inflammatory, HNF1-α inactivated, β-Catenin activated, and unclassified. The inflammatory subtype is thought to be at higher risk of hemorrhage, the β-Catenin activated at higher risk of malignant transformation, and the HNF1-α inactivated likely to be multiple and lower risk for both. [32]. Our own cohort of adenoma patients was only partially tested for these immunohistochemical markers. There were no patients with the β-Catenin mutation and only 1 with the HNF1-α mutation. This precludes us from commenting on the role of immunohistochemical markers in relation to ablation. Furthermore, additional refinements to the molecular classification system are likely forthcoming and may further alter our risk stratification [33].
In conclusion, thermal ablation performed for the treatment of hepatocellular adenomas has a similar complication rate to surgery and embolization. Since the primary application of thermal ablation is for smaller tumors (< 5 cm), future studies with comparison to conservative management are needed.
Abbreviations
- RFA:
-
Radio frequency ablation
References
Barthelmes L, Tait IS. Liver cell adenoma and liver cell adenomatosis. HPB. 2005;7(3):186–96.
Dokmak S, Paradis V, Vilgrain V, Sauvanet A, Farges O, Valla D, Bedossa P, Belghiti J. A single-center surgical experience of 122 patients with single and multiple hepatocellular adenomas. Gastroenterology. 2009;137(5):1698–705.
Deodhar A, Brody LA, Covey AM, Brown KT, Getrajdman GI. Bland embolization in the treatment of hepatic adenomas: preliminary experience. J Vasc Interv Radiol. 2011;22(6):795–9 (quiz 800).
Leese T, Farges O, Bismuth H. Liver cell adenomas. A 12-year surgical experience from a specialist hepato-biliary unit. Ann Surg. 1988;208(5):558–64.
Gugenheim J, Mazza D, Baldini E, Evangelista A, Iovine L, Mouiel J. Surgical treatment of benign hepatic tumors. A safe and efficient choice. Miner Chir. 1995;50(3):161–5.
Kammula US, Buell JF, Labow DM, Rosen S, Millis JM, Posner MC. Surgical management of benign tumors of the liver. Int J Gastrointest Cancer. 2001;30(3):141–6.
Atwell TD, Brandhagen DJ, Charboneau JW, Nagorney DM, Callstrom MR, Farrell MA. Successful treatment of hepatocellular adenoma with percutaneous radiofrequency ablation. AJR Am J Roentgenol. 2005;184(3):828–31.
Fujita S, Kushihata F, Herrmann GE, Mergo PJ, Liu C, Nelson D, Fujikawa T, Hemming AW. Combined hepatic resection and radiofrequency ablation for multiple hepatic adenomas. J Gastroenterol Hepatol. 2006;21(8):1351–4.
Rocourt DV, Shiels WE, Hammond S, Besner GE. Contemporary management of benign hepatic adenoma using percutaneous radiofrequency ablation. J Pediatr Surg. 2006;41(6):1149–52.
Rhim H, Lim HK, Kim Y-S, Choi D. Percutaneous radiofrequency ablation of hepatocellular adenoma: initial experience in 10 patients. J Gastroenterol Hepatol. 2008;23(8 Pt 2):e422–7.
Omary RA, Bettmann MA, Cardella JF, Bakal CW, Schwartzberg MS, Sacks D, Rholl KS, Meranze SG, Lewis CA. Quality improvement guidelines for the reporting and archiving of interventional radiology procedures. J Vasc Interv Radiol. 2002;13(9):879–81.
Ahmed M, Solbiati L, Brace CL, Breen DJ, Callstrom MR, Charboneau JW, Chen M-H, Choi BI, de Baère T, Dodd GD 3rd, Dupuy DE, Gervais DA, Gianfelice D, Gillams AR, Lee FT Jr, Leen E, Lencioni R, Littrup PJ, Livraghi T, Lu DS, McGahan JP, Meloni MF, Nikolic B, Pereira PL, Liang P, Rhim H, Rose SC, Salem R, Sofocleous CT, Solomon SB, Soulen MC, Tanaka M, Vogl TJ, Wood BJ, Goldberg SN. International Working Group on Image-guided Tumor Ablation, Interventional Oncology Sans Frontières Expert Panel, Technology Assessment Committee of the Society of Interventional Radiology, Standard of Practice Committee of the Cardiovascular and Interventional Radiological Society of Europe. Image-guided tumor ablation: standardization of terminology and reporting criteria–a 10-year update. Radiology. 2014;273(1):241–60.
Agrawal S, Agarwal S, Arnason T, Saini S, Belghiti J. Management of hepatocellular adenoma: recent advances. Clin Gastroenterol Hepatol. 2015;13(7):1221–30.
Neuberger J, Portmann B, Nunnerley HB, Laws JW, Davis M, Williams R. Oral-contraceptive-associated liver tumours: occurrence of malignancy and difficulties in diagnosis. Lancet. 1980;1(8163):273–6.
Rooks JB, Ory HW, Ishak KG, Strauss LT, Greenspan JR, Hill AP, Tyler CW Jr. Epidemiology of hepatocellular adenoma. The role of oral contraceptive use. JAMA. 1979;242(7):644–8.
Edmondson HA, Henderson B, Benton B. Liver-cell adenomas associated with use of oral contraceptives. N Engl J Med. 1976;294(9):470–2.
Nagorney DM. Benign hepatic tumors: focal nodular hyperplasia and hepatocellular adenoma. World J Surg. 1995;19(1):13–8.
Bühler H, Pirovino M, Akobiantz A, Altorfer J, Weitzel M, Maranta E, Schmid M. Regression of liver cell adenoma. A follow-up study of three consecutive patients after discontinuation of oral contraceptive use. Gastroenterology. 1982;82(4):775–82.
van Aalten SM, de Man RA, IJzermans JNM, Terkivatan T. Systematic review of haemorrhage and rupture of hepatocellular adenomas. Br J Surg. 2012;99(7):911–6.
Deneve JL, Pawlik TM, Cunningham S, Clary B, Reddy S, Scoggins CR, Martin RCG, D’Angelica M, Staley CA, Choti MA, Jarnagin WR, Schulick RD, Kooby DA. Liver cell adenoma: a multicenter analysis of risk factors for rupture and malignancy. Ann Surg Oncol. 2009;16(3):640–8.
Stoot JHMB, Coelen RJS, De Jong MC, Dejong CHC. Malignant transformation of hepatocellular adenomas into hepatocellular carcinomas: a systematic review including more than 1600 adenoma cases. HPB. 2010;12(8):509–22.
van der Windt DJ, Kok NFM, Hussain SM, Zondervan PE, Alwayn IPJ, de Man RA, IJzermans JNM. Case-orientated approach to the management of hepatocellular adenoma. Br J Surg. 2006;93(12):1495–502.
Cho SW, Marsh JW, Steel J, Holloway SE, Heckman JT, Ochoa ER, Geller DA, Gamblin TC. Surgical management of hepatocellular adenoma: take it or leave it? Ann Surg Oncol. 2008;15(10):2795–803.
van Rosmalen BV, Coelen RJS, Bieze M, van Delden OM, Verheij J, Dejong CHC, van Gulik TM. Systematic review of transarterial embolization for hepatocellular adenomas. Br J Surg. 2017;104(7):823–35.
van Vledder MG, van Aalten SM, Terkivatan T, de Man RA, Leertouwer T, Ijzermans JNM. Safety and efficacy of radiofrequency ablation for hepatocellular adenoma. J Vasc Interv Radiol. 2011;22(6):787–93.
Smolock AR, Cristescu MM, Potretzke TA, Ziemlewicz TJ, Lubner MG, Hinshaw JL, Brace CL, Lee FT Jr. Microwave ablation for the treatment of hepatic adenomas. J Vasc Interv Radiol. 2016;27(2):244–9.
Scheffer HJ, Melenhorst MCAM, van Tilborg AAJM, Nielsen K, van Nieuwkerk KM, de Vries RA, van den Tol PMP, Meijerink MR. Percutaneous irreversible electroporation of a large centrally located hepatocellular adenoma in a woman with a pregnancy wish. Cardiovasc Intervent Radiol. 2015;38(4):1031–5.
Ahn SY, Park SY, Kweon YO, Tak WY, Bae HI, Cho SH. Successful treatment of multiple hepatocellular adenomas with percutaneous radiofrequency ablation. World J Gastroenterol. 2013;19(42):7480–6.
McDaniel JD, Kukreja K, Ristagno RL, Yazigi N, Nathan JD, Tiao G. Radiofrequency ablation of a large hepatic adenoma in a child. J Pediatr Surg. 2013;48(6):E19–22.
Kim TY, Kim BS, Hyun CL, Song BC. Hepatocellular adenoma treated with radiofrequency ablation in young male. Korean J Gastroenterol. 2011;57(6):384–7.
van Aalten SM, Terkivatan T, van der Linden E, Verheij J, de Man RA, Ijzermans JNM. Management of liver adenomatosis by radiofrequency ablation. Dig Surg. 2011;28(3):173–7.
Bioulac-Sage P, Rebouissou S, Thomas C, Blanc JF, Saric J, Sa Cunha A, Rullier A, Cubel G, Couchy G, Imbeaud S, Balabaud C, Zucman-Rossi J. Hepatocellular adenoma subtype classification using molecular markers and immunohistochemistry. Hepatology. 2007;46(3):740–8.
Nault JC, Couchy G, Balabaud C, Morcrette G, Caruso S, Blanc JF, Bacq Y, Calderaro J, Paradis V, Ramos J, Scoazec JY, Gnemmi V, Sturm N, Guettier C, Fabre M, Savier E, Chiche L, Labrune P, Selves J, Wendum D, Pilati C, Laurent A, De Muret A, Le Bail B, Rebouissou S, Imbeaud S; GENTHEP Investigators, Bioulac-Sage P, Letouzé E, Zucman-Rossi J. Molecular Classification of Hepatocellular Adenoma Associates With Risk Factors, Bleeding, and Malignant Transformation. Gastroenterology. 2017 Mar;152(4):880-894.e6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Retrospective audit of anonymized patient records, for this type of study, formal consent was not required.
Rights and permissions
About this article
Cite this article
Mironov, O., Jaberi, A., Beecroft, R. et al. Retrospective Single-Arm Cohort Study of Patients with Hepatocellular Adenomas Treated with Percutaneous Thermal Ablation. Cardiovasc Intervent Radiol 41, 935–941 (2018). https://doi.org/10.1007/s00270-018-1893-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-1893-4