Abstract
Background
The objective of the present study was to assess the hard and soft tissue differences of skeletal Class III malocclusion patients treated with orthodontic–orthognathic surgery treatment between two decompensation approaches including extraction of maxillary premolars in preoperative orthodontics and clockwise rotation of the maxilla in orthognathic surgery.
Methods
22 skeletal Class III patients with the crowding of maxillary dental arch less than 3mm were included in this study. These patients were divided into two groups: extraction group and non-extraction group. Lateral cephalograms taken before preoperative orthodontic treatment and after postoperative orthodontic treatment were used to analyze the differences of hard and soft tissues between two groups. Independent t test was used to evaluate the differences of variables between extraction group and non-extraction group.
Results
After treatment, there was significant difference of Wits between extraction group and non-extraction group (− 4.34 mm vs − 2.82 mm, respectively, P <0.05). Co-Gn was significantly greater in non-extraction group than in extraction group (77.18 mm vs 71.58 mm, P <0.05). U1-SN and L1-MP in extraction group were significantly closer to the normal values than non-extraction group (P <0.05). Regarding the change of variables before and after orthodontic–orthognathic treatment, NLA (7.25° vs 1.46°, P <0.01) and G-Sn-Pog’ (8.06° vs 4.62°, P <0.05) were significantly greater in extraction group than in non-extraction group.
Conclusion
For patients with skeletal Class III malocclusion, extraction of maxillary premolars in preoperative orthodontic treatment can more effectively eliminate the dental compensation and achieve a more harmonious facial profile compared to clockwise rotation of the maxilla in orthognathic surgery.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Skeletal Class III malocclusion is a common facial dysmorphia in clinical practice, which accounts for 5–15% of the population all around the world [1, 2]. Deformities of jaws usually have impacts on the occlusal function, facial appearance, and mental health of the patients [3, 4]. Mild cases can be treated with orthodontics alone to compensate for the jaws’ deformation; however, patients with skeletal Class III malocclusion usually have thinner inferior anterior alveolar bone than Class I malocclusion, which adds difficulty to the movement of teeth [5]. Moreover, for the patients with skeletal Class III malocclusion, the aim of treatment is not only to correct dental malocclusion but also to improve facial aesthetics and harmonize the facial profile [6,7,8]. Therefore, skeletal Class III malocclusion usually requires orthodontic–orthognathic surgery treatment [9].
The regular procedures of orthodontic–orthognathic surgery treatment include preoperative orthodontic treatment to eliminate the dental compensation and match the dental arches, surgical correction of the skeletal discrepancy, and postoperative detailing and finishing of the occlusion [10,11,12]. In preoperative orthodontic treatment, extraction of the maxillary premolars is a common method for dental decompensation [13, 14]. Whereas not all the patients with skeletal Class III malocclusion need extraction of the maxillary premolars, many factors should be considered before orthodontic–orthognathic surgery treatment, such as the position of jaws, paranasal fullness, and the crowding of dental arch [15]. Additionally, whether to extract maxillary premolars or not, to some extent, depends on the desires of patients and the experience of doctors. For the patient who do not receive the maxillary premolar extraction, the dental compensation is usually eliminated by the clockwise rotation of maxilla and the impaction of the posterior maxilla in orthognathic surgery. Hence, the effects of the two decompensation approaches on the treatment outcomes should be evaluated for making treatment planning.
However, nearly all of the previous studies have focused on the effect of maxillary premolar extraction on the occlusion or other dental factors [16,17,18], study that reported the decompensation approaches on facial profile are lacking, although the facial appearance is of great significance for orthodontic–orthognathic surgery treatment in clinical practice. Therefore, the aim of the present study was to assess the hard and soft tissue differences of skeletal Class III malocclusion patients treated with 2-jaw surgery between two decompensation approaches including extraction of maxillary premolars in preoperative orthodontics and the clockwise rotation of maxilla in orthognathic surgery, providing practical and specific guidelines for predicting the changes of facial profile.
Materials and Methods
Study Population and Design
In this retrospective study, 22 qualified patients with skeletal Class III malocclusion who attended to Dalian Stomatological Hospital were selected. This study was approved by the Ethics Committee of Dalian Stomatological Hospital (DLKQLL2016010) and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The patients were allocated into two groups: extraction group (maxillary premolars were extracted during preoperative orthodontic treatment to eliminate the dental compensation, 10 patients) and non-extraction group (maxillary premolars were not extracted during orthodontic–orthognathic surgery treatment, and the dental compensations were eliminate by the clockwise rotation of maxilla in orthognathic surgery, 12 patients). Patients included in this study were selected based on the following inclusion criteria: (1) the age at the first visit >18; (2)−12°<ANB Angle<0°; (3) the crowding of maxillary dental arch less than 3mm and all the third molars were extracted before preoperative orthodontic treatment; (4) received orthodontic–orthognathic surgery treatment; (5) eliminating dental compensation by extraction of the maxillary premolars or clockwise rotation of maxilla in orthognathic surgery; (6) treated by maxillary LeFort I osteotomy and bilateral mandibular sagittal split ramus osteotomy (BSSRO); (7) no adjustment of anteroposterior position of incisors in the post-surgical orthodontic treatment; (8) had complete treatment records and clear lateral cephalograms. The exclusion criteria including open bite, craniofacial anomalies like cleft palate and the dysplasia of the number or size of tooth like microdontia.
Orthodontic–Orthognathic Surgery Treatment
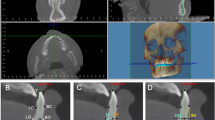
All patients received preoperative orthodontic treatment with 0.022 × 0.028-inch MBT pre-adjusted appliances which aims to align the dental arches, level the curve of Spee, remove dental compensations, and prepare for the orthognathic surgery. Maxillary premolars were extracted during preoperative orthodontic treatment in extraction group to eliminate the dental compensation. After preoperative orthodontic treatment, all patients underwent orthognathic surgery including Lefort I osteotomy and BSSRO. In non-extraction group, the maxilla was rotated in a clockwise direction and the posterior maxilla was impacted in orthognathic surgery. As for the post-surgical orthodontics, the purpose was to detailed adjust and stabilize the occlusion. All the patients were treated by the same orthodontic doctor and surgeon. After the orthodontic–orthognathic surgery treatment, all the patients achieved stable occlusion, normal overbite and overjet, harmonious curve of Spee and the neutral canine relationship. The molars relationship of extraction group was completely distal relationship, while the non-extraction group had a bilateral neutral molar relationship. Figure 1 shows the facial and intraoral photographs and lateral cephalograms of example patients of two groups before and after orthodontic–orthognathic surgery treatment.
Data Acquisition
Regarding the demographic data, gender, age, treatment durations, amounts of crowding of maxillary and mandibular arch, amounts of reverse overjet, and satisfaction level of each patient were recorded. The satisfaction rating method is for patients to rate the effectiveness of their own treatment, with a rating range of 1-5 points. The higher the score, the higher the satisfaction level. In order to analyze the effect of maxillary premolar extraction preoperatively on the treatment outcomes, the cephalometric landmarks (Fig. 2) and parameters (Figs. 3, 4) of hard and soft tissues were measured by the same operator using Dolphin Imaging software (Version 11.95.08.50 Premium); values were measured three times; then, the averages were obtained. The lateral cephalograms used in the study were taken before preoperative orthodontic treatment and after postoperative orthodontic treatment, with jaws in centric occlusion, natural head position and reposed lip. Scan conditions: tube voltage 73 kv, 15 mA tube current, and the sensor 28.1 inches from the light source, the exposure time is 9.3 seconds; the data obtained by an amorphous silicon flat panel detector.
Landmarks and reference planes of hard tissue (a) and soft tissue (b): S, Sella; N, nasion; Po, porion; O, orbitale; Co, condylion; Ar, articulare; Go, gonion; ANS, anterior nasal spine; PNS, posterior nasal spine; A, subspinale; UI, upper incisor; UIA, upper incisor apex, U1, long axis of upper incisor; Ao, foot of a perpendicular of A point to occlusal plane; B, supramental; LI, lower incisor; LIA, lower incisor apex; L1, long axis of lower incisor; Bo, foot of a perpendicular of B point to occlusal plane; Pog, pogonion; Gn, gnathion; Me, menton; SN, SN plane; FH, Frankfort horizontal plane; PP, palatal plane; OP, occlusal plane; MP, mandibular plane; G, glabella; N’, nasion of soft tissue; Pn, prenasale; Cm, columella; Sn, subnasale; A’, superior labial sulcus; UL, upper lip; Ls, labial surface of upper incisor; LL, lower lip; Si, mentolabial sulcus; Pog’, pogonion of soft tissue; H line, the line of UL to Pog’; E line, the line of Pn to Pog’
Cephalometric variables of soft tissue: 1, FH-N’Pog’ (°); 2, Nasolabial angle (NLA, °); 3, G-Sn-Pog’ (°); 4, H angle (°); 5, S-N’-Sn (°); 6, S-N’-Si (°); 7, Si-E (mm); 8, UL-E (mm); 9, LL-E (mm); 10, Superior sulcus depth (SSD, mm); 11, Basic upper lip thickness (BULT, mm); 12, UL-Ls (mm); 13, Si-H (mm); 14, Pog-Pog’ (mm)
Statistical Analysis
The collected data were analyzed utilizing IBM SPSS Statistics 20.0 software. Independent t test was used to analyze the differences of hard and soft tissues between extraction group and non-extraction group. The results were estimated and reported as mean differences with 95% confidence intervals. P value <0.05 was considered as statistical significance.
Results
Demographic Data
22 patients were included in this study (9 males and 13 females, main age = 24.2 ± 3.3 years), 10 patients in extraction group (5 males and 5 females, main age = 23.9 ± 3.7 years), and 12 patients in non-extraction group (4 males and 8 females, main age = 24.4 ± 3.0 years). The durations of preoperative orthodontic treatment and total orthodontic treatment of extraction group were increased by 35.99% and 25.31%, respectively, than non-extraction group, while no statistical difference was found in the durations of postoperative orthodontic treatment between two groups. Moreover, there were no statistical differences in amounts of crowding of maxillary and mandibular arches, amounts of reverse overjet, and satisfaction level between two groups (Table 1).
Comparison of the Variables Between Extraction Group and Non-Extraction Group Before Treatment
In the hard tissue parameters, the mean value of NA-PA Angle was significantly greater in non-extraction group than in extraction group (− 13.03° vs − 6.92°, P <0.05), showing that the depression of maxilla was more obvious in non-extraction group than that in extraction group. Moreover, Co-Gn, reflecting the length of mandible, was significantly greater in non-extraction group than in extraction group (143.38 mm vs 132.48 mm, P <0.01). No significant differences were found in other hard tissue parameters between two groups (Table 2).
Regarding the soft tissue parameters, the mean value of Angle H was significantly greater in extraction group than in non-extraction group (11.08° vs 5.71°, P <0.001), showing that the chin protrusion was greater in non-extraction group than that in extraction group. The thickness of the upper lip was significantly greater in non-extraction group than in extraction group according to the comparison of the base of upper lip and UL-Ls (P <0.05, P <0.01, respectively). No significant differences were found in other hard tissue parameters between two groups (Table 3).
Comparison of the Variables Between Extraction Group and Non-Extraction Group After Treatment
As for the hard tissue, although there was significant difference of ANB Angle between extraction group and non-extraction group (2.69° vs 1.04°, respectively, P <0.01), these two values were both in the normal range (0°–5°); there was significant difference of Wits between extraction group and non-extraction group (− 4.34 mm vs − 2.82 mm, respectively, P <0.05), and the value in extraction group was closer to the normal values (− 0.8 mm) than non-extraction group, suggesting the extraction group get more harmonious relationship between anterior maxilla and anterior mandible in sagittal plane. Significant differences of U1-SN and L1-MP were found between extraction group and non-extraction group (P <0.05), and these two variables in extraction group were closer to the normal values than non-extraction group, showing that extraction group has more ideal outcomes in terms of the inclinations of maxillary and mandibular incisors. Additionally, significant differences of Go-Gn and Co-Gn between two groups suggesting that the lengths of mandible and mandibular body in non-extraction group were greater than that in extraction group. No significant differences were found in other hard tissue parameters between two groups (Table 4).
Concerning the soft tissue, the G-Sn-Pog’ Angle was significantly greater in extraction group than in non-extraction group (6.42° vs 1.94°, P <0.01), showing that the midface depression was better corrected in extraction group than in non-extraction group. The mean value of UL-Ls, reflecting the thickness of the upper lip, was significantly greater in non-extraction group than in extraction group (14.67 mm vs 12.71 mm, P <0.01). No significant differences were found in other soft tissue parameters between two groups (Table 5).
Comparison of the Differences of Hard and Soft Tissues Before and After Orthodontic–Orthognathic Treatment Between Extraction Group and Non-Extraction Group
In the hard tissue, the change of PP angle was significantly greater in non-extraction group than in extraction group (0.49° vs 2.87°, P <0.001), exhibiting that the dental compensations in non-extraction group were eliminated by the clockwise rotation of maxilla; the change of NA-PA angle was significantly greater in non-extraction group than in extraction group (9.27° vs 2.88°, P <0.01), showing that the change of relative position of maxilla was greater in non-extraction group than in extraction group; significant differences of the change of Go-Gn between two groups suggesting that the length change of mandibular body in extraction group were greater than that in non-extraction group (− 8.98 mm vs − 6.15 mm, P <0.05); the decrease in U1-SN angle which reflecting the inclinations of maxillary incisors was significantly greater in extraction group than in non-extraction group (7.69° vs − 1.37°, P <0.05), No significant differences were found in other hard tissue parameters between two groups (Table 6).
As for soft tissue, the changes of NLA (7.25° vs 1.46°, P <0.01), G-Sn-Pog’ (8.06° vs 4.62°, P <0.05), and S-N’-Si (4.69° vs − 2.53°, P <0.05) were significantly greater in extraction group than in non-extraction group, suggesting that the changes of nasolabial angle, the depression of midfacial soft tissue, and the protrusion of mandibular soft tissue were greater in extraction group than in non-extraction group; the change of Angle H was significantly greater in non-extraction group than in extraction group (4.52° vs 1.14°, P <0.05), showing that the change of chin protrusion was greater in non-extraction group than that in extraction group. No significant differences were found in other soft tissue parameters between two groups (Table 7).
Discussion
For patients with skeletal Class III malocclusion who undergo 2-jaw surgery, there are two available methods to eliminate dental compensation during orthodontic–orthognathic surgery treatment: extraction of maxillary premolars and clockwise rotation of maxilla [13,14,15]. However, few studies have reported the effects of the decompensation approaches on the facial profile. The present study aimed to investigate the effects of two decompensation approaches, including extraction of maxillary premolars in preoperative orthodontics and the clockwise rotation of maxilla in orthognathic surgery, on the facial hard and soft tissues. The findings will provide practical and specific guidelines for treatment planning in cases of skeletal Class III malocclusion. The results of the present study indicated that although the duration of orthodontic treatment was significantly longer in the extraction group compared to non-extraction group, extraction group exhibited advantages in correcting dental compensation and midfacial depression and achieved more harmonious relationship of jaws and facial soft tissue profile.
One of the goals of preoperative orthodontic treatment for skeletal Class III malocclusion patients is to eliminate the dental compensation [19]; the extraction of maxillary premolars is an effective method in clinical practice. However, extraction of maxillary premolars may not always be feasible due to certain factors, such as: (1) severe retraction of maxilla which cannot be thoroughly corrected by orthognathic surgery; (2) maxillary anterior teeth cannot achieve large-scale movement due to thin alveolar bone or severe periodontitis; (3) patient who requires receiving orthognathic surgery as soon as possible; (4) patient whose demand is to achieve stable and functional occlusion rather than appearance. As for these patients, clockwise rotation of maxilla and the impaction of the posterior maxilla in orthognathic surgery are commonly used to eliminate the dental compensation, rather than extracting maxillary premolars [15]. Concerning the effect of maxillary premolars extraction on orthodontic–orthognathic surgery treatment, nearly all the existing studies focused on the dental arch. Lee et al. insisted that the arch-width change resulting from maxillary premolar extraction in preoperative orthodontic treatment contributed to the intermaxillary arch congruity [18]; Kim et al. and Park et.al reported that maxillary premolars extraction can achieve larger amount of the maxillary incisor inclination change than non-extraction group [16, 17]. Other studies have focused on the effects of premolar extraction on regular orthodontic treatment [20,21,22]; hence, the effect of maxillary premolars extraction on the facial profile should be well investigated.
Regarding the demographic data of the two groups, the outcomes showed that the durations of preoperative orthodontic treatment and total orthodontic treatment of extraction group increased compared to non-extraction group, due to the need to close the remaining spaces from the extraction of maxillary premolars. Furthermore, no statistical differences were found in amounts of crowding of maxillary and mandibular arches, amounts of reverse overjet, and satisfaction level between two groups. These results indicated that the two groups had the same baseline, and the patients’ condition including the amounts of crowding of dental arches and reverse overjet will not affect the selection of the treatment plan, thus ensuring the credibility of the research outcomes. The results of the satisfaction survey showed that both groups of patients had similar satisfaction with the treatment effect, even though there are some differences in parameters of hard and soft tissues. In the present study, we employed comprehensive parameters of hard and soft tissues to elaborate the effect of maxillary premolars extraction on the facial profile. In the comparison of the variables between extraction group and non-extraction group before treatment, we found that NA-PA Angle, Co-Gn and H Angle were significantly greater in non-extraction group than in extraction group. However, no significant differences were found in ANB angle, Wits, and G-Sn-Pog’ angle between two groups. This suggested that the reason for midfacial depression was the protrusion of the chin, and the relationships of maxilla and mandible between two groups had no significant difference, providing the possibility for comparing the facial profile after treatment between two groups.
In the analysis of hard tissue, the change of PP angle was significantly greater in non-extraction group than in extraction group proving that the dental compensations in non-extraction group were eliminated by the clockwise rotation of maxilla, while no obvious rotation of maxilla in extraction group was observed. Mean value of U1-SN in extraction group after treatment was significantly closer to the normal value (105.7°) than non-extraction group, and the significantly greater change before and after treatment suggesting that extraction group achieved more thoroughly decompensation of maxillary incisors than non-extraction group by moving the maxillary anterior teeth backward, which was in accordance with the reports of Kim et al. and Park et.al [16, 17]. Similarly, a significant difference of L1-MP between groups exhibited the extraction group did better in eliminating the compensation of mandibular incisors than non-extraction group. No significant difference was found in Go-Gn between two groups before treatment, while Go-Gn in non-extraction group was significantly greater than extraction group after treatment, and the change before and after treatment in non-extraction group was significantly less than extraction group, showing that extraction group had larger amount of mandibular retraction. In two groups, ANB Angles, reflecting the relationship of maxilla and mandible, were both restored to the normal range after treatment; while Wits in extraction group was significantly closer to the normal value than non-extraction group showed that extraction group get more harmonious relationship between anterior maxilla and anterior mandible in sagittal plane.
With respect to the soft tissue, no significant difference was found in G-Sn-Pog’ between two groups before treatment, while G-Sn-Pog’ in extraction group was significantly closer to the normal value 10.5° than non-extraction group after treatment and the change before and after treatment in extraction group was significantly greater than non-extraction group, showing that extraction group achieved more harmonious profile of soft tissue [23]. Significant difference of the NLA change before and after treatment between groups showed that maxillary premolars extraction has remarkable impact on the nasolabial angle. Owing to no significant differences of SNA and S-N’-Sn between groups were found, we speculate this impact may result from the inclination change of maxillary incisors. Moreover, significantly reduced S-N’-Si and significantly increased Go-Gn in extraction group before and after treatment suggested that extraction group obtained greater retraction of mandibular hard and soft tissues, which may also contribute to the change of nasolabial angle. This speculation was similar to the result of Ohba et al. who reported that the amount of nasolabial angle was associated with the retraction of mandible [24].
Due to the limitation of the sample size, we merely analyzed the patients with skeletal Class III malocclusion. In further study, other kinds of skeletal malocclusion should be included for the detailed illustration of the effects of decompensation approaches on facial profile, providing more effective guidelines for the establishment of treatment planning in clinical practice.
Conclusion
Compared to the clockwise rotation of maxilla in orthognathic surgery, extraction of maxillary premolars in preoperative orthodontic treatment can obtain better outcomes in eliminating dental compensation and achieving more harmonious facial profile in terms of hard and soft tissues for skeletal Class III malocclusion patients treated with 2-jaw surgery. This provides practical and specific guidelines for the aesthetic design of orthodontic–orthognathic surgery treatment.
References
Woon SC, Thiruvenkatachari B (2017) Early orthodontic treatment for class III malocclusion: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 151:28–52
Tseng LL, Chang CH, Roberts WE (2016) Diagnosis and conservative treatment of skeletal class III malocclusion with anterior crossbite and asymmetric maxillary crowding. Am J Orthod Dentofacial Orthop 149:555–566
Rongo R, D’antò V, Bucci R, Polito I, Martina R, Michelotti A (2017) Skeletal and dental effects of class III orthopaedic treatment: a systematic review and meta-analysis. J Oral Rehabil 44:545–562
Güzel MZ, Saraç M, Arslan H, Nejat E, Nazan K (2007) A new face by combined surgery for patients with complex dentofacial deformity. Aesthetic Plast Surg 31:32–41
Handelman CS (1996) The anterior alveolus: its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod 66:95–109 (Discussion 109-110)
Eslami S, Faber J, Fateh A, Sheikholaemmeh F, Grassia V, Jamilian A (2018) Treatment decision in adult patients with class III malocclusion: surgery versus orthodontics. Prog Orthod 19:28
Oland J, Jensen J, Elklit A, Melsen B (2011) Motives for surgical-orthodontic treatment and effect of treatment on psychosocial well-being and satisfaction: a prospective study of 118 patients. J Oral Maxillofac Surg 69:104–113
Lee SW, Cho J, Kim K, Ahn SH (2017) Frontal changes in the lower face after clockwise rotation of the maxillomandibular complex without perisurgical orthodontic treatment in angle class I and skeletal class III women. Aesthetic Plast Surg 41:641–649
Xiao Y, Sun X, Wang L, Zhang Y, Chen K, Wu G (2017) The application of 3D printing technology for simultaneous orthognathic surgery and mandibular contour osteoplasty in the treatment of craniofacial deformities. Aesthetic Plast Surg 41:1413–1424
Raposo R, Peleteiro B, Paço M, Pinho T (2018) Orthodontic camouflage versus orthodontic–orthognathic surgical treatment in class II malocclusion: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 47:445–455
Möhlhenrich SC, Kötter F, Peters F, Kniha K, Chhatwani S, Danesh G, Hölzle F, Modabber A (2021) Effects of different surgical techniques and displacement distances on the soft tissue profile via orthodontic–orthognathic treatment of class II and class III malocclusions. Head Face Med 17:13
Park CG, Yoo JW, Park IC (1994) Surgical treatment of mandibular prognathism in collaboration with orthodontic treatment in Korea. Aesthetic Plast Surg 18:407–412
Ko EW, Hsu SS, Hsieh HY, Wang YC, Huang CS, Chen YR (2011) Comparison of progressive cephalometric changes and postsurgical stability of skeletal class III correction with and without presurgical orthodontic treatment. J Oral Maxillofac Surg 69:1469–1477
Troy BA, Shanker S, Fields HW, Vig K, Johnston W (2009) Comparison of incisor inclination in patients with class III malocclusion treated with orthognathic surgery or orthodontic camouflage. Am J Orthod Dentofacial Orthop 135:146.e141-149 (Discussion 146-147)
Baek SH, Kim K, Choi JY (2009) Evaluation of treatment modality for skeletal class III malocclusion with labioversed upper incisors and/or protrusive maxilla: surgical movement and stability of rotational maxillary setback procedure. J Craniofac Surg 20:2049–2054
Park HM, Lee YK, Choi JY, Baek SH (2014) Maxillary incisor inclination of skeletal class III patients treated with extraction of the upper first premolars and two-jaw surgery: conventional orthognathic surgery vs surgery-first approach. Angle Orthod 84:720–729
Kim DK, Baek SH (2013) Change in maxillary incisor inclination during surgical-orthodontic treatment of skeletal class III malocclusion: comparison of extraction and nonextraction of the maxillary first premolars. Am J Orthod Dentofacial Orthop 143:324–335
Lee SJ, Kim TW, Nahm DS (2006) Transverse implications of maxillary premolar extraction in class III presurgical orthodontic treatment. Am J Orthod Dentofacial Orthop 129:740–748
Johnston C, Burden D, Kennedy D, Harradine N, Stevenson M (2006) Class III surgical-orthodontic treatment: a cephalometric study. Am J Orthod Dentofacial Orthop 130:300–309
Konstantonis D, Vasileiou D, Papageorgiou SN, Eliades T (2018) Soft tissue changes following extraction vs. nonextraction orthodontic fixed appliance treatment: a systematic review and meta-analysis. Eur J Oral Sci 126:167–179
Leonardi R, Annunziata A, Licciardello V, Barbato E (2010) Soft tissue changes following the extraction of premolars in nongrowing patients with bimaxillary protrusion. A systematic review. Angle Orthod 80:211–216
Iared W, Koga Da Silva EM, Iared W, Rufino Macedo C (2017) Esthetic perception of changes in facial profile resulting from orthodontic treatment with extraction of premolars: a systematic review. J Am Dent Assoc 148:9–16
Lew KK, Ho KK, Keng SB, Ho KH (1992) Soft-tissue cephalometric norms in Chinese adults with esthetic facial profiles. J Oral Maxillofac Surg 50:1184–1189 (Discussion 1189-1190)
Ohba S, Kohara H, Koga T, Kawasaki T, Miura KI, Yoshida N, Asahina I (2017) Soft tissue changes after a mandibular osteotomy for symmetric skeletal class III malocclusion. Odontology 105:375–381
Acknowledgements
The authors are grateful to the patients who provided informed consent for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to disclose.
Ethical Approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent form was signed for all the patients who underwent surgery.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, L., Liu, Y., Han, L. et al. Comparison of Different Decompensation Approaches on Facial Profile in Orthodontic–Orthognathic Treatment for Skeletal Class III Patients. Aesth Plast Surg 47, 1957–1966 (2023). https://doi.org/10.1007/s00266-023-03546-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-023-03546-1