Abstract
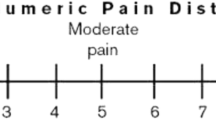
The purpose of the present study was to ascertain chronological changes in the analgesic effects of percutaneous vertebroplasty (PVP) on osteoporotic vertebral compression factures and to radiologically follow new compression fractures after PVP. Seventy-six patients (206 vertebral bodies) were followed radiologically for a mean of 11.5 months. A visual analog scale (VAS; 0–10) was used to assess pain severity, and frontal and lateral plain radiographs of the thoracic and lumbar vertebrae were taken 1–3 days and 1, 4, 10, and 22 months after PVP.
The average VAS score was 7.2 ± 2.0 (mean pain score ± standard deviation) before PVP, 2.5 ± 2.3 at 1–3 days after PVP, 2.2 ± 2.3 at 1 month, 1.9 ± 2.2 at 4 months, 1.8 ± 2.4 at 10 months, and 1.0 ± 0.2 at 22 months. A new compression fracture was confirmed in 56 vertebral bodies in 28 patients (36.8%), affecting 38 adjacent vertebral bodies (67.8%), 17 nonadjacent vertebral bodies (30.4%), and 1 treated vertebral body (1.8%). A new compression fracture occurred within 1 week of PVP in 2 vertebral bodies (3.6%), between 1 week and 1 month after PVP in 22 (39.3%), between 1 and 3 months in 12 (21.4%), between 3 and 6 months in 12 (21.4%), and after more than 6 months in 8 (14.3%). PVP was highly effective in relieving the pain associated with osteoporosis-induced vertebral compression fractures, and this analgesia was long lasting. Radiological follow-up observation revealed new compression fractures in about one-third of patients. More than half of these new compression fractures occurred in adjacent vertebral bodies within 3 months of PVP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Percutaneous vertebroplasty (PVP) was first reported in the literature in 1987 [1]. Since then, PVP has been performed to relieve the pain associated with vertebral compression fracture due to various causes, and because the procedure has been markedly effective in relieving pain, it is widely performed. However, some patients experience recurrent pain after undergoing PVP. When this is investigated, it is commonly found to result from a new compression fracture. Although there have been studies investigating the incidence of new compression fractures following PVP [2–9], very few have radiographically followed patients over a period of time [10–13]. In the present study, we conducted periodic radiographic follow-up of patients who had undergone PVP, regardless of clinical symptoms. The objective of the present study was to ascertain the chronological changes in the pain-relieving effects of PVP on osteoporotic vertebral compression fractures and to radiologically follow new compression fractures after PVP.
Subjects and Methods
The study was approved by the institutional review board. All patients provided written informed consent. From February 2003 to February 2004, 105 patients underwent 261 PVPs during 136 treatment sessions. Seventy-six of these 105 patients could be followed radiologically for at least 4 months. Subjects of this study were these 76 patients who underwent 206 PVPs for back pain secondary to osteoporotic compression fracture from February 2003 to February 2004.
Percutaneous vertebroplasty was performed on patients with back pain caused by vertebral compression fracture in whom radicular and neurological symptoms were not the principal symptoms. As a general rule, PVP was performed on a vertebral body that demonstrated pain on percussion of the spinous process while taking into account imaging findings, such as those of magnetic resonance imaging (MRI). Preoperatively, plain radiography (frontal and lateral radiographs of the thoracic and lumbar vertebrae), MRI, computed tomography (CT), and bone scintigraphy were performed. Furthermore, bone mineral density, respiratory function, ECG, and physical parameters were measured. A visual analog scale (VAS) was used to assess pain severity.
PVP Procedure
Percutaneous vertebroplasty was performed under combined CT and fluoroscopic guidance (Advantex LCA + ACT; GE Medical Systems, Milwaukee, WI). Thirty minutes preoperatively, 10 mg morphine hydrochloride (Sankyo, Tokyo, Japan), 0.5 mg atropine sulfate (Tanabe, Osaka, Japan), and 25 mg hydroxyzine hydrochloride (Pfizer Japan Inc., Tokyo, Japan) were administered intramuscularly. Local anesthesia with 10 cc of 1% lidocaine (AstraZeneca, Osaka, Japan) was performed from the skin to the periosteum of the pedicle using a 22G Cathelin needle (Terumo Europe, Leuven, Belgium) under fluoroscopic guidance. After orientation of the puncture needle was confirmed on CT and aligned with the Cathelin needle, a 13G bone biopsy needle (Osteo-Site Bone Biopsy Needle Murphy M2; Cook, Bloomington, IN) was advanced into the pedicle of the vertebral arch. CT was repeated, and after the orientation of the biopsy needle was confirmed, the visualization modality was changed to lateral fluoroscopy and the bone biopsy needle was advanced to the anterior third of the vertebral body close to the midline.
Intraosseous venography was performed with 1–5 mL of iopamidol (Iopamiron 300; Schering Japan, Osaka, Japan) or 10–20 mL of carbon dioxide to confirm that the needle was not positioned within a direct venous anastomosis to the central or epidural veins. Subsequently, 20 g of methylmethacrylate powder (Osteobond copolymer bone cement; Zimmer, Warsaw, IN, USA) was mixed with 5 g of sterile barium sulfate powder to increase its opacity. Ten milliliters of liquid methylmethacrylate monomer was added to the powder, and the mixture was blended to a toothpastelike consistency, producing polymethylmethacrylate (PMM). Using 1-mL syringes, the PMM was injected with lateral fluoroscopic guidance. A unilateral approach was used in most cases. PMM injection was terminated when adequate filling of the vertebral body was achieved or if leakage occurred. If leakage occurred, the needle was repositioned and additional PMM was injected to fill the remaining part of the vertebral body. The needle was then removed.
Computed tomography was performed immediately after the procedure to evaluate cement distribution and cement leakage outside of the vertebra. All patients were observed in the supine position for 2 h.
Follow-up Protocol
At our institution, PVP was performed on an inpatient basis. During postprocedural days 1–3, pain severity was assessed, and frontal and lateral plain radiographs of the thoracic and lumbar vertebrae were taken. In addition, at 1, 4, 10, and 22 months after discharge, patients were asked to visit our outpatient clinic, where the medical history was recorded, physical examinations carried out, and further frontal and lateral plain radiographs of the thoracic and lumbar vertebrae were taken. Patients were also instructed to return to our institution if they experienced pain, and in such cases, physical examination and plain radiography were performed. MRI was also performed as necessary.
A new compression fracture was defined as follows: a vertebral body exhibiting reduced height on plain radiography; or when this was not clear, bone marrow edema pattern on MRI in patients who had localized spontaneous pain or pain on percussion of the spinous process. Two radiologists reviewed the imaging findings, and arrived at a final diagnosis by discussion if their opinions did not agree.
Percutaneous vertebroplasty was repeated if a painful compression fracture was diagnosed during the follow-up period, in which case the same follow-up protocol was applied.
Results
Seventy-six patients underwent 105 sessions of PVP, with 206 levels treated. Cement injection was successful in all cases. The amount of cement injected was 4.0 ± 1.7 mL (mean volume ± standard deviation) per vertebra and 7.7 ± 4.4 mL per procedure. The number of treated vertebrae per procedure was 1.9 ± 0.9 (mean value ± standard deviation).
One hundred six leakages were found in 90 vertebral levels on CT images performed immediately after the cement injection. Cement leakage was found in intradiscal leakages in 48 levels (23.3%), in epidural vein or paravertebral vein in 44 levels (21.4%), in soft tissue in 10 levels (4.9%), in spinal canal or neural foramen in 3 levels (1.5%), and in the lung in 1 case (0.5%). There was no symptomatic cement leakage except for one case. Continuous pain for 1 month at the puncture site developed due to leakage into subcutaneous soft tissue in one case.
The average follow-up observation period was 11.5 months (range: 4–24 months). VAS scores were as follows: 7.2 ± 2.0 (mean pain score ± standard deviation) before PVP, 2.5 ± 2.3 at 1–3 days after PVP, 2.2 ± 2.3 at 1 month, 1.9 ± 2.2 at 4 months, 1.8 ± 2.4 at 10 months, and 1.0 ± 0.2 at 22 months.
A new compression fracture was seen in 56 vertebral bodies of 28 patients (27.2%). Of these 28 patients, 8 (28%) had painless morphological fractures, and in the other 20, PVP was repeated to relieve pain. Of these 20 patients, another fracture was confirmed in 6 patients (30.0%) after the second PVP, and because all 6 had pain, a third PVP was performed. Of these six patients, two developed yet another compression fracture, and a fourth PVP was required. In both of these patients, two physically separate fractures were confirmed at the initial visit, and PVP was performed twice initially. Hence, these two patients underwent PVP a total of five times (Fig. 1).
A 69-year-old woman with multiple compression fractures caused by osteoporosis. A Lateral plain radiograph of the thoracic vertebrae following the first PVP. Compression fracture was seen at Th9, Th11, and Th12, and 3.5, 1.5, and 4.5 cc of bone cement was injected, respectively. B Lateral plain radiograph of the thoracic vertebrae at 7 months after the first PVP. A new compression fracture was evident at Th8. C Lateral plain radiograph of the thoracic vertebrae after the second PVP; 2 cc of bone cement was injected into Th8. D Lateral plain radiograph of the thoracic vertebrae after the third PVP. A new compression fracture was evident at Th7, and 2 cc of bone cement was injected at this site.
A new compression fracture occurred at 38 vertebral bodies adjacent to previous PVP (67.8%), 17 nonadjacent vertebral bodies (30.4%) and 1 treated vertebral body (1.8%). In the patient with a recurrent compression fracture of the treated vertebral body, the cement became displaced to the ventral side 1 month after PVP, thus lowering the vertebral height (Fig. 2).
An 85-year-old woman with multiple compression fractures caused by osteoporosis. A Lateral plain radiograph of the thoracic vertebrae; 3 mL of bone cement was injected into the vertebral bodies of Th12 and L1. B Lateral plain radiograph of the thoracic vertebrae at 1 month after PVP: The injected bone cement had been displaced to the ventral side, causing a reduction of vertebral height.
A new compression fracture occurred within 1 week of PVP in 2 vertebral bodies (3.6%), between 1 week and 1 month after PVP in 22 vertebral bodies (39.3%), between 1 and 3 months after PVP in 12 vertebral bodies (21.4%), between 3 and 6 months after PVP in 12 vertebral bodies (21.4%) and more than 6 months after PVP in 8 vertebral bodies (14.3%).
Discussion
Although the pain-relieving effects of PVP on back pain caused by an osteoporotic compression fracture are widely recognized [14–17], pain recurs in some patients after undergoing PVP, and the cause of such pain is a new compression fracture in a fair number of cases. Although studies have been conducted to ascertain the incidence of compression fractures following PVP [2–12], follow-up methods have varied: Subjective symptoms were ascertained by telephone or mail [7, 9] and compression fractures were detected by plain radiography when patients returned to the medical institutions after developing back pain [8]. In order to standardize follow-up, we followed patients using periodic radiography of the thoracic and lumbar vertebrae, regardless of subjective symptoms. The results indicated that during an average of 11.5 months after PVP, a new compression fracture was seen in 56 vertebral bodies in 28 patients (36.8%).
Several studies have followed patients using diagnostic imaging [10–13]. Radiographic follow-up periods ranged from 1 year to at least 5 years, and incidence of a new compression fracture ranged from 17.7% to 52% of patients (Table 1).
In the present study, we defined a new compression fracture as follows: a vertebral body with a reduced height on plain radiography, or if this was not clear, a bone marrow edema pattern on MRI in patients exhibiting localized spontaneous pain or pain on percussion of the spinous process. Because the definition of compression fracture differed, the results of the present study cannot be compared directly to the above-mentioned studies. However, based on the radiological findings, new compression fracture occurred in around 25–50% of patients. Although these figures are higher than the 19.2% incidence of a new compression fracture reported previously in compression fracture patients [18], it cannot be concluded that the incidence of a new compression fracture is high following PVP.
Two theories on the cause of new compression fractures following PVP have been proposed: (1) a new compression fracture occurs as part of the natural course of osteoporosis—in other words, the onset of new compression fracture is unrelated to PVP [19], and (2) cement injection increases the strength of the treated vertebral body, and as a result, untreated adjacent vertebral bodies become relatively weaker, thus increasing the risk for a new compression fracture [20, 21]. At this point in time, it is not clear whether new compression fracture is caused by PVP or is part of the natural course of osteoporosis.
In the present study, of the 28 patients with new compression fractures, 8 had painless morphological fractures. When ascertaining the incidence of new compression fracture following PVP, periodic diagnostic imaging can provide more accurate data; however, PVP is not indicated for patients without subjective symptoms (i.e., back pain). The clinical significance of painless morphological fractures as detected by diagnostic imaging is not clear at present. It would be interesting to ascertain whether vertebral misalignment due to a painless morphological fracture eventually leads to more severe compression fracture and back pain.
A new compression fracture occurred at 38 adjacent vertebral bodies (67.8%), 17 nonadjacent vertebral bodies (30.4%), and 1 treated vertebral body (1.8%), in accordance with previous reports documenting that new compression fractures often occur at vertebral bodies adjacent to cement-injected vertebrae [8, 11, 12]. In one of our patients, cement was injected into Th12 and L1, but the cement at Th12 became displaced to the ventral side, causing a decrease in vertebral height. We classified this patient as having a new compression fracture.
A new compression fracture occurred within 1 week of PVP in 2 vertebral bodies (3.6%), between 1 week and 1 month after PVP in 22 vertebral bodies (39.3%), between 1 and 3 months after PVP in 12 vertebral bodies (21.4%), between 3 and 6 months after PVP in 12 vertebral bodies (21.4%) and more than 6 months after PVP in 8 vertebral bodies (14.3%). In other words, 42.9% of the new compression fractures occurred within 1 month of PVP, in accordance with Uppin and colleagues’ study [8]. Furthermore, considering that a new compression fracture occurred within 1 week of PVP in two vertebral bodies, it will be necessary to investigate the effects of the PVP procedure on adjacent vertebral bodies. In conclusion, PVP was effective in relieving the pain associated with osteoporosis-induced vertebral compression fractures and this analgesic effect was long lasting. Radiological follow-up observation showed that new compression fractures occurred in about one-third of the patients, and more than half of the new compression fractures occurred at the adjacent vertebral bodies within 3 months of PVP.
References
Galibert P, Deramond H, Rosat P, et al. (1987) Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirugie 33:166–168 (in French)
Deramond H, Depriester C, Galibert P, et al. (1998) Percutaneous vertebroplasty with polymethylmethacrylate: technique, indications, and results. Radiol Clin North Am 36:533–546
Jensen ME, Evanas AJ, Mathis JM, et al. (1997) Percutaneous methylmethacrylate vertebroplasty in the treatment of osteopolotic vertebral body compression fractures: Technical aspect. Am J Neuroradiol 18:1897–1904
Cyteval C, Sarrabere MP, Roux JO, et al. (1999) Acute osteoporotic vertebral collapse: open study on percutaneous injection of acrylic surgical cement in 20 patients. AJR Am J Roentgenol 173:1685–90
Cortet B, Cotton A, Boutry N (1999) Percutaneous vertebroplasty in the treatment of osteoporotic compression fractures: an open prospective study. J Rheumatol 26:2222–2228
Barr JD, Barr MS, Lemley TJ, et al. (2000) Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine 25:923–928
Zoarski GH, Snow P, Olan WJ (2002) Percutaneous vertebraoplasty for osteoporotic compression fractures: quantitative prospective evaluation of long-term outcomes. J Vasc Intervent Radiol 13:139–148
Uppin AA, Hirsch JA, Centenera LV, et al. (2003 Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology 226:119–124
Lin EP, Ekholm S, Hiwatashi A, et al. (2004) Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. Am J Neuroradiol 5:175–180
Legroux-Gerot I, Lormeau C, Boutry N, et al. (2004) Long-term follow-up of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Clin Rheumatol 23:310–317
Perez-Higueras A, Alvarez L, Rossi RE, et al. (2002) Percutaneous vertebroplasty: long-term clinical and radiological outcome. Neuroradiology 44:950–954
Grados F, Depriester C, Carrolle G, et al. (2000) Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford) 39:1410–1414
Heini PF, Walchli B, Berlemann U (2000) Percutaneous transpedicular vertebroplasty with PMMA: a prospective study for the treatment of osteoporotic compression fractures. Eur Spine J 9:445–450
Mathis JM, Barr JD, Belkoff SM, et al. (2001) Percutaneous vertebroplasty: a developing standard of care for vertebral compression fractures. Am J Neuroradiol 22:373–381
Evans AJ, Jensen ME, Kip KE, et al. (2003) Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty: retrospective report of 245 cases. Radiology 226:366–372
Hodler J, Peck D, Gilula LA (2003) Midterm outcome after vertebroplasty: predictive value of technical and patients-related factors. Radiology 227:662–668
Kallmes DF, Jensen ME (2003) Percutaneous vertebroplasty. Radiology 229:27–36
Lindsay R, Silverman SL, Cooper C, et al. (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–323
Jensen ME, Kallmes DF, Short JG, et al. (2000) Percutaneous vertebroplasty does not increase the risk of adjacent level fracture: a retrospective study. In: ASNR Annual Meeting Program. Oak Brook, (abstr). III: American Society of Neuroradiology 4
Polokeit A, Norte LP, Ferguson SJ (2003) The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit, finite element analysis. Spine 28:991–996
Berlemann U, Ferguson SJ, Nolte LP, et al. (2002) Adjacent vertebral failure after vertebroplasty: a biomechanical investigation. J Bone Joint Surg Br 84:748–752
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tanigawa, N., Komemushi, A., Kariya, S. et al. Radiological Follow-up of New Compression Fractures Following Percutaneous Vertebroplasty. Cardiovasc Intervent Radiol 29, 92–96 (2006). https://doi.org/10.1007/s00270-005-0097-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-005-0097-x