Abstract
Background
The evidence is sparse concerning the natural history of acute diverticulitis after successful conservative management. This observational study aimed to evaluate the rate, severity, and need of surgery for recurrence after a first episode of acute diverticulitis successfully managed conservatively.
Methods
All patients admitted for acute diverticulitis between 1994 and 2011 were considered for inclusion in the study. Severity of the first episode, demographic data, comorbidities, management, recurrence, and elective or emergency surgery during the follow-up period were prospectively recorded.
Results
The study included 560 patients. The mean follow-up period was of 67.2 ± 44.4 months. Severe diverticulitis was diagnosed in 22.3 % of the cases. Recurrence was observed in 14.8 % of the patients, and the rate of severe recurrence was 3.4 %. Most of the recurrences occurred during the first year of follow-up evaluation. Chronic corticoid therapy (P = 0.043) and the presence of more than one abscess (P < 0.001) were significantly related to recurrence. In the event of a mild recurrence, the first episode was either mild or severe (P = 0.172). In the case of severe recurrence, most patients presented with a previous severe diverticulitis (P < 0.001). During the follow-up period, 6.8 % of the patients needed an elective operation, and 1.4 % of them underwent emergency surgery.
Conclusion
The rate of severe recurrence after successful nonoperative management of acute diverticulitis was low, and emergency surgery was rare. Prophylactic surgery, even in cases of recovered severe diverticulitis, should be considered on a case-by-case basis. Strict follow-up assessment during the first year is advised.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Left-sided diverticular disease of the colon has been associated with the Western lifestyle and age [1]. An estimated 15–20 % of patients with diverticulosis will experience the development of acute diverticulitis [2], and its management depends on the stage of the disease at its presentation and on the response to the initiated treatment [1].
The classification based on computed tomography (CT) parameters proposed by Ambrosetti et al. [3] divides acute diverticulitis into mild and severe diverticulitis. The spectrum of severe diverticulitis ranges from a single localized pericolic abscess to diffuse purulent or fecal peritonitis. Whereas the therapeutic choice for mild diverticulitis and diffuse peritonitis is clear [4, 5], consensus is lacking on the management of diverticulitis associated with abscess or localized extraluminal air, both in the acute phase and during the follow-up period. The American Society of Colon and Rectal Surgeon (ASCRS) recommends management of abscesses smaller than 2 cm in diameter without intervention further than hospitalization and intravenous antibiotics while recognizing that larger abscesses need percutaneous drainage [6]. The ASCRS recommends an elective colon resection after successful conservative treatment of a severe diverticulitis due to the high risk for the development of severe recurrent sepsis [6, 7], considering that although expectant management alone has been suggested, it is controversial [8–10].
Evidence concerning the natural history of severe diverticular disease after successful conservative management is lacking due to the wide spectrum of disease presentation (size, localization, number of abscesses, and/or free extraluminal air), the patient’s characteristics (age, associated medical problems, and immunosuppression), the pattern of recurrences, and the history of previous drainage.
This study aimed to evaluate the rate and severity of diverticulitis and the need of surgery for recurrence after a first episode of acute diverticulitis successfully managed conservatively. The risk factors for recurrence were analyzed. The results are reported separately according to the severity of the first diverticulitis episode.
Methods
Setting
All patients admitted and treated for acute left colonic diverticulitis between 1994 and 2011 at Bellvitge University Hospital, Barcelona, Spain were considered for inclusion in this observational study. Starting from 1998, the diagnosis of acute diverticulitis was confirmed by CT scan for all the patients. Before 1998, some patients underwent only abdominal ultrasonography. From 1994 to 2009 all patients with the diagnosis of acute diverticulitis, including mild cases, were treated as inpatients. Starting from 2009, mild cases were included in the DIVER Trial and randomized for either out- or inpatient treatment [4].
The patients were followed up as outpatients by a colorectal surgeon until December 2013. Mortality was reviewed until December 2013. Community general mortality registries and families were consulted directly to confirm death and its causes. Admissions of patients to another hospital different from Bellvitge University Hospital also were registered. Data were collected prospectively for consecutive cases in a computer database. Approval for the study was obtained from the Hospital Ethics Committee.
Inclusion and exclusion criteria
The patients included in the study had been admitted for the first episode of left-sided colonic diverticulitis confirmed by CT scan within the study period. The patients with a diagnosis determined by ultrasonography, those with recurrences whose first episode was previous to 1994, and those with right-sided diverticulitis were excluded from the study. Diverticular hemorrhage and in-hospital deaths not related to the acute diverticulitis were excluded. The need for emergency surgery at presentation or semi-elective surgery within 2 months after the first episode for persisting sintomatology also was reason of exclusion from the study.
Definitions
Diverticulitis was classified according to the Ambrosetti classification guided by CT scan [3] as mild diverticulitis when localized sigmoid wall thickening (≥5 mm) with inflammation of pericolic fat was observed and as severe diverticulitis in cases of abscess, extraluminal air, or contrast.
Recurrence was defined as a new episode of acute diverticulitis confirmed by CT scan not earlier than 2 months after the first episode. Recurrences were classified as mild or severe according to the same definitions considered for the first episode. Time to recurrence was measured from discharge to the new admittance. Elective sigmoidectomy was proposed to the patients with or without recurrence on a case-by-case basis depending on persistent symptoms, severity of recurrence, and long-term complications such as symptomatic stenosis and fistulas.
Treatment
Conservative management consisted of nothing per mouth, intravenous fluids, analgesia, and parenteral broad-spectrum antibiotics (for at least 48 h) until oral intake could be reintroduced. Antibiotics were continued orally for 7–10 days. Patients with mild diverticulitis treated as outpatients received the first intravenous antibiotic dose in the emergency department before discharge. They continued oral antibiotic treatment for 10 days [4]. Abscesses 5 cm in size or larger were considered for percutaneous drainage. Emergency surgery was indicated for patients with diffuse peritonitis, septic shock, or an unfavorable clinical response after 48–72 h of conservative treatment. All patients managed conservatively were investigated with colonoscopy or barium enema to exclude the diagnosis of cancer once the acute episode had resolved.
Variables and statistical analyses
Size, location (pericolic, pelvic, or mesenteric), number of abscesses, and the presence of extraluminal contrast were revised by expert radiologists and recorded. The other variables studied were demographic data, American Society of Anesthesiologists (ASA) status, and associated comorbidities, with special interest in immunosuppressive preexisting conditions (malignant hematologic disease, human immunodeficiency virus [HIV], chemotherapy, biologic therapy, transplantation cases, chronic use of corticosteroids), diabetes, and chronic renal failure. Type of management (medical with or without percutaneous drainage), length of hospital stay, readmission for mild or severe recurrence, and need for elective or emergency surgery also were recorded until February 2013, when follow-up analysis was stopped.
Quantitative data are presented as mean ± standard deviation. Qualitative data are presented as absolute numbers and percentages.
The comparative study was performed using the χ 2 test and the two-tailed Fisher’s exact test for the qualitative data. The Mann-Whitney U test was used to compare quantitative data. All P values lower than 0.05 were considered significant. The Kaplan-Meier method was used to estimate the cumulative recurrence during the follow-up period, and the log-rank test was used to determine the comparisons. A Cox regression model was used to adjust for confounders. Parameters that were significant in the univariate analysis or clinically expected to be of importance were included in the regression model.
Results
Between 1994 and 2011, a total of 1,140 patients were treated for acute diverticulitis at Bellvitge University Hospital. Of these patients, 560 met the inclusion criteria and were included in the study analysis, whereas 580 were excluded for reasons shown by the flowchart in Fig. 1.
The baseline characteristics of the patients are detailed in Table 1. Mild diverticulitis was diagnosed in 435 patients (77.7 %) and severe diverticulitis in 125 patients (22.3 %). Of these 125 patients, 56 (44.8 %) had abscess, 50 (40 %) had extraluminal air, and 19 (15.2 %) had both abscess and extraluminal air. No statistical differences in the analyzed variables were found between mild and severe diverticulitis except for leucocytes exceeding 15 × 10E9/L (P = 0.001) and length of hospital stay (P < 0.001), which were greater in cases of severe diverticulitis.
The mean abscess diameter was 37.2 ± 24.3 mm, with 22 patients (29.3 %) having abscess diameters greater than 50 mm. The mean number of abscesses per patient was 1.2 ± 0.6 (range 1–5), and 10 patients (13.3 %) had more than one abscess. The abscesses had a pericolic location in 61 patients (81.3 %), a mesenteric location in 4 patients (4.3 %), and a pelvic location in 10 patients (13.3 %). Nine patients (7.2 %) with severe diverticulitis were treated with antibiotic and percutaneous drainage. The mean diameter of the nine drained abscesses (7 pericolic and 2 pelvic) was 86.6 ± 60 mm (range 40–140 mm). Because the remaining 13 patients had abscesses larger than 50 mm, percutaneous drainage was not technically feasible, and they were managed successfully with medical treatment.
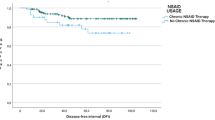
Recurrence rates
With 31 patients lost to follow-up evaluation during a mean follow-up period of 67.2 ± 44.4 months, recurrence was observed in 83 (14.8 %) of the 560 patients in the series. Recurrence did not occur for 446 of the patients (79.6 %). The median time to recurrence was 18 months (range 2.4–141.6 months). Figure 2 shows the cumulative rate of recurrence during the follow-up period.
Most recurrences take place during the first year after the initial episode. After that period, recurrences are less frequent, and the curves reach a plateau.
The rates of recurrence did not vary significantly relative to severity levels of acute diverticulitis (14 % after a mild diverticulitis and 17.6 % after severe diverticulitis) (P = 0.321).
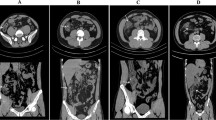
Long-term evolution of severe diverticulitis during the follow-up period is shown in Fig. 3.
The univariate analysis showed that recurrence was significantly related to chronic corticoid therapy (P = 0.043) and the presence of more than one abscess (P < 0.001). These significances were maintained in the multivariate analysis (Table 2).
Recurrence severity
Recurrent episodes after acute diverticulitis were mild in 64 patients (77 %) and severe in 19 patients (23 %). The mean number of recurrent episodes did not differ relative to a first mild or severe diverticulitis episode (Table 1).
The rate of severe recurrence after acute diverticulitis was 3.4 % (19 of 560 patients), and the episodes were more frequent after severe diverticulitis. Of the 61 patients who experienced recurrence after mild diverticulitis, 54 (88.5 %) had a mild recurrence, and 7 (11.5 %) had a severe recurrence. Of the 22 patients who experienced recurrence after severe diverticulitis, 10 (45.5 %) had a mild recurrence, and 12 (54.5 %) had a severe recurrence.
Table 3 shows overall, mild, and severe recurrence separately in relation to the characteristics of the first episode. The percentages in each column were calculated on the number of patients for each grade of severity of the first episode. The P values were calculated to find differences in overall, mild, and severe recurrences depending on the severity of the first episode.
In the event of a mild recurrence, the first episode would have been either mild or severe diverticulitis. In the case of severe recurrence, most patients presented with a report of a previous severe diverticulitis. Similar results were observed when considering the presence of an abscess or extraluminal air at the first episode. Overall recurrence did not differ between first episodes with and without abscess. However, the presence of abscess at the first episode was significantly related to severe recurrence (Table 3).
During the first year of follow-up evaluation, the cumulative rate of recurrence showed no differences between mild and severe first diverticulitis episodes in terms of overall recurrence (P = 0.087) or mild recurrence (P = 0.495) (Fig. 2a, b). Severe recurrence was significantly more frequent during first year of follow-up evaluation after a severe first diverticulitis episode (7 %) than after a mild first diverticulitis episode (1 %) (P < 0.001) (Fig. 2c).
Surgery
Of the 560 patients of the series, 38 (6.8 %) needed an elective operation, and 8 (1.4 %) underwent emergency surgery during a recurrent severe episode (Fig. 3). Among the patients who had elective surgery, 24 (4.3 %) of the 560 patients underwent surgery for persistent symptoms and fistula or symptomatic stenosis without having experienced a recurrence. Six of these patients had experienced a severe diverticulitis (4.8 % of 125 patients). Of the nine patients who needed a percutaneous drainage, none had undergone elective surgery.
Elective surgery was performed after a recurrent episode for 14 patients (2.5 % of 560 patients). One patient (0.8 % of 125 patients) had previously experienced a severe diverticulitis episode, and the remaining 13 patients (2.9 % of 435 patients) had experienced a mild diverticulitis episode. The chance of needing elective surgery after a conservatively managed acute diverticulitis was not higher after severe diverticulitis than after mild diverticulitis (4.8 % vs 4.1 %; P = 0.747). Neither did the chance of needing an elective operation after a recurrence of acute diverticulitis depend on the severity of the first episode (2.9 % after mild diverticulitis vs 0.8 % after severe diverticulitis; P = 0.167).
The median time to elective surgery after the first episode was 9.6 months (range 3.8–44.0 months). All the patients who underwent elective surgery were given a left colectomy or a sigmoidectomy with a primary anastomosis. The postoperative morbidity rate after elective surgery was 15.8 %, with a mean hospital stay of 9.4 ± 6.6 days. Two patients needed a reoperation after elective surgery: the first for anastomotic leakage and the second for acute abdominal wall dehiscence. In the first case, the colorectal anastomosis was taken down and refashioned with a protective loop ileostomy, which was closed 6 months later. No postoperative deaths were observed.
Of the eight patients who underwent emergency surgery for severe recurrence, five had experienced a severe first diverticulitis, and three had experienced a mild first diverticulitis. The median time to emergency surgery after the first acute diverticulitis episode was 4.7 months (range 3.1–35.1 months). Among the five patients with a severe first diverticulitis, one patient had a single pelvic abscess, one patient had two pericolic abscesses, and the remaining three patients presented with only extraluminal air. The two patients with abscess were managed with chronic corticoid therapy, and one of the two had undergone percutaneous drainage.
The procedures performed for emergencies comprised four sigmoidectomies with primary anastomosis, three Hartmann procedures, and one subtotal colectomy with terminal ileostomy. Three of the four patients who needed ostomy had experienced a severe first diverticulitis. Two of these patients had experienced abscess and chronic corticoid therapy. The postoperative morbidity rate after emergency surgery was 37.5 %. The mean hospital stay was of 12.6 ± 5.4 days. Two patients died of refractory septic shock and multiorgan failure. The one patient was an 82-year-old woman with chronic renal failure, hemodialysis, and chronic corticoid therapy who had undergone percutaneous drainage at the first episode. The other patient was a 70-year-old man with a mild first diverticulitis and an ASA of 4. At the recurrence, he experienced a fecal diffuse peritonitis.
Discussion
In this study, the rates of recurrence after acute and severe diverticulitis episodes were not as high as those reported in the literature. The presence of more than one abscess during the first episode of diverticulitis and chronic steroid treatment were risk factors for recurrence, and the severity of recurrent episodes was related to the severity of the first episode.
The major strength of the study was the consistency of its management and follow-up evaluation. All cases included in the study had been proved by CT scan. The follow-up period was long, and medical treatment success was strictly defined by the exclusion of recurrence before 60 days. All recurrences managed at a center other than Bellvitge University Hospital were recorded in the database.
The 18 patients in the current series who needed surgery within 2 months after the first admission deserve special mention. In fact, they could be considered as the group of patients who independently of the initial classification (mild or severe) presented a persistence of the colonic inflammatory process and symptoms a few weeks after the first episode. In such cases, differentiation of a true recurrence from persisting diverticulitis can be difficult. For this reason, we considered persistent symptoms in the first 2 months as those of persistent diverticulitis rather than a recurrence. Given that this study aimed to evaluate the rate, severity, and need of surgery for recurrence after a first episode successfully managed conservatively and that many patients with persistent symptoms in the first 2 months after the first episode need a semi-elective surgery, we decided to exclude these 18 patients from the analysis. We believe we selected undoubtful recurrences for this study.
However the study had some limitations. The number of patients with severe diverticulitis was relatively small. A significant number of patients, particularly from the first cases of the series, were excluded due to the lack of CT scan confirmation of acute diverticulitis. Even if the sensitivity and specificity of ultrasound scans are lower than those of CT scans [2], we can say that ultrasound identified mild diverticulitis for most of these patients. To reduce bias and have a more homogeneous group of patients, we decided to exclude these cases.
To categorize the severity of diverticulitis, we used the Ambrosetti classification, which is simple and widely used, as recorded in the literature. However, the Ambrosetti classification has some disadvantages compared with other classifications [11]. It includes heterogeneous patients in the group classified as severe. For this reason, size, location (pericolic, pelvic, or mesenteric) and number of abscesses, and the presence of extraluminal air were reviewed and analyzed as single predictive factors in the uni- and multivariate analyses. Furthermore, the patients with diffuse peritonitis who needed emergency surgery at their first episode were excluded from the analysis.
The recommended management for the patients recovered after a severe episode of diverticulitis was based on the high risk for the development of a severe recurrent sepsis [6, 7].
The reported recurrence rate after acute diverticulitis treated conservatively is about 30 % (range 7–54 %) [2, 7, 12]. In the current series of 560 patients followed up for a mean of more than 5 years, the overall recurrence rate after acute diverticulitis was 14.8 %. The rate of severe recurrence after acute diverticulitis was 3.4 %, and the cumulative rate of severe recurrence 1 year after severe diverticulitis was 7 %. The majority of these recurrent episodes occurred in the first year after acute diverticulitis. Whether these rates are to be considered sufficiently high for clinicians to recommend prophylactic surgery may remain controversial. This study suggests a more benign natural history of acute diverticulitis successfully managed conservatively.
Recommendations also were maintained with the assumption that the chance of recurrence and the severity of recurrence are related to the severity of the first episode. Use of the CT scan provides important details such as the presence, size, number, and location of abscesses or the presence of extraluminal air [6]. Kaiser et al. [7] reported that a CT scan finding of an abscess is a relevant prognostic sign of severe diverticulitis because it correlates with a high risk of recurrence and suggests elective surgery after successful percutaneous drainage.
In the current series, the rate of recurrence after severe diverticulitis, although higher, did not differ statistically from that of recurrence after mild diverticulitis, and the cumulative rate of recurrence at 1 year did not differ relative to the severity of first episodes. However, the rate of severe recurrence after a severe diverticulitis was 9.6 %. The chance of having a severe recurrence was greater after a severe diverticulitis than after a mild diverticulitis. Again, the magnitude of this difference needs to be considered when elective surgery is advised.
Recurrence has been related to a multitude of factors such as severity at presentation, age, and underlying comorbidities [6, 13, 14]. As recently published by our group and supported by other authors, the risk of recurrence and the need for surgery after a first successfully managed diverticulitis are independent of preexisting immunosuppression and age [13–17].
The aim of prophylactic colectomy is to avoid emergency surgery for severe diverticulitis, which implies higher morbidity, mortality, and rate of stoma construction [5]. In the current series, the chance of needing emergency surgery for a recurrence was 4 % after severe diverticulitis and higher than 0.7 % after a mild diverticulitis. For the eight patients who underwent surgery for recurrence, the morbidity rate was 37.5 %. Two patients died, and two patients needed a permanent stoma. However, prophylactic colectomy presents its own drawbacks, which must be kept in mind. The recurrence rate for diverticulitis after colectomy is 2.6–10 % [18–20], and prophylactic colectomy does not always result in improvement of symptoms, which can even worsen [21, 22]. Its reported rate of intestinal diversion ranges from 2.9 to 12.7 % [23–25].
Recently, in a retrospective multivariate analysis, Van Arendonk et al. [26] showed a poor outcome after elective colectomy for diverticular disease compared with colon resection for colonic cancer. The authors found a higher postoperative mortality rate, a higher complication rate, a longer hospital stay, more stoma construction, and higher costs.
It is reported that a substantial percentage of patients treated with percutaneous drainage are able to avoid any surgical intervention during the follow-up period without relevant morbidity [8, 27–30]. In the current series, none of the nine patients treated by percutaneous drainage were scheduled for elective surgery, and only one patient needed emergency surgery for severe recurrence. Similar results were reported by Myers et al. [31] after laparoscopic lavage and drainage of perforated diverticulitis. These authors found that only two patients were readmitted for diverticulitis, and no patient required colonic resection for complications of diverticular disease during the follow-up period. Furthermore, data suggesting that an episode of severe diverticulitis may result in a buttressing effect around the affected portion of the colon, thereby protecting from subsequent attacks, have been published [32].
In conclusion, this study describes a more benign natural history after acute diverticulitis successfully managed without surgery than that reported in the literature. Although severe recurrence is related to the severity of the first diverticulitis episode, the findings suggest that the severity of recurrence may have been overvalued and that it may be a wise strategy to individualize the indication of prophylactic surgery even in cases of recovered severe diverticulitis and percutaneous drainage of abscesses. Emergency surgery after successful conservative management of acute diverticulitis is rare. Strict follow-up evaluation during the first year is advised.
References
Ferzoco LB, Raptopoulos V, Silen W (1998) Acute diverticulitis. N Engl J Med 21:1521–1526
Biondo S, Lopez Borao J, Millan M et al (2012) Current status of the treatment of acute colonic diverticulitis: a systematic review. Colorectal Dis 14:e1–e11
Ambrosetti P, Jenny A, Becker C et al (2000) Acute left colonic diverticulitis: compared performance of computed tomography and water-soluble contrast enema: prospective evaluation of 420 patients. Dis Colon Rectum 43:1363–1367
Biondo S, Golda T, Kreisler E et al (2014) Outpatient versus hospitalization management for uncomplicated diverticulitis: a prospective, multicenter randomized clinical trial (DIVER Trial). Ann Surg 259:38–44
Trenti L, Biondo S, Golda T et al (2011) Generalized peritonitis due to perforated diverticulitis: Hartmann’s procedure or primary anastomosis? Int J Colorectal Dis 26:377–384
Rafferty J, Shellito P, Hyman NH et al (2006) Standards Committee of American Society of Colon and Rectal Surgeons: practice parameters for sigmoid diverticulitis. Dis Colon Rectum 49:939–944
Kaiser AM, Jiang JK, Lake JP et al (2005) The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol 100:910–917
Elagili F, Stocchi L, Ozuner G et al (2014) Outcomes of percutaneous drainage without surgery for patients with diverticular abscess. Dis Colon Rectum 57:331–336
Franklin ME Jr, Dorman JP, Jacobs M et al (1997) Is laparoscopic surgery applicable to complicated colonic diverticular disease? Surg Endosc 11:1021–1025
Wong WD, Wexner SD, Lowry A et al (2000) Practice parameters for the treatment of sigmoid diverticulitis-supporting documentation. The Standards Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum 43:290–297
Klarenbeek BR, de Korte N, van der Peet DL, Cuesta MA (2012) Review of current classification for diverticular disease and translation into clinical practice. Int J Colorectal Dis 27:207–214
Soni S, Sudeep T, Prasoon PM et al (2008) Management of Hinchey II diverticulitis. World J Gastroenterol 14:7163–7169
Lopez-Borao J, Kreisler E, Millan M et al (2012) Impact of age on recurrence and severity of left colonic diverticulitis. Colorectal Dis 14:e407–e412
Biondo S, Borao JL, Kreisler E et al (2012) Recurrence and virulence of colonic diverticulitis in immunocompromised patients. Am J Surg 204:172–179
Hwang SS, Cannom RR, Abbas MA et al (2010) Diverticulitis in transplant patients and patients on chronic corticosteroid therapy: a systematic review. Dis Colon Rectum 53:1699–1707
Spivak H, Weinrauch S, Harvey JC et al (1997) Acute colonic diverticulitis in the young. Dis Colon Rectum 40:570–574
Ambrosetti P, Robert JH, Witzig JA et al (1994) Acute left colonic diverticulitis in young patients. J Am Coll Surg 179:156–160
Leigh JE, Judd ES, Waugh JM (1962) Diverticulitis of the colon: recurrence after apparently adequate segmental resection. Am J Surg 103:51–54
Benn PL, Wolff BG, Ilstrup DM (1986) Level of anastomosis and recurrent colonic diverticulitis. Am J Surg 151:269–271
Thaler K, Baig MK, Berho M et al (2003) Determinants of recurrence after sigmoid resection for uncomplicated diverticulitis. Dis Colon Rectum 46:385–388
Forgione A, Leroy J, Cahill RA et al (2009) Prospective evaluation of functional outcome after laparoscopic sigmoid colectomy. Ann Surg 249:218–224
Egger B, Peter MK, Candinas D (2008) Persistent symptoms after elective sigmoid resection for diverticulitis. Dis Colon Rectum 51:1044–1048
Etzioni DA, Mack TM, Beart RW Jr et al (2009) Diverticulitis in the United States: 1998–2005: changing patterns of disease and treatment. Ann Surg 249:210–217
Klarenbeek BR, Samuels M, Van der Wal MA et al (2010) Indications for elective sigmoid resection in diverticular disease. Ann Surg 251:670–674
Lidor AO, Schneider E, Segal J et al (2010) Elective surgery for diverticulitis is associated with high risk of intestinal diversion and hospital readmission in older adults. J Gastrointest Surg 14:1867–1873
Van Arendonk KJ, Tymitz KM, Gearhart SL et al (2013) Outcomes and costs of elective surgery for diverticular disease: a comparison with other diseases requiring colectomy. JAMA Surg 148:316–321
Ambrosetti P, Chautems R, Soravia C et al (2005) Long-term outcome of mesocolic and pelvic diverticular abscesses of the left colon: a prospective study of 73 cases. Dis Colon Rectum 48:787–791
Singh B, May K, Coltart I et al (2008) The long-term results of percutaneous drainage of diverticular abscess. Ann R Coll Surg Engl 90:297–301
Durmishi Y, Gervaz P, Brandt D et al (2006) Results from percutaneous drainage of Hinchey stage II diverticulitis guided by computed tomography scan. Surg Endosc 20:1129–1133
Brandt D, Gervaz P, Durmishi Y et al (2006) Percutaneous CT scan-guided drainage vs. antibiotherapy alone for Hinchey II diverticulitis: a case–control study. Dis Colon Rectum 49:1533–1538
Myers E, Hurley M, O’Sullivan CO et al (2008) Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg 95:97–101
Chapman JR, Dozois EJ, Wolff BG et al (2006) Diverticulitis: a progressive disease? Do multiple recurrences predict less favourable outcomes? Ann Surg 243:876–880
Acknowledgments
The authors thank Mr. Bernat Miguel, Data Manager of the Colorectal Section of the Department of General and Digestive Surgery at Bellvitge University Hospital, Barcelona, for statistical analysis.
Conflict of interest
None to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trenti and Kreisler have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Trenti, L., Kreisler, E., Galvez, A. et al. Long-Term Evolution of Acute Colonic Diverticulitis After Successful Medical Treatment. World J Surg 39, 266–274 (2015). https://doi.org/10.1007/s00268-014-2773-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2773-y