Abstract
Purpose
To compare safety and efficacy of percutaneous vertebroplasty (PVP) when treating up to three vertebrae or more than three vertebrae per session.
Materials and Methods
We prospectively compared two groups of patients with symptomatic vertebral fractures who had no significant response to conservative therapy. Pathologic substrate included osteoporosis (n = 77), metastasis (n = 24), multiple myeloma (n = 13), hemangioma (n = 15), and lymphoma (n = 1). Group A patients (n = 94) underwent PVP of up to three treated vertebrae (n = 188). Group B patients (n = 36) underwent PVP with more than three treated vertebrae per session (n = 220). Decreased pain and improved mobility were recorded the day after surgery and at 12 and 24 months after surgery per clinical evaluation and the use of numeric visual scales (NVS): the Greek Brief Pain Inventory, a linear analogue self-assessment questionnaire, and a World Health Organization questionnaire.
Results
Group A presented with a mean pain score of 7.9 ± 1.1 NVS units before PVP, which decreased to 2.1 ± 1.6, 2.0 ± 1.5 and 2.0 ± 1.5 NVS units the day after surgery and at 12 and 24 months after surgery, respectively. Group B presented with a mean pain score of 8.1 ± 1.3 NVS units before PVP, which decreased to 2.2 ± 1.3, 2.0 ± 1.5, and 2.1 ± 1.6 NVS units the day after surgery and at 12 and 24 months after surgery, respectively. Overall pain decrease and mobility improvement throughout the follow-up period presented no statistical significance neither between the two groups nor between different underlying aetiology. Reported cement leakages presented no statistical significance between the two groups (p = 0.365).
Conclusion
PVP is an efficient and safe technique for symptomatic vertebral fractures independently of the vertebrae number treated per session.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In a great number of patients with vertebral fracture, pain is partially or moderately relieved by conservative treatment, which leads to dependency on others and decreased quality of life [1–8]. Moreover, the concomitant decreased mobility of these patients increases their risk for pneumonia, deep vein thrombosis, and pulmonary embolism, thus causing an overall increase in comorbidities [3, 9]. Conventional management of vertebral fractures primarily includes pain relief through the use of narcotics, analgesics, nonsteroidal anti-inflammatory agents, and immobilization.
In cases of malignancy, radiation therapy is not always able to relieve pain, and surgical intervention is not always feasible, especially in cases of multiple fracture locations or when the overall condition of the patient does not allow for any major interventional procedure. Mobilization, with or without a brace, and exercise are subsequently prescribed as rehabilitation therapy [4, 5, 10].
Failure or performance inability of the above-mentioned therapies necessitates the use of other treatment approaches. During the last 25 years, interest has been fostered on improving quality of life by using minimally invasive procedures, such as percutaneous vertebroplasty (PVP). With this technique, polymethylmethacrylate (PMMA) or other cements are injected into the vertebral body, solidifying fracture lines, thus providing thus structural support, restoring the bony space lost by the fracture, and preventing movements that result in pain [3, 11].
PVP is a minimally invasive technique that was originally described by Deramond and Galibert in 1987 for the treatment of an aggressive vertebral hemangioma [11]. This technique has greatly progressed worldwide and evolved over time to include more and more pathologies. Thus, the spectrum of diseases to be treated and the number of lesions that can be treated are continuously evolving. As the learning curve and the available materials change, so do the risk factors. What was once considered as an absolute contraindication becomes a relative one.
The purpose of this study was to evaluate safety of PVP when treating up to three vertebrae per session versus multilevel sessions (more than three).
Materials and Methods
All patients were informed about the technique itself as well as possible benefits and complications, and they provided written consent the procedure and the study. Our institutional and university board gave approval. The principles of national legislation and the Declaration of Helsinki were followed.
Patient Population
In an open prospective study, 130 consecutive patients underwent 139 PVPs in 408 vertebral levels (9 patients [6.9 %] needed further intervention by second vertebroplasty on new affected vertebral levels, n = 20].
Patients were referred to a dedicated spine clinic in our department. Before each procedure, the patient underwent thorough clinical examination, correlation with his or her medical records, and evaluation of all his imaging studies. Preoperational imaging included x-rays, multiplane magnetic resonance imaging (MRI) (T1W, T2W, Short TI Inversion Recovery (STIR)), and/or bone scintigraphy. As a rule, PVP was performed on sites on which local percussion over the posterior elements of the involved vertebral body elicited pain, and these sites were confirmed on imaging modalities (CT and MRI).
Patients’ inclusion criteria were painful primary (n = 62) or secondary (steroid induced, n = 15) osteoporotic vertebral compression fractures that were unresponsive or minimally responsive to conventional treatments (analgesics, bisphosphonates, bed rest, bracing) for at least 2 months irrespective of the fracture’s age. Patients with malignant lesions had been treated by their physicians with either chemotherapy and/or radiotherapy and were referred to our institution for persistent spinal pain.
Exclusion criteria were uncontrolled bleeding disorders, any ongoing systemic or spinal infection, myelopathy, and/or radiculopathy. Based on these exclusion criteria, five patients were not eligible for vertebroplasty and were thus excluded from this study. Decreased vertebral body height and destruction of the posterior vertebral wall were not considered exclusion criteria. Retropulsed bone was tolerated as long as there were no clinical neurological findings.
Sample characteristics are listed in Table 1. Mean age was 75 ± 15 years. Out of our total number of patients, 76.2 % were female and 23.8 % were male. Pathologic substrate included osteoporosis in 59.2 %, metastases in 29.2 %, and hemangiomas in 11.5 % of cases. Six levels were treated in 8 patients, 7 levels in 4 patients, and 8 levels in 2 patients. A unilateral transpedicular approach was used in 314 vertebrae (80.9 %); a bipedicular approach (16.5 %) was used in 64 vertebrae; a postero-lateral access (0.5 %) was used in 2 vertebrae; an antero-lateral access (1.8 %) was used in 7 vertebrae; and a transoral approach (0.25 %) was used in 1 vertebral body.
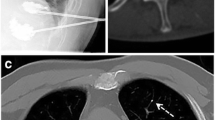
Patients were grouped into two categories: those who had 1 up to 3 vertebrae treated (Fig. 1) and those who had more than 3 levels treated per session (group A and group B respectively) (Fig. 2). Group A consisted of 94 patients (72.3 %) treated in 188 vertebral levels, and group B consisted of 36 patients (27.7 %) treated in 220 vertebral levels.
Vertebroplasty Technique
PVP was performed under a single-plain digital subtraction fluoroscopic guidance system in the angiographic suite under strict sterile conditions and with the patient under anaesthesia (general, epidural, sedation, or local). The patient’s blood pressure, electrocardiogram, and oxygen saturation were monitored during the entire procedure by an anaesthesiologist who was always present and responsible for the conscious sedation or general anaesthesia of the patient according to their evaluation of each case. Preprocedural antibiotic therapy with vancomycin 500 mg vancomycin hydrochloride (VONCON®, VIANEX, PALLINI, ATTIKI GREECE) was administered at least 1 h before the procedure.
Most of the procedures were performed with the patient in a prone position. A unilateral transpedicular approach was used in most of the cases. In the patients for whom unilateral-approach filling was not satisfactory or for whom there was a need for both pedicles to be stabilized, a bipedicular approach was used. In cases of inadequate visualization of the pedicles under fluoroscopic guidance, or when previous surgical interventions were performed, such as osteosynthesis or laminectomy, a postero-lateral access was used. For the cervical vertebral bodies, two techniques were used, the antero-lateral access and the transoral access; both of them were performed with the patient lying in a supine position.
A detailed description of vertebroplasty’s technique is beyond the scope of this study. However, all techniques were performed in accordance to Cardiovascular and Interventional Radiological Society of Europe’s (CIRSE’s) quality-assurance guidelines as well as the Society of Interventional Radiology’s (SIR’s) quality improvement guidelines for PVP [12, 13].
After the procedure, the patient was instructed to remain bedridden for a minimum of 4 h and to remain in the hospital overnight, mainly for security reasons. We routinely performed CT scans during the next 24 h to evaluate cement distribution and possible leakage outside the vertebrae.
Follow-Up Protocol: Data Collection
A database was designed to prospectively collect diagnostic, clinical, and technical information on patients who underwent PVP. Age, sex, pathology underlying the vertebral lesions, localization, number of treated vertebrae, approach technique, and complications were gathered. Specific standardized questionnaires—such as the Greek Brief Pain Inventory (G-BPI), a linear analogue self-assessment questionnaire (LASA), and a questionnaire from the World Health Organization (WHO)—were also included to assess the pain, mobility, and general quality of life in patients undergoing PVP. Questionnaire scores were collected and evaluated before the procedure and at specific predetermined time intervals, i.e., day 1 and months 12 and 24 after surgery. Data were collected by interview and during follow-up clinical assessment in prescheduled appointments.
G-BPI
The G-BPI is a pain-assessment tool translated and validated in several languages, including Greek [14]. The G-BPI uses a numeric visual scale, in which numbers are seen on the questionnaire, compared with other questionnaires, e.g., the visual analogue scale (VAS), on which numbers are not seen. The G-BPI is a simple, efficient, and valid instrument to measure both pain intensity and pain interference in the patients’ life and ability to function. The G-BPI uses a numeric scale of 0 to 10 for pain-severity items in a similar manner as the classic VAS [15–17]. Zero = “no pain,” and 10 = “pain as bad as you can imagine” [14]. For the evaluation of pain interference in the patient’s functional ability, seven “interference items” concerning work, activity, mood, enjoyment, sleep, walking, and relationships are also assessed using a numeric scale of 0 to 10, with 0 = “no interference” and 10 = “complete interference” [14]. A higher score on the G-BPI questionnaire indicates greater pain.
LASA
LASA is a single-item linear analogue self-assessment tool for evaluating patient quality of life and general feeling of well-being in a fast and simple way [18–21]. Three questions are given describing energy, ability for everyday activities, and quality of life as experienced by the patient during the previous week. The questions are graded from 0 to 10, with 0 = “worst” and 10 = “best.” A higher score on this scale reflects better quality of life.
WHO
The WHO questionnaire is a performance status scale equivalent to that of Eastern Collaborative Oncology Group and Karnofsky, and it rates functional ability from 0 to 5, where 0 = fully active (able to carry on all predisease performance without restriction), 4 = completely disabled (no self-care ability and totally confined to bed or chair), and 5 = death [22, 23].
Statistical Analysis
Variables were first tested for normality using the Kolmogorov–Smirnov criterion. Continuous variables are presented with mean ± SD. Qualitative variables are expressed as absolute and relative frequencies. Chi-square test was used for the comparison of proportions.
Wilcoxon signed-rank test was used to evaluate the differences between baseline and 2-year measurements. Repeated measurements analysis of variance (ANOVA) was further used to evaluate the differences between several groups (i.e., osteoporotic, malignancy, hemangioma) regarding the changes observed in G-BPI, LASA, and WHO scales during the 2-year period. Because of their skewed distribution, ranks of variables were used in ANOVA, and p-values reported are two-tailed. Statistical significance was set at 0.05, and analysis was conducted using SPSS 17.0 software (SPSS, Chicago, IL). A decrease equal or greater than two VAS units, was considered significant in respect of pain and mobility improvement [24].
Results
Of the total number of patients (n = 130), all patients were followed-up for a 2-year period except for one patient with metastatic breast cancer who died after 15 months after the procedure. This patient was excluded from the study because completion of a 2-year follow-up was not possible.
Nine patients underwent a second vertebroplasty procedure. These patients were included in the study, but the follow-up period started after the second vertebroplasty.
Using the G-BPI, patients in group A had pain improvement of 5.9 ± 1.9 NVS units (74.7 %), improved quality of life of 5.7 ± 1.8 NVS units, and 66.7 % increase of mobility performance. Decreased pain between the two groups, before and after vertebroplasty at certain time periods, is illustrated in Fig. 3. Similarly, group B patients reported pain improvement of 6.0 ± 1.8 NVS units (74.1 %), improved quality of life of 6.0 ± 1.4 NVS units, and 65.6 % increase of mobility performance.
The results of all three questionnaires from baseline to 2 years concerning groups A and B were not significant different (analysis of variance, p > 0.005). It is remarkable that even if patients in group B had worse immobilization status according to WHO scale at baseline (p = 0.007), this difference did not remained significant after day 1 after the procedure (Table 3).
At post-treatment CT in group A, 27 leakages were reported in 188 treated vertebral levels (14.36 %). In group B, 25 leakages were reported in 220 vertebral levels (11.36 %). There was no statistical significant difference between the two groups (chi-square test, p = 0.365).
Comparing the pain units (NVS scores) before and at 24 months after vertebroplasty, the mean value of pain decrease in our total sample was 5.9 ± 1.9 NVS units (74.7 %) (p < 0.05). Significant pain decrease (>2 NVS units) was present in 126 (96.9 %) of the patients. The pain status according to G-BPI scale was 7.9 ± 1.2 NVS units before PVP, 2.1 ± 1.5 NVS units at day 1 after the procedure, 2.0 ± 1.5 NVS units at 12 months after the procedure, and 2.0 ± 1.5 NVS units at 24 months after the procedure (Table 2). Furthermore, a subgroup analysis of pain decrease was performed according the underlying pathologic entity and demonstrated no statistical significant difference between osteoporotic, metastatic, and hemangioma lesions (Table 2).
According to WHO scale, all patients presented a mean decrease for the total sample equal to 1.9 ± 1.0 (67.9 % mean change), indicating improvement in mobilization. The mobility status was 2.8 ± 0.9 at baseline and 1.0 ± 0.8 at day 1 after the procedure, 0.9 ± 0.8 at 12 months after the procedure, and 0.9 ± 0.9 at 24 months after the procedure (Table 3). One hundred twenty-one patients (93.1 %) had >20 % improvement according to the WHO questionnaire.
The results were similar for LASA, with a mean increase for the total sample equal to 5.8 ± 1.7 (263.6 % mean change), which indicated improved quality of life. Quality of life at baseline was 2.2 ± 1.1, at day 1 after the procedure was 7.8 ± 1.5, and at 12 and 24 months after the procedure was 8.0 ± 1.4 (Table 4).
The improvement in pain, quality of life, and mobility was significant from day 1 after the procedure compared with baseline (p < 0.05 for all comparisons). The overall change for G-BPI, LASA, and WHO from baseline to 2 years was not significant different based on cause, type of transpedicular approach (analysis of variance, p > 0.05), indicating that the same trend in improved pain, quality of life, and mobilization was found in all groups during the follow-up period. Patients with malignancy had worse mobilization status according to the WHO scale at baseline compared with those having hemangiomas (p = 0.020), but after day 1 after the procedure, this difference was no longer significant.
Concerning the association of leakages to pathologic substrate, 26 patients (33.8 %) of the “osteoporotic” group had leakage, whereas the respective proportion for the “malignancy” and “hemangiomas” groups were 31.6 and 33.3 %, respectively (p = 0.973). 2 patients from the osteoporotic group had pulmonary embolism.
Discussion
In the present study, significant pain relief (>20 %) was achieved in 96.9 % of patients. The benefit from the treatment was significant already within 24 h after surgery and was sustained unchanged throughout the 2-year follow-up period. Nevertheless, all patients were also referred to their physicians for proper medical therapy (osteoporotic drugs, chemotherapeutics, etc.). Independent of the underlying aetiology, the benefit of vertebroplasty is comparable and long lasting.
Other prospective studies of osteoporotic patients that used as an evaluation method the VAS reported similar results in pain improvement [25–28]. McGraw et al. [25] confirmed that 97 % of patients had significant pain relief within 24 h after treatment and during the same year Zoarsky et al. [26] reported that 80 % of patients were feeling better. Later on and with a greater number of patients (n = 173), Singh et al. [27] documented that 77 to 85 % of patients had partial to complete pain relief, whereas Voormolen et al. [28] reported 95 to 100 % of their 112 patients being satisfied with their surgical outcome.
In cases of neoplastic involvement, Weill et al. [29] stated that of 37 patients, 73 % had clear, 21 % had moderate, and 6 % had no improvement, and Cotten et al. [30], with the same number of patients, reported that 75 % of them experienced pain relief. A pain decrease >82 % in 50 patients was later reported by Shimony et al. [31].
In our study, significant mobility improvement of >20 % was noted on 93.1 % of our patients. There are few studies dealing with mobility after PVP. First, McGraw et al. [25] evaluated 100 patients after PVP, and 93 % of them showed improved ambulatory activity due to a decrease in pain. Singh et al. [27] reported 91 to 95 % of 173 patients having the same or increased activity levels.
Single versus multiple level treatments is considered a debatable issue. Some interventional radiologists advise not to treat more than three to four vertebral levels in a single session. Some investigators, such as Barr et al. [32], have suggested that better outcomes are achieved when treating only one vertebral fracture instead of multiple levels. Zoarsky et al. [26] reported that although it is acceptable to treat up to five vertebral levels of osteoporotic fractures, treating eight or more levels simultaneously is not accepted medical practice. In the present study, there was no statistical significant difference in both pain relief and mobility improvement when comparing the two groups of patients, group A (those treated in up to three levels) and group B (those treated in more than three levels in a session). This conclusion was also reached by Singh et al. [27] in a series of 172 treatment sessions. They stated that whenever vertebral compression fractures are concerned, one, two, or more than three levels per session have equal effectiveness on pain, activity, and analgesic treatment. Anselmetti et al. [24] also reached the same conclusion treating effectively as many as seven vertebrae in one session.
A major concern with vertebroplasty is the leakage of cement into the venous system and epidural space. The percentage of leakages present was equally distributed according the different underlying pathologies. The proportion of leakage between the two groups presented no statistical significance (p = 0.365).
In our hospital, as a routine, each patient was evaluated by CT the morning after PVP for control of the implant’s distribution and identification of any complications that may have occurred. There were no major complications and, although in two patients there were small pulmonary emboli, they were asymptomatic and needed no further intervention. In one case, pedicle fracture occurred when passing the needle, that was treated by cement injection during removal of the needle, thus stabilizing the pedicle. We encountered 52 leakages in 25 patients from 408 treated levels (12.74 %): 18 anterior, 5 posterior, 1 intraforaminal, 11 intradiscal, and 17 lateral. One had presented a hematoma at the puncture site.
Murphy and Deramond [33] reported that vertebroplasty-associated complications according to etiology were more common in metastatic lesions (10 %), in hemangiomas (2.5 %), and osteoporotic fractures (1.3 %). In 2003, due to increased interest in the field of PVP from more interventional radiologists, SIR, along with McGraw et al. [13], evaluated and classified complications as major or minor according their clinical significance by needing or not needing extra care.
In a review published in 2006, an evaluation of published data series from 1997 until 2005, it was concluded that leakages were present in 41 % of cases performed, of which 32 % were in the epidural space, 32.5 % were paravertebral, 30.5 % were intradiscal, 1.7 % involved the pulmonary circulation, and 3.3 % were intraforaminal [34].
In 2007, Layton et al. [35] reported a series of 552 patients treated in 1,000 vertebral levels with 1.8 % clinical significant complications and 25 % clinical insignificant leakages.
According to CIRSE’s and SIR’s quality-assurance guidelines concerning PVP, published data have placed major complication rates at <1 % for osteoporotic fractures and <10 % for neoplastic involvement [12, 13].
Thus, although minimal cement leakage does occur with vertebroplasty, it has little if any clinical impact. In the literature only a few cases of fat embolism have been reported, and it is considered by some that the volume of PMMA injected, not multilevel treatment, is mainly responsible for this event [24].
In our study, of 130 patients, 9 underwent a second vertebroplasty procedure due to the presence of new lesion locations. Among osteoporotic patients, there were 6 such cases of 77 (7.8 %) patients. Most studies have described a greater percentage of new osteoporotic fractures, e.g., Uppin et al. [36] in 12.4 % of 177 patients, Tanigawa et al. [37] in 36.8 % of 76 patients, Mubin et al. [38] in 21.7 % of 253 patients, and Voormolen et al. [39] 24 % of 66 patients. In contrast, results of a study by Kim et al. [40] were close to ours, with 7.9 % of 106 patients having new fractures. The reason for this numerical discrepancy may be our relatively short follow-up period, the fact that we try to refer the patient to a specialised physician for proper medical therapy, the multilevel intervention, and our small sample size.
Some more limitations of our study include the fact that we were not able to have a proper control on the dosages and type of pain killers each patient was receiving. Furthermore, we were not able to control and evaluate their respiratory status and possible insufficiency, although all patients were cleared for anaesthesia with \( {\text{P}}_{{{\text{O}}_{ 2} }} \) >90 %.
Conclusion
Being able to treat a patient in several vertebral levels during one session is technically safe as well as efficient regardless of the underlying aetiology. The benefit from the procedure is immediate and long lasting with the patient being able to regain his or her previous mobility status. There is no need for further hospitalization and consequent examinations of the patient to perform a second or third vertebroplasty for the same final result.
References
Riggs BL, Meltron LJ III (1995) The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone 17(Suppl 5):505S–511S
Silverman SL (1992) The clinical consequences of vertebral compression fracture. Bone 13(Suppl 2):27–31
Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE (1997) Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral compression fractures: technical aspects. Am J Neuroradiol 18:1897–1904
Mathis JM, Barr JD, Belkoff SM, Barr MS, Jensen ME, Deramond H (2001) Percutaneous vertebroplasty: a developing standard of care for vertebral compression fractures. Am J Neuroradiol 22:373–381
Cortet B, Cotten A, Boutry N et al (1999) Percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures: an open prospective study. J Rheumatol 26(10):2222–2228
Cook DJ, Guyatt GH, Adachi JD, Clifton J, Griffith LE, Epstein RS et al (1993) Quality of life issues in women with vertebral fractures due to osteoporosis. Arthritis Rheum 36(6):750–756
Gold DT (1996) The clinical impact of vertebral fractures: quality of life in women with osteoporosis. Bone 18(Suppl 3):185–189
Schlaich C, Minne HW, Bruckner T, Wagner G, Gebest HJ, Grunze M et al (1998) Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos Int 8(3):261–267
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Arch Intern Med 159(11):1215–1220
Amar AP, Larsen DW, Esnaashari N, Albuquerque FC, Lavine SD, Teitelbaum GP (2001) Percutaneous transpedicular polymethylmethacrylate vertebroplasty for the treatment of spinal compression fractures. Neurosurgery 49(5):1105–1114
Galibert P, Deramond H, Rosat P, Le Gars D (1087) Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 33:166–168
Gangi A, Sabharwal T, Irani F et al (2006) Quality assurance guidelines for percutaneous vertebroplasty. Cardiovasc Intervent Radiol 29:173–178
McGraw JK, Candella J, Barr JD et al (2003) Society of Interventional Radiology Quality Improvement Guidelines for Percutaneous Vertebroplasty. J Vasc Interv Radiol 14:827–831
Mystekidou K, Mendoza T, Tsilika E et al (2001) Greek brief pain inventory: validation and utility in cancer pain. Oncology 60:35–42
Cleeland CS (1989) Measurement of pain by subjective report. In: Chapman LJ, Loeser JD (eds) Advances in pain research and therapy, vol 12. Raven Press, New York, pp 391–403
Doyle D, Hans GWC, MacDonald N (1995) Pain assessment and cancer pain syndromes. In: Oxford textbook of palliative medicine. Oxford University Press, Oxford, p 148
Mendoza T, Chen C, Brugger A et al (2004) The utility and validity of the modified brief pain inventory in a multiple-dose postoperative analgesic trial. Clin J Pain 20(5):357–362
Coates A, Dillenbeck CF, McNeil DR et al (1983) Linear analogue self-assessment (LASA) in evaluation of aspects of quality of life of cancer patients receiving therapy. Eur J Clin Oncol 19:1633–1637
Gough IR, Furnival CM, Schilder L, Grove W (1983) Assessment of the quality of life of patients with advanced cancer. Eur J Clin Oncol 19(8):1161–1165
Hurny C, Bernhard J, Coates A et al (1996) Responsiveness of a single-item indicator versus a multi-item scale: assessment of the emotional well-being in an international adjuvant breast cancer trial. Med Care 34(3):234–248
Padilla GV, Grant MM, Ferrell BR, et al. (1996) Quality of life—Cancer. In: Spiker B (ed) Quality of life and pharmacoeconomics in clinical trials, 2nd edn. Lippincott-Raven, Philadelphia
Roila F, Lupatteli M, Basurto C et al (1991) Intra and interobserver variability in cancer patients’ performance status assessed according to Karnofsky and ECOG scales. Ann Oncol 2(6):437–439
Oken MM, Creech RH, Tormey DC et al (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Anselmetti GC, Corrao G, Monica PD et al (2007) Pain relief following percutaneous vertebroplasty: Results of a series of 283 consecutive patients treated in a single institution. Cardiovasc Interv Radiol 30(3):441–447
McGraw JK, Lippert J, Minkus K et al (2002) Prospective evaluation of pain relief in 100 patients undergoing percutaneous vertebroplasty. J Vasc Interv Radiol 13:883–886
Zoarski GH, Snow P, Olan WJ et al (2002) Percutaneous vertebroplasty for osteoporotic compression fractures: quantitative prospective evaluation of long term outcomes. J Vasc Interv Radiol 13:139–148
Singh AK, Pilgram TK, Gilula LA (2006) Osteoporotic compression fractures: outcomes after single- versus multiple-level percutaneous vertebroplasty. Radiology 238:211–220
Voormolen MH, Lohle PN, Lampmann LE, van den Wildenberg W, Juttmann JR, Diekerhof CH et al (2006) Prospective clinical follow-up after percutaneous vertebroplasty in patients with painful osteoporotic vertebral compression fractures. J Vasc Interv Radiol 17(8):1313–1320
Weill A, Chiras J, Simon JM et al (1996) Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. Radiology 199(1):241–247
Cotten A, Dewatre F, Cortet B et al (1996) Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at the clinical follow-up. Radiology 200:525–530
Shimony JS, Gilula LA, Zeller AJ, Brown DB (2004) Percutaneous vertebroplasty for malignant compression fractures with epidural involvement. Radiology 232:846–853
Barr JD, Barr MS, Lemley TJ, McCann RM (2000) Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine 25(8):923–928
Murphy KJ, Deramond H (2000) Percutaneous vertebroplasty in benign and malignant disease. Neuroimaging Clin N Am 10(3):535–545
Hulme PA, Krebs J, Ferguson SJ, Berlemann U (2006) Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine 31(17):1983–2001
Layton KF, Thielen KR, Koch CA, Luetmer PH, Lane JI, Wald JT et al (2007) Vertebroplasty, first 1000 levels of a single center: evaluation of the outcomes and complications. Am J Neuroradiol 28(4):683–689
Uppin AA, Hirsch JA, Cantenera LV et al (2003) Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology 226:119–124
Tanigawa N, Komemushi A, Kariya S et al (2006) Radiological follow-up of new compression fractures following percutaneous vertebroplasty. Cardiovasc Interv Radiol 29:92–96
Mubin IS, Neel AP, Solomon J et al (2005) New symptomatic vertebral compression fractures within a year following vertebroplasty in osteoporotic women. Am J Neuroradiol 26:1601–1604
Voormolen MH, Lohle PN, Juttmann JR, van der Graaf Y, Fransen H, Lampmann LE (2006) The risk of new osteoporotic vertebral compression fractures in the year after percutaneous vertebroplasty. J Vasc Interv Radiol 17(1):71–76
Kim SH, Kang HS, Choi JA, Ahn JM (2004) Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty. Acta Radiol 45(4):440–445
Conflict of interest
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mailli, L., Filippiadis, D.K., Brountzos, E.N. et al. Clinical Outcome and Safety of Multilevel Vertebroplasty: Clinical Experience and Results. Cardiovasc Intervent Radiol 36, 183–191 (2013). https://doi.org/10.1007/s00270-012-0379-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-012-0379-z