Abstract
The aim of this study was to assess if percutaneous vertebroplasty (PVP) could relieve back pain, reduce drug consumption, and improve the mobility of patients with metastases and vertebral compression fractures. From August 2002 to July 2004, 283 patients (216 females; mean age: 73.8 ± 9.9 years) underwent PVP on 749 vertebrae. Pain was evaluated with the pain intensity numeric rating scale (PI-NRS) (0 = no pain; 10 = worst pain) before the procedure and at the end point in September 2004 (follow-up:1–24 months; median: 7 months). A reduction of at least two points of the PI-NRS score was considered clinically relevant. Two hundred four patients were available for evaluation at the end point. Overall results showed a reduction of the median pain score from 8 at baseline to 1 at the end point (p < 0.0001); a clinically relevant pain reduction was observed in 176/205 patients (86%); 89/147 patients (61%) gave up a brace support (p < 0.0001); and 117/190 patients (62%) gave up drug therapy. Results were similar in different subgroups stratified according to age, underlying pathology, number of fractured or treated vertebrae, and length of follow-up.
This study adds evidence that PVP is effective in treating painful vertebral fractures. A significant reduction in drug assumption and significant mobility improvement can also be achieved.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Percutaneous vertebroplasty (PVP) consists of the injection of polymethyl methacrylate (PMMA), or other nonacrylic cements, through a large needle within the vertebral body under radiological guidance. The main indication for the procedure is back pain associated with osteoporotic vertebral fractures refractory to medical treatment. Other indications for PVP are painful vertebral fractures related to malignant or benign tumors or, less frequently, fractures associated with osteonecrosis [1, 2].
In the last decade, vertebroplasty has become very popular in the United States and in some countries of western Europe and tens of thousands of procedures are being performed yearly worldwide [3]. Despite the high number of procedures performed, evidence in favor of vertebroplasty relies mostly on small single-institution studies or on large but retrospective multicenter cohort studies [4–8].
The primary goal of the present study is to evaluate whether PVP is effective in reducing symptoms in patients with painful vertebral compression fractures; the secondary goal is to assess whether there are factors that influence the outcome of the procedure such as age, pathology, and multilevel versus single-level treatment. To this purpose, we have analyzed the results of a large series of consecutive patients who underwent PVP in a single institution.
Materials and Methods
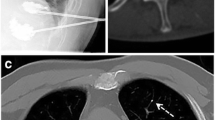
A series of consecutive patients admitted to a tertiary care center for PVP in a 2-year period (August 2002 to July 2004) were enrolled in the study. Patient evaluation and preprocedural workup were performed as previously reported [8]. Most patients were treated 3–12 weeks from the onset of pain, following the failure of conservative medical therapy. Vertebroplasty in fresh fractures was proposed exclusively to patients who underwent the procedure successfully the first time and who have subsequently sustained further fractures. Magnetic resonance imaging (MRI) was performed in addition to the routine conventional X-ray radiograms and computed tomography (CT) in subjects with multiple fractures, following indications by some authors that the presence of edema on T2-weighted or Short Tau Inversion Recovery (STIR) images is predictive of a favorable outcome of vertebroplasty [9] (Fig. 1); we did not use scintigraphy for preprocedural evaluation and PVP was performed in collapsed vertebrae even if MRI did not demonstrate the edema but pain was evoked by palpation. In addition, MRI was performed on all patients with malignant vertebral lesions to assess the extent of vertebral involvement and spinal canal compromise. Contraindications to vertebroplasty are as outlined by the guidelines of the Society of Interventional Radiology [1].
Written informed consent was obtained from all patients in accordance with the national legislation and the Declaration of Helsinki before inclusion in the study. The procedure was performed in most cases (263 out of 283 patients; 92.9%) using a C-arm angiographic unit (Advantx Tilt-C; GE Medical Systems, Milwaukee, WI) with the patient in the prone position. Treatment of upper thoracic vertebrae (from T1 to T6) and sacral vertebrae was performed under combined fluoroscopic and CT guidance. Beveled vertebroplasty needle placement was facilitated by using a CT control and cement injection was always performed under direct fluoroscopic control to monitor material outflow in real time in a direction that would be off-plane on the CT scan [10]. Vertebroplasty was always performed in sterile conditions and intravenous antibiotics (1 g of vancomycin hydrochloride; Abbott SpA, Campoverde di Aprilia, Latina, Italy) were administrated 3 days before and 5 days after the procedure. Patient pressure, heart rate, and oxygen saturation were monitored during the whole procedure. Only local anesthesia was performed in most cases (275 out of 283 patients; 97.2%) by injecting 3 mLl of 2% lidocaine hydrocloride (Lidosan; Industria Farmaceutica Galenica Senese, Monteroni d’Arbia, Siena, Italy) both at the skin level and deep to include the periostium of the pedicle. Neuroleptic analgesics were occasionally (8 out of 283 patients; 2,8%) administered by a staff anesthesiologist in the form of fentalnyl citrate (Fentanest; Pharmacia Italia, Milano, Italy) and midazolam (Ipnovel; Roche, Fontenay-sous-Bois, France).
The 11G- to 15G-diameter needle was advanced until the tip abutted the posterior profile of the pedicle. Under constant monitoring by C-arm fluoroscopy, the needle was then driven into the anterior third of the vertebral body with the aid of an orthopedic hammer. A unilateral transpedicular approach was used in most cases (732 out of 749 treated vertebrae; 97.7%). The dorsal vertebrae were treated via a parapedicular approach, whereas C2 and C3 were approached transorally [11]. A through-cut needle biopsy was performed using 16G to 18G needles introduced coaxially in patients with a vertebral compression fracture of uncertain etiology. Following reports in the literature demonstrating no significant differences in frequency or amount of extravasation and no differences in clinical outcome between patients in whom venography was performed versus that in patients in whom no venography was performed, we have abandoned its use [12].
The PMMA mixture (Osteopal®V; Biomet Merck GmbH, Altdorf, Switzerland, or SpineFix; Teknimed S.A., Bigorre, France) was injected after all of the needles were positioned, using the same batch of cement, kept in an ice bath to slow down the polimerization time [13]. In patients suffering from multiple painful vertebral collapses due to iatrogenic osteoporosis, myeloma, and metastases (46/283; 16.2%), low-volume multilevel vertebroplasty, consisting of the injection of less than 3 mL of PMMA (average: 1.5 ± 0.5 mL) in each treated vertebra, was performed to minimize the risk of a fat embolism or to avoid the depression of hematopoiesis [14, 15]. Up to seven vertebrae were treated in the same session (Fig. 2); prophylactic vertebroplasty was occasionally performed (38 out of 283 patients; 13.4%) in subjects with an higher risk of a new fracture (iatrogenic osteoporosis and myeloma) exclusively within a normal vertebra positioned between two osteoporotic collapsed bodies (Fig. 3); this procedure, not in accordance with guidelines [1], was performed at the beginning of our study.
After the procedure, the patient remained in bed in the supine position for 1 h and was discharged when he regained the ability to deambulate. On discharge, the patient agreed to be contacted by phone as part of the routine clinical follow-up.
A dedicated software database was developed to prospectively collect clinical and technical information on patients who underwent vertebroplasty. Demographic data, pathology underlying vertebral collapse, and fracture locations were recorded at each treatment session. The approach, equipment, cement type, and quantity were detailed for each treated vertebrae, together with any technical or clinical complication. As programmed, all of the treated patients were contacted by phone by one of the authors in September 2004 for interview. The standardized questionnaire included assessment of the overall patient status, degree of pain, drug prescription, and use of a brace both just before PVP (baseline) and at the time of the interview (end point). Pain was evaluated with a verbal version of the pain intensity numeric rating scale (PI-NRS): 0 represents no pain and 10 represents the worst possible pain. The raw change in the PI-NRS scores was computed by subtracting the baseline value from the end point for each patient. According to Farrar et al. [16], a reduction of two points in the raw change scores was considered clinically relevant. Analgesic drugs prescribed at baseline and at the time of the interview were classified as none, nonsteroidal anti-inflammatory drugs (NSAIDs), oral narcotic therapy on an as-needed basis, scheduled oral or intravenous narcotic therapy, and implanted pump. The use of a brace was reported as usage or no usage. Prescribed drugs were used as proxy of severity of symptoms before and after vertebroplasty and were indexed as 0 (no drugs), 1 (NSAIDs), 2 (narcotics as needed), 3 (chronically scheduled narcotics), and 4 (narcotics pump).
Descriptive statistics were calculated for each questionnaire item. Several nonparametric statistical tests (Wilcoxon signed rank, trend in median values according to Jonckheere & Terpstra, one-way analysis of variance according to Kruskal-Wallis, McNemar and Cochane, Mantel and Haensezel tests) were used where suitable to test differences or trends in distribution of the considered clinical factors.
For all of the hypotheses tested, two-tailed p-values less than 0.05 were considered significant.
Results
When the decision was made to sum up the results, at the end of July 2004, a total of 283 patients had undergone PVP. The clinical characteristics of the cohort are summarized in Table 1. More than three-quarters of patients were females and the mean age (SD) at the time of the procedure was 73.8 years (9.9). The pathology underlying vertebral collapse was most frequently osteoporosis (74.5%) or bone metastasis (17.6%). Multiple fractures were observed (by X-Ray and/or MRI) in 219 patients (77%), with more than half of the total population having at least three fractured vertebrae. Overall, 749 vertebrae were treated in 310 treatment sessions; 22 out of 283 patients (8%) were retreated one or more times for new fractures: 18 patients underwent the procedure twice, 3 patients underwent the procedure three times, and in 1 patient underwent the procedure four times. The median number of treated vertebrae was three. The mean volume of injected cement in each vertebra was 4.1 ± 1.1 mL. A bilateral approach was chosen only in a few cases, whenever satisfactory cement diffusion was not achieved with a monolateral approach (17 out of 749; 2.3%). An overnight stay was required only in 27% of the cases. All of the patients except one declared feeling better on discharge.
Of the 310 procedures, there was 1 procedure-related (CT-guided parapedicular approach of an osteoporotic collapsed T9 vertebra) severe complication (0.3%) consisting of a large hematoma that developed within the erector spinae muscle and required a blood transfusion and lengthened hospital stay. There were no instances of permanent neurologic injury or symptomatic pulmonary embolism. Mild transitory episodes of radicular pain, due to minimal cement leak n the foraminal vein, were reported occasionally (11 out of 283 patients; 3.9%) and they were successfully treated with oral drugs.
At the time of telephone contact, in September 2004, 22 patients were deceased, 56 were not traceable, which left 205 patients who were then interviewed. The elapsed time from the vertebroplasty procedure to the phone interview ranged between 1 and 24 months, with a median of 7 months.
Table 2 shows the pain status at baseline and at the end point for the overall ensemble of 205 patients and for different subgroups stratified according to patient age at baseline, number of fractured and treated vertebrae, underlying pathology, and length of time between treatment and interview. The overall results show a reduction of the median pain score from 8 at baseline to 1 at phone interview, with a raw change significantly different from zero (p < 0.0001). A clinically relevant reduction of pain, equivalent to a raw change in PI-NRS score ≤−2, was observed in 176 of 205 patients (86%). Improvements of perceived pain were observed consistently within each of the above-defined subgroups of patients.
Table 3 shows that among the 58 patients who did not use a dressing brace before vertebroplasty; only 1 (1.7%) began its use after the procedure. Conversely, 89 out of the 147 patients (61%) who had need of a brace support before vertebroplasty did not use it after the procedure (p < 0.0001). Consistently, none of the 15 patients who did not use analgesics for pain relief before the procedure required analgesics afterward, whereas among the 190 patients who used drugs before the procedure, 117 (62%) did not require them after the procedure (Table 4), suggesting that the severity of the symptoms significantly decreased after vertebroplasty (p < 0.0001).
The primary expected clinical outcome (Table 2), such as back-pain improvement, was not significantly influenced by the age of the patients (p = 0.0815), the number of fractured vertebrae (p = 0.1333), the number of treated vertebrae (p = 0.3128), and the cause of the injury (p = 0.2512) and we did not observe any statistically significant difference (p = 0.1029) of pain regression between the different times of the clinical interviews during the follow-up.
Discussion
In our series, PVP was very efficient in reducing pain from symptomatic vertebral compression fractures. These results confirm recent studies that reported success rates for the procedure above 85% [1, 6, 17]. Similarly the use of braces and drug usage was dramatically reduced following treatment. These results were obtained at a very low cost in terms of hospital stay and adverse effects. Indeed, over 70% of patients were discharged the same day of the procedure and only one severe complication, an intramuscular hematoma requiring treatment and prolonged hospital stay, occurred. This is of particular interest in view of the fact that most patients treated with PVP are elderly and frail.
In our opinion, this might be attributed to the following factors. Clinical indications to the procedure were respected, except for prophylactic vertebroplasty in 38 patients (13.4%), and a thorough preprocedural evaluation was performed with the use of MRI in multiple fractures and malignancy. In our institution, MRI with state-of-the-art equipment is readily available and a room is reserved for patients in preoperative evaluation for vertebroplasty. The procedures have all been performed by the same experienced operator using good quality fluoroscopic equipment and a dedicated CT scanner, whenever combined guidance was necessary. Furthermore, in comparison to other work, we have begun performing vertebroplasty relatively recently and therefore have had new and more reliable injection devices and optimally opacified cement available. The fact that the bilateral approach was rarely employed is another possible factor influencing the incidence of adverse events.
Interestingly, the outcome is similar for different subgroups. Age, underlying pathology, and length of follow-up do not seem to influence the outcome (Table 2). The enduring effect of vertebroplasty has been also reported by others [17–19]. No significant difference was observed in terms of pain reduction between patients with osteoporosis and with metastatic involvement. The results of our series, retrospectively evaluated, were consistent with previous reports even though the decrease in PI-NRS values was more marked in our experience. Fourney et al. [20] reported significant or complete pain relief in 84% of 56 patients with malignancies; Alvarez et al. [17] observed a decrease in preprocedural pain from 9.1 to 3.2 in a series of 21 patients with cancer.
The number of multilevel treatments performed (patients suffering from secondary osteoporosis and myeloma) and therefore the median number of treated vertebrae per patient was higher in our cohort in comparison to other published series. In our opinion, this is probably due to the characteristics of patients sent for evaluation in our center, who were mostly referred from the rheumatology, nephrology, and hematology departments, and to our policy of proposing treatment of as many as seven vertebrae in one session, which is not recommended by most researchers but has been proposed and used in different published works [21, 22]. In addition, in few cases, PVP was performed on unfractured vertebrae positioned between two collapsed bodies. To reduce the risk of symptomatic cement leakage, fat embolism and depression of hematopoiesis low-volume vertebroplasty was performed in multilevel treatment (< 3 mL/vertebra), taking care to limit use of cement to one batch per procedure. Using this approach, the results in terms of pain reduction were consistent regardless of the number of treated vertebrae. Kobayashi et al. [6] reported similar results using the same average quantities of PMMA as we used in this study. The fact that in our cohort only 22 of 283 patients (8%) developed new painful fractures during follow-up is in contrast with recent reports that found significantly higher percentages of new fractures in subjects treated with vertebroplasty [23–25]. It could be that a correct medical treatment for osteoporosis (performed by an experienced endocrinologist in all osteoporotic patients after the procedure) and PVP reduces the rate of new fractures; a further study is ongoing to verify this point.
There are limitations to the study. First, demographic and procedural data have been collected prospectively, but patients have been recalled for pain evaluation. Retrospective collection of data might be a source of bias, as patients might not recall pain prior to treatment or, if treatment has been very successful, might enhance the memory of pain prior to the procedure. Furthermore, patients who have a longer follow-up might recall pain differently than patients with a shorter follow-up. Nevertheless, the reported benefits of vertebroplasty in terms of pain reduction were constant even as time from vertebroplasty to phone interview increased;: this suggests that the survey was homogenous because the outcome opinion is not influenced by time.
Second, even if used as a standard instrument in chronic pain evaluation, raw or percentage changes in PI-NRS scores do not give information on the subjective nature of pain. Therefore, the clinical relevance of the effect might not be determined. Farrar et al. have examined data from 10 multicenter chronic pain studies that have utilized both PI-NRS and the patient’s global impression of change scores and have found that a reduction from baseline of two points is equivalent to being clinically relevant [16].
Third, without a comparison group it is not possible to assess whether PVP is more effective than conservative management in treating painful vertebral compression fractures. Although this was not the objective of this study, we have now designed a randomized trial comparing vertebroplasty and medical treatment.
This large single-institution study shows that PVP is a safe and reliable procedure in the treatment of vertebral compression fractures from osteoporosis and metastatic disease. Furthermore, our preliminary results suggest that multilevel treatment using low-volume PMMA might be effective in preventing a new fracture in high-risk patients.
References
McGraw JK, Cardella J, Barr JD, et al. (2003) Society of Interventional Radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Intervent Radiol 14:S311–S315
Barr JD, Barr MS, Lemley TJ, et al. (2000) Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine 25(8):923–928
Nussbaum DA, Gailloud P, Murphy K (2004) A review of complications associated with vertebroplasty and kyphoplasty as reported to the Food and Drug Administration medical device related web site. J Vasc Intervent Radiol 15:1185–1192
Evans AJ, Jensen ME, Kip KE, et al. (2003) Vertebral compression fractures: Pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty retrospective report of 245 cases. Radiology 226:366–372
McGraw JK, Lippert JA, Minkus KD, et al. (2002) Prospective evaluation of pain relief in 100 patients undergoing percutaneous vertebroplasty: results and follow-up. J Vasc Intervent Radiol 13:883–886
Kobayashi K, Shimoyama K, Nakamura K, et al. (2005) Percutaneous vertebroplasty immediately relieves pain of osteoporotic vertebral compression fractures and prevents prolonged immobilization of patients. Eur Radiol 15:360–367
Chen JF, Wu CT, Lee ST (2004) Percutaneous vertebroplasty for the treatment of burst fractures. Case report. J Neurosurg Spine 1(2):228–231
Kallmes DF, Jensen ME (2003) Percutaneous vertebroplasty. Radiology 229(1):27–36
Mathis JM, Barr JD, Belkoff SM, et al. (2001) Percutaneous vertebroplasty: A developing standard of care for vertebral compression fractures. Am J Neuroradiol 22:373–381
Gangi A, Kastler BA, Dietemann JL (1994) Percutaneous vertebroplasty guided by a combination of CT and fluoroscopy. Am J Neuroradiol 15(1):83–86
Martin JB, Gailloud P, et al. (2002) Direct transoral approach to C2 for percutaneous vertebroplasty. Cardiovasc Intervent Radiol 25(6):517–519
Gaughen JR Jr, Jensen ME, Schweickert PA, et al. (2002) Relevance of antecedent venography in percutaneous vertebroplasty for the treatment of osteoporotic compression fractures. Am J Neuroradiol 23(4):594–600
Chavali R, Resijek R, Knight SK, et al. (2003) Extending polymerization time of polymethylmethacrylate cement in percutaneous vertebroplasty with ice bath cooling. Am J Neuroradiol 24(3):545–546
Mathis JM. (2003) Percutaneous vertebroplasty: Complication avoidance and technique optimization. Am J Neuroradiol 24(8):1697–1706
Syed MI, Jan S, Patel NA, et al. (2006) Fatal fat embolism after vertebroplasty: identification of the high-risk patient. Am J Neuroradiol 27(2):343–345
Farrar JT, Young JP, LaMoreaux L, et al. (2001) Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 94:149–158
Alvarez L, Perez-Higueras A, Quinones D, et al. (2003) Vertebroplasty in the treatment of vertebral tumors: postprocedural outcome and quality of life. Eur Spine J 12:356–360
Grados F, Depriester C, Cayrolle G, et al. (2000) Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford) 39(12):1410–1414
Legroux-Gerot I, Lormeau C, Boutry N, et al. (2004) Long-term follow-up of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Clin Rheumatol 23:310–317
Fourney DR, Schomer DF, Nader R, et al. (2003) Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg 98:21–30
Kayanja MM, Schlenk R, Togawa D, et al. (2006) The biomechanics of 1, 2, and 3 levels of vertebral augmentation with polymethylmethacrylate in multilevel spinal segments. Spine 31(7):769–74
Singh K, Heller JG, Samartzis D, et al. (2005) Open vertebral cement augmentation combined with lumbar decompression for the operative management of thoracolumbar stenosis secondary to osteoporotic burst fractures. J Spinal Disord Tech 18(5):413–419
Syed MI, Patel NA, Jan S, et al. (2005) New symptomatic vertebral compression fractures within a year following vertebroplasty in osteoporotic women. Am J Neuroradiol 26(6):1601–1604
Uppin AA, Hirsch JA, Centenera LV, et al. (2003) Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology 226(1):119–124
Voormolen MH, Lohle PN, Juttmann JR, et al. (2006) The risk of new osteoporotic vertebral compression fractures in the year after percutaneous vertebroplasty. J Vasc Intervent Radiol 17(1):71–76
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anselmetti, G.C., Corrao, G., Monica, P.D. et al. Pain Relief Following Percutaneous Vertebroplasty: Results of a Series of 283 Consecutive Patients Treated in a Single Institution. Cardiovasc Intervent Radiol 30, 441–447 (2007). https://doi.org/10.1007/s00270-006-0146-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-006-0146-0