Abstract
Background
Because of the limitation of specific preoperative design and surgical templates, orthognathic surgery and mandibular contour osteoplasty are generally performed in two stages. Three-dimensional printing technology has improved the accuracy of the surgery and results in good surgical predictability easily. This study aims to confirm the effectiveness, feasibility and precision of simultaneous mandibular contour osteoplasty and orthognathic surgery with the assistance of 3D printing technology.
Methods
Ten patients, who were diagnosed with mandibular hypertrophy and bimaxillary deformities, were included in the study. In addition to conventional orthognathic surgery, mandibular angle ostectomy, mandibular outer cortex grinding or mandibular border ostectomy was designed for mandibular hypertrophy. Optimal osteotomy lines and simulated surgeries were designed according the 3D printing model of the mandible. Then, surgical templates were made on the 3D printing model. No muscle excision was performed in any patient. Preoperative, predicted and postoperative measurements were taken, including the gonial angle (Ar–Go–Me) and the mandibular width (Go–Go).
Results
All the patients had a reposeful postoperative recovery, with no indication of obvious infection, facial paralysis, osteonecrosis or bone displacement. The gonial angle was improved from 110.3° ± 11.1 to 121.3° ± 2.9, and the mandibular width was improved from 117.5 mm ± 6.8 to 111.9 mm ± 4.2. The discrepancies between simulation and postoperation of the left gonial angle, the right gonial angle and the mandibular width were 0.56° ± 0.22, 0.65° ± 0.3 and 0.49 mm ± 0.43, respectively.
Conclusions
The results of our study illustrated the predictability, feasibility and reliability of simultaneous mandibular contour osteoplasty and orthognathic surgery with the assistance of 3D printing technology. Our technique could achieve functional improvement and an aesthetic profile at the same time.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
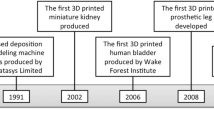
Introduction
Unlike Westerners, Orientals prefer an ovoid and slender outline rather than a square and salient one, so they hope to change their appearance by surgical approaches [1]. The position of the maxilla and mandible is usually altered by orthognathic surgery (OGS) to treat dentofacial deformities and obtain functional improvement in the dentoalveolar complex [2]. Besides the postoperative function, more and more emphases on aesthetics have been put forward. Particularly the mandibular contour including the angle of the mandibular angle and the width of mandible has great influence on the frontal and lateral views. However, without specific preoperative design or surgical templates, mandibular contour osteoplasty and orthognathic surgery are generally performed in two stages [3]. It is difficult to perform the two types of operations in a single-stage surgery precisely. Due to much time and expense spent on two-stage treatment, the desire for one-stage treatment has become increasingly strong. But the reports regarding simultaneous procedures of orthognathic surgery and mandibular angle osteoplasty are few.
Three-dimensional printing technology has gained substantial popularity in recent years, such as the 3D-printed intermediate and final occlusal splint, computerized fabrication of osteotomy and locating guides, individually designed 3D-printed patient-specific implants (PSI) and the simple 3D printing model of bones [4,5,6,7,8]. As simulated surgeries can be performed on the 3D-reconstructed images and surgical templates can be made on the 3D printing model, the surgeon can improve the accuracy of the surgery easily and achieve good surgical predictability and low incidence of complications [9]. Thanks to 3D printing technology, the accuracy of orthognathic surgery has been improved extraordinarily [10, 11].
In view of the shortcomings of two-stage surgery and the desire for one-stage surgery, it is essential to explore the feasibility, effectiveness and security of simultaneous mandibular contour osteoplasty and orthognathic surgery. In this study, several primary practices were taken with the help of 3D printing technology to overcome the drawbacks of one-stage surgery.
Patients and Methods
Ten patients who were diagnosed with mandibular hypertrophy and bimaxillary deformities were recruited from our hospital from July 1, 2015, to June 30, 2016. They were all within the index of orthognathic functional treatment needs (IOFTN) score of 4 (Great Need for Treatment) or 3 (Moderate Need for Treatment) [12]. The patients included seven females and three males ranging from 18 to 36 years old, with an average age of 25 years old. All the patients were informed of the therapeutic process before treatment and gave consent for participation. Patient information, diagnosis and clinical treatment are summarized in Table 1. With the help of the 3D printing model and the surgical templates, all the patients had orthognathic surgery and mandibular contour osteoplasty simultaneously. The institutional review board approved the study protocol, and all the participants signed the informed consent form.
Definite Diagnosis and Preoperative Design
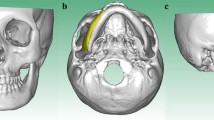
The preoperative three-dimensional scan data of the maxillofacial skeleton and the dental biting casts were exported as communication in digital imaging (DICOM) format files and imported into a specific computer graphics software (Mimics17.0). The corresponding coordinate system and the relevant landmarks were calibrated, as well as the base center line and the reference plane. According to the 3D-reconstructed images, a definite diagnosis can be made, such as asymmetric deformity, mandibular protrusion or retrusion and square mandible deformity.
In the view of individual treatment, besides the objective aesthetic and functional requirement, patients’ aesthetic wishes were also taken into consideration while designing the osteotomy lines. In addition to conventional orthognathic surgery, mandibular angle ostectomy (MAO), mandibular border ostectomy (MBO) or mandibular outer cortex grinding (MOCG) were also designed for mandibular hypertrophy. For MAO and MBO, similar to Han and Kim [13], the osteotomy line was designed according to the following three standards: Firstly, the new gonion (Go) would be located below the auricular lobule 2.5 ± 0.5 cm. It should be within the regular range of the mandibular plane (MP) angle (31.1° ± 5.6) and on the angle bisecting the MP-RP (ramus plane). Secondly, the osteotomy line must be designed under the mandibular nerve tube. The prior end of the osteotomy line might arrive at the mental region, and the posterior end should not be above the occlusion plane. Thirdly, the osteotomy line must be natural and smooth. For MOCG, the borderline resectable area of the lateral cortex is 10.0 mm lateral to the mental foramen and 10.0 mm below the sigmoid notch. The mandibles of most patients were asymmetric accompanied by protrusion, so the resection must be different on both sides to achieve a new facial symmetry. The excised bone was removed on the relatively larger side according to the method above. The osteotomy line of the other side was planned referenced to the mirror graph of the contralateral. All the preoperative designs were made on the 3D-reconstructed image through the software.
Creating the 3D Printing Models and Surgical Templates
The 3D printing model of the 1:1 ratio emulational lower jaw bone was fabricated by rapid prototyping (Objet Eden 250, Israel). The 3D printing model reproduced the actual anatomy of the mandible, especially the location of the inferior alveolar canal and the thickness of the lateral cortex of the mandible.
The 3D printing model was used to simulate the actual operational process by segmenting, moving and spelling. The preoperative design was transferred to the 3D printing model, and the surgical templates were made with self-curing plastic according to the designed osteotomy lines (Fig. 1). To locate the templates on the mandible accurately, the templates were appropriately extended to the inferior border and lingual surface of the mandible.
Surgical Procedures
All the patients were operated on through the intraoral approach under general anesthesia. Equal lidocaine (2%) mixed with epinephrine (1:100,000) was injected along the incision line, and the mucosa was incised to expose the maxilla and mandible. The surgical sequence was as follows. We did the Le Fort I osteotomy first and then mandibular angle ostectomy or mandibular border ostectomy, sagittal split ramus osteotomy or unilateral inverted-L osteotomy of the ramus. Mandibular outer cortex grinding and genioplasty were performed last. While performing the conventional orthognathic surgeries, the new position of the jaw was routinely determined by intraoperative and postoperative bite plates. While performing MAO (Fig. 2a, b) and MBO (Fig. 2c), the osteotomy was easily performed along the edge of the surgical templates. While performing MOCG (Fig. 2d), the mark with a reciprocating saw was performed along the edge of the surgical template first and the grinding was performed after the template was taken out. It should be noted that to avoid excessive grinding, the grinding thickness must be strictly according to the preoperative design. While performing genioplasty, patented instruments were used, including the precise repositioning instrument and the appropriate retractors for genioplasty [7, 14]. It took approximately 2–3 h for the whole surgical procedure. No muscle was resected, and no alveolar neurovascular bundle was directly injured in any patient. A negative pressure drain device was kept for one day. Pressure dressings were applied for 5 days, cold packs for 3 days and antibiotics for 3–4 days after operation.
Postoperative Evaluation
The follow-up of each patient was more than one year. The 3D-reconstructed graphs of the maxillofacial skeleton were performed preoperatively and three months after operation, whereas photographs were taken preoperatively and six months after the operation, including occlusive, frontal and lateral photographs. Preoperative, predicted and postoperative measurements were taken, including the gonial angle (Ar–Go–Me) and the mandibular width (Go–Go). The deviations between simulation and postoperation were calculated.
Results
All the patients had a reposeful postoperative recovery, with no indication of obvious infection, facial paralysis, osteonecrosis or bone displacement. As summarized in Table 2, the gonial angle was improved from 110.3° ± 11.1 to 121.3° ± 2.9 and the mandibular width was improved from 117.5 mm ± 6.8 to 111.9 mm ± 4.2. The discrepancies between simulation and postoperation of the left gonial angle, the right gonial angle and the mandibular width were, respectively, 0.56° ± 0.22, 0.65° ± 0.3 and 0.49 mm ± 0.43. All the patients were satisfied with the cosmetic and functional consequences.
Typical Cases
Patient 1
A 30-year-old female patient was diagnosed with asymmetric deformity, prominent angles and class I malocclusion (patient 1 in Table 1). Her lower face was asymmetric and wide, while the right side of the mandible was significantly bigger than the left. The maxilla was minorly overdeveloped, while the chin was not too weak. The data were obtained through the software, including SNA 83°, SNB 86.5° and ANB −3.5°. The gonial angle of the left was 110.3°, the right 108.8°, and the mandibular width 115.6 mm.
The preoperative plan and simulated operation were performed according to the 3D-reconstructed model, including Le Fort I osteotomy, SSRO, bilateral mandibular angle ostectomy and right outer cortex grinding. The right mandibular angle was cut off about 15.0 mm high, whereas 10.0 mm was done on the left side. Part of the right mandibular bone cortex was ground, while the thickness of the remaining part was at least 2.0 mm. No orthodontic treatment was needed. The postoperative occlusion can attain individual normal occlusion by grinding off the high points and occluding interferences. According to the plan above, two bite plates were manufactured and three surgical templates were made to guide the osteotomy (Fig. 3).
Under general anesthesia, intraoral surgical approaches were used to expose the upper and lower jaw. The surgical sequence was as follows. Firstly, Le Fort I osteotomy was performed to treat the maxillary hypoplasia and cant with the help of an intermediate splint. Secondly, the surgical template for mandibular angle ostectomy was fixed on the mandibular angle (Fig. 4). The ostectomy could be easily performed along the edge of the template (Fig. 5). Thirdly, SSRO was performed with the help of a final occlusal splint. Finally, the template for mandibular outer cortex grinding was fixed on the right mandibular angle. The mark with a reciprocating saw was performed along the edge of the surgical template first, and grinding was performed after the template was taken out (Fig. 6). All the rigid internal fixations were achieved with screws and plates routinely.
The patient showed good jaw bone symmetry by CT scan (Figs. 7, 8) and good facial symmetry (Figs. 9, 10) after six months of follow-up. The data after operation were obtained, including SNA 82°, SNB 79° and ANB 3°. The gonial angle of the left was 119.9°, the right 120.5°, and the mandibular width 107.4 mm. The gonial angle and the facial width were improved markedly. The wide lower face had been converted to slender, and the overall facial contour was symmetrical, balanced and harmonious. No osteonecrosis or bone displacement happened.
Patient 2
A 24-year-old male patient was diagnosed with asymmetric deformity and class III malocclusion (patient 5 in Table 1). Facial characteristics: His mandible was asymmetric with the hyperevolutism of the right side. The maxilla, mandible and chin deviated to the right. The anterior cross-bite and the posterior centric occlusion were obvious. The data were obtained through the software, including SNA 81.5°, SNB 87.0° and ANB −5.5°. The both gonial angles were 138.2°, and the mandibular width was 110.5 mm.
The preoperative plan and simulated operation were performed according the 3D-reconstructed model, including Le Fort I osteotomy, SSRO, genioplasty and right mandibular border ostectomy. According to the design above, two bite plates and one surgical template were made (Fig. 11).
The patient was prepared under general anesthesia. The upper and lower jaws were exposed. The surgical sequence was as follows. First, Le Fort I osteotomy was performed and then the mandibular border ostectomy. SSRO and genioplasty were last. While performing mandibular border ostectomy, the surgical template was fixed (Fig. 12) and the osteotomy was performed along the edge of it (Fig. 13). No alveolar neurovascular bundle was directly injured during the surgical procedure. All the rigid internal fixations were achieved with screws and plates routinely.
The patient showed good jaw bone symmetry by CT scan (Figs. 14, 15) and good facial symmetry (Figs. 16, 17) after six months of follow-up. The data after operation were obtained, including SNA 83°, SNB 80° and ANB 3°. The gonial angle of the left was 124.1° and the right 123.5°. The asymmetry and hyperevolutism of the mandible were improved markedly. The overall facial contour was symmetrical, balanced and harmonious. No osteonecrosis or bone displacement happened.
Conclusion
The results of our study illustrated the predictability, feasibility and reliability of simultaneous mandibular contour osteoplasty and orthognathic surgery with the assistance of 3D printing technology. Our technique could achieve functional improvement and an aesthetic profile at the same time.
Discussion
It is a proverbially accepted concept in Oriental culture that prominent facial bones tend to express a forceful temperament and ovoid facial features tend to express a soft temperament [1]. So our clinical study is relatively unique to Orientals. According to our study, the single-stage surgery, which combines orthognathic surgery with mandibular contour osteoplasty, was confirmed feasible with the aid of 3D printing technology.
The 3D printing technique plays a significant role in the mandibular contour osteoplasty. The precise 3D printing model shows the anatomical details of the mandible, especially the location of the inferior alveolar canal and the thickness of the lateral cortex of the mandible [15]. Accurate diagnosis, preoperative plans, simulated operation and surgical templates could be made before the surgical procedures. Besides, the surgical template is an accurate way of transferring the preoperative plan to the actual operation. The surgeons can perform osteotomy easily and achieve accurate reconstruction of skeletal constructs with the help of the 3D printing technique. Some unfavorable results could be avoided, such as overcorrection/undercorrection, inferior alveolar nerve injury and facial asymmetry. So the extra time and expense (about 250 dollars) spent on the 3D printing model are worth it. What is more, it provides an effective way for communicating with the patients.
There were tiny deviations between simulation and postoperation in our study. Several authors have proposed the success criteria—a difference of a maximum of a 2.0 mm between the expected and the actual outcome [16, 17]. Our study showed that the deviations of the gonial angle and the mandibular width were 0.61° ± 0.27 and 0.49 mm ± 0.43, respectively. There was no significant difference between simulation and postoperation (Table 2). Furthermore, it is reported that the CT scan data are highly accurate with a mean error of less than 0.5 mm, whereas a mean error of less than 0.3 mm may occur because of the course of 3D rendering [18, 19]. Our sample capacity was relatively less. We could not subdivide the sample into smaller groups to analyze the effects of different surgeons and methods. In addition, although the surgical template could guide the range of bone grinding in MOCG, there was still some unpredictability in the thickness of bone resection. It is a significant issue to be addressed in a future study [20].
The problem of mandibular bone segments healing has been considered. According to oriented animal experiments and clinical trials about postoperative skeletal stability, MAO Xiao-bin et al. [21] and Kim et al. [15] had proved that mandibular angle ostectomy and SSRO could be carried out simultaneously. They have confirmed that postoperative blood supply returns to normal and necrosis of bone segments generally does not occur. Our team did not find the case of poor healing or long-term resorption of bone during the follow-up. So we come to the conclusion that indication and preoperative design are keys to favorable outcomes.
The hameochronous resection of partial masseter muscle has been reported [22]. Nevertheless, it is not certainly necessary at all times, even if requested [23]. As masseter atrophy may occur spontaneously after the operation, the hameochronous resection of muscle may lead to excessive atrophy and too narrow of a facial outline [24, 25]. The postoperative soft tissue swelling or absorption is controversial in any osteotomy. For these situations, secondary repair is sometimes suggested, such as injection of botulinum toxin, lipectomy of buccal pads or excision of partial masseter muscle, which can be performed under local anesthesia [26].
Orthognathic surgery is becoming more and more precise, and many new cross-designs of multiple surgical procedures have been achieved. Our team has proposed the concept of “Precision Technique in Orthognathic Surgery.” The precision technique in orthognathic surgery relies on the progress of multidisciplinary coordination, such as digital technology, 3D printing, navigation technology and special surgical instruments for orthognathic surgery, which pushes orthognathic surgery toward the digital and personal direction. We believe that the concept will become increasingly popular.
References
Terajima M, Nakasima A, Aoki Y, Goto TK, Tokumori K, Mori N, Hoshino Y (2009) A 3-dimensional method for analyzing the morphology of patients with maxillofacial deformities. Am J Orthod Dentofacial Orthop 136(6):857–867
Lonic D, Lo LJ (2016) Three-dimensional simulation of orthognathic surgery-surgeon’s perspective. J Formos Med Assoc 115(6):387–388
Borzabadi-Farahani A, Eslamipour F, Shahmoradi M (2016) Functional needs of subjects with dentofacial deformities: a study using the index of orthognathic functional treatment need (IOFTN). J Plast Reconstr Aesthet Surg 69(6):796–801
Tian KY, Li QQ, Liu XJ, Wang XX, Li ZL, Wang X (2016) Evaluation of therapeutic effect of virtual design for correcting facial asymmetry of skeletal Class III deformity. Zhonghua Kou Qiang Yi Xue Za Zhi 51(10):594–599
Cousley RR, Turner MJ (2014) Digital model planning and computerized fabrication of orthognathic surgery wafers. J Orthod 41(1):38–45
Suojanen J, Leikola J, Stoor P (2017) The use of patient-specific implants in orthognathic surgery: a series of 30 mandible sagittal split osteotomy patients. J Craniomaxillofac Surg 44(12):1913–1916
Wang L, Tian D, Sun X, Xiao Y, Chen L, Wu G (2017) The precise repositioning instrument for genioplasty and a three-dimensional printing technique for treatment of complex facial asymmetry. Aesth Plast Surg. doi:10.1007/s00266-017-0875-2
Hernandez-Alfaro F, Guijarro-Martinez R (2013) New protocol for three-dimensional surgical planning and CAD/CAM splint generation in orthognathic surgery: an in vitro and in vivo study. J Oral Maxillofac Surg 42:1547–1556
Lee YC, Sohn HB, Kim SK, Bae OY, Lee JH (2015) A novel method for the management of proximal segment using computer assisted simulation surgery: correct condyle head positioning and better proximal segment placement. Maxillofac Plast Reconstr Surg 37(1):21
Gateno J, Xia JJ, Teichgraeber JF (2011) New 3-dimensional cephalometric analysis for orthognathic surgery. J Oral Maxillofac Surg 69(3):606–622
Popat H, Richmond S, Marshall D, Rosin P (2012) Three-dimensional assessment of functional change following class 3 orthognathic correction—a preliminary report. J Cranio maxillofac Surg 40:36–42
Ireland AJ, Cunningham SJ, Petrie A (2014) An index of orthognathic functional treatment need (IOFTN). J Orthod 41:77–83
Ye N, Long H, Zhu S (2015) The accuracy of computer image-guided template for mandibular angle ostectomy. Aesthet Plast Surg 39:117
Zhao M, ZWu G (2017) The appropriative retractors for genioplasty. J Craniofac Surg 28(1):252–253
Kim CH, Lee JH, Cho JY, Kim KW (2007) Skeletal stability after simultaneous mandibular angle resection and sagittal split ramus osteotomy for correction of mandible prognathism. J Oral Maxillofac Surg 65:192
Hsu SSP, Gateno J, Bell RB, Hirsch DL, Markiewicz MR, Teichgraeber JF, Zhou XB, Xia JJ (2013) Accuracy of a computer-aided surgical simulation protocol for orthognathic surgery: a prospective multicenter study. J Oral Maxillofac Surg 71(1):128–142
Tucker S, Cevidanes LHS, Styner M, Kim H, Reyes M, Proffit W, Turvey T (2010) Comparison of actual surgical outcomes and 3-dimensional surgical simulations. J Oral Maxillofac Surg 61(10):2412–2421
Marmulla R, Wo¨rtche R, Mu¨hling J, Hassfeld S (2005) Geometric accuracy of the NewTom 9000 cone beam CT. Dentomaxillofac Radiol 34:28–31
Maloney K, Bastidas J, Freeman K, Olson TR, Kraut RA (2011) Cone beam computed tomography and SimPlant materialize dental software versus direct measurement of the width and height of the posterior mandible: an anatomic study. J Oral Maxillofac Surg 69:1923–1929
Sun XM, Wu GM (2015) The precise repositioning instrument for genioplasty. J Craniofac Surg 26(8):2417
Mao XB, Wang T, Yang DK, Zang GM (2011) The dynamics of blood supply of animal experimental study for simultaneous mandibular sagittal split osteotomy and mandibular angle plasty. J Chongqing Med Univ 6(36):718–720
Anderson J Greg, Laney Thomas J (2002) Combined orthognathic and facial aesthetic surgery with case reports. J Tenn Dent Assoc 82(3):52
RaffainiM Pisani C (2015) Orthognathic surgery with or without autologous fat micrograft injection: preliminary report on aesthetic outcomes and patient satisfaction. Int J Oral Maxillofac Surg 44(3):362–370
Trawitzki LV, Dantas RO, Mello-Filho FV, Elias-Júnior J (2006) Effect of treatment of dentofacial deformity on masseter muscle thickness. Arch Oral Biol 51(12):1086–1092
Lee ST, Mori Y, Minami K, An CH, Park JW, Kwon TG (2013) Does skeletal surgery for asymmetric mandibular prognathism influence the soft tissue contour and thickness? J Oral Maxillofac Surg 71(9):1577–1587
Sarver DM, Rousso DR (2004) Plastic surgery combined with orthodontic and orthognathic procedures. Am J Orthod Dentofacial Orthop 126(3):305–307
Acknowledgements
This study was funded by grants from the Committee of National Nature Science Foundation (No. 81400532) in China, Norman Bethune Program of Jilin University (No. 2015301), Fund Project of Jilin Health and Family Planning Commission (No. 2015Q017), Jilin University’s Outstanding Young Teacher Training Program (No. 419080500367), the Program for Fundamental Research of Jilin University (No. 450060491134) and the 13th Five-Year science and technology project of the Education Department of Jilin Province (No. 2016486).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the hospital research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Xiao, Y., Sun, X., Wang, L. et al. The Application of 3D Printing Technology for Simultaneous Orthognathic Surgery and Mandibular Contour Osteoplasty in the Treatment of Craniofacial Deformities. Aesth Plast Surg 41, 1413–1424 (2017). https://doi.org/10.1007/s00266-017-0914-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-017-0914-z